Abstract
This study aimed to determine the effects of balance training with weight shift-triggered electrical stimulation to improve balance, lower-extremity motor function, and activities of daily living in patients with stroke. The participants were randomly allocated to the balance training with electrical stimulation group (BT-ESG, n = 29) or the balance training group (BTG, n = 30). Both groups were trained 5 times per week for 6 weeks for 50 min per session. To evaluate static balance, postural sway was assessed and dynamic balance was assessed using the Berg Balance Scale (BBS), Timed Up and Go (TUG) test, and functional reach test (FRT). Lower-extremity motor function was assessed using the Fugl–Meyer assessment. Daily activities were assessed using the Modified Barthel Index. As for static balance, BT-ESG showed a significant improvement compared to BTG in postural swat in both the eyes-open (velocity moment; effect size, 0.88; 95% confidence interval, −1.16 to −1.30), or eyes-closed state (velocity moment; effect size, 0.81; 95% confidence interval, −1.22 to −0.27). Dynamic balance, which includes TUG (effect size, 0.90; 95% confidence interval, −4.67 to −1.25), BBS (effect size, 1.26; 95% confidence interval, −2.84 to 6.83), and FRT (effect size, 1.45; 95% confidence interval, 1.92 to 4.08), in addition to lower-extremity motor function (effect size, 1.38; 95% confidence interval, 2.25 to 4.97), and activities of daily living (effect size, 2.04; 95% confidence interval, 2.04 to 937), showed significant improvement in BT-ESG compared to BTG. These results suggest that balance training with weight shift-triggered electrical stimulation effectively improves balance, lower-extremity motor function, and activities of daily living in patients with stroke.
1. Introduction
Postural symmetry is essential for motor system function. The ability to transfer weight from one leg to the other is a fundamental component of walking and activities of daily living (ADL) [1]. Significant problems in chronic stroke patients include asymmetrical weight-bearing, body imbalance, and defects in weight transfer ability [2]. Patients with hemiplegia due to stroke show unbalanced weight-bearing, with less than 25–43% of the body weight on paretic limbs in the standing position [3,4,5]. Chronic stroke patients adopt compensatory strategies and an asymmetrical posture that puts less weight on the paretic limb, thereby not putting weight on the paretic limb [2,6]. This imbalance between the paretic and non-paretic limbs significantly reduces the walking ability of chronic hemiplegic patients, putting them at risk of falls and limiting their ADL [6,7]. The ideal goal in the functional rehabilitation of stroke patients is to restore their walking ability by maintaining a symmetrical posture with even weight support [2].
Electrical stimulation has been used for various purposes in the rehabilitation of stroke patients. It is an effective method for improving balance and walking ability and restoring posture and motor function [8]. Neuromuscular electrical stimulation induces muscle contraction on the paralyzed side and is widely used to prevent foot drop during gait training in patients with stroke [9]. Electrical stimulation induces functionally useful movements in muscles that cannot control voluntary movements in the central nervous system, thereby increasing the strength of specific muscles [10].
Electrical stimulation reportedly has the ability to improve the lower-extremity motor function of stroke patients [9,10]. However, it is necessary to induce muscle contraction at a specific time because equal weight-bearing is delayed, but current methods are insufficient. Thus, an electrical stimulation intervention method that can improve weight distribution and postural control ability between the paretic and non-paretic sides of stroke patients is needed.
An intelligent healthcare system that can help improve health based on IT technology has recently emerged [11,12]. In particular, as smartphones have become popular, technology that connects wearable devices that record health-related information and smartphones to provide this information has developed [13]. Wearable devices help health management by collecting data on patterns such as the number of steps, amount of physical activity, movement, and posture [14]. The use of wearable devices in the rehabilitation area can effectively promote motor learning by providing information accurately and quickly in real time [14].
Previous studies demonstrated the effectiveness of weight transfer training through biofeedback in hemiplegic patients at improving balance and walking ability [15]. As such, the augmentative feedback-based training method, which is useful in clinical practice, is being studied in various ways to improve patient function [16]. Stroke patients wore smart shoes and a wearable device and were trained with reinforcement feedback to reduce weight dependence of the non-paretic limb and improve gait asymmetry in the increased stance and single-support phases of the paretic limb [17,18].
Therefore, we hypothesized that weight dependence focused on the non-paretic limb could be controlled using balance training that induces equal weight support with electrical stimulation feedback, along with a pneumatic-pressure insole. We also believed that it would improve balance, lower-extremity motor function recovery, and ADL in patients with stroke. This study aimed to investigate the effects of balance training with weight shift-triggered electrical stimulation on static balance, dynamic balance, lower-extremity motor function recovery, and ADL in hemiplegic patients.
2. Materials and Methods
2.1. Subjects
Participants were recruited from chronic stroke patients hospitalized at S Hospital in Seoul, South Korea by publicizing the research purpose and inclusion criteria. In addition, the current study recruited late chronic phase patients whose onsets were more than a year without spontaneous recovery to observe the effects of intervention even more clearly. Among stroke patients, those who understood verbal instructions and had a Mini-Mental State Exam score of ≥24 were included. Those who could stand independently without assistance, with a Brunnstrom motor recovery level ≥ 4, with severe neglect or musculoskeletal abnormalities, with superficial metal (e.g., staples, pins and external fixators), who were suffering from cerebellar disease or dizziness, or with cardiovascular disease were excluded.
Among the patients who wished to participate, those who met the selection criteria were given an explanation of the study purpose, procedures, and precautions and were included upon completing a voluntary consent form. The study was approved by the Research Ethics Committee of Kyungdong University.
This was a randomized controlled trial. Because the intervention was an exercise, blinding of the therapist was not performed, and only the assessor was blinded so that the subject did not know the group allocations. A pilot study using the same exercise protocol was conducted to determine the sample size. Outcome measures in the pilot study were the Timed Up and Go (TUG) test, Berg Balance Scale (BBS), and functional reach test (FRT). We determined the effect size (f = 0.29) based on the value of the TUG test from the pilot study. The alpha error was set to 0.05, and the power was set to 0.8. Therefore, a total of 26 participants were required. Considering a dropout rate of 10%, 30 participants per group were selected. G* Power version 3.19 (Heinrich Heine University Düsseldor, Düsseldorf, Germany) was used for the sample size calculations.
2.2. Experimental Procedure
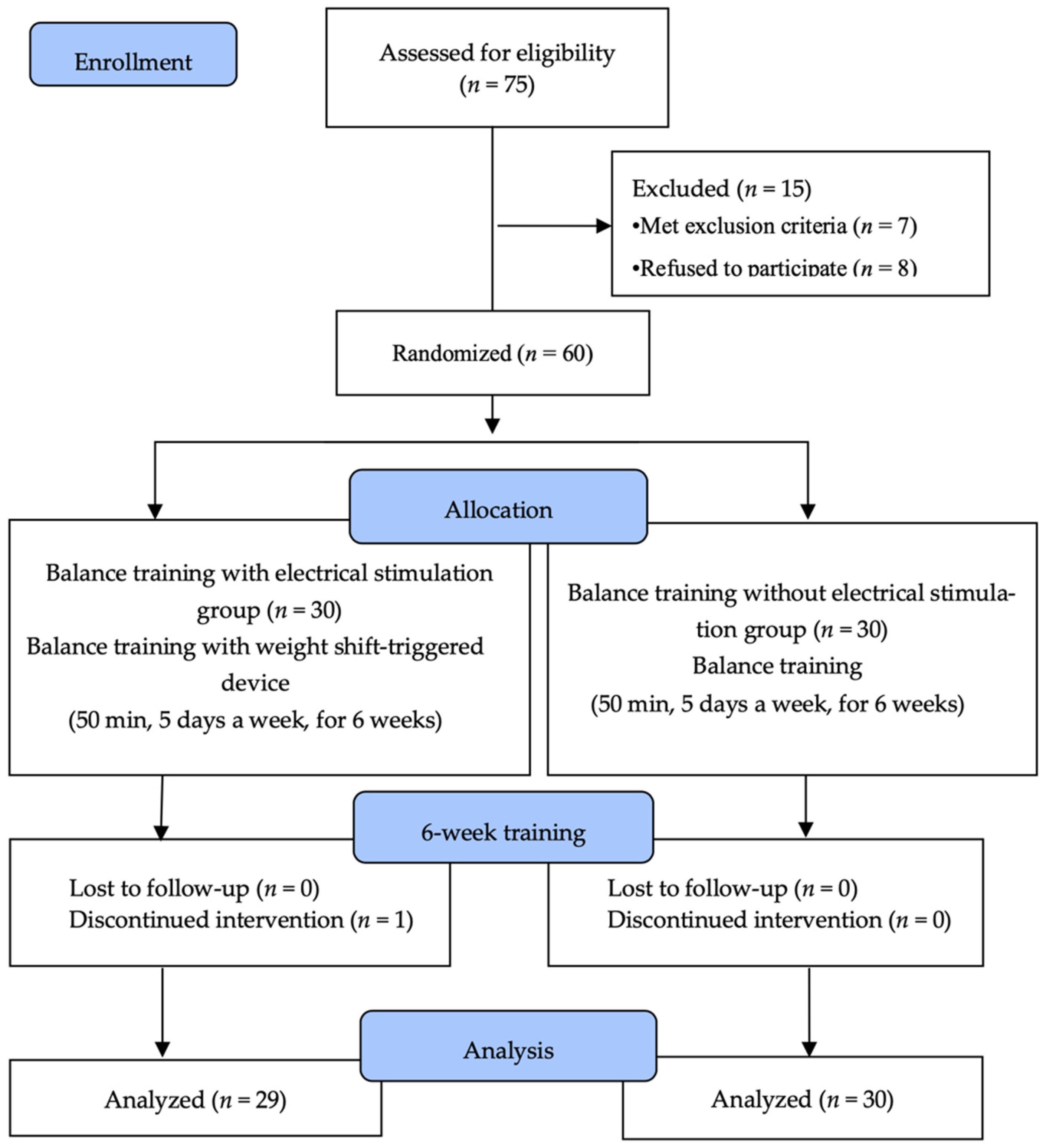
Seventy-five patients were recruited for the study. After receiving an explanation of the study procedure, eight people refused to participate, while another seven were excluded because they did not meet the selection criteria. Sixty subjects were randomly assigned to the balance training with electrical stimulation group (BT-ESG; n = 30) or the balance training group (BTG; n = 30). To minimize selection bias, a computer program called Random allocation software (version 2.0) (M. Saghei, Isfahan, Iran) was used [19], and the ratio of the two groups was 1:1, and the sequence of patients was in the order of patient number.
Subjects in the BT-ESG performed balance training for 50 min 5 times per week for 6 weeks using a weight shift-triggered electrical stimulation device. Subjects in the BTG performed balance training for 50 min 5 times per week for 6 weeks without a weight shift-triggered electrical stimulation device. Pre- and post-tests were conducted to evaluate the effectiveness of training before and after intervention. The primary outcome was static balance and dynamic balance, and lower-extremity motor function and ADL were evaluated as a secondary outcome. All evaluations were performed in triplicate and averaged by three physiotherapists. All tests were performed by raters blinded to the participants’ information. Participants who were unable to continue the program due to changes in their medical condition during the intervention period and those participating in less than 80% of the total program were excluded from the final study. In the BT-ESG, one patient who was transferred to another hospital during the experiment was excluded, while no subjects in the BTG dropped out.
Finally, 29 individuals from the BT-ESG and 30 from the BTG participated. All subjects underwent pre- and post-tests, and data from these tests were statistically analyzed (Figure 1).
Figure 1.
Flow diagram of the study.
2.3. Experimental Method
2.3.1. Weight Shift-Triggered Electrical Stimulation Device
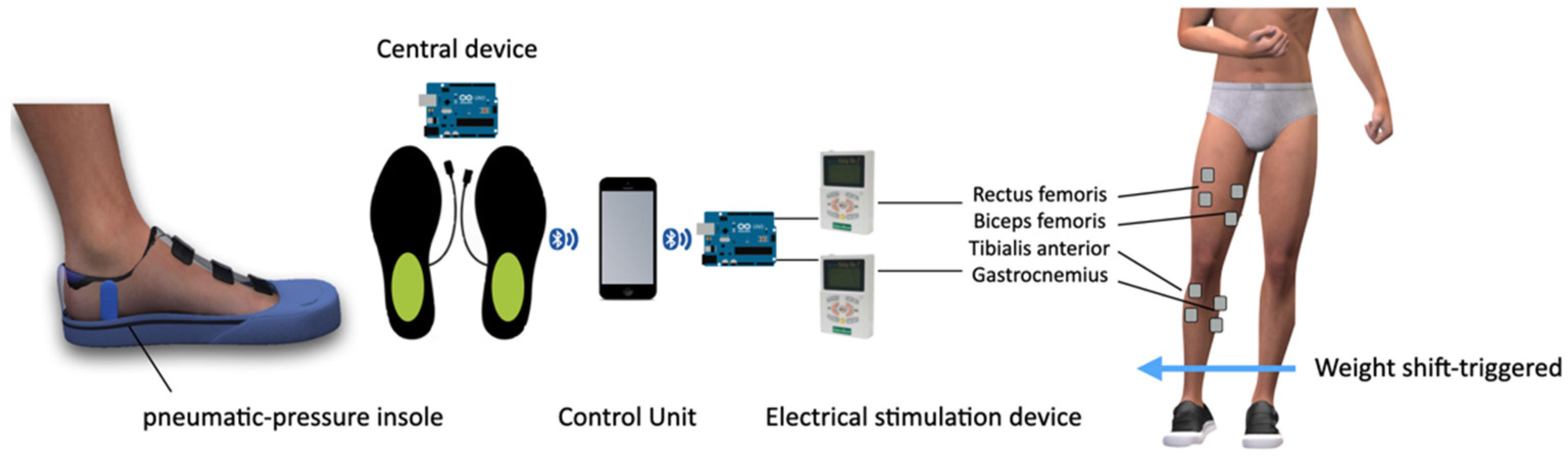
The weight shift-triggered electrical stimulation device triggers a low-frequency output and induces muscle contraction when a decrease in the pressure signal is detected by the insole pressure-measuring device inside the shoe.
We developed an insole-type pressure-measuring device to measure the weight shift in stroke patients. The device measured the air pressure recorded by the weights of both feet. The weight-bearing ratio is calculated by converting the force applied to the affected and unaffected sides from the sum of both feet. The device consisted of an insole with an air tube, a central device, and a control unit. The air insole measures the pressure caused by the air cap inserted into the sole using an air pressure-measuring device. It wirelessly transmits signals to the central device, which sends signals from both feet to the control device. The control device was developed as a smart phone application.
When the patient tried to transfer the weight from the healthy side to the affected side, the weight support rate of the healthy side decreased, and the electric stimulation device operated as a trigger. Two electrical stimulation devices (EMS-1000; Cyber Medic, Iksan, Republic of Korea) with two channels were used. Electrodes were attached to the rectus femoris, biceps femoris, gastrocnemius lateral head, and tibialis anterior muscle bellies, which are important muscles for weight bearing [20,21,22]. Activation was checked every time training was performed, and the position of the electrodes was attached. All electrodes were square hydrogel electrodes (HRTS50AP 50 × 54 mm2; Hurev, Wonju, Republic of Korea). When 90% of the measured value was reached in the insole-type measuring device on the unaffected side, the electrical stimulation device was triggered and the threshold value was adjusted according to individual characteristics. Electrical stimulation was delivered to the muscles through electrodes when the input stimulation reached a threshold. A rectangular two-phase pulse with a pulse width of 300 μs was used. Pulse intensity (mA) was chosen to elicit contraction of the affected limb according to the target intensity (5–60 mA; mean, 16–18 mA). The standard current frequency is 30–35 Hz. Patients were asked to contract lower-extremity muscles when actively supporting weight. The intensity of the electrical stimulation was below the level of inducing muscle contraction. The intensity was adjusted for each patient according to the patient’s muscle contraction ability and sensory state (Figure 2).
Figure 2.
Weight shift-triggered electrical stimulation device.
2.3.2. Balance Training Program
The balance training program was designed to improve weight shift in stroke patients and was based on the exercise programs of previous studies. The total exercise time was 50 min and consisted of 10 min of warm-up, consisting of stretching and a range of motion exercises to relieve spasticity and leg muscle massage, 30 min of main exercise with weight shift as the main exercise, and 10 min of cool-down. The weight shift exercises included the following: (1) sideways weight shift; (2) diagonal forward shift; (3) diagonal back weight shift; (4) weight shift up a short flight of stairs; (5) weight shift down a short flight of stairs; and (6) sideways weight shift on the platform. Each patient’s functional ability was evaluated and the program was configured accordingly.
2.4. Outcome Measurements
2.4.1. Static Balance Ability
A postural assessment system (GB300; Metitur Ltd., Jyvaskyla, Finland) was used to measure static balance ability. The system consisted of a movable triangular platform for feet marked with a ruler on the platform for proper foot positioning. It was used to determine the balance and rehabilitation outcomes and administer the training. This instrument has been widely used to measure balance in adults, the elderly, and stroke patients [23,24,25]. In the test–retest method, the intraclass correlation coefficient (ICC; 0.83) of the measuring instrument exceeded 0.83 [26]. The sampling frequency was 50 Hz. The subject stood still on the equipment with eyes open for 30 s 3 times. The subjects were then measured 3 times while standing forward for 30 s with closed eyes.
2.4.2. Dynamic Balance Ability
The TUG test is used to evaluate the dynamic balance ability of stroke patients. The TUG test is a simple and rapid functional movement test, consisting of standing up, walking 3 m, returning, and sitting back down. It measures the time taken to sit in a chair with armrests and a backrest, stand up, walk 3 m, walk back, and return to sitting in the chair. This test measures the dynamic balance, functional movement, and gait ability of stroke patients with lower-extremity disabilities such as spasticity. It is a highly reliable and valid method for assessing risk (ICC = 0.99) [27]. In this experiment, a chair with a height of 50 cm was used for measurements. The measurements were performed three times using a stopwatch, and the mean value was calculated and recorded.
The FRT was used to evaluate stability limits. During this measurement, the subject stood approximately 10 cm away from the wall, bent their shoulder at 90°, made a fist, and extended their arm forward as far as possible parallel to the floor. The evaluation–revaluation reliability and inter-measurement reliability were high at r = 0.89 and r = 0.98, respectively [28]. In this experiment, three measurements were performed and the mean was recorded.
The BBS is used to measure balance in patients with stroke or older adults. The 14 items were scored on a 5-point scale from 0 to 4 for a total possible score of 56. This tool has high reliability and internal validity for assessing balance ability (r = 0.99 and r = 0.98, respectively) [29].
2.4.3. Lower-Extremity Motor Function
Lower-extremity motor function was assessed in this study using the Fugl–Meyer assessment lower-extremity scale, which assesses functional recovery in patients with stroke. Each item on the test was rated on the following 3-point scale: 0 points for not being able to progress, 1 point for partial task completion, and 2 points for full task completion. The perfect score for lower-limb function was 34 points, and the test items consisted of the hip, knee, ankle, and coordination joints. Moreover, it is possible to evaluate balance, sensation, and pain; however, only lower-extremity function was considered in this study. This test has good inter- (r = 0.94) and intra-rater (r = 0.99) reliabilities [30].
2.4.4. Activities of Daily Living (ADL)
The Modified Barthel Index (MBI) was used to evaluate the subjects’ ADL. The MBI is a scale that can be used to evaluate the level of performance in daily life. It includes the following 10 items: personal hygiene, bathing, feeding, toileting, stair climbing, dressing, bowel control, bladder control, ambulation, wheelchair transfer, and mobility. Each item was scored numerically according to the degree of assistance required by the individual. The maximum score for each figure is 100 points. A score of 0–24 indicates complete dependence, 25–49 indicates severe dependence, 50–74 indicates moderate dependence, and 75–90 indicates little dependence. The inter- (r = 0.99) and intra-rater (r = 0.99) reliabilities were high [31].
2.5. Data Analysis
The Statistical Package for the Social Sciences (SPSS version 19; IBM, Armonk, NY, USA) was used for the statistical analysis. To confirm the assumption of data normality, the Shapiro–Wilk test was used, which confirmed that the assumption of normality was satisfied. Two-way repeated measure ANOVA was used to analyze the main effects of “training type” (BT-ESG or BTG) and “time” on static and dynamic balance and function, and the interaction of treatment type and time was analyzed. Before and after comparisons within groups were analyzed using a paired t-test. Effect sizes were calculated to assess the strength of the training effect, and 95% confidence intervals, which reflect the actual changes in addition to errors, were calculated. The statistical significance level (α) was set at p < 0.05.
3. Results
3.1. General Characteristics of the Subjects
Sixty subjects were enrolled in this study. Of them, one from the BT-ESG dropped out, while all the subjects from the BTG completed the study. A total of 59 subjects completed the study. Before the intervention, the general characteristics of the two groups were homogeneous (Table 1).

Table 1.
General characteristics of the subjects.
3.2. Changes in Static Balance Ability
Changes in static balance ability, medial and lateral sway speed, anterior and posterior sway speed, and velocity of moment variables showed significant improvement after the intervention in both groups, regardless of the eyes-open or eyes-closed state (p < 0.05). However, the BT-ESG showed greater improvement than the BTG (p < 0.05) (Table 2).

Table 2.
Changes in static balance ability.
3.3. Changes in Dynamic Balance Ability
The BT-ESG and BTG showed significant improvements in TUG and BBS scores after training, with significantly better improvements in the former versus latter (p < 0.05) (Table 3).

Table 3.
Changes in dynamic balance ability.
3.4. Changes in Lower-Extremity Motor Function and ADL
Both the BT-ESG and BTG showed significant improvements in the Fugl–Meyer assessment lower-extremity scale and MBI scores after training, with significantly better improvements in the former versus latter (p < 0.05) (Table 4).

Table 4.
Changes in lower-extremity motor function and ADL.
4. Discussion
Electrical stimulation is a harmless method used to enhance the activation of residual muscles. In a study of stroke patients, electrical stimulation was used to recover patients with reduced function or paralysis [9,10]. In this study, it was applied to the four lower-extremity muscles that are necessary for weight support by triggering a weight shift, and muscle contraction was induced at an appropriate time to support weight support. Electrical stimulation induces direct muscle mobilization, unlike visual or auditory feedback [32] used in previous balance training studies. In this study, both groups showed significant improvements in static balance, dynamic balance, lower-extremity motor function, and ADL, and the BT-ESG showed significant improvement versus the BTG.
Maintaining postural balance is a complex task that requires appropriate sensory inputs and motor control [33]. An asymmetrical weight load causes the center of gravity to become unstable, increasing movement variability and making balancing difficult, owing to postural fluctuations. In this study, static balance ability was evaluated using postural sway, while dynamic balance ability was assessed using the TUG, FRT, and BBS. Both groups showed significant improvement, while the BT-ESG showed greater improvement than the BTG.
In this study, postural sway in the BT-ESG improved with a mediolateral speed increase of 28.2%, anterioposterior speed of 21.5%, velocity moment of 34.4% with eyes open and mediolateral speed of 26.2%, anterioposterior speed of 15.2% and velocity moment of 26.5% with eyes closed, while postural sway in the BTG improved with a mediolateral speed increase of 13.6%, anterioposterior speed of 10.9%, velocity moment of 17.8% with eyes open and a mediolateral speed of 11.6%, anterioposterior speed of 8.3% and velocity moment of 12.8% with eyes closed. In this study, postural sway in the BT-ESG showed more remarkable improvement compared to the BTG.
Even when proprioception is normal, postural sway increases more when the eyes are closed versus open [34]. In particular, when proprioception is impaired, such as in stroke patients, postural agitation becomes more severe when the eyes are closed [35]. Lobo et al. [36] showed that weight shift training and proprioceptive training improved the balance ability of stroke patients. Weight-bearing training, which induces a shift in the center of gravity toward the midline, reportedly improves joint stability, postural control, and balance by promoting load receptor feedback to the central nervous system and forcing the paralyzed limb to bear weight [36,37]. Cha et al. [38] reported that weight shift training is an intervention that can improve stroke patients’ proprioceptive and balance abilities. Moreover, applying somatosensory stimulation, such as electrical stimulation and manipulation of the surface beneath the feet to alter the proprioceptive input to the legs, effectively improves the sensory retraining and balance ability of stroke patients [8]. In this study, postural agitation improved more significantly in the BT-ESG than the BTG with electrical stimulation along with balance training, in which an insole-type pressure-measuring device was inserted under the foot of a chronic stroke patient and weight support was induced.
With dynamic balance, the TUG time showed a decrease of 14%. Since the TUG test includes gait, sitting, standing, and turning, balance ability is a predictor of gait [39]. The FRT showed an improvement of 23.6%, confirming improved stability. The BBS showed a 21.5% improvement, confirming that it is an intervention method that can mitigate the risk of falling. In this study, the progress of balance ability is thought to include improved postural symmetry by enhancing lower-limb muscle activation on the affected side and the weight-bearing capacity of the affected side. Previous studies reported that improving muscle tone, joint flexibility, and lower-extremity symmetry on the affected side improved balance ability [40,41,42].
Balance training with weight shift-triggered electrical stimulation was performed in stroke patients with asymmetrical weight-bearing, that is, asymmetrical plantar pressure, improved motor function, stimulated sensory input on the paralyzed leg, and repetitive use of the non-paretic leg. In this balance training program, weight shift-triggered electrical stimulation was provided so that the weight load could be symmetrically induced, while the center of the body moved in various directions in a standing position. Feedback made the subject aware of the incorrect posture, and their balance ability was improved because muscle contraction of the paretic leg was induced.
Alhirsan et al. [43] and Lin et al. [44] reported that repetitive task performance without feedback in stroke patients could continuously increase compensatory actions, create an inappropriate posture, and negatively restore motor function. In this study, the movement of hip extension on the affected side led to the improvement of dynamic balance by promoting weight-bearing and electrical stimulation on the affected side. When severe postural fluctuations occur while maintaining balance, the hip joint strategy is used, and the FRT evaluates the limit of stability while using the hip joint strategy as much as possible [28,45]. Balance training with weight shift-triggered electrical stimulation improved the dynamic balance ability by increasing the weight-bearing rate on the paralyzed side. Moreover, these results were consistent with those of a previous study that reported that dynamic balance was improved through weight shift training for stroke patients and a previous study reported that it was more beneficial to improve balance when combined with electrical stimulation balance training [46]. This finding is consistent with the results reported by Mahmoudi et al. [47].
A significant cause of postural balance problems in stroke patients is an imbalance in lower-extremity function and muscle activity between the affected and unaffected sides. The current study attempted to improve the lower-extremity function of the affected leg through balance training, which induces muscle contraction by triggering electrical stimulation of the affected leg. Since the Fugl–Meyer assessment lower-extremity scale evaluates voluntary movement and active contraction of the leg, it proved the effectiveness of this training for inducing muscle contractions in the affected leg [48]. In this study, the Fugl–Meyer assessment lower-extremity scale showed an improvement of 31.4%, confirming that the lower-extremity function was improved. Previous studies also reported that neuromuscular electrical stimulation and weight shift training reduced muscle tone through muscle activity on the affected side and improved lower-limb functional recovery [49,50]. Balance training with weight shift-triggered electrical stimulation is thought to lead to changes in lower-limb function by promoting the use of the affected side.
As for ADL, both groups showed significant improvement in the MBI score, but a greater improvement was observed in the BT-ESG. In previous studies, balance training seemed to have a positive effect by improving ADL in stroke patients [51]. These results are consistent with previous research results, showing that balance has a high correlation with ADL [52]. In this study, improved weight transfer ability improved balance ability and lower-limb function, which impacted daily life.
In this study, balance training with weight shift-triggered electrical stimulation improved balance ability and lower-extremity function, improving daily life movements. However, since no gait measurement was performed, it is difficult to conclude whether improvements in balance ability, lower-extremity function, and ADL are correlated with gait ability and the risk of falling. In addition, since all the study participants were chronic stroke patients with stroke onset of more than 1 year, the effect of the intervention cannot be generalized to all patients. Further research is needed to address these points.
5. Conclusions
Balance training with weight shift-triggered electrical stimulation, compared with balance training alone, resulted in significant improvements in static balance, dynamic balance, lower-extremity motor function, and ADL in chronic stroke patients. Since the primary outcome of this study used several primary variables for dynamic and static balance, multiplicity adjustment was clearly important. Our findings suggest that balance training with weight shift-triggered electrical stimulation can help to improve the postural symmetry and functional movements of stroke patients.
Funding
This research was supported by Kyungdong University Research Fund, 2022.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Kyungdong University (1041455-202110-HR-012-01).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors gratefully acknowledge the support of the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1F1A1069225).
Conflicts of Interest
The author declares no conflict of interest.
References
- Jonsson, E.; Henriksson, M.; Hirschfeld, H. Age-related differences in postural adjustments in connection with different tasks involving weight transfer while standing. Gait Posture 2007, 26, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Adegoke, B.O.; Olaniyi, O.; Akosile, C.O. Weight bearing asymmetry and functional ambulation performance in stroke survivors. Glob. J. Health Sci. 2012, 4, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Laufer, Y.; Dickstein, R.; Resnik, S.; Marcovitz, E. Weight-bearing shifts of hemiparetic and healthy adults upon stepping on stairs of various heights. Clin. Rehabil. 2000, 14, 125–129. [Google Scholar] [CrossRef]
- Dickstein, R.; Nissan, M.; Pillar, T.; Scheer, D. Foot-ground pressure pattern of standing hemiplegic patients. Major characteristics and patterns of improvement. Phys. Ther. 1984, 64, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, J.; Solzi, P.; Ring, H.; Nisell, R. Postural stability in stroke patients: Vectorial expression of asymmetry, sway activity and relative sequence of reactive forces. Med. Biol. Eng. Comput. 1989, 27, 181–190. [Google Scholar] [CrossRef]
- Eng, J.J.; Chu, K.S. Reliability and comparison of weight-bearing ability during standing tasks for individuals with chronic stroke. Arch. Phys. Med. Rehabil. 2002, 83, 1138–1144. [Google Scholar] [CrossRef]
- Umemura, G.S.; Makhoul, M.P.; Torriani-Pasin, C.; Forner-Cordero, A. Circadian parameter as a possible indicator of gait performance and daily activity levels in chronic stroke survivors. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2022, 2022, 4370–4373. [Google Scholar] [PubMed]
- Aries, A.M.; Downing, P.; Sim, J.; Hunter, S.M. Effectiveness of somatosensory stimulation for the lower limb and foot to improve balance and gait after stroke: A systematic review. Brain Sci. 2022, 12, 1102. [Google Scholar] [CrossRef]
- Knutson, J.S.; Fu, M.J.; Sheffler, L.R.; Chae, J. Neuromuscular electrical stimulation for motor restoration in hemiplegia. Phys. Med. Rehabil. Clin. N. Am. 2015, 26, 729–745. [Google Scholar] [CrossRef]
- Hong, Z.; Sui, M.; Zhuang, Z.; Liu, H.; Zheng, X.; Cai, C.; Jin, D. Effectiveness of neuromuscular electrical stimulation on lower limbs of patients with hemiplegia after chronic stroke: A systematic review. Arch. Phys. Med. Rehabil. 2018, 99, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Riaz, M.T.; AlSanad, A.A.; Ahmad, S.; Akbar, M.A.; AlSuwaidan, L.; Al, A.H.A.; AlSagri, H.S. A wireless controlled intelligent healthcare system for diplegia patients. Math. Biosci. Eng. 2022, 19, 456–472. [Google Scholar] [CrossRef] [PubMed]
- Luque-Moreno, C.; Oliva-Pascual-Vaca, A.; Kiper, P.; Rodriguez-Blanco, C.; Agostini, M.; Turolla, A. Virtual reality to assess and treat lower extremity disorders in post-stroke patients. Methods Inf. Med. 2016, 55, 89–92. [Google Scholar] [PubMed]
- Liu, X.; Zhao, C.; Zheng, B.; Guo, Q.; Duan, X.; Wulamu, A.; Zhang, D. Wearable devices for gait analysis in intelligent healthcare. Front. Comput. Sci. 2021, 3, 661676. [Google Scholar] [CrossRef]
- Bowman, T.; Gervasoni, E.; Arienti, C.; Lazzarini, S.G.; Negrini, S.; Crea, S.; Cattaneo, D.; Carrozza, M.C. Wearable devices for biofeedback rehabilitation: A systematic review and meta-analysis to design application rules and estimate the effectiveness on balance and gait outcomes in neurological diseases. Sensors 2021, 21, 3444. [Google Scholar] [CrossRef] [PubMed]
- De Nunzio, A.; Zucchella, C.; Spicciato, F.; Tortola, P.; Vecchione, C.; Pierelli, F.; Bartolo, M. Biofeedback rehabilitation of posture and weightbearing distribution in stroke: A center of foot pressure analysis. Funct. Neurol. 2014, 29, 127–134. [Google Scholar]
- Stanton, R.; Ada, L.; Dean, C.M.; Preston, E. Biofeedback improves activities of the lower limb after stroke: A systematic review. J. Physiother. 2011, 57, 145–155. [Google Scholar] [CrossRef]
- Delgado-Gonzalo, R.; Hubbard, J.; Renevey, P.; Lemkaddem, A.; Vellinga, Q.; Ashby, D.; Willardson, J.; Bertschi, M. Real-time gait analysis with accelerometer-based smart shoes. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Republic of Korea, 11–15 July 2017. [Google Scholar]
- Kim, S.H.; Huizenga, D.E.; Handzic, I.; Ditwiler, R.E.; Lazinski, M.; Ramakrishnan, T.; Bozeman, A.; Rose, D.Z.; Reed, K.B. Relearning functional and symmetric walking after stroke using a wearable device: A feasibility study. J. Neuroeng. Rehabil. 2019, 16, 106. [Google Scholar] [CrossRef]
- Saghaei, M. Random allocation software for parallel group randomized trials. BMC Med. Res. Methodol. 2004, 4, 26. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M.; Ordway, N.R.; Ploutz-Snyder, L.L. Leg muscle activity during walking with assistive devices at varying levels of weight bearing. Arch. Phys. Med. Rehabil. 2004, 85, 1555–1560. [Google Scholar] [CrossRef]
- Flaxman, T.E.; Speirs, A.D.; Benoit, D.L. Joint stabilisers or moment actuators: The role of knee joint muscles while weight-bearing. J. Biomech. 2012, 45, 2570–2576. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, S.; Shields, R.K. Weight-bearing exercise accuracy influences muscle activation strategies of the knee. J. Neurol. Phys. Ther. 2007, 31, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Lee, K.; Kim, M.; Song, C. Audiovisual biofeedback-based trunk stabilization training using a pressure biofeedback system in stroke patients: A randomized, single-blinded study. Stroke Res. Treat. 2017, 2017, 6190593. [Google Scholar] [CrossRef] [PubMed]
- Maciaszek, J. Effects of posturographic platform biofeedback training on the static and dynamic balance of older stroke patients. J. Stroke Cerebrovasc. Dis. 2018, 27, 1969–1974. [Google Scholar] [CrossRef]
- Maciaszek, J.; Borawska, S.; Wojcikiewicz, J. Influence of posturographic platform biofeedback training on the dynamic balance of adult stroke patients. J. Stroke Cerebrovasc. Dis. 2014, 23, 1269–1274. [Google Scholar] [CrossRef]
- Era, P.; Sainio, P.; Koskinen, S.; Haavisto, P.; Vaara, M.; Aromaa, A. Postural balance in a random sample of 7979 subjects aged 30 years and over. Gerontology 2006, 52, 204–213. [Google Scholar] [CrossRef]
- Ng, S.S.; Hui-Chan, C.W. The timed up & go test: Its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch. Phys. Med. Rehabil. 2005, 86, 1641–1647. [Google Scholar]
- Katz-Leurer, M.; Fisher, I.; Neeb, M.; Schwartz, I.; Carmeli, E. Reliability and validity of the modified functional reach test at the sub-acute stage post-stroke. Disabil. Rehabil. 2009, 31, 243–248. [Google Scholar] [CrossRef]
- Downs, S.; Marquez, J.; Chiarelli, P. The berg balance scale has high intra- and inter-rater reliability but absolute reliability varies across the scale: A systematic review. J. Physiother. 2013, 59, 93–99. [Google Scholar] [CrossRef]
- Duncan, P.W.; Propst, M.; Nelson, S.G. Reliability of the fugl-meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys. Ther. 1983, 63, 1606–1610. [Google Scholar] [CrossRef]
- Ohura, T.; Hase, K.; Nakajima, Y.; Nakayama, T. Validity and reliability of a performance evaluation tool based on the modified barthel index for stroke patients. BMC Med. Res. Methodol. 2017, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- van Vliet, P.M.; Wulf, G. Extrinsic feedback for motor learning after stroke: What is the evidence? Disabil. Rehabil. 2006, 28, 831–840. [Google Scholar] [CrossRef]
- Chastan, N.; Westby, G.W.; du Montcel, S.T.; Do, M.C.; Chong, R.K.; Agid, Y.; Welter, M.L. Influence of sensory inputs and motor demands on the control of the centre of mass velocity during gait initiation in humans. Neurosci. Lett. 2010, 469, 400–404. [Google Scholar] [CrossRef]
- Hansson, E.E.; Beckman, A.; Hakansson, A. Effect of vision, proprioception, and the position of the vestibular organ on postural sway. Acta Otolaryngol. 2010, 130, 1358–1363. [Google Scholar] [CrossRef] [PubMed]
- Marigold, D.S.; Eng, J.J. The relationship of asymmetric weight-bearing with postural sway and visual reliance in stroke. Gait Posture 2006, 23, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.A.; Joshua, A.M.; Nayak, A.; Mithra, P.P.; Misri, Z.; Pai, S. Effect of compelled body weight shift (cbws) therapy in comparison to proprioceptivetraining on functional balance, gait, andmuscle strength among acute stroke subjects. Ann. Neurosci. 2021, 28, 162–169. [Google Scholar] [CrossRef]
- Lobo, A.A.; Joshua, A.M.; Nayak, A. Effects of compelled body weight shift therapy on weight-bearing symmetry, balance and gait in patients with stroke: A narrative review. Crit. Rev.™ Phys. Rehabil. Med. 2021, 33, 45–64. [Google Scholar] [CrossRef]
- Cha, J.H.; Kim, N.H.; Cha, Y.J. Effect of proprioceptive stimulation induced by footplate during center of pressure movement tracking training on the balance abilities of patients with chronic hemiplegic stroke: A randomized, controlled, pilot study. Top. Stroke Rehabil. 2020, 27, 38–43. [Google Scholar] [CrossRef]
- Wrisley, D.M.; Kumar, N.A. Functional gait assessment: Concurrent, discriminative, and predictive validity in community-dwelling older adults. Phys. Ther. 2010, 90, 761–773. [Google Scholar] [CrossRef]
- Suputtitada, A.; Yooktanan, P.; Rarerng-Ying, T. Effect of partial body weight support treadmill training in chronic stroke patients. J. Med. Assoc.Thai. 2004, 87 (Suppl. S2), S107–S111. [Google Scholar]
- Ivey, F.M.; Hafer-Macko, C.E.; Macko, R.F. Task-oriented treadmill exercise training in chronic hemiparetic stroke. J. Rehabil. Res. Dev. 2008, 45, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, B.; Parvataneni, K.; Olney, S.J. A comparison of gait biomechanics and metabolic requirements of overground and treadmill walking in people with stroke. Clin. Biomech. 2009, 24, 729–734. [Google Scholar] [CrossRef]
- Alhirsan, S.M.; Capo-Lugo, C.E.; Brown, D.A. Effects of different types of augmented feedback on intrinsic motivation and walking speed performance in post-stroke: A study protocol. Contemp. Clin. Trials Commun. 2021, 24, 100863. [Google Scholar] [CrossRef]
- Lin, S.; Mann, J.; Mansfield, A.; Wang, R.H.; Harris, J.E.; Taati, B. Investigating the feasibility and acceptability of real-time visual feedback in reducing compensatory motions during self-administered stroke rehabilitation exercises: A pilot study with chronic stroke survivors. J. Rehabil. Assist. Technol. Eng. 2019, 6, 2055668319831631. [Google Scholar] [CrossRef] [PubMed]
- Ray, C.T.; Horvat, M.; Croce, R.; Mason, R.C.; Wolf, S.L. The impact of vision loss on postural stability and balance strategies in individuals with profound vision loss. Gait Posture 2008, 28, 58–61. [Google Scholar] [CrossRef]
- Tsaklis, P.V.; Grooten, W.J.; Franzen, E. Effects of weight-shift training on balance control and weight distribution in chronic stroke: A pilot study. Top. Stroke Rehabil. 2012, 19, 23–31. [Google Scholar] [CrossRef]
- Mahmoudi, Z.; Mohammadi, R.; Sadeghi, T.; Kalbasi, G. The effects of electrical stimulation of lower extremity muscles on balance in stroke patients: A systematic review of literatures. J. Stroke Cerebrovasc. Dis. 2021, 30, 105793. [Google Scholar] [CrossRef] [PubMed]
- Satjanitikun, A.; Pichaiyongwongdee, S.; Jalayondeja, C. Correlation between weight transfer on paretic limb while standing in three directions and fugl-meyer assessment for lower extremities in individuals with stroke. J. Med. Assoc. Thai. 2015, 98 (Suppl. S5), S1–S5. [Google Scholar] [PubMed]
- Knutson, J.S.; Hansen, K.; Nagy, J.; Bailey, S.N.; Gunzler, D.D.; Sheffler, L.R.; Chae, J. Contralaterally controlled neuromuscular electrical stimulation for recovery of ankle dorsiflexion: A pilot randomized controlled trial in patients with chronic post-stroke hemiplegia. Am. J. Phys. Med. Rehabil. 2013, 92, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Mohapatra, S.; Eviota, A.C.; Ringquist, K.L.; Muthukrishnan, S.R.; Aruin, A.S. Compelled body weight shift technique to facilitate rehabilitation of individuals with acute stroke. ISRN Rehabil. 2012, 2012, 328018. [Google Scholar] [CrossRef]
- Aphiphaksakul, P.; Siriphorn, A. Home-based exercise using balance disc and smartphone inclinometer application improves balance and activity of daily living in individuals with stroke: A randomized controlled trial. PLoS ONE 2022, 17, e0277870. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, M.M.; Meyer, S.; Sandstad, S.; Wiskerke, E.; Thuwis, R.; Vandekerckhove, C.; Myny, C.; Ghosh, N.; Beyens, H.; Dejaeger, E.; et al. A cross-sectional study comparing lateral and diagonal maximum weight shift in people with stroke and healthy controls and the correlation with balance, gait and fear of falling. PLoS ONE 2017, 12, e0183020. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).