Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic and Anthropometric Characteristics and MD Adherence Evaluation
3.2. Health-Related Quality of Life, Physical Activity, and Sleep Quality Evaluation
3.3. Association of MD Adherence with Sociodemographic and Anthropometric Characteristics
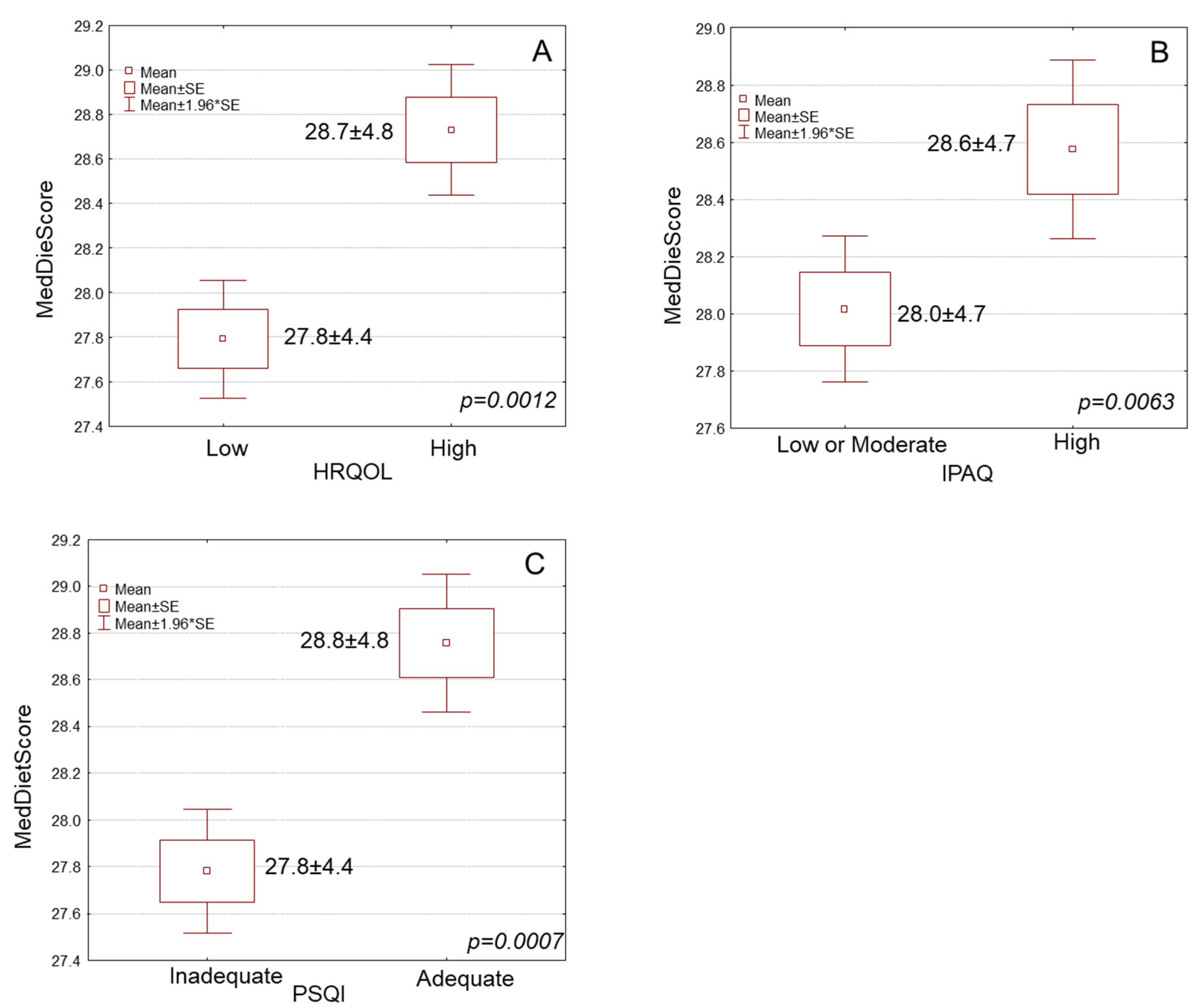
3.4. Association of MD Adherence with Health-Related Quality of Life, Physical Activity, and Sleep Quality
3.5. Multiple Regression Analysis for MD Adherence after Adjustment for Potential Confounding Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The United Nations Decade of Healthy Ageing (2021–2030). Available online: https://www.who.int/initiatives/decade-of-healthy-ageing (accessed on 18 February 2023).
- Gotsis, E.; Anagnostis, P.; Mariolis, A.; Vlachou, A.; Katsiki, N.; Karagiannis, A. Health benefits of the Mediterranean Diet: An update of research over the last 5 years. Angiology 2015, 66, 304–318. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Sofi, F. A Heart-Healthy Diet: Recent Insights and Practical Recommendations. Curr. Cardiol. Rep. 2017, 19, 95. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Adherence to Mediterranean diet and risk of cancer: An updated systematic review and meta-analysis of observational studies. Cancer Med. 2015, 4, 1933–1947. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Giugliano, D. Mediterranean diet and type 2 diabetes. Diabetes Metab. Res. Rev. 2015, 30 (Suppl. S1), 34–40. [Google Scholar] [CrossRef] [PubMed]
- Mantzorou, M.; Vadikolias, K.; Pavlidou, E.; Tryfonos, C.; Vasios, G.; Serdari, A.; Giaginis, C. Mediterranean diet adherence is associated with better cognitive status and less depressive symptoms in a Greek elderly population. Aging Clin. Exp. Res. 2021, 33, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Frias-Toral, E.; Chapela, S.; de los Angeles Carignano, M.; Moretti, D.; Martinuzzi, A.; Rodriguez-Veintimilla, D.; Guerrero, M.; Pugliese, G.; Muscogiuri, G.; Barrea, L. Mediterranean diet and physical activity for successful aging: An update for nutritionists and endocrinologists. Endocrines 2021, 2, 366–383. [Google Scholar] [CrossRef]
- Foscolou, A.; D’Cunha, N.M.; Naumovski, N.; Tyrovolas, S.; Chrysohoou, C.; Rallidis, L.; Polychronopoulos, E.; Matalas, A.L.; Sidossis, L.S.; Panagiotakos, D. The association between the level of adherence to the Mediterranean diet and successful aging: An analysis of the ATTICA and MEDIS (MEDiterranean Islands Study) epidemiological studies. Arch. Gerontol. Geriatr. 2020, 89, 104044. [Google Scholar] [CrossRef]
- Andreo-López, M.C.; Contreras-Bolívar, V.; Muñoz-Torres, M.; García-Fontana, B.; García-Fontana, C. Influence of the Mediterranean Diet on Healthy Aging. Int. J. Mol. Sci. 2023, 24, 4491. [Google Scholar] [CrossRef]
- Tsigalou, C.; Konstantinidis, T.; Paraschaki, A.; Stavropoulou, E.; Voidarou, C.; Bezirtzoglou, E. Medi-terranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicines 2020, 8, 201. [Google Scholar] [CrossRef]
- Finicelli, M.; Di Salle, A.; Galderisi, U.; Peluso, G. The Mediterranean Diet: An Update of the Clinical Trials. Nutrients 2022, 14, 2956. [Google Scholar] [CrossRef]
- Gantenbein, K.V.; Kanaka-Gantenbein, C. Mediterranean Diet as an Antioxidant: The Impact on Metabolic Health and Overall Wellbeing. Nutrients 2021, 13, 1951. [Google Scholar] [CrossRef] [PubMed]
- Sikalidis, A.K.; Kelleher, A.H.; Kristo, A.S. Mediterranean Diet. Encyclopedia 2021, 1, 371–387. [Google Scholar] [CrossRef]
- Maykish, A.; Rex, R.; Sikalidis, A.K. Organic Winemaking and Its Subsets; Biodynamic, Natural, and Clean Wine in California. Foods 2021, 10, 127. [Google Scholar] [CrossRef] [PubMed]
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized con-trolled trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487. [Google Scholar] [CrossRef]
- Govindaraju, T.; Sahle, B.W.; McCaffrey, T.A.; McNeil, J.J.; Owen, A.J. Dietary Patterns and Quality of Life in Older Adults: A Systematic Review. Nutrients 2018, 10, 971. [Google Scholar] [CrossRef]
- Pérez-Tasigchana, R.F.; León-Muñoz, L.M.; López-García, E.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Mediterranean Diet and Health-Related Quality of Life in two cohorts of commu-nity-dwelling older adults. PLoS ONE 2016, 11, e0151596. [Google Scholar] [CrossRef]
- Galilea-Zabalza, I.; Buil-Cosiales, P.; Salas-Salvado, J.; Toledo, E.; Ortega-Azorín, C.; Díez-Espino, J.; Vázquez-Ruiz, Z.; Zomeño, M.D.; Vioque, J.; Martínez, J.A.; et al. PREDIMED-PLUS Study Investigators. Mediterranean diet and quality of life: Baseline cross-sectional analysis of the PREDIMED-PLUS trial. PLoS ONE 2018, 13, e0198974. [Google Scholar] [CrossRef]
- Veronese, N.; Stubbs, B.; Noale, M.; Solmi, M.; Luchini, C.; Maggi, S. Adherence to the Mediterranean diet is associated with better quality of life: Data from the Osteoarthritis Initiative. Am. J. Clin. Nutr. 2016, 104, 1403–1409. [Google Scholar] [CrossRef]
- Word Health Organization. Physical Activity. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 15 February 2023).
- Gluchowski, A.; Bilsborough, H.; Mcdermott, J.; Hawley-Hague, H.; Todd, C. A lot of people just go for walks, and don’t do anything else’: Older adults in the UK are not aware of the strength component embedded in the chief medical officers’ physical activity guidelines—A qualitative study. Int. J. Environ. Res. Public Health 2022, 19, 10002. [Google Scholar] [CrossRef]
- Vagetti, G.C.; Barbosa Filho, V.C.; Moreira, N.B.; de Oliveira, V.; Mazzardo, O.; de Campos, W. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Braz. J. Psychiatry 2014, 36, 76–88. [Google Scholar] [CrossRef]
- Mok, A.; Khaw, K.T.; Luben, R.; Wareham, N.; Brage, S. Physical activity trajectories and mortality: Population based cohort study. BMJ 2019, 365, l2323. [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.E.; Lee, I.M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br. J. Sport. Med. 2019, 53, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Yan, W.; Wang, T.; Zhu, L.J.; Xu, Y.; Zhao, J.; Yu, L.L.; Bao, H.H.; Cheng, X.S. Independent and joint association of physical activity and sedentary behavior on all-cause mortality. Chin. Med. J. 2021, 134, 2857–2864. [Google Scholar] [CrossRef]
- Lok, N.; Lok, S.; Canbaz, M. The effect of physical activity on depressive symptoms and quality of life among elderly nursing home residents: Randomized controlled trial. Arch. Gerontol. Geriatr. 2017, 70, 92–98. [Google Scholar] [CrossRef]
- Ebeling, P.R.; Cicuttini, F.; Scott, D.; Jones, G. Promoting mobility and healthy aging in men: A narrative review. Osteoporos. Int. 2019, 30, 1911–1922. [Google Scholar] [CrossRef]
- Hosker, D.K.; Elkins, R.M.; Potter, M.P. Promoting mental health and wellness in youth through physical activity, nutrition, and sleep. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 171–193. [Google Scholar] [CrossRef]
- Wolkove, N.; Elkholy, O.; Baltzan, M.; Palayew, M. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007, 176, 1299–1304. [Google Scholar] [CrossRef]
- Arora, T.; Choudhury, S.; Taheri, S. The relationships among sleep, nutrition, and obesity. Curr. Sleep Med. Rep. 2015, 1, 218–225. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M.; Bhatt, D.L.; American Heart Association, Behavior Change, Diabetes, and Nutrition Committees of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; et al. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the American Heart Association. Circulation 2016, 134, 367–386. [Google Scholar] [CrossRef]
- Fenton, S.; Burrows, T.L.; Skinner, J.A.; Duncan, M.J. The influence of sleep health on dietary intake: A systematic review and meta-analysis of intervention studies. J. Hum. Nutr. Diet. 2021, 34, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Antza, C.; Kostopoulos, G.; Mostafa, S.; Nirantharakumar, K.; Tahrani, A. The links between sleep duration, obesity and type 2 diabetes mellitus. J. Endocrinol. 2021, 252, 125–141. [Google Scholar] [CrossRef] [PubMed]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Schoeller, D.A.; Penev, P.D. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann. Intern. Med. 2010, 153, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Yannakoulia, M.; Anastasiou, C.A.; Karfopoulou, E.; Pehlivanidis, A.; Panagiotakos, D.B.; Vgontzas, A. Sleep quality is associated with weight loss maintenance status: The MedWeight study. Sleep Med. 2017, 34, 242–245. [Google Scholar] [CrossRef]
- Frank, S.; Gonzalez, K.; Lee-Ang, L.; Young, M.C.; Tamez, M.; Mattei, J. Diet and sleep physiology: Public health and clinical implications. Front. Neurol. 2017, 8, 393. [Google Scholar] [CrossRef]
- Scoditti, E.; Tumolo, M.R.; Garbarino, S. Mediterranean diet on sleep: A health alliance. Nutrients 2022, 14, 2998. [Google Scholar] [CrossRef]
- Ikonte, C.J.; Mun, J.G.; Reider, C.A.; Grant, R.W.; Mitmesser, S.H. Micronutrient Inadequacy in Short Sleep: Analysis of the NHANES 2005–2016. Nutrients 2019, 11, 2335. [Google Scholar] [CrossRef]
- Rondanelli, M.; Opizzi, A.; Monteferrario, F.; Antoniello, N.; Manni, R.; Klersy, C. The effect of melatonin, magnesium, and zinc on primary insomnia in long-term care facility residents in Italy: A double-blind, placebo-controlled clinical trial. J. Am. Geriatr. Soc. 2011, 59, 82–90. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Carr, M.; Gorman, C.; Perlis, M.L. Effects of a tart cherry juice beverage on the sleep of older adults with insomnia: A pilot study. J. Med. Food 2010, 13, 579–583. [Google Scholar] [CrossRef]
- Gupta, C.C.; Irwin, C.; Vincent, G.E.; Khalesi, S. The Relationship Between Diet and Sleep in Older Adults: A Narrative Review. Cur. Nutr. Rep. 2021, 10, 166–178. [Google Scholar] [CrossRef]
- Barile, J.P.; Horner-Johnson, W.; Krahn, G.; Zack, M.; Miranda, D.; DeMichele, K.; Ford, D.; Thompson, W.W. Measurement characteristics for two health-related quality of life measures in older adults: The SF-36 and the CDC Healthy Days items. Disabil. Health J. 2016, 9, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Salahuddin, M.; Maru, T.T.; Kumalo, A.; Pandi-Perumal, S.R.; Bahammam, A.S.; Manzar, M.D. Validation of the Pittsburgh sleep quality index in community dwelling Ethiopian adults. Health Qual. Life Outcomes 2017, 15, 58. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Arvaniti, F.; Stefanadis, C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev. Med. 2007, 44, 335–340. [Google Scholar] [CrossRef]
- Mantzorou, M.; Vadikolias, K.; Pavlidou, E.; Serdari, A.; Vasios, G.; Tryfonos, C.; Giaginis, C. Nutritional status is associated with the degree of cognitive impairment and depressive symptoms in a Greek elderly population. Nutr. Neurosci. 2020, 23, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Filippidis, F.T.; Tzavara, C.; Dimitrakaki, C.; Tountas, Y. Compliance with a healthy lifestyle in a representative sample of the Greek population: Preliminary results of the Hellas Health I study. Public Health 2011, 125, 436–441. [Google Scholar] [CrossRef] [PubMed]
- Bracale, R.; Vaccaro, C.M.; Coletta, V.; Cricelli, C.; Gamaleri, F.C.; Parazzini, F.; Carruba, M. Nutrition behaviour and compliance with the Mediterranean diet pyramid recommendations: An Italian survey-based study. Eat Weight Disord. 2020, 25, 1789–1798. [Google Scholar] [CrossRef]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef]
- Ventriglio, A.; Sancassiani, F.; Contu, M.P.; Latorre, M.; Di Slavatore, M.; Fornaro, M.; Bhugra, D. Medi-terranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin. Pract. Epidemiol. Ment. Health 2020, 16 (Suppl. S1), 156–164. [Google Scholar] [CrossRef]
- Apostolaki, I.; Pepa, A.; Vlassopoulos, A.; Kapsokefalou, M. Social capital and self-perceived quality of life-interrelated predictors of Mediterranean diet adherence in older adults. Nutrients 2021, 13, 3100. [Google Scholar] [CrossRef]
- Zaragoza-Martí, A.; Ferrer-Cascales, R.; Hurtado-Sánchez, J.A.; Laguna-Pérez, A.; Cabañero-Martínez, M.J. Relationship between adherence to the Mediterranean diet and health-related quality of life and life satisfaction among older adults. J. Nutr. Health Aging 2018, 22, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Milte, C.M.; Thorpe, M.G.; Crawford, D.; Ball, K.; McNaughton, S.A. Associations of diet quality with health-related quality of life in older Australian men and women. Exp. Gerontol. 2015, 64, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Henríquez Sánchez, P.; Ruano, C.; de Irala, J.; Ruiz-Canela, M.; Martínez-González, M.A.; Sánchez-Villegas, A. Adherence to the Mediterranean diet and quality of life in the SUN Project. Eur. J. Clin. Nutr. 2012, 66, 360–368. [Google Scholar] [CrossRef]
- Ruano, C.; Henriquez, P.; Martínez-González, M.Á.; Bes-Rastrollo, M.; Ruiz-Canela, M.; Sánchez-Villegas, A. Empirically derived dietary patterns and health-related quality of life in the SUN project. PLoS ONE 2013, 8, e61490. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Aguadero, N.; Alonso-Dominguez, R.; Garcia-Ortiz, L.; Agudo-Conde, C.; Rodriguez-Martin, C.; de Cabo-Laso, A.; Sanchez-Salgado, B.; Ramos, R.; Maderuelo-Fernandez, J.A.; Gomez-Marcos, M.A.; et al. Diet and physical activity in people with intermediate cardiovascular risk and their relationship with the health-related quality of life: Results from the MARK study. Health Qual. Life Outcomes 2016, 14, 169. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Liu, G.G.; Shi, Q.L.; Sun, Y.; Zhang, H.; Wang, M.J.; Jia, H.P.; Zhao, Y.L.; Yao, Y. Health-Related Quality of Life and associated factors among oldest-old in China. J. Nutr. Health Aging 2020, 24, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.; Fenton, S.; Duncan, M. Diet and sleep health: A scoping review of intervention studies in adults. J. Hum. Nutr. Diet. 2020, 33, 308–329. [Google Scholar] [CrossRef]
- Akbaraly, T.N.; Jaussent, I.; Besset, A.; Marion Bertrand, M.; Barberger-Gateau, P.; Ritchie, K.; Ferrie, J.E.; Kivimaki, M.; Dauvilliers, Y. Sleep complaints and metabolic syndrome in an elderly population: The three-city study. Am. J. Geriatr. Psychiatry 2015, 23, 818–828. [Google Scholar] [CrossRef]
- López-García, E.; Faubel, R.; León-Muñoz, L.; Zuluaga, M.C.; Banegas, J.R.; Rodríguez-Artalejo, F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am. J. Clin. Nutr. 2008, 87, 310–316. [Google Scholar] [CrossRef]
- Zhao, M.; Tuo, H.; Wang, S.; Zhao, L. The Effects of Dietary Nutrition on Sleep and Sleep Disorders. Mediat. Inflamm. 2020, 2020, 3142874. [Google Scholar] [CrossRef]
- Naja, F.; Hasan, H.; Khadem, S.H.; Buanq, M.A.; Al-Mulla, H.K.; Aljassmi, A.K.; Faris, M.E. Adherence to the Mediterranean diet and its association with sleep quality and chronotype among youth: A cross-sectional study. Front. Nutr. 2022, 8, 805955. [Google Scholar] [CrossRef]
- Gupta, K.; Jansen, E.C.; Campos, H.; Baylin, A. Associations between sleep duration and Mediterranean diet score in Costa Rican adults. Appetite 2022, 170, 105881. [Google Scholar] [CrossRef] [PubMed]
- Mamalaki, E.; Anastasiou, C.A.; Ntanasi, E.; Tsapanou, A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. Associations between the Mediterranean diet and sleep in older adults: Results from the Hellenic longitudinal investigation of aging and diet study. Geriatr. Gerontol. Int. 2018, 11, 1543–1548. [Google Scholar] [CrossRef] [PubMed]
- Campanini, M.Z.; Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Mediterranean Diet and Changes in Sleep Duration and Indicators of Sleep Quality in Older Adults. Sleep 2017, 40, zsw093. [Google Scholar] [CrossRef] [PubMed]
- Flor-Alemany, M.; Nestares, T.; Alemany-Arrebola, I.; Marín-Jiménez, N.; Borges-Cosic, M.; Aparicio, V.A. Influence of dietary habits and Mediterranean diet adherence on sleep quality during pregnancy. The GESTAFIT Project. Nutrients 2020, 12, 3569. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Barrea, L.; Aprano, S.; Framondi, L.; Di Matteo, R.; Laudisio, D.; Pugliese, G.; Savastano, S.; Colao, A.; on behalf of the OPERA PREVENTION Project. Sleep quality in obesity: Does adherence to the Mediterranean diet matter? Nutrients 2020, 12, 1364. [Google Scholar] [CrossRef]
- Zuraikat, F.M.; Makarem, N.; St-Onge, M.P.; Xi, H.; Akkapeddi, A.; Aggarwal, B. A Mediterranean dietary pattern predicts better sleep quality in US women from the American Heart Association Go Red for Women Strategically Focused Research Network. Nutrients 2020, 12, 2830. [Google Scholar] [CrossRef]
- Castro-Diehl, C.; Wood, A.C.; Redline, S.; Reid, M.; Johnson, D.A.; Maras, J.E.; Jacobs, D.R.J.; Shea, S.; Crawford, A.; St-Onge, M.P. Mediterranean diet pattern and sleep duration and insomnia symptoms in the Multi-Ethnic Study of Atherosclerosis. Sleep 2018, 41, zsy158. [Google Scholar] [CrossRef]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between diet and sleep quality: A systematic review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef]
- Štefan, L.; Radman, I.; Podnar, H.; Vrgoč, G. Sleep Duration and Sleep Quality Associated with Dietary Index in Free-Living Very Old Adults. Nutrients 2018, 10, 1748. [Google Scholar] [CrossRef]
- Godos, J.; Ferri, R.; Caraci, F.; Cosentino, F.I.I.; Castellano, S.; Shivappa, N.; Hebert, J.R.; Galvano, F.; Grosso, G. Dietary Inflammatory Index and Sleep Quality in Southern Italian Adults. Nutrients 2019, 11, 1324. [Google Scholar] [CrossRef] [PubMed]
- Rostami, H.; Parastouei, K.; Samadi, M.; Taghdir, M.; Eskandari, E. Adherence to the MIND dietary pattern and sleep quality, sleep related outcomes and mental health in male adults: A cross-sectional study. BMC Psychiatry 2022, 22, 167. [Google Scholar] [CrossRef]
- Sejbuk, M.; Mirończuk-Chodakowska, I.; Witkowska, A.M. Sleep quality: A narrative review on nutrition, stimulants, and physical activity as important factors. Nutrients 2022, 14, 1912. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.-P.; Mikic, A.; Pietrolungo, C.E. Effects of diet on sleep quality. Adv. Nutr. Int. Rev. J. 2016, 7, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Binks, H.; Vincent, G.E.; Gupta, C.; Irwin, C.; Khalesi, S. Effects of diet on sleep: A narrative review. Nutrients 2020, 12, 936. [Google Scholar] [CrossRef]
- Ogilvie, R.P.; Patel, S. The epidemiology of sleep and obesity. Sleep Health 2018, 3, 383–388. [Google Scholar] [CrossRef]
- Capurso, C.; Bellanti, F.; Buglio, A.L.; Vendemiale, G. The Mediterranean diet slows down the progression of aging and helps to prevent the onset of frailty: A narrative review. Nutrients 2019, 12, 35. [Google Scholar] [CrossRef]
- Kojima, G.; Avgerinou, C.; Iliffe, S.; Walters, K. Adherence to Mediterranean Diet Reduces Incident Frailty Risk: Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2018, 66, 783–788. [Google Scholar] [CrossRef]
- Coelho-Júnior, H.J.; Trichopoulou, A.; Panza, F. Cross-sectional and longitudinal associations between adherence to Mediterranean diet with physical performance and cognitive function in older adults: A systematic review and meta-analysis. Ageing Res. Rev. 2021, 70, 101395. [Google Scholar] [CrossRef]
- Cárdenas-Fuentes, G.; Subirana, I.; Martinez-Gonzalez, M.A.; Salas-Salvadó, J.; Corella, D.; Estruch, R.; Fíto, M.; Muñoz-Bravo, C.; Fiol, M.; Lapetra, J.; et al. Multiple approaches to associations of physical activity and adherence to the Mediterranean diet with all-cause mortality in older adults: The PREvención con DIeta MEDiterránea study. Eur. J. Nutr. 2019, 58, 1569–1578. [Google Scholar] [CrossRef]
- Serra, M.C.; Dondero, K.R.; Larkins, D.; Burns, A.; Addison, O. Healthy lifestyle and cognition: Interaction between diet and physical activity. Curr. Nutr. Rep. 2020, 9, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Knoops, K.T.B.; de Groot, L.C.P.G.M.; Kromhout, D.; Perrin, A.-E.; Moreiras-Varela, O.; Menotti, A.; van Staveren, W.A. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: The HALE Project. JAMA 2004, 292, 1433–1439. [Google Scholar] [CrossRef] [PubMed]
- Conde-Pipó, J.; Bouzas, C.; Zurita-Ortega, F.; Olea-Serrano, F.; Tur, J.A.; Mariscal-Arcas, M. Adherence to a Mediterranean diet pattern, physical activity, and physical self-concept in Spanish older adults. Nutrients 2022, 14, 2404. [Google Scholar] [CrossRef] [PubMed]
- Saadeh, M.; Prinelli, F.; Vetrano, D.L.; Xu, W.; Welmer, A.K.; Dekhtyar, S.; Fratiglioni, L.; Calderón-Larrañaga, A. Mobility and muscle strength trajectories in old age: The beneficial effect of Mediterranean diet in combination with physical activity and social support. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 120. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Oguma, Y.; Asakura, K.; Takayama, M.; Abe, Y.; Arai, Y. Relationship between dietary patterns and subjectively measured physical activity in Japanese individuals 85 years and older: A cross-sectional study. Nutrients 2022, 14, 2924. [Google Scholar] [CrossRef] [PubMed]
- Jezewska-Zychowicz, M.; Gębski, J.; Guzek, D.; Świątkowska, M.; Stangierska, D.; Plichta, M.; Wasilewska, M. The Associations between dietary patterns and sedentary behaviors in Polish adults (LifeStyle Study). Nutrients 2018, 10, 1004. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Critselis, E.; Panagiotakos, D. Adherence to the Mediterranean diet and healthy ageing: Current evidence, biological pathways, and future directions. Crit. Rev. Food Sci. Nutr. 2020, 60, 2148–2157. [Google Scholar] [CrossRef]
- Moschny, A.; Platen, P.; Klaaßen-Mielke, R.; Trampisch, U.; Hinrichs, T. Barriers to physical activity in older adults in Germany: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 121. [Google Scholar] [CrossRef]
- Bullo, V.; Gobbo, S.; Vendramin, B.; Duregon, F.; Cugusi, L.; Di Blasio, A.; Bocalini, D.S.; Zaccaria, M.; Bergamin, M.; Ermolao, A. Nordic Walking Can Be Incorporated in the Exercise Prescription to In-crease Aerobic Capacity, Strength, and Quality of Life for Elderly: A Systematic Review and Meta-Analysis. Rejuvenation Res. 2018, 21, 141–161. [Google Scholar] [CrossRef]
- Granado-Casas, M.; Martin, M.; Martínez-Alonso, M.; Alcubierre, N.; Hernández, M.; Alonso, N.; Castelblanco, E.; Mauricio, D. The Mediterranean Diet is Associated with an Improved Quality of Life in Adults with Type 1 Diabetes. Nutrients 2020, 12, 131. [Google Scholar] [CrossRef] [PubMed]
- Klonizakis, M.; Grammatikopoulou, M.G.; Theodoridis, X.; Milner, M.; Liu, Y.; Chourdakis, M. Effects of Long-Versus Short-Term Exposure to the Mediterranean Diet on Skin Microvascular Function and Quality of Life of Healthy Adults in Greece and the UK. Nutrients 2019, 11, 2487. [Google Scholar] [CrossRef] [PubMed]
- Al-Biltagi, M.; El Amrousy, D.; El Ashry, H.; Maher, S.; Mohammed, M.A.; Hasan, S. Effects of adherence to the Mediterranean diet in children and adolescents with irritable bowel syndrome. World J. Clin. Pediatr. 2022, 11, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Bayes, J.; Schloss, J.; Sibbritt, D. The effect of a Mediterranean diet on the symptoms of depression in young males (the “AMMEND: A Mediterranean Diet in MEN with Depression” study): A randomized controlled trial. Am. J. Clin. Nutr. 2022, 116, 572–580. [Google Scholar] [CrossRef]
- Santulli, G.; Pascale, V.; Finelli, R.; Visco, V.; Giannotti, R.; Massari, A.; Morisco, C.; Ciccarelli, M.; Illario, M.; Iaccarino, G.; et al. We are What We Eat: Impact of Food from Short Supply Chain on Metabolic Syndrome. J. Clin. Med. 2019, 8, 2061. [Google Scholar] [CrossRef]
- Grace-Farfaglia, P. Self-Reported Diet and Health Outcomes of Participants of the CCSVI-Tracking Survey Study. Nutrients 2021, 13, 1891. [Google Scholar] [CrossRef]
- Zelicha, H.; Kloting, N.; Kaplan, A.; Meir, A.Y.; Rinott, E.; Tsaban, G.; Chassidim, Y.; Bluher, M.; Ceglarek, U.; Isermann, B.; et al. The effect of high-polyphenol Mediterranean diet on visceral adiposity: The DIRECT PLUS randomized controlled trial. BMC Med. 2022, 20, 327. [Google Scholar] [CrossRef]
- Dragun, R.; Veček, N.N.; Marendić, M.; Pribisalić, A.; Đivić, G.; Cena, A.; Polašek, O.; Kolčić, I. Have Lifestyle Habits and Psychological Well-Being Changed among Adolescents and Medical Students Due to COVID-19 Lockdown in Croatia? Nutrients 2020, 13, 97. [Google Scholar] [CrossRef]
- Pastori, D.; Carnevale, R.; Nocella, C.; Novo, M.; Santulli, M.; Cammisotto, V.; Menichelli, D.; Pignatelli, P.; Violi, F. Gut-Derived Serum Lipopolysaccharide is Associated with Enhanced Risk of Major Adverse Cardiovascular Events in Atrial Fibrillation: Effect of Adherence to Mediterranean Diet. J. Am. Heart Assoc. 2017, 6, e005784. [Google Scholar] [CrossRef]
- Hidalgo-Liberona, N.; Meroño, T.; Zamora-Ros, R.; Rabassa, M.; Semba, R.; Toshiko, T.; Bandinelli, S.; Ferrucci, L.; Andres-Lacueva, C.; Cherubini, A. Adherence to the Mediterranean diet assessed by a novel dietary biomarker score and mortality in older adults: The InCHIANTI cohort study. BMC Med. 2021, 19, 280. [Google Scholar] [CrossRef]
| Parameters, n = 3254 | Mediterranean Diet Adherence | ||||
|---|---|---|---|---|---|
| Very Low (25.8%) | Low (25.6%) | Moderate (24.8%) | High (23.8%) | p-Value | |
| Age (yrs ± SD) | 77.1 ± 8.5 | 74.7 ± 7.9 | 74.5 ± 8.8 | 72.5 ± 7.6 | p < 0.0001 |
| Sex (n, %) | p < 0.0001 | ||||
| Female | 358 (42.6) | 404 (48.6) | 414 (51.4) | 504 (64.9) | |
| Male | 482 (57.4) | 428 (51.4) | 392 (48.6) | 272 (35.1) | |
| Body mass index | 27.7 ± 4.0 | 27.6 ± 3.8 | 27.4 ± 4.2 | 26.9 ± 4.3 | p = 0.0047 |
| Mid arm circumference (n, %) | p = 0.0008 | ||||
| <22 cm | 278 (33.1) | 232 (27.9) | 216 (26.8) | 115 (14.8) | |
| ≥22 cm | 562 (66.9) | 600 (72.1) | 590 (73.2) | 661 (85.2) | |
| Calf circumference (n, %) | p = 0.0011 | ||||
| <31 cm | 362 (43.1) | 332 (39.9) | 286 (35.5) | 178 (22.9) | |
| ≥31 cm | 478 (56.9) | 500 (60.1) | 520 (64.5) | 598 (77.1) | |
| Educational level (yrs ± SD) | 7.0 ± 2.2 | 7.1 ± 2.7 | 7.3 ± 3.3 | 7.7 ± 3.0 | p = 0.0026 |
| Financial status (n, %) | p = 0.0005 | ||||
| Low | 414 (49.3) | 395 (47.5) | 307 (38.1) | 268 (34.5) | |
| Medium | 377 (44.9) | 371 (44.6) | 272 (33.7) | 222 (28.6) | |
| High | 49 (5.8) | 66 (7.9) | 227 (28.2) | 286 (36.9) | |
| Living status (n, %) | p = 0.0016 | ||||
| Alone | 403 (48.0) | 372 (44.7) | 242 (30.0) | 170 (21.9) | |
| With others | 437 (52.0) | 460 (52.3) | 564 (70.0) | 606 (78.1) | |
| Smoking habits (n, %) | p = 0.0031 | ||||
| Never smokers | 683 (81.3) | 691 (83.0) | 542 (67.2) | 513 (66.1) | |
| Smokers | 157 (18.7) | 141 (17.0) | 264 (32.8) | 263 (33.9) | |
| HRQOL (n, %) | p < 0.0001 | ||||
| Very low | 273 (32.5) | 256 (30.8) | 163 (20.2) | 124 (16.0) | |
| Low | 251 (30.0) | 246 (29.6) | 154 (19.1) | 130 (16.7) | |
| Moderate | 158 (18.8) | 180 (21.6) | 258 (32.0) | 256 (33.0) | |
| High | 158 (18.8) | 150 (18.0) | 231 (28.7) | 266 (34.3) | |
| IPAQ (n, %) | p < 0.0001 | ||||
| Low | 435 (51.8) | 408 (49.0) | 281 (34.9) | 206 (26.5) | |
| Moderate | 389 (46.3) | 360 (43.3) | 232 (28.8) | 168 (21.7) | |
| High | 16 (1.9) | 64 (7.7) | 293 (36.3) | 402 (51.8) | |
| PSQI (n, %) | p < 0.0001 | ||||
| Inadequate | 312 (62.9) | 461 (55.4) | 233 (28.9) | 222 (28.6) | |
| Adequate | 249 (37.1) | 371 (44.6) | 573 (71.1) | 554 (71.4) | |
| Parameters | OR (95% CI) | p-Value |
|---|---|---|
| Age | 0.1173 | |
| Below mean value | 1.0 | |
| Over mean value | 0.93 (0.48–1.51) | |
| Sex | 0.0032 | |
| Male | 1.0 | |
| Female | 1.36 (1.02–1.68) | |
| BMI | 0.2657 | |
| Normal | 1.0 | |
| Overweight or obese | 0.87 (0.36–1.49) | |
| Mid arm circumference | 0.2895 | |
| <22 cm | 1.0 | |
| ≥22 cm | 1.22 (0.70–1.73) | |
| Calf circumference | 0.1246 | |
| <31 cm | 1.0 | |
| ≥31 cm | 1.15 (0.77–1.54) | |
| Educational level | 0.0812 | |
| Below mean value | 1.0 | |
| Over mean value | 1.11 (0.58–1.63) | |
| Economic status | 0.2301 | |
| Low or medium | 1.0 | |
| High | 1.17 (0.73–1.60) | |
| Living status | 0.0375 | |
| Alone | 1.0 | |
| With others | 1.24 (0.81–1.76) | |
| Smoking habits | 0.0763 | |
| No | 1.0 | |
| Yes | 0.83 (0.42–1.30) | |
| HRQOL | 0.0008 | |
| Very low or low | 1.0 | |
| Moderate or high | 2.31 (2.06–2.68) | |
| IPAQ | 0.0141 | |
| Low | 1.0 | |
| Moderate or high | 1.89 (1.47–2.35) | |
| PSQI | 0.0018 | |
| Inadequate | 1.0 | |
| Adequate | 2.11 (1.79–2.44) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantzorou, M.; Mentzelou, M.; Vasios, G.K.; Kontogiorgis, C.; Antasouras, G.; Vadikolias, K.; Psara, E.; Vorvolakos, T.; Poulios, E.; Serdari, A.; et al. Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants 2023, 12, 983. https://doi.org/10.3390/antiox12050983
Mantzorou M, Mentzelou M, Vasios GK, Kontogiorgis C, Antasouras G, Vadikolias K, Psara E, Vorvolakos T, Poulios E, Serdari A, et al. Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants. 2023; 12(5):983. https://doi.org/10.3390/antiox12050983
Chicago/Turabian StyleMantzorou, Maria, Maria Mentzelou, Georgios K. Vasios, Christos Kontogiorgis, Georgios Antasouras, Konstantinos Vadikolias, Evmorfia Psara, Theofanis Vorvolakos, Efthymios Poulios, Aspasia Serdari, and et al. 2023. "Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population" Antioxidants 12, no. 5: 983. https://doi.org/10.3390/antiox12050983
APA StyleMantzorou, M., Mentzelou, M., Vasios, G. K., Kontogiorgis, C., Antasouras, G., Vadikolias, K., Psara, E., Vorvolakos, T., Poulios, E., Serdari, A., Papadopoulou, S. K., & Giaginis, C. (2023). Mediterranean Diet Adherence Is Associated with Favorable Health-Related Quality of Life, Physical Activity, and Sleep Quality in a Community-Dwelling Greek Older Population. Antioxidants, 12(5), 983. https://doi.org/10.3390/antiox12050983










