The Use of Technology-Based Simulation among Medical Students as a Global Innovative Solution for Training
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hill, C.S.; Dias, L.; Kitchen, N. Perceptions of Neurosurgery: A Survey of Medical Students and Foundation Doctors. Br. J. Neurosurg. 2011, 25, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Tomasello, F. Neurosurgical Recruitment: The Gold Rush. World Neurosurg. 2015, 83, 37–38. [Google Scholar] [CrossRef] [PubMed]
- Nahed, B.V.; Babu, M.A.; Smith, T.R.; Heary, R.F. Malpractice Liability and Defensive Medicine: A National Survey of Neurosurgeons. PLoS ONE 2012, 7, e39237. [Google Scholar] [CrossRef] [PubMed]
- Stumpo, V.; Latour, K.; Traylor, J.I.; Staartjes, V.E.; Giordano, M.; Caccavella, V.M.; Olivi, A.; Ricciardi, L.; Signorelli, F. Medical Student Interest and Recruitment in Neurosurgery. World Neurosurg. 2020, 141, 448–454.e6. [Google Scholar] [CrossRef] [PubMed]
- Bernardo, A. Virtual Reality and Simulation in Neurosurgical Training. World Neurosurg. 2017, 106, 1015–1029. [Google Scholar] [CrossRef]
- Hanrahan, J.; Sideris, M.; Tsitsopoulos, P.P.; Bimpis, A.; Pasha, T.; Whitfield, P.C.; Papalois, A.E. Increasing Motivation and Engagement in Neurosurgery for Medical Students through Practical Simulation-Based Learning. Ann. Med. Surg. 2018, 34, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Smith, R. The Long History of Gaming in Military Training. Simul. Gaming 2010, 41, 6–19. [Google Scholar] [CrossRef]
- Aebersold, M. The History of Simulation and Its Impact on the Future. AACN Adv. Crit. Care 2016, 27, 56–61. [Google Scholar] [CrossRef]
- Rehder, R.; Abd-El-Barr, M.; Hooten, K.; Weinstock, P.; Madsen, J.R.; Cohen, A.R. The Role of Simulation in Neurosurgery. Childs Nerv. Syst. 2016, 32, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Bova, F.J.; Rajon, D.A.; Friedman, W.A.; Murad, G.J.; Hoh, D.J.; Jacob, R.P.; Lampotang, S.; Lizdas, D.E.; Lombard, G.; Lister, J.R. Mixed-Reality Simulation for Neurosurgical Procedures. Neurosurgery 2013, 73, S138–S145. [Google Scholar] [CrossRef]
- Benet, A.; Rincon-Torroella, J.; Lawton, M.T.; González Sánchez, J.J. Novel Embalming Solution for Neurosurgical Simulation in Cadavers: Laboratory Investigation. J. Neurosurg. 2014, 120, 1229–1237. [Google Scholar] [CrossRef]
- Pelargos, P.E.; Nagasawa, D.T.; Lagman, C.; Tenn, S.; Demos, J.V.; Lee, S.J.; Bui, T.T.; Barnette, N.E.; Bhatt, N.S.; Ung, N.; et al. Utilizing Virtual and Augmented Reality for Educational and Clinical Enhancements in Neurosurgery. J. Clin. Neurosci. 2017, 35, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Eric, L.; Grimson, W.; Kikinis, R.; Jolesz, F.A.; Mc, L.; Black, P. Image-Guided Surgery. Sci. Am. 1999, 280, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Mitha, A.P.; Almekhlafi, M.A.; Janjua, M.J.J.; Albuquerque, F.C.; McDougall, C.G. Simulation and Augmented Reality in Endovascular Neurosurgery: Lessons From Aviation. Neurosurgery 2013, 72, A107–A114. [Google Scholar] [CrossRef] [PubMed]
- Kockro, R.A.; Stadie, A.; Schwandt, E.; Reisch, R.; Charalampaki, C.; Ng, I.; Yeo, T.T.; Hwang, P.; Serra, L.; Perneczky, A. A collaborative virtual reality environment for neurosurgical planning and training. Oper. Neurosurg. 2007, 61, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Pourmand, A.; Davis, S.; Marchak, A.; Whiteside, T.; Sikka, N. Virtual Reality as a Clinical Tool for Pain Management. Curr. Pain Headache Rep. 2018, 22, 53. [Google Scholar] [CrossRef] [PubMed]
- Gourlay, D.; Lun, K.C.; Lee, Y.N.; Tay, J. Virtual Reality for Relearning Daily Living Skills. Int. J. Med. Inform. 2000, 60, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Madhavan, K.; Kolcun, J.P.G.; Chieng, L.O.; Wang, M.Y. Augmented-Reality Integrated Robotics in Neurosurgery: Are We There Yet? Neurosurg. Focus 2017, 42, E3. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.; Narayanan, M.D.K.; Umana, G.E.; Montemurro, N.; Chaurasia, B.; Deora, H. Virtual Reality in Neurosurgery: Beyond Neurosurgical Planning. Int. J. Environ. Res. Public Health 2022, 19, 1719. [Google Scholar] [CrossRef]
- Abhari, K.; Baxter, J.S.H.; Chen, E.C.S.; Khan, A.R.; Peters, T.M.; De Ribaupierre, S.; Eagleson, R. Training for Planning Tumour Resection: Augmented Reality and Human Factors. IEEE Trans. Biomed. Eng. 2015, 62, 1466–1477. [Google Scholar] [CrossRef]
- Cannizzaro, D.; Zaed, I.; Safa, A.; Jelmoni, A.J.M.; Composto, A.; Bisoglio, A.; Schmeizer, K.; Becker, A.C.; Pizzi, A.; Cardia, A.; et al. Augmented Reality in Neurosurgery, State of Art and Future Projections. A Systematic Review. Front. Surg. 2022, 9, 864792. [Google Scholar] [CrossRef] [PubMed]
- Gasco, J.; Holbrook, T.J.; Patel, A.; Smith, A.; Paulson, D.; Muns, A.; Desai, S.; Moisi, M.; Kuo, Y.-F.; Macdonald, B.; et al. Neurosurgery Simulation in Residency Training: Feasibility, Cost, and Educational Benefit. Neurosurgery 2013, 73, S39–S45. [Google Scholar] [CrossRef] [PubMed]
- Joseph, F.J.; Weber, S.; Raabe, A.; Bervini, D. Neurosurgical Simulator for Training Aneurysm Microsurgery—A User Suitability Study Involving Neurosurgeons and Residents. Acta Neurochir. 2020, 162, 2313–2321. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.A.; Bhandarkar, A.R.; Riviere-Cazaux, C.; Bauman, M.M.J.; Wang, K.; Carlstrom, L.P.; Graffeo, C.S.; Spinner, R.J. The Early Bird Gets the Worm: Introducing Medical Students to Microsurgical Technique via a Low-Cost, User-Friendly, Reusable Simulation System. World Neurosurg. 2022, 167, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Robertson, F.C.; Stapleton, C.J.; Coumans, J.-V.C.E.; Nicolosi, F.; Vooijs, M.; Blitz, S.; Guerrini, F.; Spena, G.; Giussani, C.; Zoia, C.; et al. Applying Objective Metrics to Neurosurgical Skill Development with Simulation and Spaced Repetition Learning. J. Neurosurg. 2023, 139, 1092–1100. [Google Scholar] [CrossRef]
- Dewan, M.C.; Rattani, A.; Fieggen, G.; Arraez, M.A.; Servadei, F.; Boop, F.A.; Johnson, W.D.; Warf, B.C.; Park, K.B. Global Neurosurgery: The Current Capacity and Deficit in the Provision of Essential Neurosurgical Care. Executive Summary of the Global Neurosurgery Initiative at the Program in Global Surgery and Social Change. J. Neurosurg. 2018, 130, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Dada, O.E.; Ooi, S.Z.Y.; Bukenya, G.W.; Kenfack, Y.J.; Le, C.; Ohonba, E.; Adeyemo, E.; Narain, K.; Awad, A.K.; Barrie, U.; et al. Evaluating the Impact of Neurosurgical Rotation Experience in Africa on the Interest and Perception of Medical Students Towards a Career in Neurosurgery: A Continental, Multi-Centre, Cross-Sectional Study. Front. Surg. 2022, 9, 766325. [Google Scholar] [CrossRef] [PubMed]
- Menna, G.; Kolias, A.; Esene, I.N.; Barthélemy, E.J.; Hoz, S.; Laeke, T.; Veiga Silva, A.C.; Longo-Calderón, G.M.; Baticulon, R.E.; Zabala, J.P.; et al. Reducing the Gap in Neurosurgical Education in LMICs: A Report of a Non-Profit Educational Program. World Neurosurg. 2024, 182, e792–e797. [Google Scholar] [CrossRef]


| QUESTION | ANSWERED REQUIRED |
|---|---|
| PERSONAL INFO | |
| Age | Open (numerical) |
| Nationality | Open |
| STUDIES AND BACKGROUND | |
| University | Open |
| Current year of studies | Open (numerical) |
| High school attended (type) | Open |
| Interest in pursuing a medical career | Clinical/surgical |
| If clinical, does it involve neurosciences? | Yes/No |
| If surgical, which field | Open |
| Dominant hand | Left/Right |
| Visual defects | Myopia/Hypermetropia/Astigmatism/None |
| MOTIVATION | |
| Why have you chosen to take part in this project? | Multiple choice |
| QUESTION | ANSWERED REQUIRED |
|---|---|
| MEDICAL SKILLS POSSESSED BEFORE THE EVENT | |
| Seen a surgical operation | Yes/No |
| Attended a suture technique course | Yes/No |
| GENERAL SKILLS POSSESED BEFORE THE EVENT | |
| I know how to play a musical instrument. | Likert scale from 1 to 5 |
| I know how to draw or paint | Likert scale from 1 to 5 |
| I know how to make a sculpture | Likert scale from 1 to 5 |
| I am practical with DIY/gardening | Likert scale from 1 to 5 |
| I am practical with needlework | Likert scale from 1 to 5 |
| I play videogames | Likert scale from 1 to 5 |
| If you play videogames (answer ≥ 3): | |
| Which kind of videogames? | Open |
| Have you ever used kinematic sensors? | Yes/No |
| POST SIMULATION ASSESMENT | |
| The event made me realize that I am interested in pursuing a surgical path. | Likert scale from 1 to 5 |
| The event made me realize that I am interested in pursuing a medical path in the neurosciences. | Likert scale from 1 to 5 |
| The event was useful to understand my postgraduate orientation outside of a surgical path. | Likert scale from 1 to 5 |
| The event was useful to understand my postgraduate orientation in the neurosciences’ field. | Likert scale from 1 to 5 |
| I would like to join another simulation event. | Likert scale from 1 to 5 |
| I felt comfortable while handling the surgical instruments. | Likert scale from 1 to 5 |
| Number of Participants | 141 | |
| Mean Age | 21 | |
| Year of Medical School | 1st | 10 |
| 2nd | 56 | |
| 3rd | 39 | |
| 4th | 22 | |
| 5th | 7 | |
| 6th | 7 | |
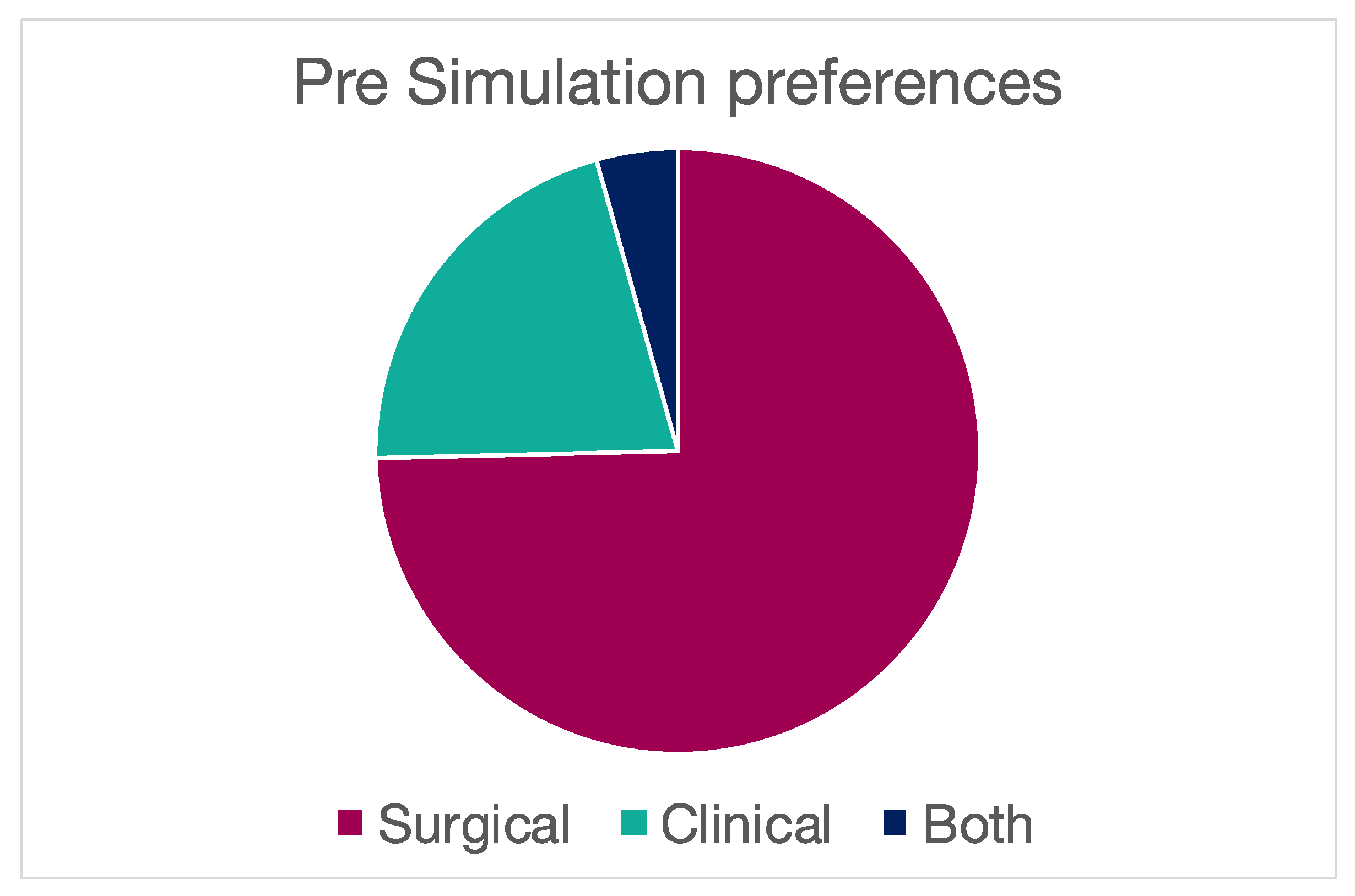
| Orientation | Surgical | 98 |
| Clinical | 21 | |
| Both | 6 | |
| Hand | R | 127 |
| L | 15 | |
| Vision | M | 53 |
| M/A | 22 | |
| H | 3 | |
| NONE | 42 | |
| M/A/H | 1 | |
| Surgical Intervention | Yes | 79 |
| No | 67 | |
| Suture Course | Yes | 41 |
| No | 105 | |
| Kinetic Sensors | Yes | 19 |
| No | 49 |
| The event made me realize that I am interest in pursuing a surgical path | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Surgical | 13 (12.3) | 93 (87.8) | <0.001 |
| Clinical | 17 (58.6) | 12 (41.4) | |
| Both | 2 (33.3) | 4 (66.6) | |
| The event made me realize that I am interest in pursuing a medical path in the neurosciences | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Neuro | 26 (32.5) | 45 (72.6) | <0.001 |
| No neuro | 54 (67.5) | 17 (27.4) | |
| The event was useful in understanding my postgraduate orientation outside of a surgical path | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Surgical | 72 (67.9) | 34 (32.0) | 0.259 |
| Clinical | 16 (53.3) | 14 (46.7) | |
| Both | 3 (50) | 3 (50) | |
| The event was useful in understanding my postgraduate orientation in the neuroscience’s field | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Neuro | 34 (47.9) | 37 (52.1) | 0.004 |
| No neuro | 52 (72.2) | 20 (27.8) | |
| I would like to join another simulation event | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Sutures | 3 (7.3) | 38 (92.6) | 0.072 |
| No sutures | 1 (0.9) | 100 (99.0) | |
| I felt comfortable while handling the surgical instruments | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Sutures YES | 5 (12.2) | 36 (87.8) | 0.012 |
| Sutures NO | 34 (33.7) | 67 (66.3) | |
| I felt comfortable while handling the surgical instruments | |||
| Precourse Attitude | Bad outcome (%) | Good outcome (%) | p value |
| Surgical | 26 (24.5) | 80 (75.5) | 0.204 |
| Clinical | 12 (40.0) | 18 (60.0) | |
| Both | 1 (16.7) | 5 (83.3) | |
| The event made me realize that I am interested in pursuing a surgical path | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 2 (1.4) | Bad | 32 (22.5) |
| 2 | 5 (3.5) | ||
| 3 | 25 (17.6) | ||
| 4 | 58 (40.8) | Good | 110 (77.5) |
| 5 | 52 (36.6) | ||
| The event made me realize that I am interested in pursuing a medical path in neuroscience | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 11 (7.8) | Bad | 80 (56.3) |
| 2 | 13 (9.2) | ||
| 3 | 56 (39.4) | ||
| 4 | 31 (21.8) | Good | 62 (43.7) |
| 5 | 31 (21.8) | ||
| The event was useful in understanding my postgraduate orientation outside of a surgical path. | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 19 (13.3) | Bad | 92 (64.3) |
| 2 | 23 (16.1) | ||
| 3 | 50 (35.0) | ||
| 4 | 38 (26.6) | Good | 51 (35.7) |
| 5 | 13 (9.1) | ||
| the event was useful in understanding my postgraduate orientation in the neuroscience’s field | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 10 (7.0) | Bad | 86 (60.1) |
| 2 | 26 (18.2) | ||
| 3 | 50 (35.0) | ||
| 4 | 37 (25.9) | Good | 57 (39.9) |
| 5 | 20 (14.0) | ||
| I would like to join another simulation event | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 0 (0.0) | Bad | 4 (2.8) |
| 2 | 0 (0.0) | ||
| 3 | 4 (2.8) | ||
| 4 | 26 (18.2) | Good | 139 (97.2) |
| 5 | 113 (79.0) | ||
| I felt comfortable while handling the surgical instruments | |||
| Grade | Outcome (%) | Grade | Outcome (%) |
| 1 | 1 (0.6) | Bad | 39 (27.3) |
| 2 | 10 (7.0) | ||
| 3 | 28 (19.6) | ||
| 4 | 57 (39.9) | Good | 104 (72.7) |
| 5 | 47 (32.9) | ||
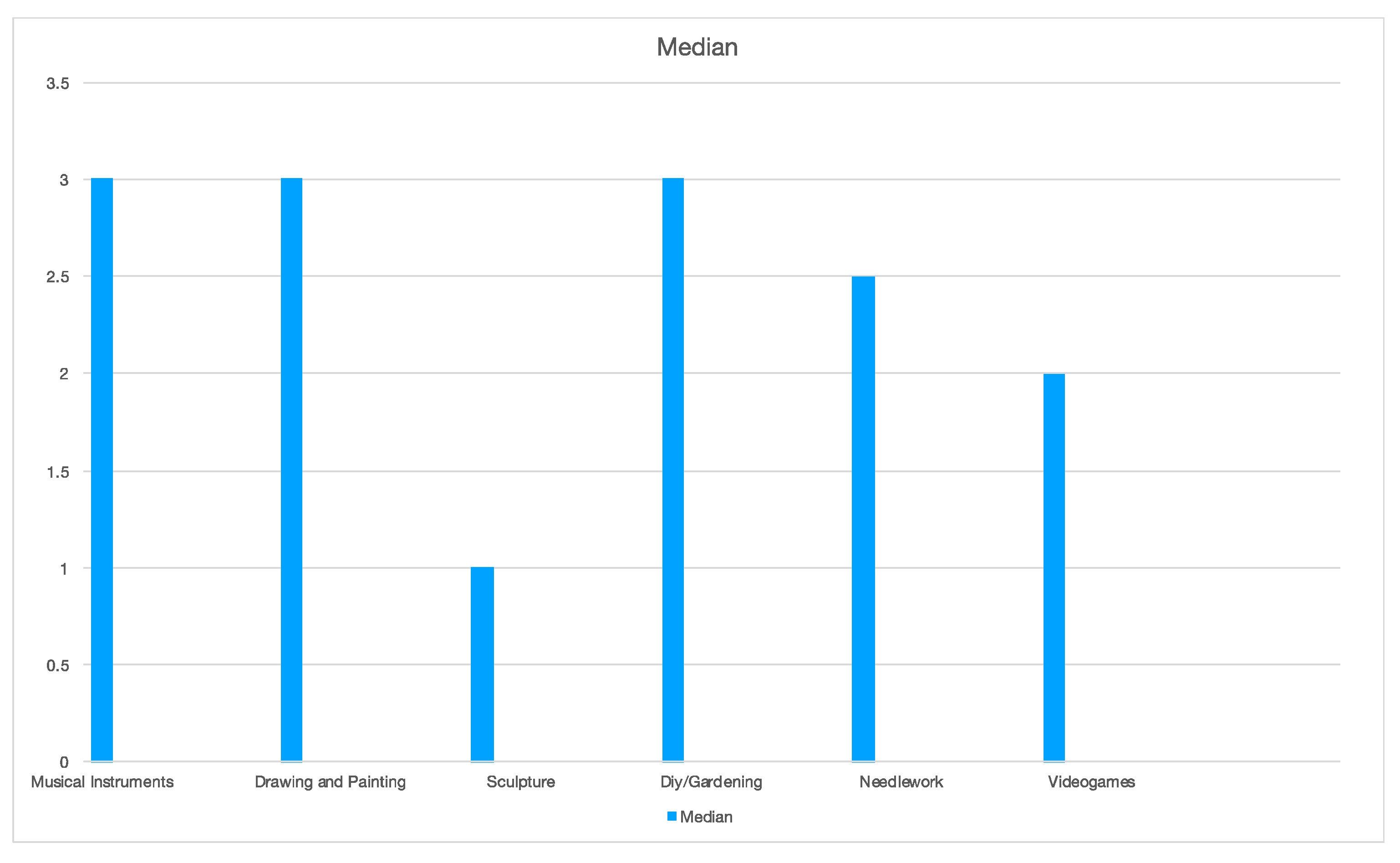
| Musical Instruments | |||
| Grade | N. of Participants | % | Median |
| 1 | 26 | 18.2 | 3 |
| 2 | 25 | 17.5 | |
| 3 | 22 | 15.4 | |
| 4 | 41 | 28.7 | |
| 5 | 29 | 20.3 | |
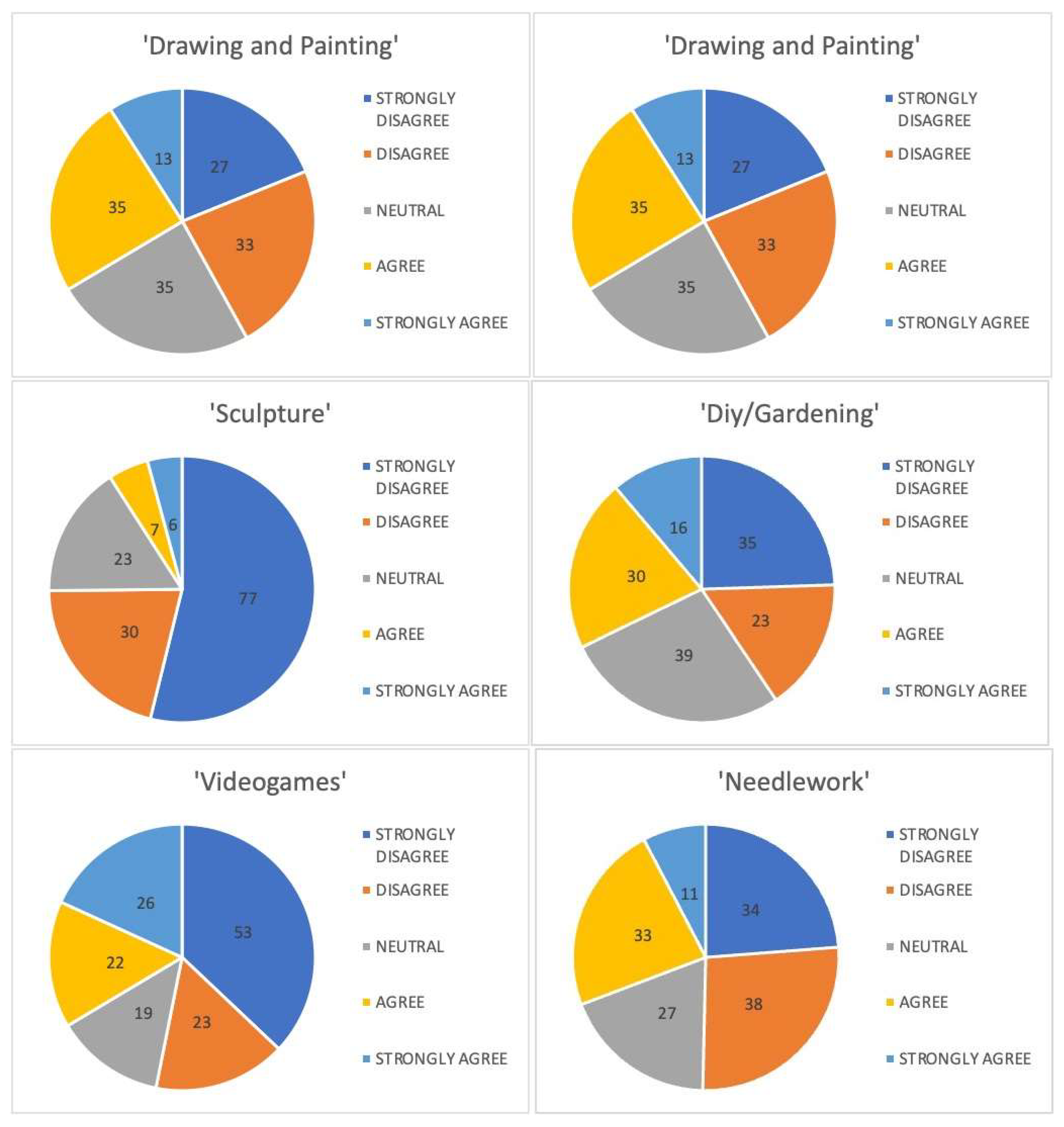
| Drawing and Painting | |||
| Grade | N. of Participants | % | Median |
| 1 | 27 | 18.9 | 3 |
| 2 | 33 | 23.1 | |
| 3 | 35 | 24.5 | |
| 4 | 35 | 24.5 | |
| 5 | 13 | 9.1 | |
| Sculpture | |||
| Grade | N. of Participants | % | Median |
| 1 | 77 | 53.8 | 1 |
| 2 | 30 | 21.0 | |
| 3 | 23 | 16.1 | |
| 4 | 7 | 4.9 | |
| 5 | 6 | 4.2 | |
| Diy/Gardening | |||
| Grade | N. of Participants | % | Median |
| 1 | 35 | 24.5 | 3 |
| 2 | 23 | 16.1 | |
| 3 | 39 | 27.3 | |
| 4 | 30 | 21.0 | |
| 5 | 16 | 11.2 | |
| Needlework | |||
| Grade | N. of Participants | % | Median |
| 1 | 34 | 23.8 | 2.5 |
| 2 | 38 | 26.6 | |
| 3 | 27 | 18.9 | |
| 4 | 33 | 23.1 | |
| 5 | 11 | 7.7 | |
| Videogames | |||
| Grade | N. of Participants | % | Median |
| 1 | 53 | 37.1 | 2 |
| 2 | 23 | 16.1 | |
| 3 | 19 | 13.3 | |
| 4 | 22 | 15.4 | |
| 5 | 26 | 18.2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerrini, F.; Bertolino, L.; Safa, A.; Pittarello, M.; Parisi, A.; Beretta, L.V.; Zambelli, E.; Totis, F.; Campanaro, G.; Pavia, L.; et al. The Use of Technology-Based Simulation among Medical Students as a Global Innovative Solution for Training. Brain Sci. 2024, 14, 627. https://doi.org/10.3390/brainsci14070627
Guerrini F, Bertolino L, Safa A, Pittarello M, Parisi A, Beretta LV, Zambelli E, Totis F, Campanaro G, Pavia L, et al. The Use of Technology-Based Simulation among Medical Students as a Global Innovative Solution for Training. Brain Sciences. 2024; 14(7):627. https://doi.org/10.3390/brainsci14070627
Chicago/Turabian StyleGuerrini, Francesco, Luca Bertolino, Adrian Safa, Matilde Pittarello, Anna Parisi, Ludovica Vittoria Beretta, Elena Zambelli, Francesca Totis, Giovanni Campanaro, Lorenzo Pavia, and et al. 2024. "The Use of Technology-Based Simulation among Medical Students as a Global Innovative Solution for Training" Brain Sciences 14, no. 7: 627. https://doi.org/10.3390/brainsci14070627
APA StyleGuerrini, F., Bertolino, L., Safa, A., Pittarello, M., Parisi, A., Beretta, L. V., Zambelli, E., Totis, F., Campanaro, G., Pavia, L., Spena, G., Nicolosi, F., & Servadei, F. (2024). The Use of Technology-Based Simulation among Medical Students as a Global Innovative Solution for Training. Brain Sciences, 14(7), 627. https://doi.org/10.3390/brainsci14070627






