Potential Role of Superoxide Dismutase 3 (SOD3) in Resistance to Influenza A Virus Infection
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cells and Viruses
2.2. Plasmids
2.3. Antibodies
2.4. Viral Infection
2.5. ROS Measurement
2.6. Plaque Assay
2.7. Determination of Malondialdehyde (MDA) and Superoxide Dismutase (SOD) Detection
2.8. The Activity of NOX Oxidase
2.9. siRNA Transfection
2.10. SOD3 Overexpression
2.11. Quantitative Real-Time PCR (qRT-PCR)
2.12. Western Blotting
2.13. Immunofluorescence Staining
2.14. Mini-Replicon Assay
2.15. Apoptosis Detection
2.16. SOD3 Expression In Vivo
2.17. Statistical Analysis
3. Results
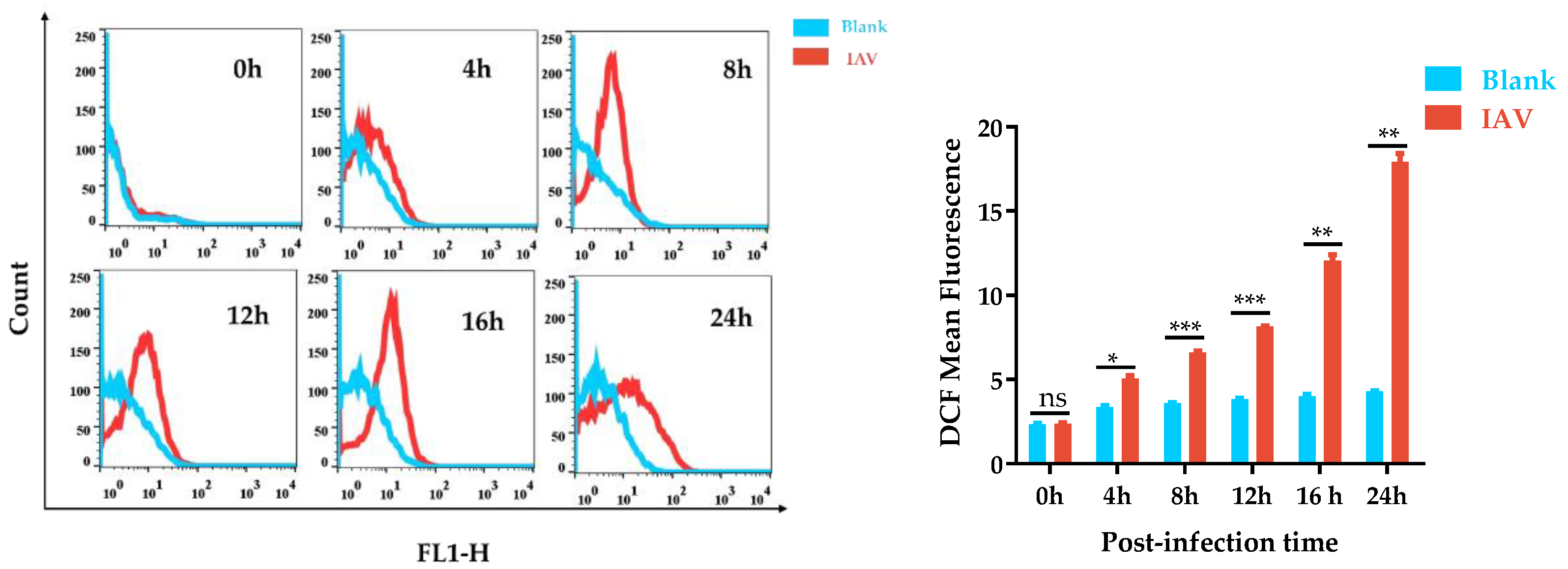
3.1. ROS Production by IAV-Stimulated A549 Cells Was Time-Dependent
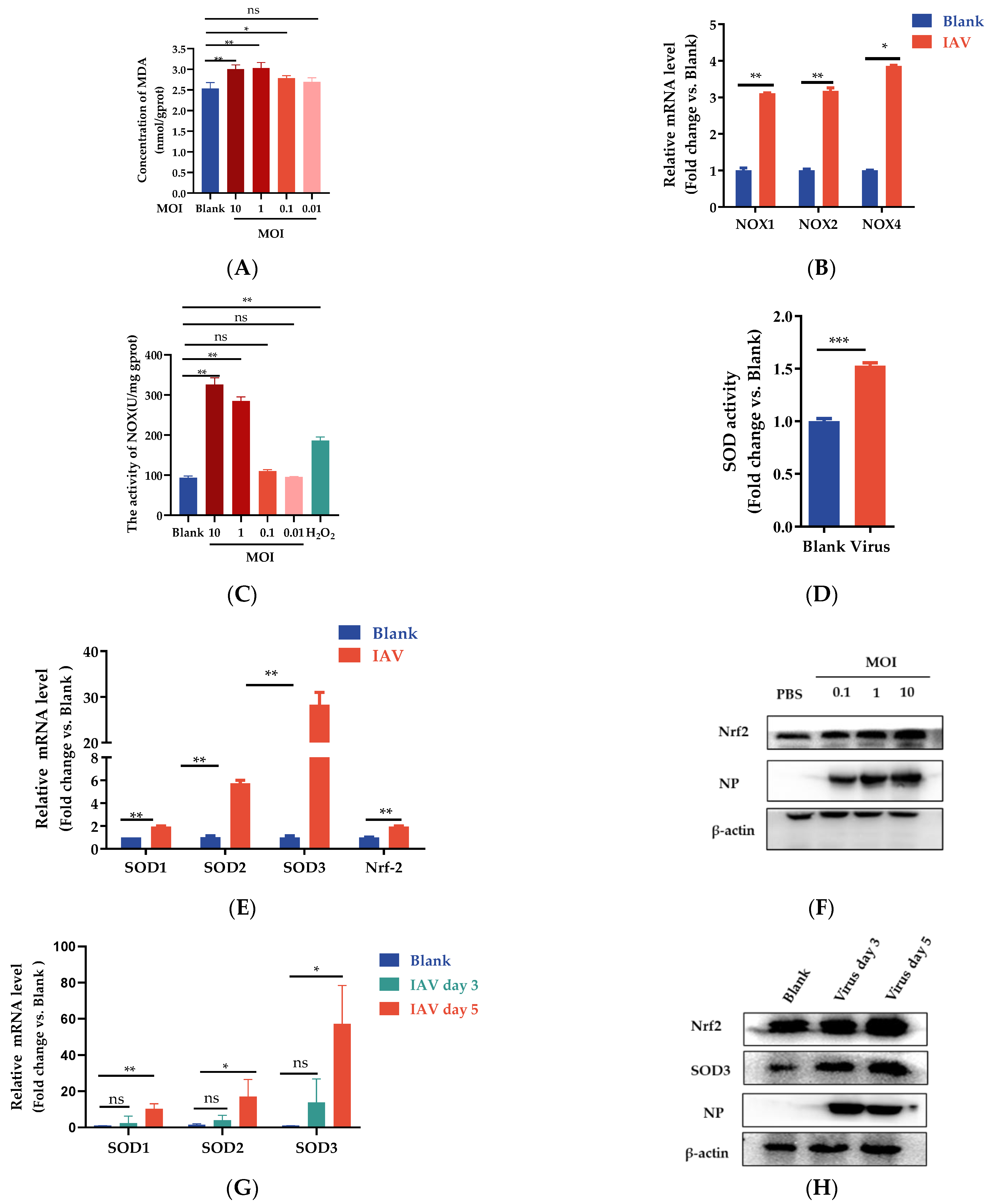
3.2. IAV Infection Induces Oxidative Stress and Decreases Antioxidant Enzyme Activities
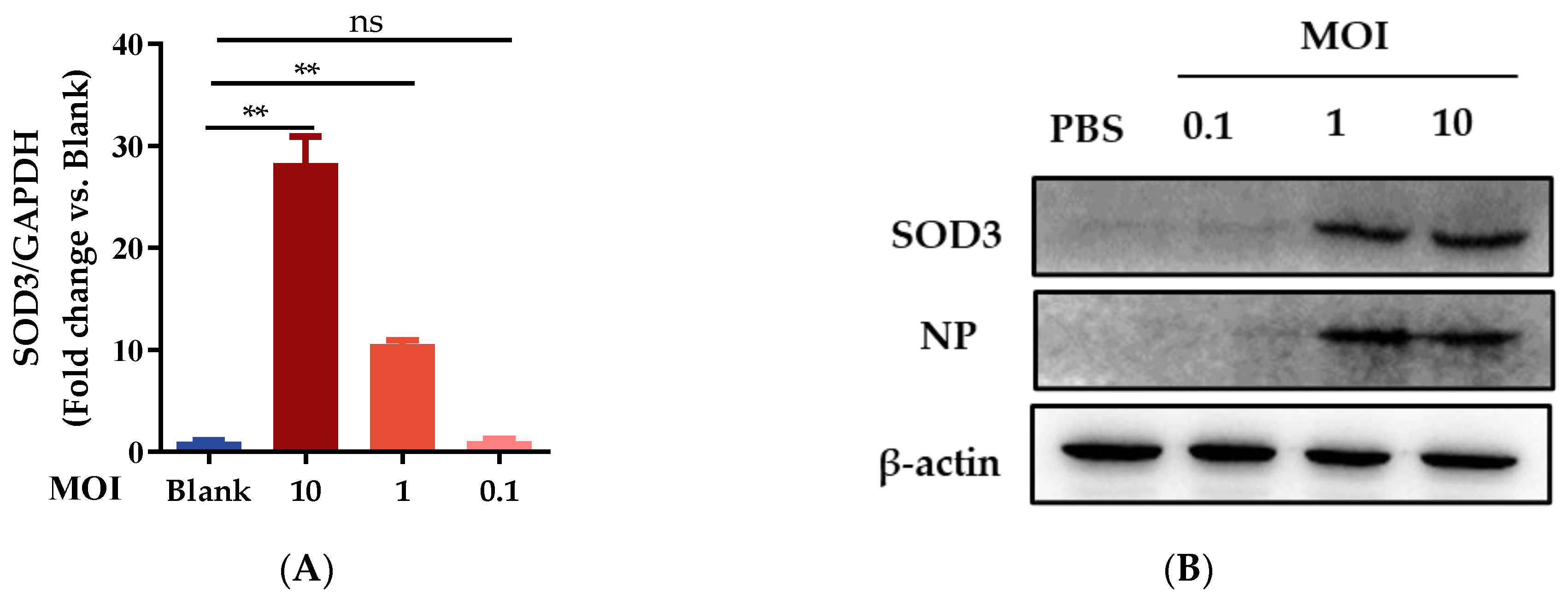
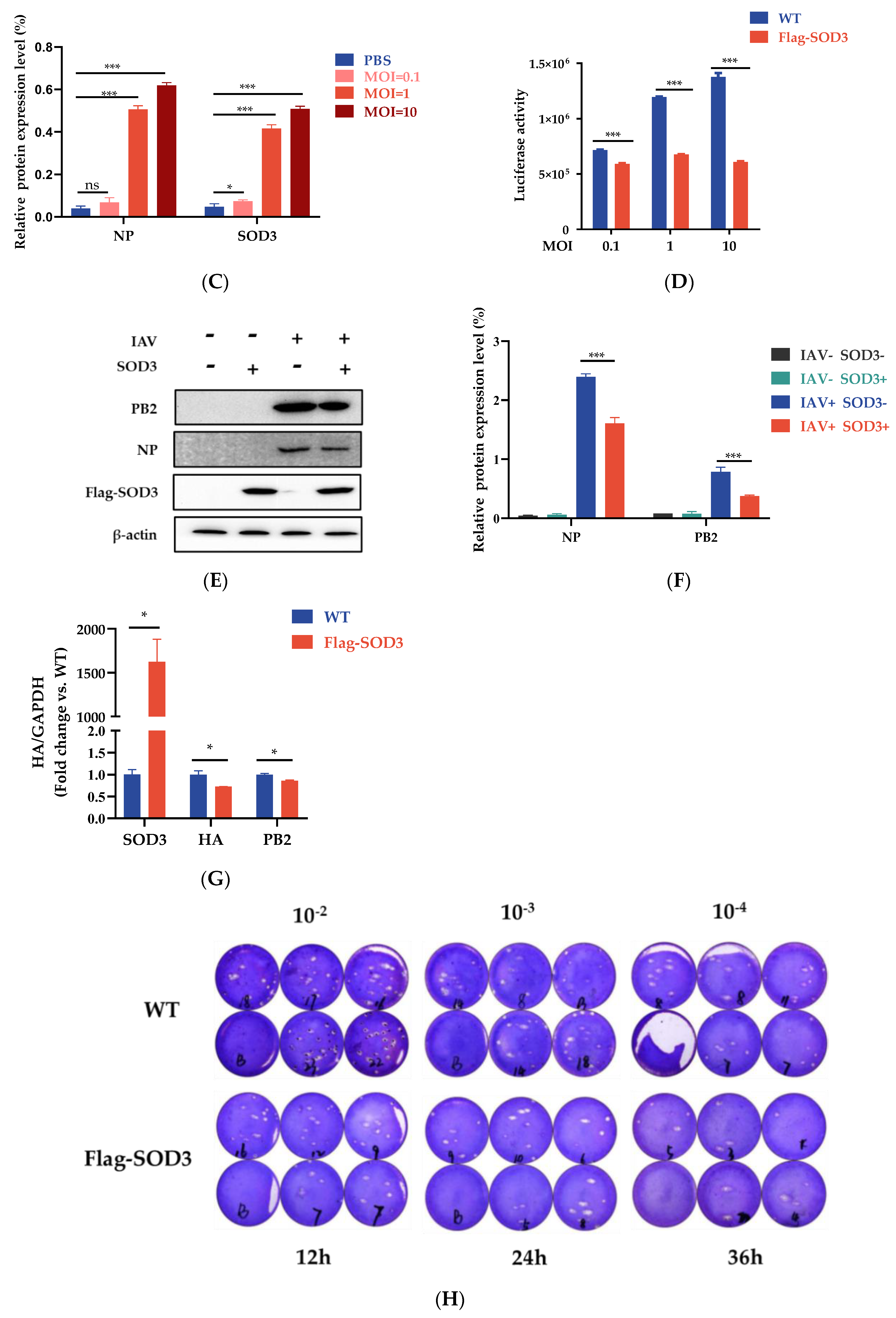
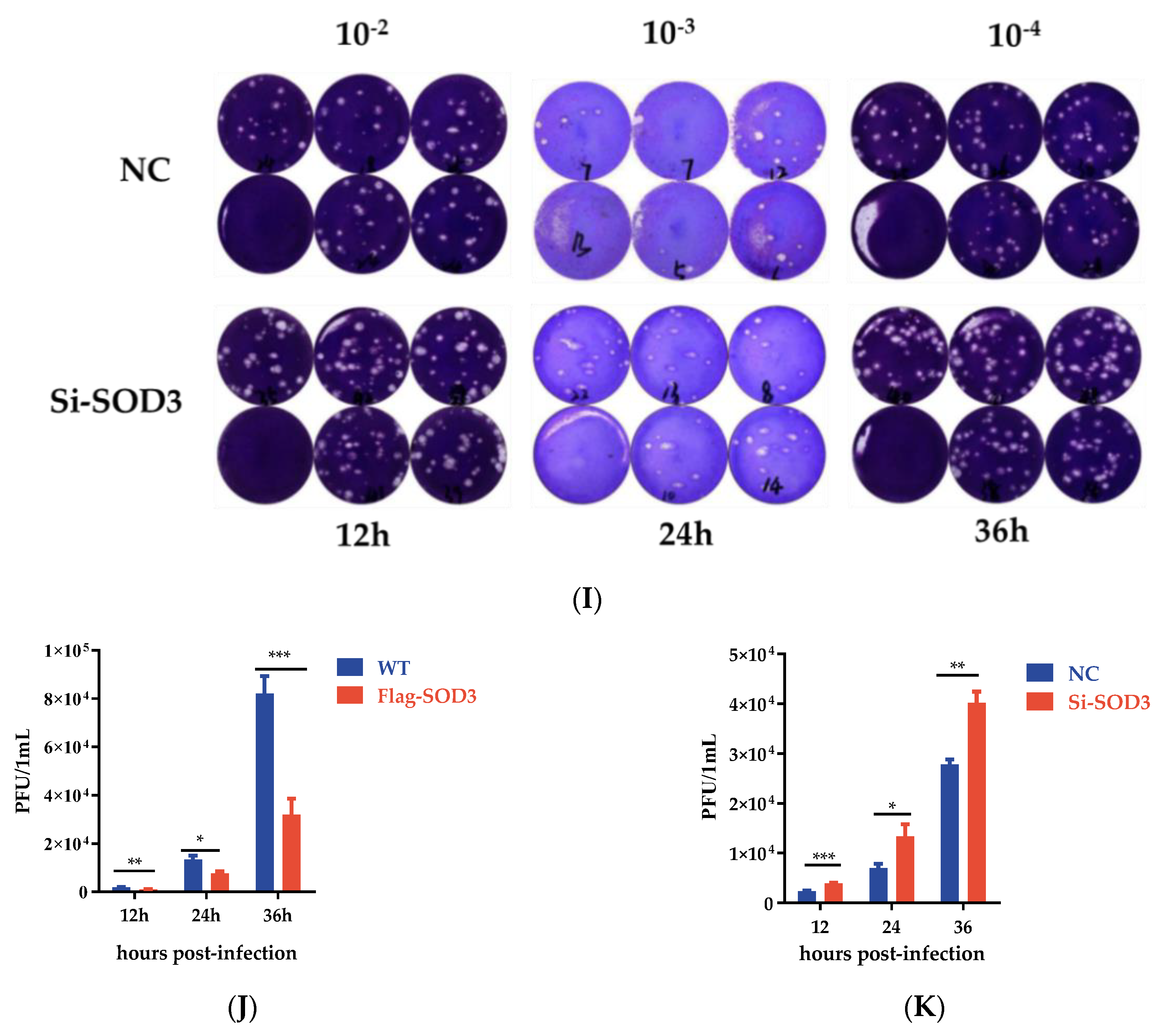
3.3. SOD3 Disrupted IAV Replication in A549 Cells
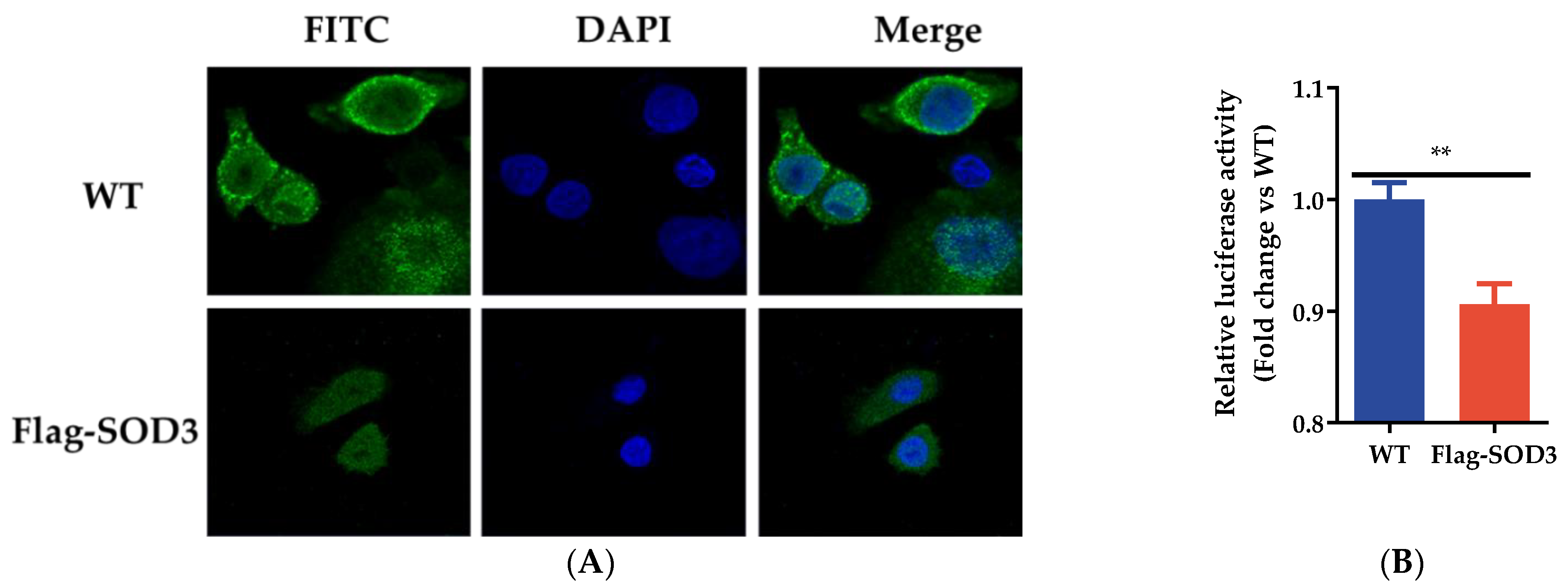
3.4. SOD3 Disrupted IAV Replication by Impairing the Synthesis of Viral RNA
3.5. Effects of SOD3 on ROS Production in IAV-Induced A549 Cells
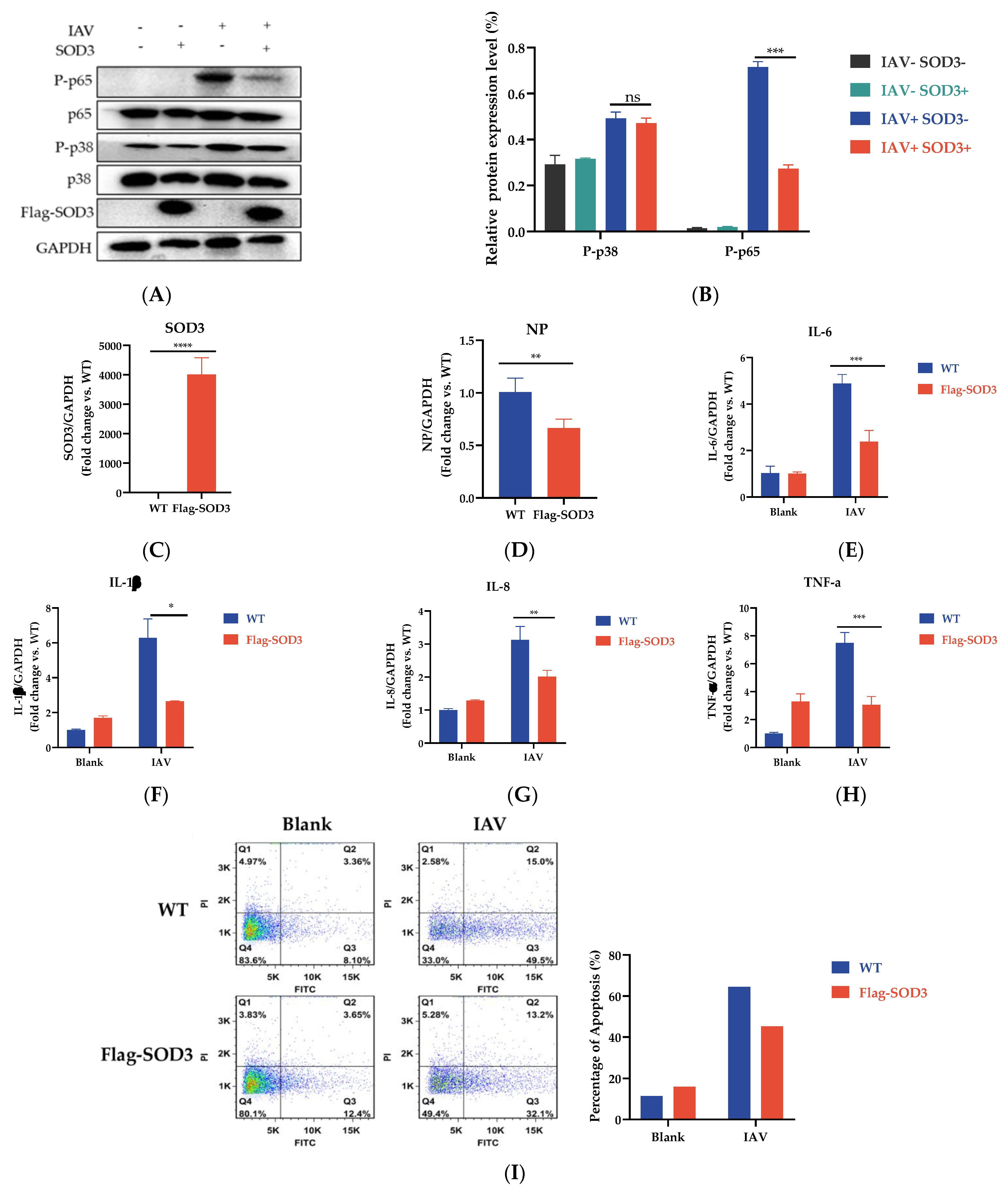
3.6. SOD3 Overexpression Reduced Cellular Inflammation and Apoptosis Induced by IAV
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Cumulative Number of Confirmed Human Cases of Avian Influenza A(H5N1) Reported to WHO; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Su, S.; Gu, M.; Liu, D.; Cui, J.; Gao, G.F.; Zhou, J.; Liu, X. Epidemiology, Evolution, and Pathogenesis of H7N9 Influenza Viruses in Five Epidemic Waves since 2013 in China. Trends Microbiol. 2017, 25, 713–728. [Google Scholar] [CrossRef]
- Gounder, A.P.; Boon, A.C.M. Influenza Pathogenesis: The Effect of Host Factors on Severity of Disease. J. Immunol. 2019, 202, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Meineke, R.; Rimmelzwaan, G.F.; Elbahesh, H. Influenza Virus Infections and Cellular Kinases. Viruses 2019, 11, 171. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Chen, F.; Liu, T.; Chen, F.; Liu, S.; Yang, J. The role of oxidative stress in influenza virus infection. Microbes Infect. 2017, 19, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, K.B. Oxidative stress during viral infection: A review. Free. Radic. Biol. Med. 1996, 21, 641–649. [Google Scholar] [CrossRef]
- Hosakote, Y.M.; Liu, T.; Castro, S.M.; Garofalo, R.P.; Casola, A. Respiratory Syncytial Virus Induces Oxidative Stress by Modulating Antioxidant Enzymes. Am. J. Respir. Cell Mol. Biol. 2009, 41, 348–357. [Google Scholar] [CrossRef] [PubMed]
- Pal, S.; Polyak, S.J.; Bano, N.; Qiu, W.C.; Carithers, R.L.; Shuhart, M.; Gretch, D.R.; Das, A. Hepatitis C virus induces oxidative stress, DNA damage and modulates the DNA repair enzyme NEIL1. J. Gastroenterol. Hepatol. 2010, 25, 627–634. [Google Scholar] [CrossRef]
- Akaike, T.; Noguchi, Y.; Ijiri, S.; Setoguchi, K.; Suga, M.; Zheng, Y.M.; Dietzschold, B.; Maeda, H. Pathogenesis of influenza virus-induced pneumonia: Involvement of both nitric oxide and oxygen radicals. Proc. Natl. Acad. Sci. USA 1996, 93, 2448–2453. [Google Scholar] [CrossRef]
- Suhail, S.; Zajac, J.; Fossum, C.; Lowater, H.; McCracken, C.; Severson, N.; Laatsch, B.; Narkiewicz-Jodko, A.; Johnson, B.; Liebau, J.; et al. Role of Oxidative Stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) Infection: A Review. Protein J. 2020, 39, 644–656. [Google Scholar] [CrossRef]
- Bresciani, G.; da Cruz, I.B.M.; González-Gallego, J. Manganese Superoxide Dismutase and Oxidative Stress Modulation. Adv. Clin. Chem. 2015, 68, 87–130. [Google Scholar] [CrossRef]
- Wang, X.-L.; Jiang, R.-W. Therapeutic Potential of Superoxide Dismutase Fused with Cell-Penetrating Peptides in Oxidative Stress-Related Diseases. Mini-Rev. Med. Chem. 2022, 22, 2287–2298. [Google Scholar] [CrossRef] [PubMed]
- Culotta, V.C. Superoxide dismutase, oxidative stress, and cell metabolism. Curr. Top. Cell. Regul. 2001, 36, 117–132. [Google Scholar] [CrossRef]
- Camini, F.C.; Caetano, C.C.D.S.; Almeida, L.T.; Guerra, J.F.D.C.; Silva, B.D.M.; Silva, S.D.Q.; de Magalhães, J.C.; Magalhães, C.L.D.B. Oxidative stress in Mayaro virus infection. Virus Res. 2017, 236, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, A.; Popova, T.; Turell, M.; Kidd, J.; Chertow, J.; Popov, S.G.; Bailey, C.; Kashanchi, F.; Kehn-Hall, K. Alteration in Superoxide Dismutase 1 Causes Oxidative Stress and p38 MAPK Activation Following RVFV Infection. PLoS ONE 2011, 6, e20354. [Google Scholar] [CrossRef] [PubMed]
- Griess, B.; Tom, E.; Domann, F.; Teoh-Fitzgerald, M. Extracellular superoxide dismutase and its role in cancer. Free. Radic. Biol. Med. 2017, 112, 464–479. [Google Scholar] [CrossRef]
- Dhar, S.K.; Clair, D.K.S. Manganese superoxide dismutase regulation and cancer. Free. Radic. Biol. Med. 2012, 52, 2209–2222. [Google Scholar] [CrossRef]
- Lin, X.; Wang, R.; Zou, W.; Sun, X.; Liu, X.; Zhao, L.; Wang, S.; Jin, M. The Influenza Virus H5N1 Infection Can Induce ROS Production for Viral Replication and Host Cell Death in A549 Cells Modulated by Human Cu/Zn Superoxide Dismutase (SOD1) Overexpression. Viruses 2016, 8, 13. [Google Scholar] [CrossRef]
- Zelko, I.N.; Mariani, T.J.; Folz, R.J. Superoxide dismutase multigene family: A comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free. Radic. Biol. Med. 2002, 33, 337–349. [Google Scholar] [CrossRef]
- Borgstahl, G.E.O.; Oberley-Deegan, R.E. Superoxide Dismutases (SODs) and SOD Mimetics. Antioxidants 2018, 7, 156. [Google Scholar] [CrossRef]
- Laurila, J.P.; Castellone, M.D.; Curcio, A.; Laatikainen, L.E.; Haaparanta-Solin, M.; Gronroos, T.J.; Marjamaki, P.; Martikainen, S.; Santoro, M.; Laukkanen, M.O. Extracellular Superoxide Dismutase Is a Growth Regulatory Mediator of Tissue Injury Recovery. Mol. Ther. 2009, 17, 448–454. [Google Scholar] [CrossRef]
- Folz, R.J.; Abushamaa, A.M.; Suliman, H.B. Extracellular superoxide dismutase in the airways of transgenic mice reduces inflammation and attenuates lung toxicity following hyperoxia. J. Clin. Investig. 1999, 103, 1055–1066. [Google Scholar] [CrossRef] [PubMed]
- Laukkanen, M.O.; Leppanen, P.; Turunen, P.; Tuomisto, T.; Naarala, J.; Yla-Herttuala, S. EC-SOD gene therapy reduces paracetamol-induced liver damage in mice. J. Gene Med. 2001, 3, 321–325. [Google Scholar] [CrossRef]
- Mouradian, G.C.; Gaurav, R.; Pugliese, S.; El Kasmi, K.; Hartman, B.; Hernandez-Lagunas, L.; Stenmark, K.R.; Bowler, R.P.; Nozik-Grayck, E. Superoxide Dismutase 3 R213G Single-Nucleotide Polymorphism Blocks Murine Bleomycin-Induced Fibrosis and Promotes Resolution of Inflammation. Am. J. Respir. Cell Mol. Biol. 2017, 56, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Eruslanov, E.; Kusmartsev, S. Identification of ROS Using Oxidized DCFDA and Flow-Cytometry. Methods Inmolecularbiol. 2010, 594, 57–72. [Google Scholar] [CrossRef]
- Sang, H.; Huang, Y.; Tian, Y.; Liu, M.; Chen, L.; Li, L.; Liu, S.; Yang, J. Multiple modes of action of myricetin in influenza A virus infection. Phytother. Res. 2021, 35, 2797–2806. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Li, R.; Li, X.; He, J.; Jiang, S.; Liu, S.; Yang, J. Quercetin as an Antiviral Agent Inhibits Influenza A Virus (IAV) Entry. Viruses 2015, 8, 6. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Xin, Z.-T.; Liang, Y.; Ly, H.; Liang, Y. NF-κB Signaling Differentially Regulates Influenza Virus RNA Synthesis. J. Virol. 2008, 82, 9880–9889. [Google Scholar] [CrossRef]
- Li, R.; Liu, T.; Liu, M.; Chen, F.; Liu, S.; Yang, J. Anti-influenza A Virus Activity of Dendrobine and Its Mechanism of Action. J. Agric. Food Chem. 2017, 65, 3665–3674. [Google Scholar] [CrossRef]
- Janero, D.R. Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of lipid peroxidation and peroxidative tissue injury. Free Radic. Biol. Med. 1990, 9, 515–540. [Google Scholar] [CrossRef]
- Drummond, G.R.; Selemidis, S.; Griendling, K.K.; Sobey, C.G. Combating oxidative stress in vascular disease: NADPH oxidases as therapeutic targets. Nat. Rev. Drug Discov. 2011, 10, 453–471. [Google Scholar] [CrossRef] [Green Version]
- Vermot, A.; Petit-Härtlein, I.; Smith, S.; Fieschi, F. NADPH Oxidases (NOX): An Overview from Discovery, Molecular Mechanisms to Physiology and Pathology. Antioxidants 2021, 10, 890. [Google Scholar] [CrossRef] [PubMed]
- Aldini, G.; Altomare, A.; Baron, G.; Vistoli, G.; Carini, M.; Borsani, L.; Sergio, F. N-Acetylcysteine as an antioxidant and disulphide breaking agent: The reasons why. Free. Radic. Res. 2018, 52, 751–762. [Google Scholar] [CrossRef] [PubMed]
- Haidari, M.; Ali, M.; Casscells, S.W.; Madjid, M. Pomegranate (Punica granatum) purified polyphenol extract inhibits influenza virus and has a synergistic effect with oseltamivir. Phytomedicine 2009, 16, 1127–1136. [Google Scholar] [CrossRef] [PubMed]
- Rushworth, G.F.; Megson, I.L. Existing and potential therapeutic uses for N-acetylcysteine: The need for conversion to intracellular glutathione for antioxidant benefits. Pharmacol. Ther. 2014, 141, 150–159. [Google Scholar] [CrossRef]
- Pinto, R.; Herold, S.; Cakarova, L.; Hoegner, K.; Lohmeyer, J.; Planz, O.; Pleschka, S. Inhibition of influenza virus-induced NF-kappaB and Raf/MEK/ERK activation can reduce both virus titers and cytokine expression simultaneously in vitro and in vivo. Antivir. Res. 2011, 92, 45–56. [Google Scholar] [CrossRef]
- Börgeling, Y.; Schmolke, M.; Viemann, D.; Nordhoff, C.; Roth, J.; Ludwig, S. Inhibition of p38 Mitogen-activated Protein Kinase Impairs Influenza Virus-induced Primary and Secondary Host Gene Responses and Protects Mice from Lethal H5N1 Infection. J. Biol. Chem. 2014, 289, 13–27. [Google Scholar] [CrossRef]
- Zhu, X.-W.; Ding, K.; Dai, X.-Y.; Ling, W.-Q. β-aminoisobutyric acid accelerates the proliferation and differentiation of MC3T3-E1 cells via moderate activation of ROS signaling. J. Chin. Med. Assoc. 2018, 81, 611–618. [Google Scholar] [CrossRef]
- Shi, X.-L.; Shi, Z.-H.; Huang, H.; Zhu, H.-G.; Zhou, P.; Ju, D. Therapeutic Effect of Recombinant Human Catalase on H1N1 Influenza-induced Pneumonia in Mice. Inflammation 2009, 33, 166–172. [Google Scholar] [CrossRef]
- Jacoby, D.; Choi, A.M. Influenza virus induces expression of antioxidant genes in human epithelial cells. Free. Radic. Biol. Med. 1994, 16, 821–824. [Google Scholar] [CrossRef]
- Knobil, K.; Choi, A.M.K.; Weigand, G.W.; Jacoby, D.B. Role of oxidants in influenza virus-induced gene expression. Am. J. Physiol. Cell. Mol. Physiol. 1998, 274, L134–L142. [Google Scholar] [CrossRef]
- Suliman, H.B.; Ryan, L.K.; Bishop, L.; Folz, R.J. Prevention of influenza-induced lung injury in mice overexpressing extracellular superoxide dismutase. Am. J. Physiol. Cell. Mol. Physiol. 2001, 280, L69–L78. [Google Scholar] [CrossRef]
- Chang, S.; Sun, D.; Liang, H.; Wang, J.; Li, J.; Guo, L.; Wang, X.; Guan, C.; Boruah, B.M.; Yuan, L.; et al. Cryo-EM Structure of Influenza Virus RNA Polymerase Complex at 4.3 Å Resolution. Mol. Cell 2015, 57, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.-Y.; Tang, Y.-S.; Shaw, P.-C. Structure and Function of Influenza Virus Ribonucleoprotein. Virus Protein Nucl. Complexes 2018, 88, 95–128. [Google Scholar] [CrossRef]
- Gangehei, L.; Ali, M.; Zhang, W.; Chen, Z.; Wakame, K.; Haidari, M. Oligonol a low molecular weight polyphenol of lychee fruit extract inhibits proliferation of influenza virus by blocking reactive oxygen species-dependent ERK phosphorylation. Phytomedicine 2010, 17, 1047–1056. [Google Scholar] [CrossRef]
- Pflug, A.; Lukarska, M.; Resa-Infante, P.; Reich, S.; Cusack, S. Structural insights into RNA synthesis by the influenza virus transcription-replication machine. Virus Res. 2017, 234, 103–117. [Google Scholar] [CrossRef]
- Walker, A.P.; Sharps, J.; Fodor, E. Mutation of an Influenza Virus Polymerase 3′ RNA Promoter Binding Site Inhibits Transcription Elongation. J. Virol. 2020, 94, e00498-20. [Google Scholar] [CrossRef] [PubMed]
- Tiley, L.S.; Hagen, M.; Matthews, J.T.; Krystal, M. Sequence-specific binding of the influenza virus RNA polymerase to sequences located at the 5′ ends of the viral RNAs. J. Virol. 1994, 68, 5108–5116. [Google Scholar] [CrossRef]
- Sinha, K.; Das, J.; Pal, P.B.; Sil, P.C. Oxidative stress: The mitochondria-dependent and mitochondria-independent pathways of apoptosis. Arch. Toxicol. 2013, 87, 1157–1180. [Google Scholar] [CrossRef]


| RNA Species | RNA Segment | Levels after Treatment with: | CT Difference | p Value | |
|---|---|---|---|---|---|
| WT | Flag-SOD3 | ||||
| vRNA | NA | 18.96 ± 0.47 | 19.67 ± 0.11 | 0.71 | 0.0249 |
| NP | 16.52 ± 0.40 | 17.22 ± 0.34 | 0.70 | 0.0379 | |
| PB1 | 19.73 ± 0.16 | 20.29 ± 0.02 | 0.56 | 0.0004 | |
| PA | 16.42 ± 0.33 | 16.93 ± 0.05 | 0.51 | 0.0209 | |
| PB2 | 18.02 ± 0.09 | 19.03 ± 0.07 | 1.01 | <0.0001 | |
| NS | 17.78 ± 0.13 | 18.67 ± 0.12 | 0.89 | <0.0001 | |
| M2 | 18.33 ± 0.14 | 19.16 ± 0.11 | 0.83 | <0.0001 | |
| HA | 21.85 ± 0.20 | 23.12 ± 0.40 | 1.27 | 0.0013 | |
| cRNA | NA | 22.27 ± 0.45 | 22.20 ± 0.12 | −0.07 | 0.7726 |
| NP | 19.79 ± 0.22 | 19.78 ± 0.24 | −0.01 | 0.9451 | |
| PB1 | 20.81 ± 0.11 | 20.89 ± 0.09 | 0.08 | 0.2922 | |
| PA | 20.13 ± 0.40 | 19.76 ± 0.06 | −0.37 | 0.1171 | |
| PB2 | 20.79 ± 0.06 | 20.90 ± 0.08 | 0.11 | 0.0654 | |
| NS | 21.80 ± 0.13 | 21.96 ± 0.10 | 0.16 | 0.1014 | |
| M2 | 20.84 ± 0.07 | 20.96 ± 0.06 | 0.12 | 0.0474 | |
| HA | 26.12 ± 0.29 | 26.44 ± 0.32 | 0.32 | 0.1777 | |
| mRNA | NA | 17.42 ± 0.28 | 17.63 ± 0.14 | 0.21 | 0.234 |
| NP | 13.51 ± 0.41 | 13.52 ± 0.19 | 0.01 | 0.9496 | |
| PB1 | 16.83 ± 0.08 | 16.92 ± 0.13 | 0.09 | 0.2895 | |
| PA | 16.64 ± 0.07 | 16.71 ± 0.04 | 0.07 | 0.0952 | |
| PB2 | 16.88 ± 0.08 | 17.21 ± 0.13 | 0.33 | 0.0047 | |
| NS | 14.82 ± 0.11 | 14.90 ± 0.09 | 0.08 | 0.31 | |
| M2 | 15.45 ± 0.09 | 15.66 ± 0.10 | 0.21 | 0.0183 | |
| HA | 19.36 ± 0.33 | 19.49 ± 0.14 | 0.13 | 0.4828 | |
| RNA Species | RNA Segment | Levels after Treatment with: | CT Difference | p Value | |
|---|---|---|---|---|---|
| WT | Flag-SOD3 | ||||
| vRNA | NA | 20.02 ± 0.18 | 21.53 ± 0.14 | 1.51 | 0.0003 |
| NP | 17.8 ± 0.01 | 19.12 ± 0.03 | 1.32 | <0.0001 | |
| PB1 | 20.91 ± 0.05 | 21.88 ± 0.03 | 0.97 | <0.0001 | |
| PA | 18.78 ± 0.09 | 20.01 ± 0.02 | 1.23 | <0.0001 | |
| PB2 | 19.49 ± 0.1 | 20.91 ± 0.01 | 1.42 | <0.0001 | |
| NS | 18.84 ± 0.17 | 20.12 ± 0.03 | 1.28 | 0.0002 | |
| M2 | 19.62 ± 0.04 | 21.04 ± 0.05 | 1.42 | <0.0001 | |
| HA | 23.79 ± 0.19 | 25.27 ± 0.19 | 1.48 | 0.0007 | |
| cRNA | NA | 23.28 ± 0.25 | 24.22 ± 0.14 | 0.94 | 0.0047 |
| NP | 20.09 ± 0.27 | 19.77 ± 0.17 | −0.32 | 0.1563 | |
| PB1 | 20.79 ± 0.13 | 21.41 ± 0.06 | 0.62 | 0.0016 | |
| PA | 20.15 ± 0.59 | 20.51 ± 0.12 | 0.36 | 0.3695 | |
| PB2 | 20.51 ± 0.01 | 21.01 ± 0.07 | 0.5 | 0.0002 | |
| NS | 21.7 ± 0.06 | 22.21 ± 0.09 | 0.51 | 0.0012 | |
| M2 | 20.59 ± 0.15 | 21.51 ± 0.04 | 0.92 | 0.0006 | |
| HA | 26.72 ± 0.39 | 27.54 ± 0.19 | 0.82 | 0.0312 | |
| mRNA | NA | 20.34 ± 0.31 | 20.54 ± 0.25 | 0.20 | 0.4510 |
| NP | 15.31 ± 0.25 | 15.58 ± 0.18 | 0.27 | 0.1908 | |
| PB1 | 18.59 ± 0.13 | 18.85 ± 0.12 | 0.26 | 0.0684 | |
| PA | 18.69 ± 0.78 | 18.76 ± 0.08 | 0.07 | 0.8906 | |
| PB2 | 18.38 ± 0.21 | 18.82 ± 0.11 | 0.44 | 0.0317 | |
| NS | 15.82 ± 0.11 | 16.32 ± 0.08 | 0.50 | 0.0029 | |
| M2 | 16.56 ± 0.12 | 17.00 ± 0.08 | 0.44 | 0.0059 | |
| HA | 22.91 ± 0.63 | 23.32 ± 0.70 | 0.41 | 0.4953 | |
| RNA Species | RNA Segment | Levels after Treatment with: | CT Difference | p Value | |
|---|---|---|---|---|---|
| NC | si-SOD3 | ||||
| vRNA | HA | 17.98 ± 0.2 | 16.08 ± 0.20 | −1.90 | <0.0001 |
| NA | 19.03 ± 0.39 | 16.91 ± 0.10 | −2.12 | <0.0001 | |
| NP | 14.28 ± 0.15 | 12.72 ± 0.10 | −1.56 | <0.0001 | |
| PB2 | 15.51 ± 0.26 | 14.08 ± 0.17 | −1.43 | <0.0001 | |
| NS | 14.42 ± 0.18 | 13.07 ± 0.04 | −1.35 | <0.0001 | |
| cRNA | HA | 25.43 ± 0.1 | 26.00 ± 0.25 | 0.57 | 0.0078 |
| NA | 24.7 ± 0.08 | 24.06 ± 0.30 | −0.64 | 0.00600 | |
| NP | 20.85 ± 0.16 | 20.80 ± 0.17 | −0.05 | 0.6697 | |
| PB2 | 20.39 ± 0.14 | 20.95 ± 0.15 | 0.56 | 0.0017 | |
| NS | 21.08 ± 0.1 | 20.73 ± 0.19 | −0.35 | 0.0168 | |
| mRNA | HA | 22.37 ± 0.47 | 21.76 ± 0.07 | −0.61 | 0.0424 |
| NA | 20.71 ± 0.36 | 19.88 ± 0.09 | −0.83 | 0.0044 | |
| NP | 16.84 ± 0.1 | 16.40 ± 0.19 | −0.44 | 0.0063 | |
| PB2 | 16.69 ± 0.11 | 16.45 ± 0.20 | −0.24 | 0.0773 | |
| NS | 17.06 ± 0.27 | 16.73 ± 0.29 | −0.33 | 0.1552 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, F.; Chen, L.; Liang, J.; Chen, Z.; Zhang, C.; Zhang, Z.; Yang, J. Potential Role of Superoxide Dismutase 3 (SOD3) in Resistance to Influenza A Virus Infection. Antioxidants 2023, 12, 354. https://doi.org/10.3390/antiox12020354
Chen F, Chen L, Liang J, Chen Z, Zhang C, Zhang Z, Yang J. Potential Role of Superoxide Dismutase 3 (SOD3) in Resistance to Influenza A Virus Infection. Antioxidants. 2023; 12(2):354. https://doi.org/10.3390/antiox12020354
Chicago/Turabian StyleChen, Feimin, Liurong Chen, Jinlong Liang, Zhixuan Chen, Chunyu Zhang, Zhengyin Zhang, and Jie Yang. 2023. "Potential Role of Superoxide Dismutase 3 (SOD3) in Resistance to Influenza A Virus Infection" Antioxidants 12, no. 2: 354. https://doi.org/10.3390/antiox12020354
APA StyleChen, F., Chen, L., Liang, J., Chen, Z., Zhang, C., Zhang, Z., & Yang, J. (2023). Potential Role of Superoxide Dismutase 3 (SOD3) in Resistance to Influenza A Virus Infection. Antioxidants, 12(2), 354. https://doi.org/10.3390/antiox12020354






