How Long Is Long Enough? Controlling for Acute Caffeine Intake in Cardiovascular Research
Abstract
:1. Introduction
1.1. The Physiology of Caffeine
1.2. Aims and Objectives
2. Methods
2.1. Subjects and Study Design
2.2. Procedure
2.2.1. Phase One
2.2.2. Phase Two
2.2.3. Phase Three
2.3. Measures (Refer to Table 2 for List of Measures Used)
2.3.1. Physiological Measures
Electrocardiography (ECG)
Respiration
Blood Pressure (BP)
Impedance Cardiography (ICG)
2.3.2. Psychological Measures
Depression Anxiety and Stress Scale (DASS)
Brief Mood Introspection Scale (BMIS)
Task Ratings
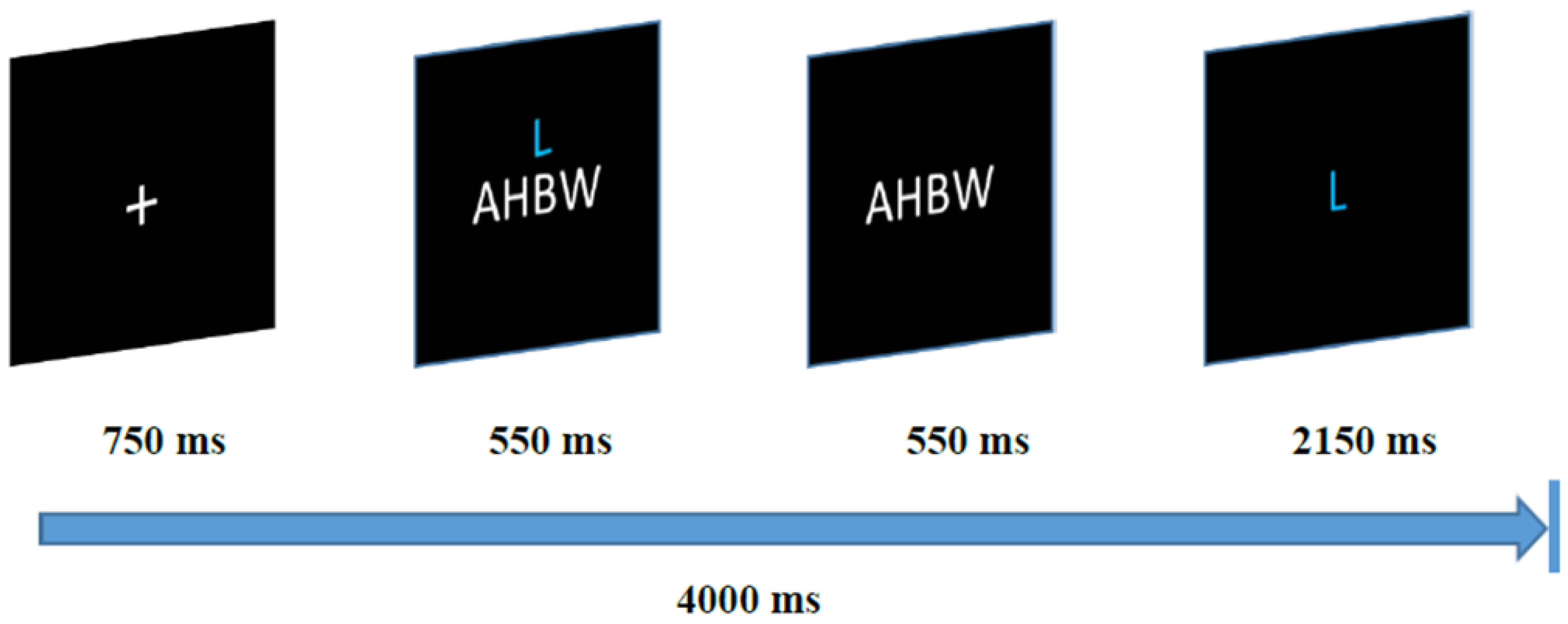
2.4. Experimental Tasks
| Physiological | Psychological/Self-Report | Experimental Tasks |
|---|---|---|
| ECG-derived: Heart Rate, High-Frequency Heart Rate Variability (HF-HRV), root mean square of successive R-R interval differences (RMSSD) | Depression Anxiety and Stress Scale (DASS): Depression, Anxiety, and Stress subscales Brief Mood Introspection Scale (BMIS): Dimensions of Mood: Pleasant-Unpleasant, Arousal-Calm, Positive-Tired, and Negative-Calm Self-Reported Task Ratings | Hand Cold Pressor (3 min) Working Memory Task (3 min): Percentage Correct |
| Blood Pressure: Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Mean Arterial Pressure (MAP) | ||
| Impedance Cardiography (ICG)-derived: Pre-ejection period (PEP), Left-ventricular ejection time (LVET), Systemic Vascular Resistance (SVR), and Systemic Vascular Resistance Index (SVRI) |
2.5. Data Reduction and Analyses
2.5.1. Physiological Measures
2.5.2. Self-Report Measures
2.5.3. Sex Effects
2.5.4. Missing Data
3. Results
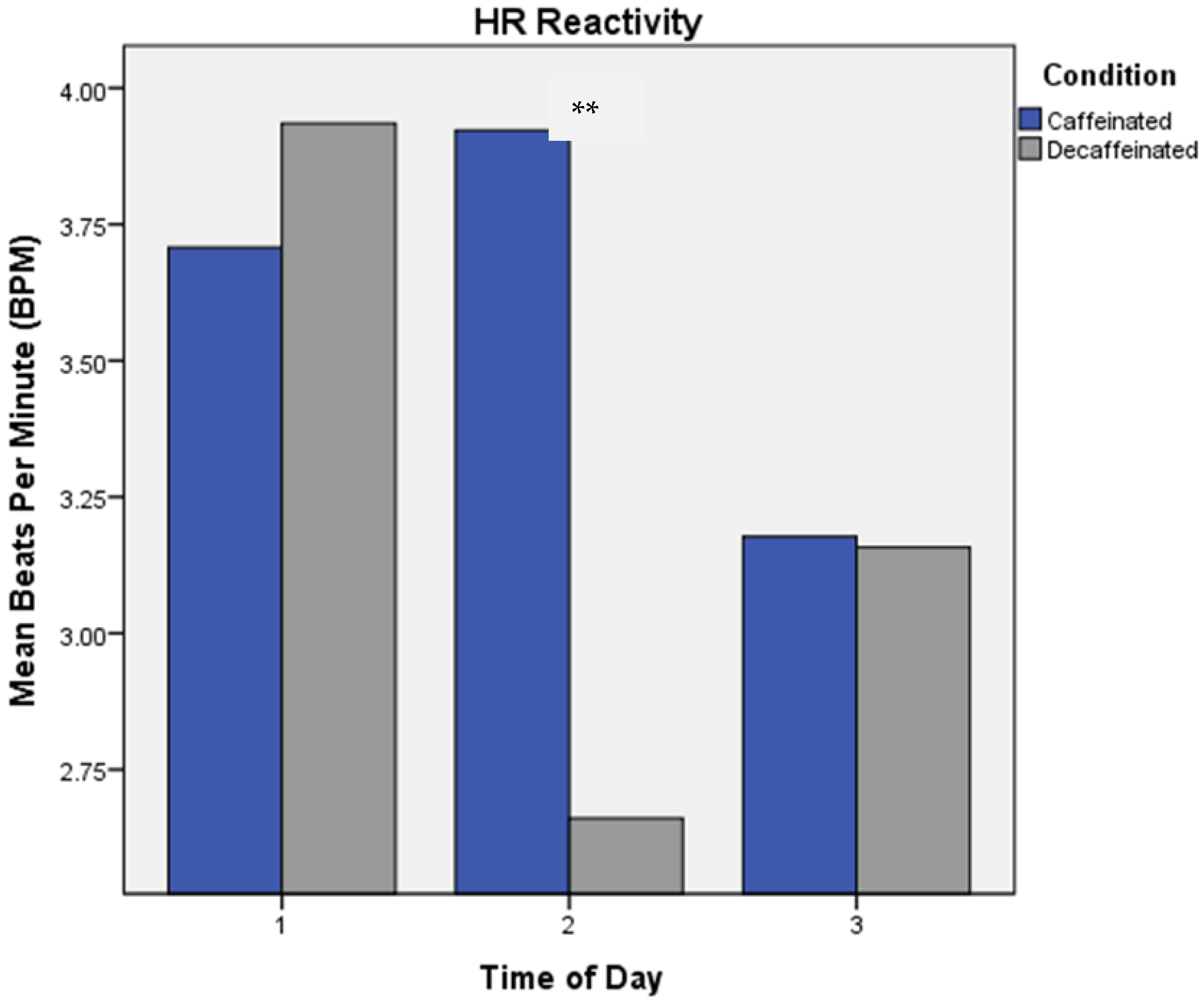
3.1. Heart Rate (HR)
3.2. High-Frequency Heart Rate Variability (HF-HRV)
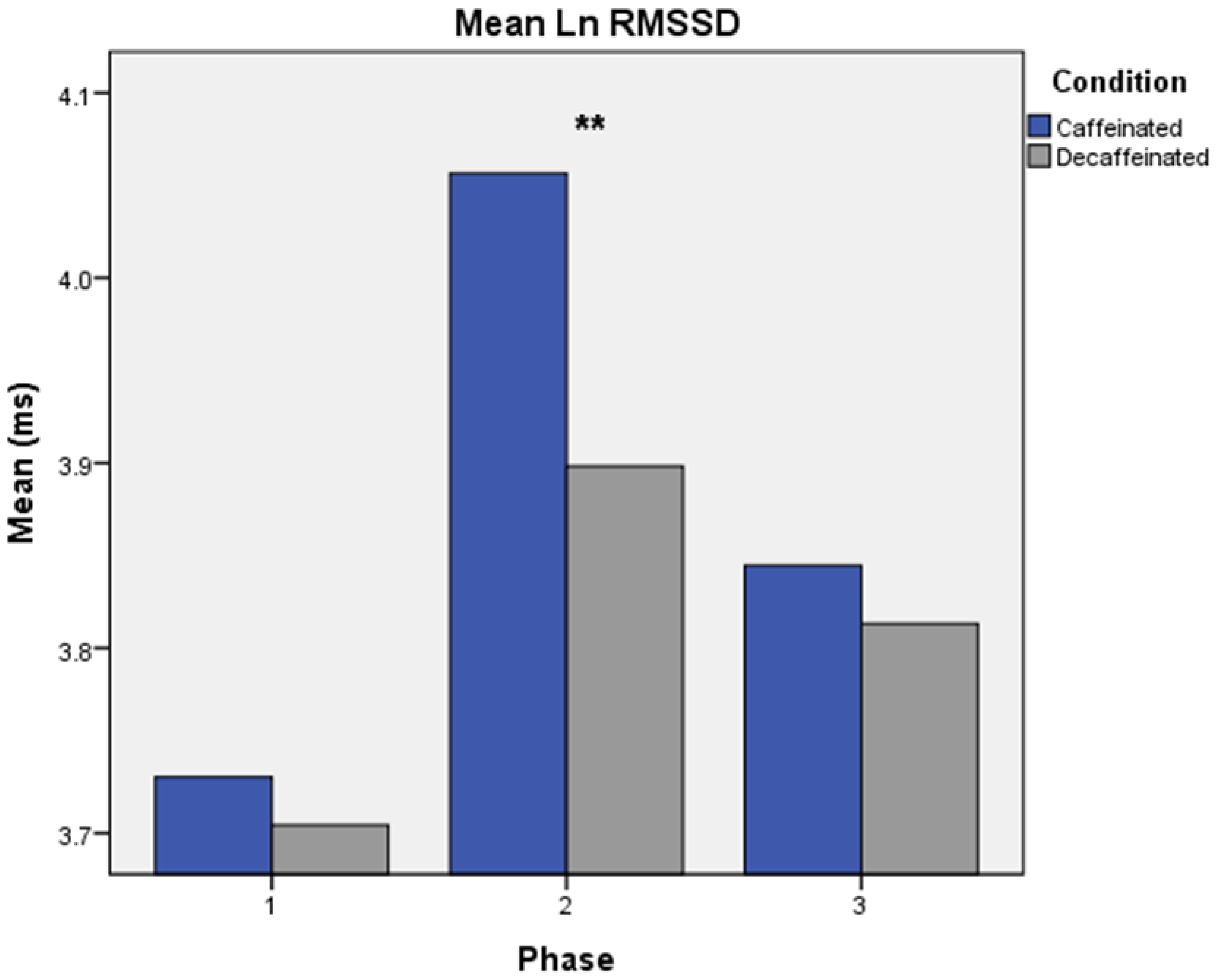
3.3. Root Mean Squared Successive Differences of R-R Intervals (RMSSD)
3.4. Blood Pressure (BP)
3.5. Pre-Ejection Period (PEP) and Left Ventricular Ejection Time (LVET)
3.6. Systemic Vascular Resistance (SVR) and Systemic Vascular Resistance Index (SVRI)
3.7. Self-Report Measures
3.8. Ancillary Post Hoc Analyses
3.8.1. Sex Differences
3.8.2. Task Ratings
3.8.3. Consumption Patterns and Perceptions of Caffeine Condition
4. Discussion
4.1. Physiological Responses
4.2. Self-Report Responses
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Mitchell, D.C.; Knight, C.A.; Hockenberry, J.; Teplansky, R.; Hartman, T.J. Beverage caffeine intakes in the U.S. Food Chem. Toxicol. 2014, 63, 136–142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koenig, J.; Jarczok, M.N.; Kuhn, W.; Morsch, K.; Schäfer, A.; Hillecke, T.K.; Thayer, J.F. Impact of caffeine on heart rate variability: A systematic review. J. Caffeine 2013, 3, 22–37. [Google Scholar] [CrossRef]
- Lane, J.D.; Adcock, R.A.; Williams, R.B.; Kuhn, C.M. Caffeine effects on cardiovascular and neuroendocrine responses to acute psychosocial stress and their relationship to level of habitual caffeine consumption. Psychosom. Med. 1990, 52, 320–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lane, J.D.; Williams, R.B., Jr. Cardiovascular effects of caffeine and stress in regular coffee drinkers. Psychophysiology 1987, 24, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Lovallo, W.R.; Pincomb, G.A.; Sung, B.H.; Everson, S.A.; Passey, R.B.; Wilson, M.F. Hypertension risk and caffeine’s effect on cardiovascular activity during mental stress in young men. Health Psychol. 1991, 10, 236–243. [Google Scholar] [CrossRef]
- Grant, S.S.; Magruder, K.P.; Friedman, B.H. Controlling for caffeine in cardiovascular research: A critical review. Int. J. Psychophysiol. 2018, 133, 193–201. [Google Scholar] [CrossRef]
- Schmidt, B. Proof of Principle studies. Epilepsy Res. 2006, 68, 48–52. [Google Scholar] [CrossRef]
- Echeverri, D.; Montes, F.R.; Cabrera, M.; Galán, A.; Prieto, A. Caffeine’s Vascular Mechanisms of Action. Int. J. Vasc. Med. 2010, 2010, 834060. [Google Scholar] [CrossRef] [Green Version]
- Mort, J.R.; Kruse, H.R. Timing of blood pressure measurement related to caffeine consumption. Ann. Pharmacother. 2008, 42, 105–110. [Google Scholar] [CrossRef]
- Kroon, L.A. Drug interactions with smoking. Am. J. Health Syst. Pharm. 2007, 64, 1917–1921. [Google Scholar] [CrossRef]
- Nichols, M.; Robinson, G.; Bounds, W.; Newman, B.; Guillebaud, J. Effect of four combined oral contraceptives on blood pressure in the pill-free interval. Contraception 1993, 47, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Renda, G.; Zimarino, M.; Antonucci, I.; Tatasciore, A.; Ruggieri, B.; Bucciarelli, T.; Prontera, T.; Stuppia, L.; De Caterina, R. Genetic determinants of blood pressure responses to caffeine drinking. Am. J. Clin. Nutr. 2012, 95, 241–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitsett, T.L.; Manion, C.V.; Christensen, H.D. Cardiovascular effects of coffee and caffeine. Am. J. Cardiol. 1984, 53, 918–922. [Google Scholar] [CrossRef]
- Nurminen, M.L.; Niittynen, L.; Korpela, R.; Vapaatalo, H. Coffee, caffeine and blood pressure: A critical review. Eur. J. Clin. Nutr. 1999, 53, 831–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pincomb, G.A.; Sung, B.H.; Lovallo, W.R.; Wilson, M.F. Consistency of cardiovascular response pattern to caffeine across multiple studies using impedance and nuclear cardiography. Biol. Psychol. 1993, 36, 131–138. [Google Scholar] [CrossRef]
- James, J.E. Critical review of dietary caffeine and blood pressure: A relationship that should be taken more seriously. Psychosom. Med. 2004, 66, 63–71. [Google Scholar] [CrossRef]
- Bender, A.M.; Donnerstein, R.L.; Samson, R.A.; Zhu, D.; Goldberg, S.J. Hemodynamic effects of acute caffeine ingestion in young adults. Am. J. Cardiol. 1997, 79, 696–699. [Google Scholar] [CrossRef]
- Conrad, K.A.; Blanchard, J.; Trang, J.M. Cardiovascular effects of caffeine in elderly men. J. Am. Geriatr. Soc. 1982, 30, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Hartley, T.R.; Lovallo, W.R.; Whitsett, T.L. Cardiovascular effects of caffeine in men and women. Am. J. Cardiol. 2004, 93, 1022–1026. [Google Scholar] [CrossRef]
- Farag, N.H.; Vincent, A.S.; McKey, B.S.; Al’Absi, M.; Whitsett, T.L.; Lovallo, W.R. Sex differences in the hemodynamic responses to mental stress: Effect of caffeine consumption. Psychophysiology 2006, 43, 337–343. [Google Scholar] [CrossRef]
- Friedman, B.H. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol. Psychol. 2007, 74, 185–199. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.H.; Thayer, J.F. Anxiety and autonomic flexibility: A cardiovascular approach. Biol. Psychol. 1998, 47, 243–263. [Google Scholar] [CrossRef] [PubMed]
- Farag, N.H.; Vincent, A.S.; McKey, B.S.; Whitsett, T.L.; Lovallo, W.R. Hemodynamic mechanisms underlying the incomplete tolerance to caffeine’s pressor effects. Am. J. Cardiol. 2005, 95, 1389–1392. [Google Scholar] [CrossRef] [PubMed]
- Juliano, L.M.; Griffiths, R.R. A critical review of caffeine withdrawal: Empirical validation of symptoms and signs, incidence, severity, and associated features. Psychopharmacology 2004, 176, 1–29. [Google Scholar] [CrossRef]
- Dodd, F.L.; Kennedy, D.O.; Riby, L.M.; Haskell-Ramsay, C.F. A double-blind, placebo-controlled study evaluating the effects of caffeine and L-theanine both alone and in combination on cerebral blood flow, cognition and mood. Psychopharmacology 2015, 232, 2563–2576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McIlvain, G.E.; Noland, M.P.; Bickel, R. Caffeine consumption patterns and beliefs of college freshmen. Am. J. Health Educ. 2011, 42, 235–244. [Google Scholar] [CrossRef] [Green Version]
- Mahoney, C.R.; Giles, G.E.; Marriott, B.P.; Judelson, D.A.; Glickman, E.L.; Geiselman, P.J.; Lieberman, H.R. Intake of caffeine from all sources and reasons for use by college students. Clin. Nutr. 2019, 38, 668–675. [Google Scholar] [CrossRef] [Green Version]
- Fulgoni, V.L., III; Keast, D.R.; Lieberman, H.R. Trends in intake and sources of caffeine in the diets of US adults: 2001–2010. Am. J. Clin. Nutr. 2015, 101, 1081–1087. [Google Scholar] [CrossRef] [Green Version]
- Arciero, P.J.; Gardner, A.; Benowitz, N.; Poehlman, E. Relationship of blood pressure, heart rate and behavioral mood state to norepinephrine kinetics in syounger and older men following caffeine ingestion. Eur. J. Clin. Nutr. 1998, 52, 805–812. [Google Scholar] [CrossRef] [Green Version]
- Addicott, M.A.; Yang, L.L.; Peiffer, A.M.; Laurienti, P.J. Methodological considerations for the quantification of self-reported caffeine use. Psychopharmacology 2009, 203, 571–578. [Google Scholar] [CrossRef]
- Mayer, J.D.; Gaschke, Y.N. The experience and meta-experience of mood. J. Pers. Soc. Psychol. 1988, 55, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Piferi, R.L.; Kline, K.A.; Younger, J.; Lawler, K.A. An alternative approach for achieving cardiovascular baseline: Viewing an aquatic video. Int. J. Psychophysiol. 2000, 37, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Jennings, J.R.; Kamarck, T.; Stewart, C.; Eddy, M.; Johnson, P. Alternate cardiovascular baseline assessment techniques: Vanilla or resting baseline. Psychophysiology 1992, 29, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Reggio, G. (Director) Powaqaatsi: Life in Transformation; Motion Picture; MGM/United Artists: Beverly Hills, CA, USA, 1988. [Google Scholar]
- Richter, M.; Friedrich, A.; Gendolla, G.H. Task difficulty effects on cardiac activity. Psychophysiology 2008, 45, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, S. High-speed scanning in human memory. Science 1966, 153, 652–654. [Google Scholar] [CrossRef] [Green Version]
- Jern, S. Effects of acute carbohydrate administration on central and peripheral hemodynamic responses to mental stress. Hypertension 1991, 18, 790–797. [Google Scholar] [CrossRef] [Green Version]
- Synowski, S.J.; Kop, W.J.; Warwick, Z.S.; Waldstein, S.R. Effects of glucose ingestion on autonomic and cardiovascular measures during rest and mental challenge. J. Psychosom. Res. 2013, 74, 149–154. [Google Scholar] [CrossRef] [Green Version]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Vella, E.J.; Friedman, B.H. Autonomic characteristics of defensive hostility: Reactivity and recovery to active and passive stressors. Int. J. Psychophysiol. 2007, 66, 95–101. [Google Scholar] [CrossRef] [Green Version]
- Etzel, J.A.; Johnsen, E.L.; Dickerson, J.; Tranel, D.; Adolphs, R. Cardiovascular and respiratory responses during musical mood induction. Int. J. Psychophysiol. 2006, 61, 57–69. [Google Scholar] [CrossRef]
- Brown, T.A.; Chorpita, B.F.; Korotitsch, W.; Barlow, D.H. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav. Res. Ther. 1997, 35, 79–89. [Google Scholar] [CrossRef]
- McGinley, J.J.; Friedman, B.H. Autonomic responses to lateralized cold pressor and facial cooling tasks. Psychophysiology 2015, 52, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.W.; Olchowski, A.E.; Gilreath, T.D. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev. Sci. 2007, 8, 206–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van den Buuse, M.; Van Acker, S.A.; Fluttert, M.; De Kloet, E.R. Blood pressure, heart rate, and behavioral responses to psychological "novelty" stress in freely moving rats. Psychophysiology 2001, 38, 490–499. [Google Scholar] [CrossRef] [PubMed]
- La Monica, M.B.; Fukuda, D.H.; Gonzalez, A.M.; Wang, R.; Wells, A.J.; Stout, J.R.; Hoffman, J.R. Time-Released Caffeine Ingestion in Habitual Users May Extend Parasympathetic Influence as Determined by Heart Rate Variability. FASEB J. 2017, 31, 843.15. [Google Scholar]
- Monda, M.; Viggiano, A.; Vicidomini, C.; Viggiano, A.; Iannaccone, T.; Tafuri, D.; De Luca, B. Espresso coffee increases parasympathetic activity in young, healthy people. Nutr. Neurosci. 2009, 12, 43–48. [Google Scholar] [CrossRef]
- Zimmermann-Viehoff, F.; Thayer, J.; Koenig, J.; Herrmann, C.; Weber, C.S.; Deter, H.C. Short-term effects of espresso coffee on heart rate variability and blood pressure in habitual and non-habitual coffee consumers—A randomized crossover study. Nutr. Neurosci. 2016, 19, 169–175. [Google Scholar] [CrossRef]
- Hibino, G.; Moritani, T.; Kawada, T.; Fushiki, T. Caffeine enhances modulation of parasympathetic nerve activity in humans: Quantification using power spectral analysis. J. Nutr. 1997, 127, 1422–1427. [Google Scholar] [CrossRef] [Green Version]
- McIntosh, H.D.; Russell, B.R.; Cochran, J.R.; Sollers, J.J., III. The heart of the pressor effect: Acute caffeine ingestion and resting heart rate variability. J. Caffeine Res. 2017, 7, 23–30. [Google Scholar] [CrossRef]
- Huang, C.M.; Chang, H.C.; Kao, S.T.; Li, T.C.; Wei, C.C.; Chen, C.; Liao, Y.T.; Chen, F.J. Radial pressure pulse and heart rate variability in heat- and cold-stressed humans. Evid.-Based Complement. Altern. Med. 2011, 2011, 751317. [Google Scholar] [CrossRef] [Green Version]
- Park, G.; Thayer, J.F. From the heart to the mind: Cardiac vagal tone modulates top-down and bottom-up visual perception and attention to emotional stimuli. Front. Psychol. 2014, 5, 278. [Google Scholar] [CrossRef]
- Mravec, B. Role of catecholamine-induced activation of vagal afferent pathways in regulation of sympathoadrenal system activity: Negative feedback loop of stress response. Endocr. Regul. 2011, 45, 37–41. [Google Scholar]
- Ruxton, C. The impact of caffeine on mood, cognitive function, performance and hydration: A review of benefits and risks. Nutr. Bull. 2008, 33, 15–25. [Google Scholar] [CrossRef]
- Rennefeld, C.; Wiech, K.; Schoell, E.D.; Lorenz, J.; Bingel, U. Habituation to pain: Further support for a central component. Pain 2010, 148, 503–508. [Google Scholar] [CrossRef]
- Keogh, E.; Witt, G. Hypoalgesic effect of caffeine in normotensive men and women. Psychophysiology 2001, 38, 886–895. [Google Scholar] [CrossRef]
- Norton, T.R.; Lazev, A.B.; Sullivan, M.J. The “buzz” on caffeine: Patterns of caffeine use in a convenience sample of college students. J. Caffeine Res. 2011, 1, 35–40. [Google Scholar] [CrossRef]
- Goldstein, H. Multilevel Statistical Models; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Porkka-Heiskanen, T.; Strecker, R.E.; McCarley, R.W. Brain site-specificity of extracellular adenosone concentration changes during sleep-deprivation and spontaneous sleep: An in vivo microdialysis study. Neuroscience 2000, 99, 507–517. [Google Scholar] [CrossRef]
- Scammell, T.E.; Gerashchenko, D.Y.; Mochizuki, T.; McCarthy, M.T.; Estabrooke, V.; Sears, C.A.; Saper, C.B.; Urade, Y.; Hayaish, O. An adenosine A2a agonist increases sleep and induces Fos in ventrolateral preoptic neurons. Neuroscience 2001, 107, 653–663. [Google Scholar] [CrossRef]
- Thakkar, M.M.; Winston, S.; McCarley, R.W. Orexin neurons of the hypothalamus express adenosine A1 receptors. Brain Res. 2002, 944, 190–194. [Google Scholar] [CrossRef]



| Demographic Measures | Mean ± SD or N (%) |
|---|---|
| Age (years) | 20.9 ± 1.92 |
| Race | |
| Caucasian African American/Black Asian Latino/Hispanic | 26 (60.4%) 1 (2.3%) 11 (25.5%) 1 (2.3%) |
| BMI (kg/m2) | |
| Male Female | 25.9 ± 3.43 24.0 ± 3.52 |
| Baseline Physiological Measures HR (bpm) RR (bpm) Ln HF-HRV (ms2) Ln RMSSD (ms) SBP (mmHg) DBP (mmHg) MAP (mmHg) PEP (ms) LVET (ms) SVR (dynes·s·cm−5) SVRI (dynes·s·cm−5·m2) | Mean (SE) 72.43 (1.76) 16.38 (0.54) 6.63 (0.17) 3.70 (0.11) 120.42 (1.64) 69.50 (1.09) 86.76 (1.22) 96.52 (2.40) 340.60 (4.14) 1038.61 (45.76) 1973.65 (102.43) |
| Physiological Measure | Mean (SD) | Mean (SD) | N |
|---|---|---|---|
| Caffeinated Day | Memory Task | Cold Pressor Task | |
| HR (bpm) | 70.19 (13.96) | 73.22 (11.45) | 36 |
| RR (bpm) | 18.63 (3.51) | 16.10 (4.59) | 39 |
| Ln HF-HRV (ms2) | 7.43 (1.09) | 7.16 (1.25) | 36 |
| Ln RMSSD (ms) | 4.14 (0.59) | 4.00 (0.50) | 36 |
| SBP (mmHg) | 131.14 (14.45) | 137.32 (17.93) | 37 |
| DBP (mmHg) | 77.42 (9.67) | 83.09 (11.88) | 37 |
| MAP (mmHg) | 95.74 (10.82) | 101.02 (15.64) | 37 |
| PEP (ms) | 99.84 (15.90) | 99.15 (15.44) | 24 |
| LVET (ms) | 357.02 (27.67) | 358.84 (23.54) | 24 |
| SVR (dynes·s·cm−5) | 1124.85 (298.87) | 1186.24 (271.25) | 24 |
| SVRI (dynes·s·cm−5·m2) | 2124.77 (737.86) | 2224.13 (667.94) | 24 |
| Decaffeinated Day | |||
| HR (bpm) | 73.78 (12.38) | 75.50 (10.62) | 36 |
| RR (bpm) | 18.06 (3.25) | 16.44 (4.05) | 39 |
| Ln HF-HRV (ms2) | 7.01 (1.08) | 6.82 (1.25) | 36 |
| Ln RMSSD (ms) | 3.89 (0.54) | 3.88 (0.58) | 36 |
| SBP (mmHg) | 126.52 (12.95) | 138.77 (14.86) | 37 |
| DBP (mmHg) | 73.53 (9.48) | 82.45 (10.69) | 37 |
| MAP (mmHg) | 91.35 (10.36) | 100.34 (12.60) | 37 |
| PEP (ms) | 101.21 (13.53) | 98.54 (10.77) | 24 |
| LVET (ms) | 347.33 (27.65) | 357.07 (25.72) | 24 |
| SVR (dynes·s·cm−5) | 1188.92 (426.12) | 1059.03 (282.11) | 24 |
| SVRI (dynes·s·cm−5·m2) | 2236.12 (990.19) | 1956.95 (672.61) | 24 |
| Cardiovascular Measure | Experimental Phase | Mean Reactivity (± SD) | |
|---|---|---|---|
| Memory Task | CP Task | ||
| HR (bpm) | 1 2 3 | 3.88 (5.80) 3.06 (7.24) 3.77 (5.73) | 3.54 (5.72) 4.79 (6.74) 2.58 (0.77) |
| Ln HF-HRV (ms2) | 1 2 3 | 0.14 (0.90) 0.43 (1.01) 0.26 (0.75) | 0.29 (0.76) 0.03 (0.73) 0.27 (0.77) |
| Ln RMSSD (ms) | 1 2 3 | 0.05 (0.32) 0.11 (0.39) 0.09 (0.36) | 0.06 (0.36) −0.06 (0.28) 0.06 (0.30) |
| SBP (mmHg) | 1 2 3 | 5.69 (6.98) 3.14 (6.11) 3.73 (5.64) | 13.98 (8.22) 11.97 (10.29) 11.84 (7.42) |
| DBP (mmHg) | 1 2 3 | 3.41 (5.20) 2.39 (5.62) 2.88 (4.20) | 11.34 (6.30) 10.41 (7.66) 7.69 (6.21) |
| MAP (mmHg) | 1 2 3 | 4.29 (5.57) 2.84 (5.34) 3.41 (4.51) | 12.76 (7.62) 10.24 (11.35) 9.98 (7.42) |
| PEP (ms) | 1 2 3 | 1.87 (8.28) −0.35 (4.37) 1.26(5.91) | −0.02 (8.92) −0.52 (6.41) 1.80 (5.78) |
| LVET (ms) | 1 2 3 | −0.25 (10.41) 0.04 (11.18) 0.69 (11.81) | 8.45 (18.29) 5.95 (14.48) 7.32 (16.97) |
| SVR (dynes·s·cm−5) | 1 2 3 | −8.94 (89.90) −24.36 (77.91) 11.76 (56.93) | 58.48 (140.89) 51.18 (282.74) 69.73 (151.14) |
| SVRI (dynes·s·cm−5·m2) | 1 2 3 | −15.62 (174.26) −55.47(165.93) 21.78 (108.40) | 97.50 (275.38) 46.67 (665.42) 126.34 (283.47) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grant, S.S.; Kim, K.; Friedman, B.H. How Long Is Long Enough? Controlling for Acute Caffeine Intake in Cardiovascular Research. Brain Sci. 2023, 13, 224. https://doi.org/10.3390/brainsci13020224
Grant SS, Kim K, Friedman BH. How Long Is Long Enough? Controlling for Acute Caffeine Intake in Cardiovascular Research. Brain Sciences. 2023; 13(2):224. https://doi.org/10.3390/brainsci13020224
Chicago/Turabian StyleGrant, Shara S., Kye Kim, and Bruce H. Friedman. 2023. "How Long Is Long Enough? Controlling for Acute Caffeine Intake in Cardiovascular Research" Brain Sciences 13, no. 2: 224. https://doi.org/10.3390/brainsci13020224
APA StyleGrant, S. S., Kim, K., & Friedman, B. H. (2023). How Long Is Long Enough? Controlling for Acute Caffeine Intake in Cardiovascular Research. Brain Sciences, 13(2), 224. https://doi.org/10.3390/brainsci13020224





