Predicted Brain Age in First-Episode Psychosis: Association with Inexpressivity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. MRI Acquisition
2.3. Data Availability
2.4. Brain Age Estimation
2.5. Statistical Analysis
3. Results
3.1. Demographics, Neuropsychological, and Social Functioning
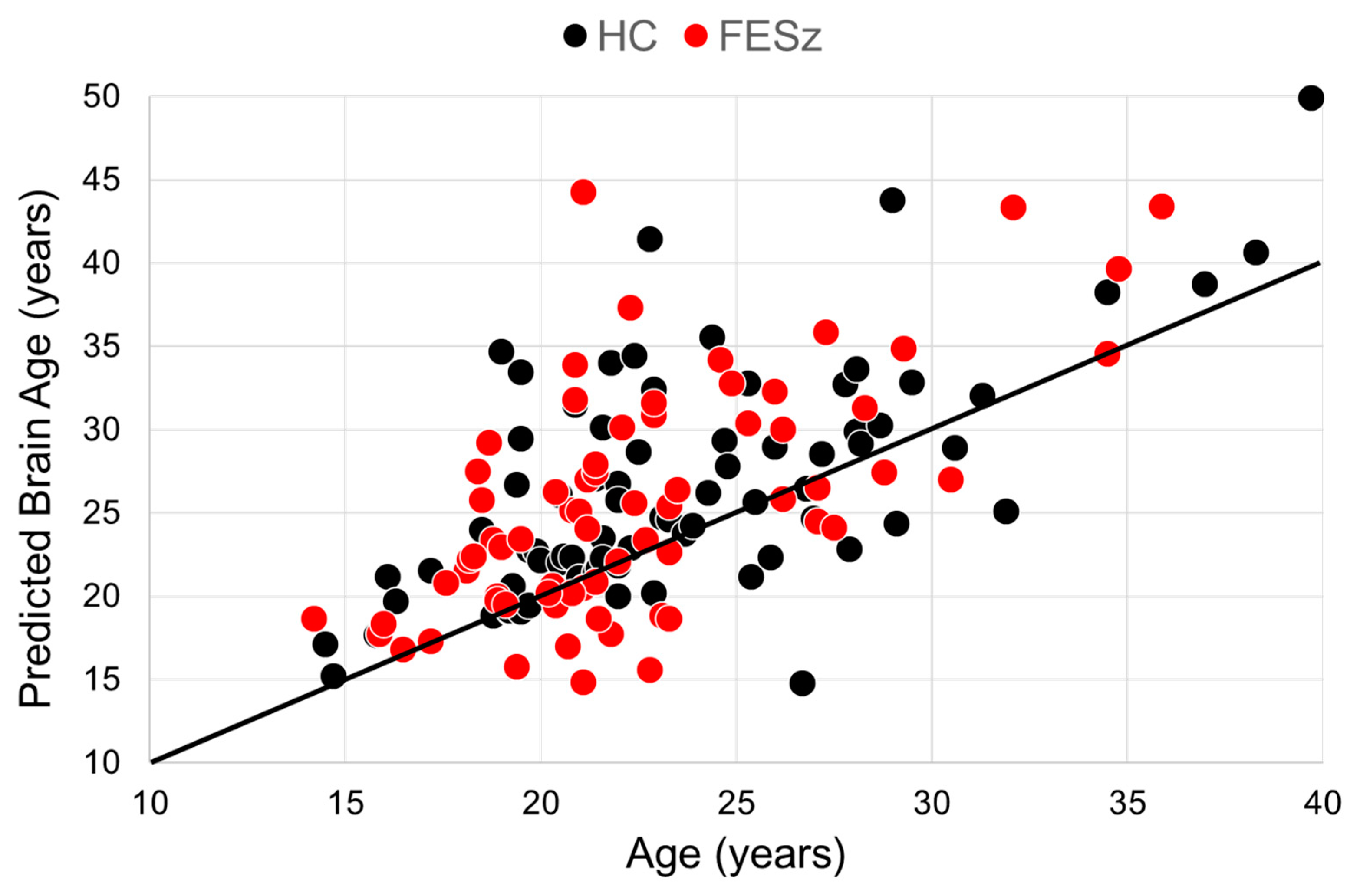
3.2. Predicted Brain Age and Brain Age Gap
3.2.1. Regression Analyses
3.2.2. Neuropsychological Performance
3.2.3. Social Functioning
3.2.4. Symptoms
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kraepelin, E. Psychiatrie: Ein Lehrbuch fur Studirende und Aerzte; Verlag Von Johann Ambrosius Barth: Leipzig, Germany, 1899. [Google Scholar]
- Bleuler, E. Dementia Praecox, or the Group of Schizophrenias; Zinkin, J., Translator; International Universities Press: New York, NY, USA, 1911. [Google Scholar]
- Kendler, K.S.; Tabb, K.; Wright, J. The emergence of psychiatry: 1650–1850. Am. J. Psychiatry 2022, 179, 329–335. [Google Scholar] [CrossRef]
- Moore, M.T.; Nathan, D.; Elliott, A.R.; Laubach, C. Encephhalographic studies in schizophrenia (dementia praecox): Report of Sixty Cases. Am. J. Psychiatry 1933, 89, 801–810. [Google Scholar] [CrossRef]
- Weinberger, D.R. Implications of normal brain development for the pathogenesis of schizophrenia. Arch. Gen. Psychiatry 1987, 44, 660–669. [Google Scholar] [CrossRef]
- Lipska, B.K. Using animal models to test a neurodevelopmental hypothesis of schizophrenia. J. Psychiatry Neurosci. 2004, 29, 282–286. [Google Scholar]
- Benes, F.M. Evidence for neurodevelopment disturbances in anterior cingulate cortex of post-mortem schizophrenic brain. Schizophr. Res. 1991, 5, 187–188. [Google Scholar] [CrossRef]
- Feinberg, I. Schizophrenia: Caused by a fault in programmed synaptic elimination during adolescence? J. Psychiatr. Res. 1982, 17, 319–334. [Google Scholar] [CrossRef]
- McGlashan, T.H.; Hoffman, R.E. Schizophrenia as a disorder of developmentally reduced synaptic connectivity. Arch. Gen. Psychiatry 2000, 57, 637–648. [Google Scholar] [CrossRef]
- Waddington, J.L.; Scully, P.J.; Youssef, H.A. Developmental trajectory and disease progression in schizophrenia: The conundrum, and insights from a 12-year prospective study in the Monaghan 101. Schizophr. Res. 1997, 23, 107–118. [Google Scholar] [CrossRef]
- Gur, R.E.; Cowell, P.; Turetsky, B.I.; Gallacher, F.; Cannon, T.; Bilker, W.; Gur, R.C. A follow-up magnetic resonance imaging study of schizophrenia: Relationship of neuroanatomical changes to clinical and neurobehavioral measures. Arch. Gen. Psychiatry 1998, 55, 145–152. [Google Scholar] [CrossRef]
- Thompson, P.M.; Vidal, C.; Giedd, J.N.; Gochman, P.; Blumenthal, J.; Nicolson, R.; Toga, A.W.; Rapoport, J.L. Mapping adolescent brain change reveals dynamic wave of accelerated gray matter loss in very early-onset schizophrenia. Proc. Natl. Acad. Sci. USA 2001, 98, 11650–11655. [Google Scholar] [CrossRef]
- Lieberman, J.; Chakos, M.; Wu, H.; Alvir, J.; Hoffman, E.; Robinson, D.; Bilder, R. Longitudinal study of brain morphology in first episode schizophrenia. Biol. Psychiatry 2001, 49, 487–499. [Google Scholar] [CrossRef]
- Cahn, W.; Pol, H.E.H.; Lems, E.B.; van Haren, N.E.; Schnack, H.G.; van der Linden, J.A.; Schothorst, P.F.; van Engeland, H.; Kahn, R.S. Brain volume changes in first-episode schizophrenia: A 1-year follow-up study. Arch. Gen. Psychiatry 2002, 59, 1002–1010. [Google Scholar] [CrossRef]
- Kasai, K.; Shenton, M.E.; Salisbury, D.F.; Hirayasu, Y.; Lee, C.U.; Ciszewski, A.A.; Yurgelun-Todd, D.; Kikinis, R.; Jolesz, F.A.; McCarley, R.W. Progressive decrease of left superior temporal gyrus gray matter volume in patients with first-episode schizophrenia. Am. J. Psychiatry 2003, 160, 156–164. [Google Scholar] [CrossRef]
- Kasai, K.; Shenton, M.E.; Salisbury, D.F.; Hirayasu, Y.; Onitsuka, T.; Spencer, M.H.; Yurgelun-Todd, D.A.; Kikinis, R.; Jolesz, F.A.; McCarley, R.W. Progressive decrease of left Heschl gyrus and planum temporale gray matter volume in first-episode schizophrenia: A longitudinal magnetic resonance imaging study. Arch. Gen. Psychiatry 2003, 60, 766–775. [Google Scholar] [CrossRef]
- Ho, B.C.; Andreasen, N.C.; Nopoulos, P.; Arndt, S.; Magnotta, V.; Flaum, M. Progressive structural brain abnormalities and their relationship to clinical outcome: A longitudinal magnetic resonance imaging study early in schizophrenia. Arch. Gen. Psychiatry 2003, 60, 585–594. [Google Scholar] [CrossRef]
- Bachmann, S.; Bottmer, C.; Pantel, J.; Schröder, J.; Amann, M.; Schad, M.E.L.R. MRI-morphometric changes in first-episode schizophrenic patients at 14 months follow-up. Schizophr. Res. 2004, 67, 301–303. [Google Scholar] [CrossRef]
- Pantelis, C.; Velakoulis, D.; McGorry, P.D.; Wood, S.J.; Suckling, J.; Phillips, L.J.; Yung, A.R.; Bullmore, E.T.; Brewer, W.; Soulsby, B.; et al. Neuroanatomical abnormalities before and after onset of psychosis: A cross-sectional and longitudinal MRI comparison. Lancet 2003, 361, 281–288. [Google Scholar] [CrossRef]
- Job, D.E.; Whalley, H.C.; Johnstone, E.C.; Lawrie, S.M. Grey matter changes over time in high risk subjects developing schizophrenia. Neuroimage 2005, 25, 1023–1030. [Google Scholar] [CrossRef]
- Olney, J.W. Excitotoxic amino acids and neuropsychiatric disorders. Annu. Rev. Pharmacol. Toxicol. 1990, 30, 47–71. [Google Scholar] [CrossRef]
- Okusaga, O.O. Accelerated aging in schizophrenia patients: The potential role of oxidative stress. Aging Dis. 2014, 5, 256–262. [Google Scholar] [CrossRef]
- Kirkpatrick, B.; Messias, E.; Harvey, P.D.; Fernandez-Egea, E.; Bowie, C.R. Is schizophrenia a syndrome of accelerated aging? Schizophr. Bull. 2008, 34, 1024–1032. [Google Scholar] [CrossRef]
- Harvey, P.D.; Rosenthal, J.B. Cognitive and functional deficits in people with schizophrenia: Evidence for accelerated or exaggerated aging? Schizophr. Res. 2018, 196, 14–21. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Eyler, L.T.; Jeste, D.V. Systemic biomarkers of accelerated aging in schizophrenia: A critical review and future directions. Schizophr. Bull. 2018, 44, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Ballester, P.L.; Romano, M.T.; de Azevedo Cardoso, T.; Hassel, S.; Strother, S.C.; Kennedy, S.H.; Frey, B.N. Brain age in mood and psychotic disorders: A systematic review and meta-analysis. Acta Psychiatr. Scand. 2022, 145, 42–55. [Google Scholar] [CrossRef]
- Shahab, S.; Mulsant, B.H.; Levesque, M.L.; Calarco, N.; Nazeri, A.; Wheeler, A.L.; Foussias, G.; Rajji, T.K.; Voineskos, A.N. Brain structure, cognition, and brain age in schizophrenia, bipolar disorder, and healthy controls. Neuropsychopharmacology 2019, 44, 898–906. [Google Scholar] [CrossRef]
- Schnack, H.G.; Van Haren, N.E.; Nieuwenhuis, M.; Hulshoff Pol, H.E.; Cahn, W.; Kahn, R.S. Accelerated brain aging in schizophrenia: A longitudinal pattern recognition study. Am. J. Psychiatry 2016, 173, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Constantinides, C.; Han, L.K.; Alloza, C.; Antonucci, L.A.; Arango, C.; Ayesa-Arriola, R.; Banaj, N.; Bertolino, A.; Borgwardt, S.; Bruggemann, J.; et al. Brain ageing in schizophrenia: Evidence from 26 international cohorts via the ENIGMA Schizophrenia consortium. Mol. Psychiatry 2023, 28, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, T.; van der Meer, D.; Doan, N.T.; Schwarz, E.; Lund, M.J.; Agartz, I.; Alnæs, D.; Barch, D.M.; Baur-Streubel, R.; Bertolino, A.; et al. Common brain disorders are associated with heritable patterns of apparent aging of the brain. Nat. Neurosci. 2019, 22, 1617–1623. [Google Scholar] [CrossRef]
- Hajek, T.; Franke, K.; Kolenic, M.; Capkova, J.; Matejka, M.; Propper, L.; Uher, R.; Stopkova, P.; Novak, T.; Paus, T.; et al. Brain age in early stages of bipolar disorders or schizophrenia. Schizophr. Bull. 2019, 45, 190–198. [Google Scholar] [CrossRef]
- Chung, Y.; Addington, J.; Bearden, C.E.; Cadenhead, K.; Cornblatt, B.; Mathalon, D.H.; McGlashan, T.; Perkins, D.; Seidman, L.J.; Tsuang, M.; et al. Use of machine learning to determine deviance in neuroanatomical maturity associated with future psychosis in youths at clinically high risk. JAMA Psychiatry 2018, 75, 960–968. [Google Scholar] [CrossRef]
- Butler, E.R.; Chen, A.; Ramadan, R.; Le, T.T.; Ruparel, K.; Moore, T.M.; Satterthwaite, T.D.; Zhang, F.; Shou, H.; Gur, R.C.; et al. Pitfalls in brain age analyses. Hum. Brain Mapp. 2021, 42, 4092–4101. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, D. Wechsler Abbreviated Scale of Intelligence (WASI); APA: Washington, DC, USA, 1999. [Google Scholar]
- First, M.B.; Gibbon, M. The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In Comprehensive Handbook of Psychological Assessment, Vol. 2. Personality Assessment; Hilsenroth, M.J., Segal, D.L., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004. [Google Scholar]
- Overall, J.E.; Gorham, D.R. The Brief Psychiatric Rating Scale. Psychol. Rep. 1962, 10, 799–812. [Google Scholar] [CrossRef]
- Andreasen, N.C. Scale for the Assessment of Negative Symptoms (SANS); The University of Iowa: Iowa City, IA, USA, 1981. [Google Scholar]
- Andreasen, N.C. The Scale for the Assessment of Positive Symptoms (SAPS); The University of Iowa: Iowa City, IA, USA, 1984. [Google Scholar]
- Longenecker, J.M.; Haas, G.L.; Salisbury, D.F. Hierarchical symptom components in early psychosis. Schizophr. Bull. 2022, 48, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Nuechterlein, K.H.; Green, M.F.; Kern, R.S.; Baade, L.E.; Barch, D.M.; Cohen, J.D.; Essock, S.; Fenton, W.S.; Frese, F.J., III; Gold, J.M.; et al. The MATRICS Consensus Cognitive Battery, part 1: Test selection, reliability, and validity. Am. J. Psychiatry 2008, 165, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Cornblatt, B.A.; Auther, A.M.; Niendam, T.; Smith, C.W.; Zinberg, J.; Bearden, C.E.; Cannon, T.D. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr. Bull. 2007, 33, 688–702. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.H.; Ritchie, S.J.; Bastin, M.E.; Hernández, V.; Muñoz Maniega, S.; Royle, N.; Corley, J.; Pattie, A.; Harris, S.E.; Zhang, Q.; et al. Brain age predicts mortality. Mol. Psychiatry 2018, 23, 1385–1392. [Google Scholar] [CrossRef] [PubMed]
- Bashyam, V.M.; Erus, G.; Doshi, J.; Habes, M.; Nasrallah, I.M.; Truelove-Hill, M.; Srinivasan, D.; Mamourian, L.; Pomponio, R.; Fan, Y.; et al. MRI signatures of brain age and disease over the lifespan based on a deep brain network and 14 468 individuals worldwide. Brain 2020, 143, 2312–2324. [Google Scholar] [CrossRef]
- Bethlehem, R.A.I.; Seidlitz, J.; White, S.R.; Vogel, J.W.; Anderson, K.M.; Adamson, C.; Adler, S.; Alexopoulos, G.S.; Anagnostou, E.; Areces-Gonzalez, A.; et al. Brain charts for the human lifespan. Nature 2022, 604, 525–533. [Google Scholar] [CrossRef]

| FESz | HC | Cohen’s | |||
|---|---|---|---|---|---|
| (N = 70) | (N = 76) | Statistic * | p-Value | d | |
| Age | 22.5 (4.5) | 23.6 (5.1) | t144 = 1.37 | 0.172 | 0.227 |
| PBA | 25.6 (7.0) | 26.5 (6.8) | t144 = 0.84 | 0.201 | 0.139 |
| BAG | 3.1 (5.3) | 3.0 (5.2) | t144 = 0.16 | 0.877 | 0.026 |
| Sex (F/M) | 18/52 | 29/47 | X2 = 2.59 | 0.108 | |
| pSES | 41.0 (13.8) | 47.7 (11.6) | t144 = 3.19 | 0.002 | 0.532 |
| WASI vocabulary | 51.1 (9.7) | 51.6 (6.5) | t144 = 0.34 | 0.738 | 0.055 |
| WASI matrix reasoning | 52.3 (8.7) | 58.5 (5.7) | t144 = 4.58 | <0.001 | 0.759 |
| MATRICS TMT | 40.0 (13.0) | 48.4 (9.9) | t142 = 4.41 | <0.001 | 0.735 |
| MATRICS processing speed | 39.2 (14.0) | 52.4 (8.4) | t142 = 6.91 | <0.001 | 1.153 |
| MATRICS attention | 36.4 (13.5) | 47.8 (8.9) | t142 = 6.00 | <0.001 | 1.00 |
| MATRICS working memory | 39.4 (13.5) | 48.6 (8.7) | t142 = 4.94 | <0.001 | 0.825 |
| MATRICS verbal learning | 43.6 (11.2) | 52.7 (9.2) | t142 = 5.37 | <0.001 | 0.897 |
| MATRICS visual learning | 39.7 (12.7) | 46.1 (7.7) | t142 = 3.71 | <0.001 | 0.619 |
| MATRICS reasoning | 44.2 (11.5) | 51.2 (7.2) | t142 = 4.47 | <0.001 | 0.745 |
| MATRICS social cognition | 41.6 (14.1) | 54.5 (8.4) | t142 = 6.72 | <0.001 | 1.125 |
| MATRICS composite | 34.9 (15.6) | 50.6 (7.1) | t142 = 7.90 | <0.001 | 1.323 |
| SFS Engagement/Withdrawal | 102.5 (11.8) | 110.7 (10.4) | t142 = 4.42 | <0.001 | 0.737 |
| SFS Interpersonal Interaction | 118.2 (18.5) | 141.8 (8.0) | t142 = 10.03 | <0.001 | 1.674 |
| SFS Recreation | 110.0 (13.4) | 112.7 (9.7) | t142 = 1.38 | 0.170 | 0.231 |
| SFS Employment | 115.5 (7.7) | 120.9 (4.3) | t142 = 5.21 | <0.001 | 0.870 |
| SFS Independence Performance | 100.3 (11.5) | 106.7 (9.0) | t142 = 3.74 | <0.001 | 0.624 |
| SFS Independence Competence | 112.3 (11.8) | 120.0 (7.1) | t142 = 4.82 | <0.001 | 0.803 |
| SFS Prosocial | 108.4 (12.6) | 112.1 (9.3) | t142 = 2.01 | 0.046 | 0.335 |
| GF:R current | 5.5 (2.2) | 9.0 (0.1) | t144 = 13.50 | <0.001 | 2.237 |
| GF:R lowest in last year | 5.4 (2.2) | 8.9 (0.3) | t144 = 14.19 | <0.001 | 2.350 |
| GF:R highest in last year | 7.4 (1.5) | 9.0 (0.2) | t144 = 9.66 | <0.001 | 1.600 |
| GF:S current | 5.4 (1.7) | 9.0 (0.2) | t144 = 18.10 | <0.001 | 2.998 |
| GF:S lowest in last year | 5.2 (1.8) | 8.9 (0.3) | t144 = 18.22 | <0.001 | 3.017 |
| GF:S highest in last year | 7.3 (1.2) | 9.0 (0.1) | t144 = 12.10 | <0.001 | 2.004 |
| Test | Score |
|---|---|
| BPRS Total score | 47.20 (9.53) |
| SANS/SAPS-derived components | |
| Auditory Hallucinations | 3.37 (3.21) |
| Unusual Perceptions | 0.93 (1.33) |
| Delusions | 5.95 (3.87) |
| Thought Disorder | 0.23 (0.34) |
| Inattention | 2.17 (2.10) |
| Inexpressivity | 7.43 (5.76) |
| Apathy/Asociality | 7.57 (3.94) |
| Medicated/Unmedicated | 54/16 |
| Medication dosage (CPZ equivalents) | 222.40 (122.17) |
| Mean days from first clinical contact to scan | 53.26 (71.2) |
| Median days from first contact to scan | 27 |
| Mean months DUP | 23.17 (38.53) |
| Median months DUP | 6.89 |
| Variable | B | ß | t-Statistic | p-Value | VIF |
|---|---|---|---|---|---|
| Age | 0.886 | 0.624 | 9.703 | <0.001 | 1.080 |
| Scanner | 1.902 | 0.136 | 2.111 | 0.037 | 1.096 |
| Sex | −2.865 | −0.196 | 3.126 | 0.002 | 1.031 |
| pSES | −0.016 | −0.031 | 0.478 | 0.633 | 1.085 |
| Group (FESz vs. HC) | −0.278 | −0.04 | 0.616 | 0.539 | 1.133 |
| Variable | B | ß | t-Statistic | p-Value | VIF |
|---|---|---|---|---|---|
| Premorbid IQ model | |||||
| Age | 0.887 | 0.623 | 10.093 | <0.001 | 1.072 |
| Scanner | 1.573 | 0.113 | 1.833 | 0.069 | 1.074 |
| Sex | −2.692 | −0.184 | 3.074 | 0.003 | 1.004 |
| WASI vocabulary t-score | −0.138 | −1.630 | −2.725 | 0.007 | 1.005 |
| MATRICS battery model | |||||
| Age | 0.969 | 0.684 | 10.381 | <0.001 | 1.207 |
| Scanner | 1.678 | 0.121 | 1.911 | 0.058 | 1.121 |
| Sex | −2.626 | −0.180 | −2.891 | 0.004 | 1.079 |
| Trail Making Test | −0.076 | −0.136 | −1.231 | 0.221 | 3.392 |
| Speed of Processing | 0.087 | 0.167 | 1.228 | 0.221 | 5.144 |
| Attention and Vigilance | −0.036 | −0.065 | −0.761 | 0.448 | 2.011 |
| Working Memory | −0.032 | −0.055 | −0.564 | 0.574 | 2.697 |
| Verbal Learning | 0.047 | 0.077 | 0.940 | 0.349 | 1.850 |
| Visual Learning | −0.058 | −0.092 | −1.146 | 0.254 | 1.810 |
| Reasoning and Problem Solving | −0.108 | −0.157 | −1.923 | 0.057 | 1.859 |
| Social Cognition | 0.013 | 0.025 | 0.366 | 0.715 | 1.282 |
| Social Functioning Model | |||||
| Age | 0.829 | 0.584 | 7.973 | <0.001 | 1.379 |
| Scanner | 2.180 | 0.158 | 2.381 | 0.019 | 1.137 |
| Sex | −1.972 | −0.136 | −1.908 | 0.059 | 1.296 |
| SFS Social Engagement/Withdrawal | 0.056 | 0.097 | 1.307 | 0.193 | 1.411 |
| SFS Interpersonal Interaction | −0.062 | −0.169 | −1.871 | 0.064 | 2.093 |
| SFS Recreation | −0.047 | −0.080 | −1.100 | 0.328 | 1.403 |
| SFS Employment Occupation | 0.054 | 0.053 | 0.698 | 0.486 | 1.508 |
| SFS Independence Performance | 0.068 | 0.108 | 1.282 | 0.202 | 1.825 |
| SFS Independence Competence | 0.007 | 0.011 | 0.129 | 0.898 | 1.752 |
| SFS Prosocial | 0.029 | 0.048 | 0.640 | 524 | 1.543 |
| GF:R Highest in Last Year | −0.416 | −0.080 | −0.674 | 0.502 | 3.657 |
| GF:S Highest in Last Year | 0.448 | 0.082 | 0.662 | 0.509 | 3.936 |
| Symptom Models (FESz only) | |||||
| Age | 1.041 | 0.669 | 7.582 | <0.001 | 1.117 |
| Scanner | 0.729 | 0.053 | 0.588 | 0.559 | 1.155 |
| Sex | −4.763 | −0.301 | −3.353 | 0.001 | 1.159 |
| Auditory Hallucinations | 0.019 | 0.009 | 0.088 | 0.930 | 1.378 |
| Unusual Perceptions and Behaviors | −0.773 | −0.147 | −1.556 | 0.125 | 1.285 |
| Delusions | 0.262 | 0.145 | 1.355 | 0.181 | 1.653 |
| Thought Disorder | 0.863 | 0.043 | 0.438 | 0.663 | 1.355 |
| Inattention | 0.343 | 0.103 | 0.997 | 0.323 | 1.545 |
| Inexpressivity | 0.312 | 0.258 | 2.472 | 0.016 | 1.568 |
| Apathy and Asociality | −0.150 | −0.085 | −0.857 | 0.395 | 1.406 |
| Age | 1.038 | 0.667 | 8.006 | <0.001 | 1.091 |
| Scanner | 0.900 | 0.065 | 0.769 | 0.444 | 1.091 |
| Sex | −4.035 | −0.255 | −3.053 | 0.003 | 1.066 |
| WASI Vocabulary t-score | −0.128 | −0.178 | −2.073 | 0.042 | 1.121 |
| Inexpressivity | 0.254 | 0.210 | 2.532 | 0.014 | 1.054 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salisbury, D.F.; Wulf, B.M.; Seebold, D.; Coffman, B.A.; Curtis, M.T.; Karim, H.T. Predicted Brain Age in First-Episode Psychosis: Association with Inexpressivity. Brain Sci. 2024, 14, 532. https://doi.org/10.3390/brainsci14060532
Salisbury DF, Wulf BM, Seebold D, Coffman BA, Curtis MT, Karim HT. Predicted Brain Age in First-Episode Psychosis: Association with Inexpressivity. Brain Sciences. 2024; 14(6):532. https://doi.org/10.3390/brainsci14060532
Chicago/Turabian StyleSalisbury, Dean F., Brian M. Wulf, Dylan Seebold, Brian A. Coffman, Mark T. Curtis, and Helmet T. Karim. 2024. "Predicted Brain Age in First-Episode Psychosis: Association with Inexpressivity" Brain Sciences 14, no. 6: 532. https://doi.org/10.3390/brainsci14060532
APA StyleSalisbury, D. F., Wulf, B. M., Seebold, D., Coffman, B. A., Curtis, M. T., & Karim, H. T. (2024). Predicted Brain Age in First-Episode Psychosis: Association with Inexpressivity. Brain Sciences, 14(6), 532. https://doi.org/10.3390/brainsci14060532






