Endoscopic Ipsilateral Interhemispheric Approach for Middle-Third Falcine Meningioma: A Case Report and Literature Review
Abstract
:1. Introduction
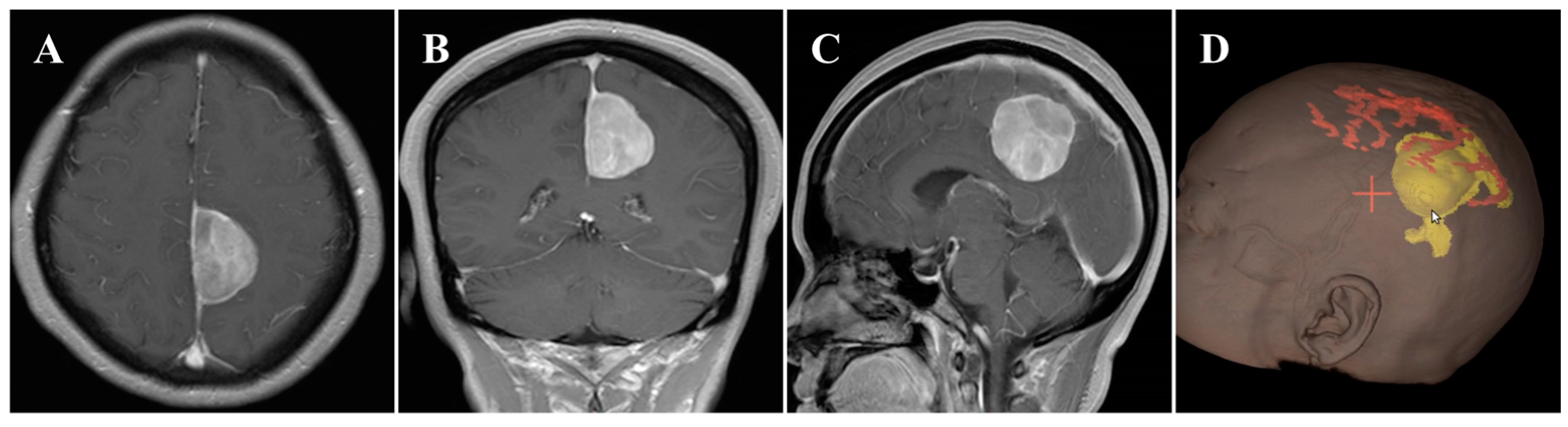
2. Case Description
2.1. History and Examination
2.2. Surgical Treatment
2.3. Postoperative Course
2.4. Literature Review
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mooney, M.A.; Abolfotoh, M.; Bi, W.L.; Tavanaiepour, D.; Almefty, R.O.; Bassiouni, H.; Pravdenkova, S.; Dunn, I.F.; Al-Mefty, O. Is falcine meningioma a diffuse disease of the falx? case series and analysis of a “Grade Zero” resection. Neurosurgery 2020, 87, 900–909. [Google Scholar] [CrossRef] [PubMed]
- Karthigeyan, M.; Rajasekhar, R.; Salunke, P.; Singh, A. Modified unilateral approach for mid-third giant bifalcine meningiomas: Resection using an oblique surgical trajectory and falx window. Acta Neurochir. 2019, 161, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Yang, Z.; You, H.; Song, J. How I do it: The surgical resection of a middle third parasagittal meningioma with venous preservation strategy. Acta Neurochir. 2022, 164, 1385–1389. [Google Scholar] [CrossRef]
- Yamashiro, K.; Muto, J.; Wakako, A.; Murayama, K.; Kojima, D.; Omi, T.; Adachi, K.; Hasegawa, M.; Hirose, Y. Diploic veins as collateral venous pathways in patients with dural venous sinus invasion by meningiomas. Acta Neurochir. 2021, 163, 1687–1696. [Google Scholar] [CrossRef]
- Eichberg, D.G.; Casabella, A.M.; Menaker, S.A.; Shah, A.H.; Komotar, R.J. Parasagittal and parafalcine meningiomas: Integral strategy for optimizing safety and retrospective review of a single surgeon series. Br. J. Neurosurg. 2020, 34, 559–564. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Wang, X.; Zhang, X.; Quan, K.; Hua, W.; Yang, Z.; Li, P.; Liu, P.; Song, J.; Zhu, W. Gravity-assisted ipsilateral paramedian approach for parafalcine meningioma resection. World Neurosurg. 2020, 135, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, M.Y.; Qian, K.; Chen, L.; Zhang, F.C. Classification and protection of peritumoral draining veins of parasagittal and falcine meningiomas. World Neurosurg. 2018, 117, e362–e370. [Google Scholar] [CrossRef]
- Schwartz, T.H.; Morgenstern, P.F.; Anand, V.K. Lessons learned in the evolution of endoscopic skull base surgery. J. Neurosurg. 2019, 130, 337–346. [Google Scholar] [CrossRef] [Green Version]
- Khan, D.Z.; Muskens, I.S.; Mekary, R.A.; Zamanipoor Najafabadi, A.H.; Helmy, A.E.; Reisch, R.; Broekman, M.L.D.; Marcus, H.J. The endoscope-assisted supraorbital “keyhole” approach for anterior skull base meningiomas: An updated meta-analysis. Acta Neurochir. 2021, 163, 661–676. [Google Scholar] [CrossRef]
- Spektor, S.; Margolin, E.; Eliashar, R.; Moscovici, S. Purely endoscopic removal of a parasagittal/falx meningioma. Acta Neurochir. 2016, 158, 451–456. [Google Scholar] [CrossRef]
- Roser, F.; Rigante, L. The endoscope-assisted contralateral paramedian approach to large falcine meningiomas. Acta Neurochir. 2018, 160, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Sakaeyama, Y.; Morisako, H.; Ohata, H.; Nakajo, K.; Valenzuela, J.C.; Fernandez-Miranda, J.C.; Goto, T. Endoscopic contralateral interhemispheric transfalcine keyhole approach for large falcine meningiomas. World Neurosurg. 2022, 166, e237–e244. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Gong, S.; Lee, I.T.; Yang, Y. Microsurgical treatment of parafalcine meningiomas: A retrospective study of 126 cases. Oncol. Targets Ther. 2018, 11, 5279–5285. [Google Scholar] [CrossRef] [Green Version]
- Tsutsumi, S.; Ono, H.; Ishii, H. Cortical and bridging veins of the upper cerebral convexity: A magnetic resonance imaging study. Surg. Radiol. Anat. 2021, 43, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Munich, S.A.; Eddelman, D.; Byrne, R.W. Retrospective review of a venous sparing approach to resection of parasagittal meningiomas. J. Clin. Neurosci. 2019, 64, 194–200. [Google Scholar] [CrossRef]
- Mukherjee, S.; Minhas, P.S. Contralateral approach to resection of a parafalcine meningioma—A technical note. Br. J. Neurosurg. 2014, 28, 699–700. [Google Scholar] [CrossRef]
- Hendricks, B.K.; Spetzler, R.F. Contralateral interhemispheric approach for resection of a meningioma: 2-dimensional operative video. Oper. Neurosurg. 2020, 18, E159. [Google Scholar] [CrossRef] [Green Version]
- Baussart, B.; Vanden Bulcke, D.; Villa, C.; Reina, V.; Gaillard, S. The dural dark-side approach for falcine and tentorial meningioma: A surgical series of five patients. Neurochirurgie 2022, 68, 29–35. [Google Scholar] [CrossRef]
- Tsutsumi, S.; Ono, H.; Yasumoto, Y.; Ishii, H. Venous channels of the falx cerebri in adult Japanese population: Delineation using magnetic resonance imaging. Surg. Radiol. Anat. 2019, 41, 203–207. [Google Scholar] [CrossRef]
- Tatarli, N.; Ceylan, D.; Canaz, H.; Tokmak, M.; Bay, H.H.; Şeker, A.; Keleş, E.; Kiliç, T.; Cavdar, S. Falcine venous plexus within the falx cerebri: Anatomical and scanning electron microscopic findings and clinical significance. Acta Neurochir. 2013, 155, 2183–2189, discussion 2189. [Google Scholar] [CrossRef]
- Voß, K.M.; Spille, D.C.; Sauerland, C.; Suero Molina, E.; Brokinkel, C.; Paulus, W.; Stummer, W.; Holling, M.; Jeibmann, A.; Brokinkel, B. The Simpson grading in meningioma surgery: Does the tumor location influence the prognostic value? J. Neurooncol. 2017, 133, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, A.E.; Khalafallah, A.M.; Huq, S.; Horowitz, M.A.; Azmeh, O.; Lam, S.; Oliveira, L.A.P.; Brem, H.; Mukherjee, D. Predictors of nonroutine discharge disposition among patients with Parasagittal/Parafalcine meningioma. World Neurosurg. 2020, 142, e344–e349. [Google Scholar] [CrossRef] [PubMed]
- Chotai, S.; Schwartz, T.H. The simpson grading: Is it still valid? Cancers 2022, 14, 2007. [Google Scholar] [CrossRef] [PubMed]



| Author/Year | Sample Size | Tumor Location | Surgical Approach | Extent of Resection |
|---|---|---|---|---|
| Spektor S et al. [10] 2016 | 1 | Ant | Oblique surgical trajectory | STR; SG I |
| Roser F et al. [11] 2018 | 1 | Ant | Contralateral interhemispheric approach | GTR; SG I |
| Sakaeyama Y et al. [12] 2022 | 4 | Ant 2; Mid 1; Post 1 | Contralateral interhemispheric approach | GTR; SG I |
| Zhang G et al. (present study) | 1 | Mid | Ipsilateral interhemispheric approach | GTR; SG II |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, G.; Wang, J.; Wang, P.; Wu, N. Endoscopic Ipsilateral Interhemispheric Approach for Middle-Third Falcine Meningioma: A Case Report and Literature Review. Brain Sci. 2023, 13, 1085. https://doi.org/10.3390/brainsci13071085
Zhang G, Wang J, Wang P, Wu N. Endoscopic Ipsilateral Interhemispheric Approach for Middle-Third Falcine Meningioma: A Case Report and Literature Review. Brain Sciences. 2023; 13(7):1085. https://doi.org/10.3390/brainsci13071085
Chicago/Turabian StyleZhang, Gang, Junwei Wang, Pan Wang, and Nan Wu. 2023. "Endoscopic Ipsilateral Interhemispheric Approach for Middle-Third Falcine Meningioma: A Case Report and Literature Review" Brain Sciences 13, no. 7: 1085. https://doi.org/10.3390/brainsci13071085
APA StyleZhang, G., Wang, J., Wang, P., & Wu, N. (2023). Endoscopic Ipsilateral Interhemispheric Approach for Middle-Third Falcine Meningioma: A Case Report and Literature Review. Brain Sciences, 13(7), 1085. https://doi.org/10.3390/brainsci13071085







