The Adaptation of the Communicative Effectiveness Index (CETI) into Greek: A Reliability and Validity Study
Abstract
1. Introduction
1.1. Evidence-Based Functional Communication Assessment Measures
1.2. The Communication Effectiveness Index (CETI)
1.3. Other Language Adaptations of the CETI
1.4. The Importance of the Greek Validation of the CETI
1.5. Foundational Theoretical Frameworks
1.6. Aim
2. Materials and Methods
2.1. Design
2.2. Participation Criteria
2.3. Recruitment
2.4. Sample Size
2.5. Participants
2.6. Data Collection and Procedures
2.7. Measures
- The Aphasia Severity Rating Scale (ASRS) from the Greek adaptation of the Boston Diagnostic Aphasia Examination Short Form (BDAE-SF) [39]. The ASRS is a rating scale used to measure aphasia severity. This scale was used to evaluate the severity of the observed language and communication difficulties of the participants with aphasia. This included (1) a 10 min semi-structured interview about their previous employment, their stroke story, and basic demographic information and (2) a description of the “Cookie Theft” picture. Aphasia severity was evaluated based on the fluency and intelligibility of the spoken output. The scores of the ASRS ranged from 0 to 5, with 0 indicating very severe non-fluent aphasia and 5, very mild aphasia predominantly characterized by naming difficulties [39].
- The standardized Greek version of the Hospital Anxiety and Depression Scale (HADS-GR) [40]. The HADS-GR evaluates potential depression and anxiety in people with medical conditions. The HADS-GR is a self-report rating scale with 14 items each rated on a 4-point Likert scale, ranging between 0 and 3. The anxiety and depression subscales contain 7 items each. The total score is calculated by the sum of the 7 items for each subscale. A score of 0–7 indicates no depression (or anxiety, respectively), 8–10 indicates abnormal borderline, and 11–21 indicates severe depression or anxiety [40].
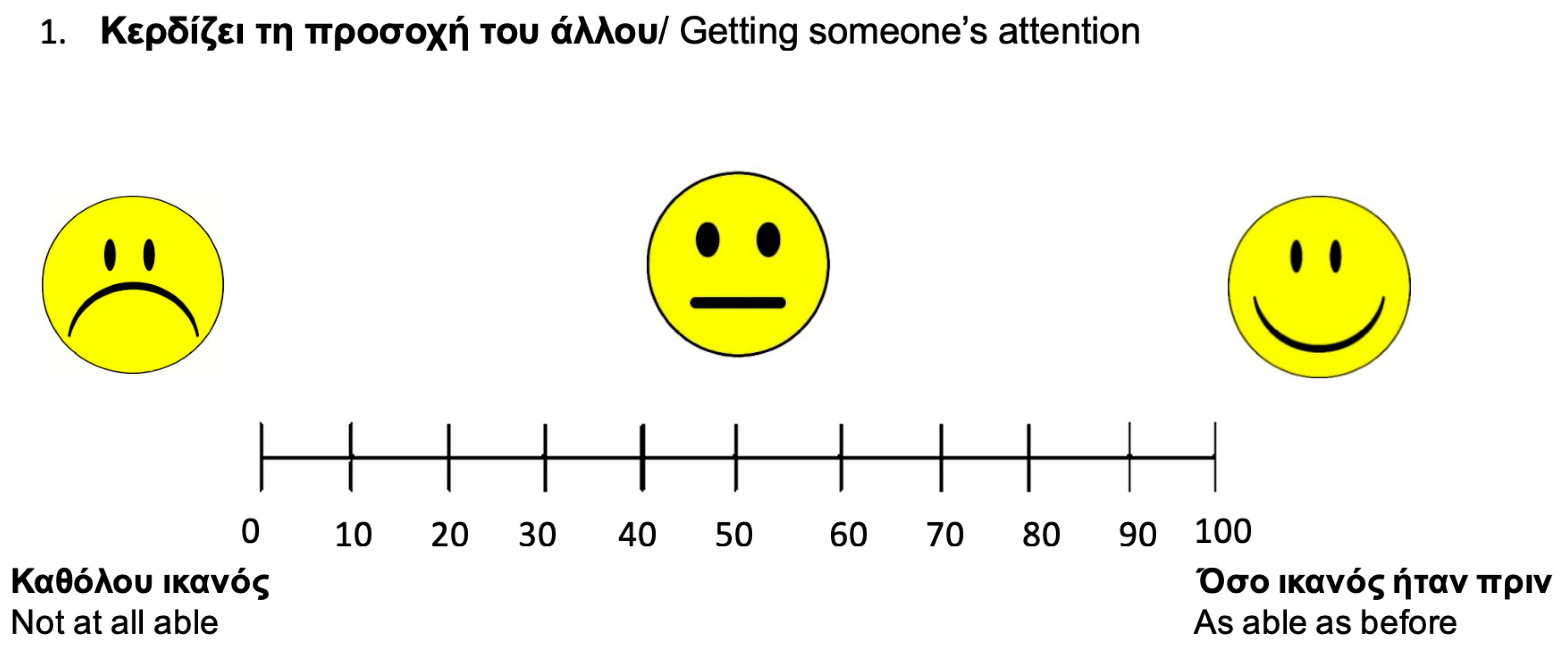
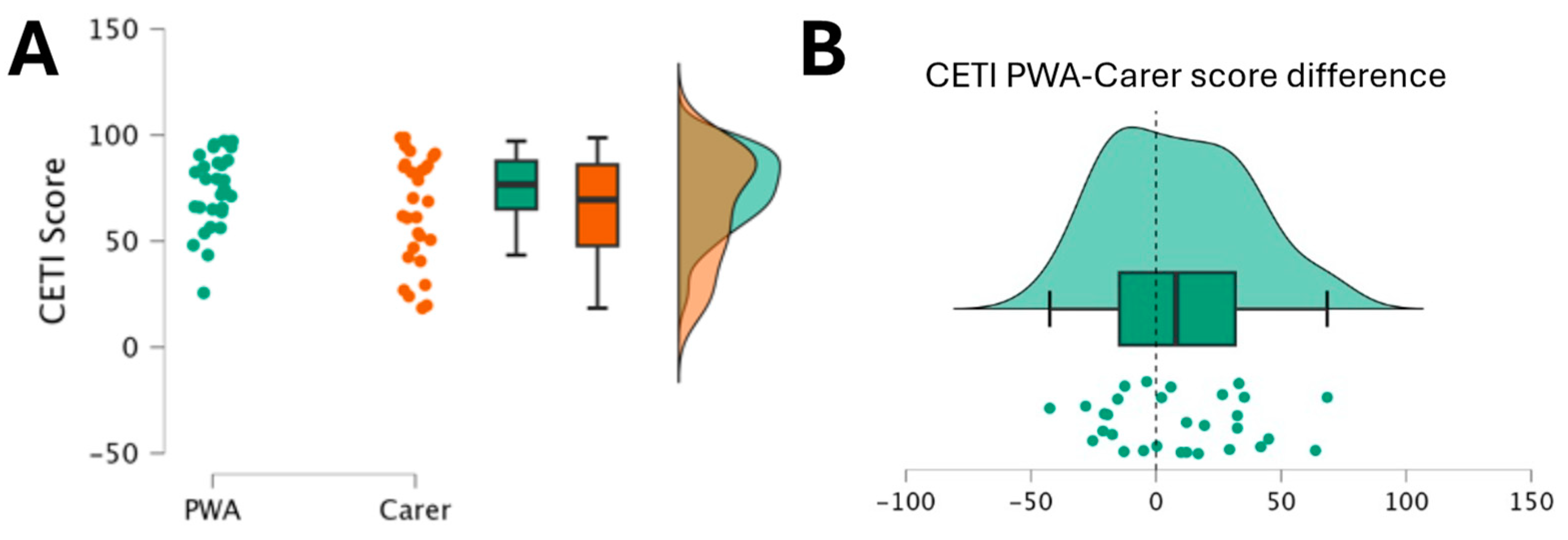
- The Greek version of the CETI. The CETI is a 16-item questionnaire completed by the carers of people with chronic aphasia. The CETI assesses both verbal (10 items) and non-verbal (6 items) communication skills in 16 different daily situations [10]. Each statement was presented to the respondents using a visual analog scale represented by a horizontal line of 100 mm. Zero means “not able at all” and 100 “as able as before”. Pedersen et al. [12] found that raters often placed their crosses midway on the visual analog scale lines when scoring 0 or 100 on the Danish CETI. Therefore, to improve precision in the Greek version, smiling faces were added to signify key indicators from “not able at all” to “as able as before”, assisting raters in marking the scale more accurately (see Figure 1).For each statement, the carer and the person with aphasia had to mark their response on the visual analog scale with a pencil. Each answer was rated from 0 to 100 and the total score was calculated by dividing the sum of the individual situation ratings by the total number of situations [10]. Lower scores show lower abilities in everyday functional communication and higher scores show better functional communication in everyday life [10].
- The standardized Greek version of the Scenario Test-GR [6]. The Scenario Test-GR is a tool that evaluates functional communication in simulated everyday communication situations. Scoring is completed by the clinician. The Scenario Test-GR consists of 18 items as part of six daily life scenarios (each scenario has 3 questions) using black and white pictures. The score for each item ranges from 0 to 3 for each question. The total score is calculated from the sum of all questions. The scores range from 0 to 54, with a lower score indicating poor functional communication and a higher score indicating better functional communication [9].
- The standardized Greek version of the Aphasia Impact Questionnaire-21 (AIQ-21-GR) [41]. The AIQ-21-GR is a self-reported questionnaire that evaluates the impact of aphasia on the quality of life of PWA. It includes 21 questions and is divided into three domains: participation, communication, and emotional state. Participation includes 7 items, communication 6 items, and emotional state 11 items. Each item has a 5-point rating scale (0–4), with 0 indicating “no problem” and 4 indicating “impossible”. Total scores range from 0 to 84, with lower scores indicating a lower impact of aphasia on quality of life [42].
2.8. Testing of Reliability
2.8.1. Test–Retest Reliability
2.8.2. Inter-Rater Reliability
2.9. Testing of Validity
2.9.1. Convergent Validity
- Scores of the CETI-GR will significantly correlate with measures of the psychosocial domain, that is, the AIQ-21-GR, as there is evidence of a link between low functional communication and poor quality of life [44].
2.9.2. Content Validity
2.10. Criteria for Psychometric Testing
2.11. Data Analysis
3. Results
3.1. Measures
3.2. Reliability Analyses
3.2.1. Internal Consistency
3.2.2. Intraclass Correlations
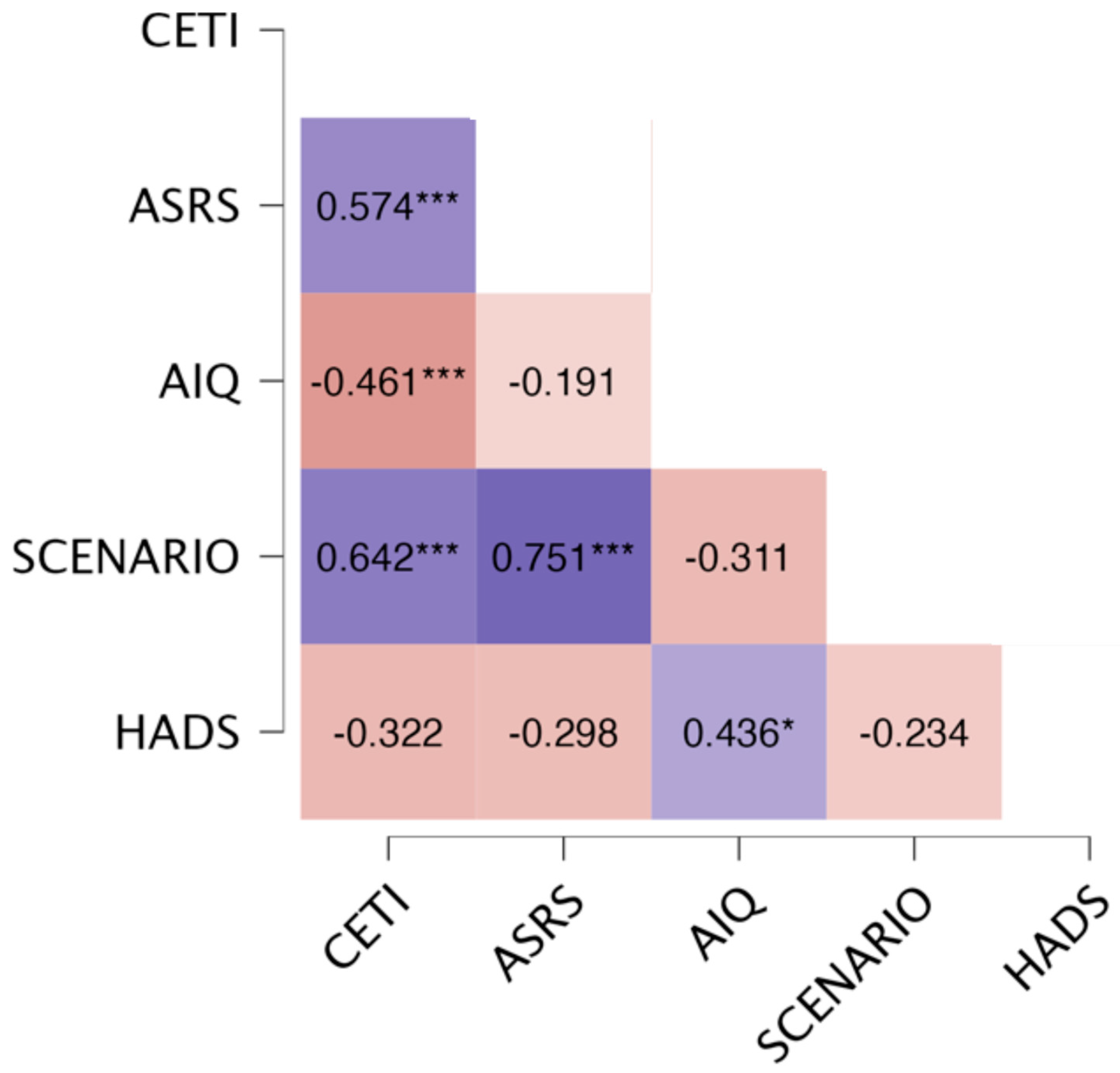
3.3. Validity Analyses
Content Validity
4. Discussion
4.1. CETI-GR’s Reliability
4.1.1. Internal Consistency
4.1.2. Test–Retest Reliability
4.1.3. Inter-Rater Reliability
4.1.4. Reliability and the Social Context
4.2. CETI-GR’s Validity
4.2.1. Convergent Validity
Correlation of the CETI-GR with Aphasia Severity
Correlation of the CETI-GR with the Scenario Test
Correlation of the CETI-GR with the Aphasia Impact Questionnaire
Correlation of the CETI-GR with Depression and Anxiety
4.2.2. Content Validity
4.3. The Use of the Modified Index
4.4. Clinical Implications
4.5. Limitations of the Study
4.6. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| CETI | Communicative Effectiveness Index |
| CETI-GR | Greek version of the Communicative Effectiveness Index |
| PWA | People with aphasia |
| ROMA-COS | Research Outcome Measurement in Aphasia Consensus Statement |
| WAB | Western Aphasia Battery |
| SQ | Speech Questionnaire |
| PICA | Porch Index of Communicative Ability |
| ADL | Activities of Daily Living scale |
| IADL | Activities of Daily Living scale |
| BI | Barthel Index |
| FAI | Frenchay Activity Index |
| ADRS | Aphasic Depression Rating Scale |
| NID | Non-Verbal Index of Depression |
| BDI | Beck Depression Inventory |
| PPI | Patient and Public Involvement |
| ASRS | Aphasia Severity Rating Scale |
| HADS | Hospital Anxiety and Depression Scale |
| AIQ-21-GR | Greek version of the Aphasia Impact Questionnaire-21 |
| BDAE-SF | Boston Diagnostic Aphasia Examination Short Form |
| HADS-GR | Greek version of the Hospital Anxiety and Depression Scale |
| COSMIN | Consensus-based Standards for the selection of health Measurement Instruments guidelines |
Appendix A
| Situations Rated by the Communicative Effectiveness Index (CETI) | ||
| Item # | Original English Version | Adapted Greek Version |
| 1 | Getting someone’s attention | Κερδίζει τη προσοχή του άλλου |
| 2 | Getting involved in group conversations about him/her | Συμμετέχει σε ομαδικές συζητήσεις που τον/την αφορούν |
| 3 | Giving “yes” and “no” answers appropriately | Aπαντάει «ναι» και «όχι» κατάλληλα |
| 4 | Communicating his/her emotions | Εκφράζει τα συναισθήματα του/της |
| 5 | Indicating he/she understands what is being said to him/her | Δείχνει ότι αυτός/αυτή καταλαβαίνει τι του/της λένε |
| 6 | Having coffee, time visits and conversations with friends and neighbors | Συμμετέχει σε επισκέψεις για καφέ και συζητήσεις με φίλους και γείτονες |
| 7 | Having a one-to-one conversation | Συζητάει ένας προς ένας |
| 8 | Saying the name of someone whose face is in front of him/her | Λέει το όνομα του ατόμου που είναι μπροστά του/της |
| 9 | Communicating physical needs such as aches and pains | Εκφράζει προβλήματα όπως πόνοι στο σώμα |
| 10 | Having a spontaneous conversation | Ξεκινάει μια συζήτηση αυθόρμητα |
| 11 | Responding to or communicating anything (including “yes” or “no”) without words | Aνταποκρίνεται ή εκφράζεται (συμπεριλαμβανομένου του «ναι» και του «όχι») χωρίς λέξεις |
| 12 | Starting a conversation with people who are not close family | Ξεκινά μια συζήτηση με άτομα τα οποία δεν είναι στενοί συγγενείς |
| 13 | Understanding writing | Κατανοεί την γραφή |
| 14 | Being a part of a conversation when it is fast and there are a number of people involved | Λαμβάνει μέρος σε μια γρήγορη συζήτηση με πολλά άτομα |
| 15 | Participating in a conversation with strangers | Συμμετέχει σε μια συζήτηση με αγνώστους |
| 16 | Describing or discussing something at length | Περιγράφει ή συζητά κάτι εις βάθος |
References
- Holland, A.L. The Value of “Communication Strategies” in the Treatment of Aphasia. Aphasiology 2021, 35, 984–994. [Google Scholar] [CrossRef]
- Hilari, K.; Behn, N.; James, K.; Northcott, S.; Marshall, J.; Thomas, S.; Simpson, A.; Moss, B.; Flood, C.; McVicker, S.; et al. Supporting Wellbeing through Peer-Befriending (SUPERB) for People with Aphasia: A Feasibility Randomised Controlled Trial. Clin. Rehabil. 2021, 35, 1151–1163. [Google Scholar] [CrossRef]
- Baker, C.; Thomas, S.; Tjokrowijoto, P.; Ryan, B.; Kneebone, I.; Stolwyk, R. Aphasia Depression and Psychological Therapy (ADaPT): Perspectives of People with Post-Stroke Aphasia on Participating in a Modified Cognitive Behavioral Therapy. Healthcare 2024, 12, 771. [Google Scholar] [CrossRef]
- Doedens, W.; Meteyard, L. What is Functional Communication? A Theoretical Framework for Real-World Communication Applied to Aphasia Rehabilitation. Neuropsychol. Rev. 2022, 32, 937–973. [Google Scholar] [CrossRef]
- Worrall, L.; Ryan, B.; Hudson, K.; Kneebone, I.; Simmons-Mackie, N.; Khan, A.; Hoffmann, T.; Power, E.; Togher, L.; Rose, M. Reducing the Psychosocial Impact of Aphasia on Mood and Quality of Life in People with Aphasia and the Impact of Caregiving in Family Members through the Aphasia Action Success Knowledge (Aphasia ASK) Program: Study Protocol for a Randomized Controlled Trial. Trials 2016, 17, 153. [Google Scholar] [CrossRef]
- Charalambous, M.; Phylactou, P.; Elriz, T.; Psychogios, L.; Annoni, J.M.; Kambanaros, M. Adaptation of The Scenario Test for Greek-Speaking People with Aphasia: A Reliability and Validity Study. Int. J. Lang. Commun. Disord. 2022, 57, 865–880. [Google Scholar] [CrossRef]
- Wallace, S.J.; Worrall, L.; Rose, T.; Le Dorze, G.; Breitenstein, C.; Hilari, K.; Babbitt, E.; Bose, A.; Brady, M.; Cherney, L.R.; et al. A Core Outcome Set for Aphasia Treatment Research: The ROMA Consensus Statement. Int. J. Stroke 2019, 14, 180–185. [Google Scholar] [CrossRef]
- Wallace, S.J.; Worrall, L.; Rose, T.A.; Alyahya, R.S.W.; Babbitt, E.; Beeke, S.; de Beer, C.; Bose, A.; Bowen, A.; Brady, M.C.; et al. Measuring Communication as a Core Outcome in Aphasia Trials: Results of the ROMA-2 International Core Outcome Set Development Meeting. Int. J. Lang. Commun. Disord. 2023, 58, 1017–1028. [Google Scholar] [CrossRef]
- van der Meulen, I.; van de Sandt-Koenderman, W.; Duivenvoorden, H.; Ribbers, G. Measuring Verbal and Non-Verbal Communication in Aphasia: Reliability, Validity, and Sensitivity to Change of the Scenario Test. Int. J. Lang. Commun. Disord. 2010, 45, 424–435. [Google Scholar] [CrossRef]
- Lomas, J.; Pickard, L.; Bester, S.; Elbard, H.; Finlayson, A.; Zoghaib, C. The Communicative Effectiveness Index: Development and Psychometric Evaluation of a Functional Communication Measure for Adult Aphasia. J. Speech Hear. Disord. 1989, 54, 113–124. [Google Scholar] [CrossRef]
- Penn, C.; Milner, K.; Fridjhon, P. The Communicative Effectiveness Index: Its Use with South African Stroke Patients. S. Afr. J. Commun. Disord. 1992, 39, 74–82. [Google Scholar] [CrossRef]
- Pedersen, P.; Vinter, K.; Olsen, T. The Communicative Effectiveness Index: Psychometric Properties of a Danish Adaptation. Aphasiology 2011, 15, 787–802. [Google Scholar] [CrossRef]
- Moretta, P.; Lanzillo, A.; Sapio, M.D.L.; Spaccavento, S.; Cellamare, F.; Nisoli, F.; Ianni, A.; Pain, D.; Feroldi, S.; Forlani, C.A.; et al. The Italian Validation of the Communicative Effectiveness Index Questionnaire: A Multicentric Study. Neurol. Sci. 2021, 42, 2283–2290. [Google Scholar] [CrossRef]
- Kertesz, A. Western Aphasia Battery; The Psychological Corporation, Harcourt Brace Jovanovich: New York, NY, USA, 1982. [Google Scholar]
- Ciurli, P.; Marangolo, P.; Basso, A. Esame del Linguaggio II; Giunti Organizzazioni Speciali: Firenze, Italy, 1996. [Google Scholar]
- Porch, B.E. Porch Index of Communicative Ability; Consulting Psychologists Press: Washington, DC, USA, 1967. [Google Scholar]
- Katz, S.; Down, T.D.; Cash, H.R.; Grotz, R.C. Progress in the Development of the Index of ADL. Gerontologist 1970, 10, 20–30. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Maryland State Med. J. 1965, 14, 61–65. [Google Scholar]
- Wade, D.T.; Collin, C. The Barthel ADL Index: A Standard Measure of Physical Disability. Int. Disabil. Studies 1988, 10, 64–67. [Google Scholar] [CrossRef]
- Benaim, C.; Cailly, B.; Perennou, D.; Pelissier, J. Validation of the Aphasic Depression Rating Scale. Stroke 2004, 35, 1692–1696. [Google Scholar] [CrossRef]
- Argyle, M.; Cook, M. The Non-Verbal Index of Depression. In Gaze and Mutual Gaze; Argyle, M., Cook, M., Eds.; Cambridge University Press: Cambridge, UK, 1976; pp. 155–162. [Google Scholar]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. *Manual for the Beck Depression Inventory-II; Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Fotiou, C.; Grohmann, K.K. A Small Island With Big Differences? Folk Perceptions in the Context of Dialect Levelling and Koineization. Front. Commun. 2022, 6, 770088. [Google Scholar] [CrossRef]
- Hesketh, A.; Long, A.; Bowen, A.; on behalf of the ACTNoW Research Study. Agreement on Outcome: Speaker, Carer, and Therapist Perspectives on Functional Communication after Stroke. Aphasiology 2011, 25, 291–308. [Google Scholar] [CrossRef]
- Shafer, J.S.; Shafer, P.R.; Haley, K.L. Caregivers Navigating Rehabilitative Care for People with Aphasia after Stroke: A Multi-lens Perspective. Int. J. Lang. Commun. Disord. 2019, 54, 634–644. [Google Scholar] [CrossRef]
- Goering, S. Rethinking Disability: The Social Model of Disability and Chronic Disease. Curr. Rev. Musculoskelet. Med. 2015, 8, 134–138. [Google Scholar] [CrossRef]
- American Geriatrics Society Expert Panel on Person-Centered Care. Person-Centered Care: A Definition and Essential Elements. J. Am. Geriatr. Soc. 2016, 64, 15–18. [Google Scholar] [CrossRef]
- Byng, S.; Duchan, J. Social Model Philosophies and Principles: Their Applications to Therapies for Aphasia. Aphasiology 2005, 19, 906–922. [Google Scholar] [CrossRef]
- World Health Organization (WHO). International Classification of Functioning, Disability, and Health. Available online: https://icd.who.int/dev11/l-icf/en (accessed on 15 April 2024).
- Charalambous, M.; Kountouri, A.; Schwyter, J.R.; Annoni, J.M.; Kambanaros, M. The Development of the People with Aphasia and Other Layperson Involvement (PAOLI) Framework for Guiding Patient and Public Involvement (PPI) in Aphasia Research. Res. Involv. Engagem. 2023, 9, 74. [Google Scholar] [CrossRef]
- Sharma, T.; Bamford, M.; Dodman, D. Person-Centered Care: An Overview of Reviews. Contemp. Nurse 2015, 51, 107–120. [Google Scholar] [CrossRef]
- Shiggins, C.; Coe, D.; Gilbert, L.; Collaboration Aphasia; Mares, K. Development of an “Aphasia-Accessible Participant in Research Experience Survey” through Co-Production. Aphasiology 2022, 1–34. [Google Scholar] [CrossRef]
- Carragher, M.; Steel, G.; O’Halloran, R.; Lamborn, E.; Torabi, T.; Johnson, H.; Rose, M.L. Aphasia Disrupts Usual Care: “I’m Not Mad, I’m Not Deaf”—The Experiences of Individuals with Aphasia and Family Members in Hospital. Disabil. Rehabil. 2024, 5, 1–12. [Google Scholar] [CrossRef]
- Ranganai, E.; Matizirofa, L. An Analysis of Recent Stroke Cases in South Africa: Trend, Seasonality and Predictors. S. Afr. Med. J. 2020, 110, 92–99. [Google Scholar] [CrossRef]
- Krueger, H.; Koot, J.; Hall, R.E.; O’Callaghan, C.; Bayley, M.; Corbett, D. Prevalence of Individuals Experiencing the Effects of Stroke in Canada: Trends and Projections. Stroke 2015, 46, 2226–2231. [Google Scholar] [CrossRef] [PubMed]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Messinis, L.; Panagea, E.; Papathasopoulos, P.; Kastellakis, A. Boston Diagnostic Aphasia Examination-Short Form in Greek Language; Gotsis: Patras, Greece, 2013. [Google Scholar]
- Michopoulos, I.; Douzenis, A.; Kalkavoura, C.; Christodoulou, C.; Michalopoulou, P.; Kalemi, G.; Fineti, K.; Patapis, P.; Protopapas, K.; Lykouras, L. Hospital Anxiety and Depression Scale (HADS): Validation in a Greek General Hospital Sample. Ann. Gen. Psychiatry 2008, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Charalambous, M.; Phylactou, P.; Kountouri, A.; Serafeim, M.; Psychogios, L.; Annoni, J.-M.; Kambanaros, M. Adaptation of the Aphasia Impact Questionnaire-21 into Greek: A Reliability and Validity Study. Clin. Transl. Neurosci. 2022, 6, 24. [Google Scholar] [CrossRef]
- Swinburn, K.; Best, W.; Beeke, S.; Cruice, M.; Smith, L.; Willis, E.P.; Ledingham, K.; Sweeney, J.; McVicker, S.J. A Concise Patient-Reported Outcome Measure for People with Aphasia: The Aphasia Impact Questionnaire 21. Aphasiology 2018, 33, 1035–1060. [Google Scholar] [CrossRef]
- Hilari, K.; Galante, L.; Huck, A.; Pritchard, M.; Allen, L.; Dipper, L. Cultural Adaptation and Psychometric Testing of The Scenario Test UK for People with Aphasia. Int. J. Lang. Commun. Disord. 2018, 53, 748–760. [Google Scholar] [CrossRef]
- Doedens, W.J.; Meteyard, L. Measures of Functional, Real-World Communication for Aphasia: A Critical Review. Aphasiology 2019, 34, 1–23. [Google Scholar] [CrossRef]
- Schumacher, R.; Bruehl, S.; Halai, A.D.; Lambon Ralph, M.A. The Verbal, Non-Verbal and Structural Bases of Functional Communication Abilities in Aphasia. Brain Commun. 2020, 2, fcaa118. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Prinsen, C.A.C.; Chiarotto, A.; Westerman, M.J.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Mokkink, L.B. COSMIN Methodology for Evaluating the Content Validity of Patient-Reported Outcome Measures: A Delphi Study. Qual. Life Res. 2018, 27, 1159–1170. [Google Scholar] [CrossRef]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Streiner, D.; Norman, G.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Akoglu, H. User’s Guide to Correlation Coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Phylactou, P.; Papadatou-Pastou, M.; Konstantinou, N. The Bayesian One-sample t-Test Supersedes Cor-relation Analysis as a Test of Validity. PsyArXiv 2022. [Google Scholar] [CrossRef]
- Crockford, C.; Lesser, R. Assessing Functional Communication in Aphasia: Clinical Utility and Time Demands of Three Methods. Int. J. Lang. Commun. Disord. 1994, 29, 165–182. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, S.; Xu, S.; Wang, Y.; Jin, X.; Wan, P.; Sun, J.; Tao, J.; Zhang, S.; Zhang, G.; et al. Augmentative and Alternative Communication Intervention for In-Patient Individuals with Post-Stroke Aphasia: Study Protocol of a Parallel-Group, Pragmatic Randomized Controlled Trial. Trials 2021, 22, 837. [Google Scholar] [CrossRef] [PubMed]
- Shewan, C.M.; Kertesz, A. Reliability and Validity Characteristics of the Western Aphasia Battery (WAB). J. Speech Hear. Disord. 1980, 45, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Azios, J.H.; Strong, K.A.; Archer, B.; Douglas, N.F.; Simmons-Mackie, N.; Worrall, L. Friendship Matters: A Research Agenda for Aphasia. Aphasiology 2021, 36, 317–336. [Google Scholar] [CrossRef]
- Olsson, C.; Arvidsson, P.; Blom Johansson, M. Relations between Executive Function, Language, and Functional Communication in Severe Aphasia. Aphasiology 2019, 33, 821–845. [Google Scholar] [CrossRef]
- Grawburg, M.; Howe, T.; Worrall, L.; Scarinci, N. Third-Party Disability in Family Members of People with Aphasia: A Systematic Review. Disabil. Rehabil. 2013, 35, 1324–1341. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.B.; Carlsson, M.; Sonnander, K. Communication Difficulties and the Use of Communication Strategies: From the Perspective of Individuals with Aphasia. Int. J. Lang. Commun. Disord. 2012, 47, 144–155. [Google Scholar] [CrossRef]
- Fromm, D.; Holland, A.; Armstrong, E.; Forbes, M.; Macwhinney, B.; Risko, A.; Mattison, N. “Better But No Cigar”: Persons with Aphasia Speak about their Speech. Aphasiology 2011, 25, 1431–1447. [Google Scholar] [CrossRef][Green Version]
- Dalemans, R.J.; de Witte, L.; Wade, D.; van den Heuvel, W. Social Participation through the Eyes of People with Aphasia. Int. J. Lang. Commun. Disord. 2010, 45, 537–550. [Google Scholar] [CrossRef]
- Braley, M.; Pierce, J.; Saxena, S.; Oliveira, E.; Taraboanta, L.; Anantha, V.; Lakhan, S.; Kiran, S. A Virtual, Randomized, Control Trial of a Digital Therapeutic for Speech, Language, and Cognitive Intervention in Post-stroke Persons with Aphasia. Front. Neurol. 2021, 12, 626780. [Google Scholar] [CrossRef]
- Fox, L.; Poulsen, S.; Bawden, K.; Packard, D. Critical Elements and Outcomes of a Residential Family-Based Intervention for Aphasia Carers. Aphasiology 2004, 18, 1177–1199. [Google Scholar] [CrossRef]
- Hachioui, H.; Lingsma, H.; Sandt-Koenderman, M.; Dippel, D.; Koudstaal, P.; Visch-Brink, E. Long-term Prognosis of Aphasia after Stroke. J. Neurol. Neurosurg. Psychiatry 2012, 84, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Nichol, L.; Wallace, S.J.; Pitt, R.; Rodriguez, A.D.; Diong, Z.Z.; Hill, A.J. People with Aphasia Share Their Views on Self-Management and the Role of Technology to Support Self-Management of Aphasia. Disabil. Rehabil. 2022, 44, 7399–7412. [Google Scholar] [CrossRef]
| CETI Version | English | South African | Danish | Italian |
|---|---|---|---|---|
| Participants (n) | 33 | 56 | 68 | 136 |
| PWA (n) | 22 | 22 | 68 | 68 |
| Stroke no aphasia (n) | - | 6 | - | - |
| Carers (n) | 11 | 28 | - | 68 |
| Psychometric Properties | ||||
| Reliability | ||||
| Internal consistency | + | + | + | + |
| Test–retest | + | + | + | + |
| Inter-rater | + | - | + | + |
| Validity | ||||
| Construct | + | - | + | + |
| Convergent | + | - | + | + |
| Tools | ||||
| Language | ||||
| Western Aphasia Battery (WAB) [14] | + | - | + | - |
| Brief Exam of Language Impairment-II [15] | - | - | - | + |
| Functional Communication | ||||
| Speech Questionnaire (SQ) of the WAB [14] | + | - | + | - |
| Porch Index of Communicative Ability (PICA) [16] | - | - | + | - |
| Activities of Daily Living | ||||
| Activities of Daily Living scale (ADL) [17] | - | - | - | + |
| Activities of Daily Living scale (IADL) [18] | - | - | - | + |
| Barthel Index (BI) [19] | - | - | + | - |
| Frenchay Activity Index (FAI) [20] | - | - | + | - |
| Depression | ||||
| Aphasic Depression Rating Scale (ADRS) [21] | - | - | - | + |
| Non-Verbal Index of Depression (NID) [22] | - | - | + | - |
| Beck Depression Inventory (BDI) [23,24] | - | - | + | - |
| Country | Population | Incidence Estimate | CETI Sample Size (n) + [Study] |
|---|---|---|---|
| Canada | 39,034,588 | 50,000 strokes/year | n = 33 [10] 22 PWA + 11 carers |
| South Africa | 54,956,900 | 120,000 strokes/year | n = 56 [11] 28 PWA + 28 carers |
| Denmark | 5,368,854 | 5297 strokes/year | n = 68 PWA [12] |
| Italy | 60,665,625 | 73,116 strokes/year | n = 136 [13] 68 PWA + 68 carers |
| Cyprus | 803,147 | 564 strokes/year | n = 60 (current study) 30 PWA + 30 carers |
| Characteristics | People with Aphasia (n = 30) | Carers (n = 30) |
|---|---|---|
| Gender | ||
| Male | 16 (47%) | 7 (77%) |
| Female | 14 (53%) | 23 (23%) |
| Age | ||
| Mean (sd) | 67.67 (10.71) | 47.4 (16.33) |
| Min–Max | 36–89 | 26–78 |
| Stroke Type | ||
| Ischemic | 15 (50%) | N/A |
| Hemorrhagic | 12 (40%) | N/A |
| Other | 3 (10%) | N/A |
| Lesion Location | ||
| Left | 15 (50%) | N/A |
| Right | 15 (50%) | N/A |
| Hemiplegia | ||
| Left | 8 (27%) | N/A |
| Right | 10 (33%) | N/A |
| None | 12 (40%) | N/A |
| Months Post Stroke Diagnosis | ||
| Mean (sd) | 44.07 (48.81) | N/A |
| Min–Max | 6–180 | N/A |
| Completed Education | ||
| Primary | 4 (13%) | 0 |
| Secondary | 19 (63%) | 7 (23%) |
| College | 0 | 4 (13%) |
| Bachelor’s | 5 (17%) | 8 (27%) |
| Master’s | 2 (7%) | 9 (30%) |
| PhD | 0 | 2 (7%) |
| Marital Status | ||
| Married | 13 (43%) | 16 (53%) |
| Single | 5 (17%) | 11 (37%) |
| Divorced | 4 (13%) | 1 (3%) |
| Widowed | 8 (23%) | 2 (7%) |
| Socioeconomic Status Based on Former or Current Occupation | ||
| Higher managerial, e.g., chief executive officer | 3 (10%) | 6 (20%) |
| Intermediate occupation, e.g., clerical, sales, service | 5 (16%) | 16 (53%) |
| Manual occupation, e.g., painter, builder | 14 (47%) | 6 (20%) |
| Unemployed | 8 (27%) | 2 (7%) |
| Group | Mean | sd | Minimum | Maximum | |
|---|---|---|---|---|---|
| ASRS | PWA | 3.3 | 1.58 | 1 | 5 |
| Carer | - | - | - | - | |
| CETI-GR | PWA | 74.49 | 17.92 | 25.63 | 97.19 |
| Carer | 65.71 | 25.6 | 18.44 | 98.75 | |
| AIQ-21-GR | PWA | 23.43 | 14 | 0 | 47 |
| Carer | 30.63 | 13.62 | 6 | 52 | |
| Scenario Test-GR | PWA | 38.2 | 19.05 | 0 | 54 |
| Carer | - | - | - | - | |
| HADS-GR | PWA | 11.67 | 6.39 | 3 | 25 |
| Carer | - | - | - | - |
| Percentiles | ||||
|---|---|---|---|---|
| Group | Median | 25th | 75th | |
| Importance | PWA | 4.5 | 4.38 | 4.63 |
| SNA | 4 | 4 | 4.25 | |
| Professional Carers | 4 | 4 | 4.25 | |
| Family Carers | 4 | 4 | 4.25 | |
| Comprehensiveness | PWA | 5 | 5 | 5 |
| SNA | 4 | 4 | 4.25 | |
| Professional Carers | 4 | 4 | 4.25 | |
| Family Carers | 4 | 4 | 4.25 | |
| Relevance | PWA | 5 | 4.75 | 5 |
| SNA | 4 | 4 | 4.25 | |
| Professional Carers | 4 | 4 | 4.25 | |
| Family Carers | 4 | 4 | 4.25 | |
| Appropriateness | PWA | 5 | 4.75 | 5 |
| SNA | 4 | 4 | 4.25 | |
| Professional Carers | 4 | 4 | 4.25 | |
| Family Carers | 4 | 4 | 4.25 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charalambous, M.; Phylactou, P.; Antoniou, E.; Christodoulou, M.; Kambanaros, M. The Adaptation of the Communicative Effectiveness Index (CETI) into Greek: A Reliability and Validity Study. Brain Sci. 2024, 14, 689. https://doi.org/10.3390/brainsci14070689
Charalambous M, Phylactou P, Antoniou E, Christodoulou M, Kambanaros M. The Adaptation of the Communicative Effectiveness Index (CETI) into Greek: A Reliability and Validity Study. Brain Sciences. 2024; 14(7):689. https://doi.org/10.3390/brainsci14070689
Chicago/Turabian StyleCharalambous, Marina, Phivos Phylactou, Eleftheria Antoniou, Maria Christodoulou, and Maria Kambanaros. 2024. "The Adaptation of the Communicative Effectiveness Index (CETI) into Greek: A Reliability and Validity Study" Brain Sciences 14, no. 7: 689. https://doi.org/10.3390/brainsci14070689
APA StyleCharalambous, M., Phylactou, P., Antoniou, E., Christodoulou, M., & Kambanaros, M. (2024). The Adaptation of the Communicative Effectiveness Index (CETI) into Greek: A Reliability and Validity Study. Brain Sciences, 14(7), 689. https://doi.org/10.3390/brainsci14070689







