Neuroprotective Effects of Olive Oil: A Comprehensive Review of Antioxidant Properties
Abstract
1. Introduction
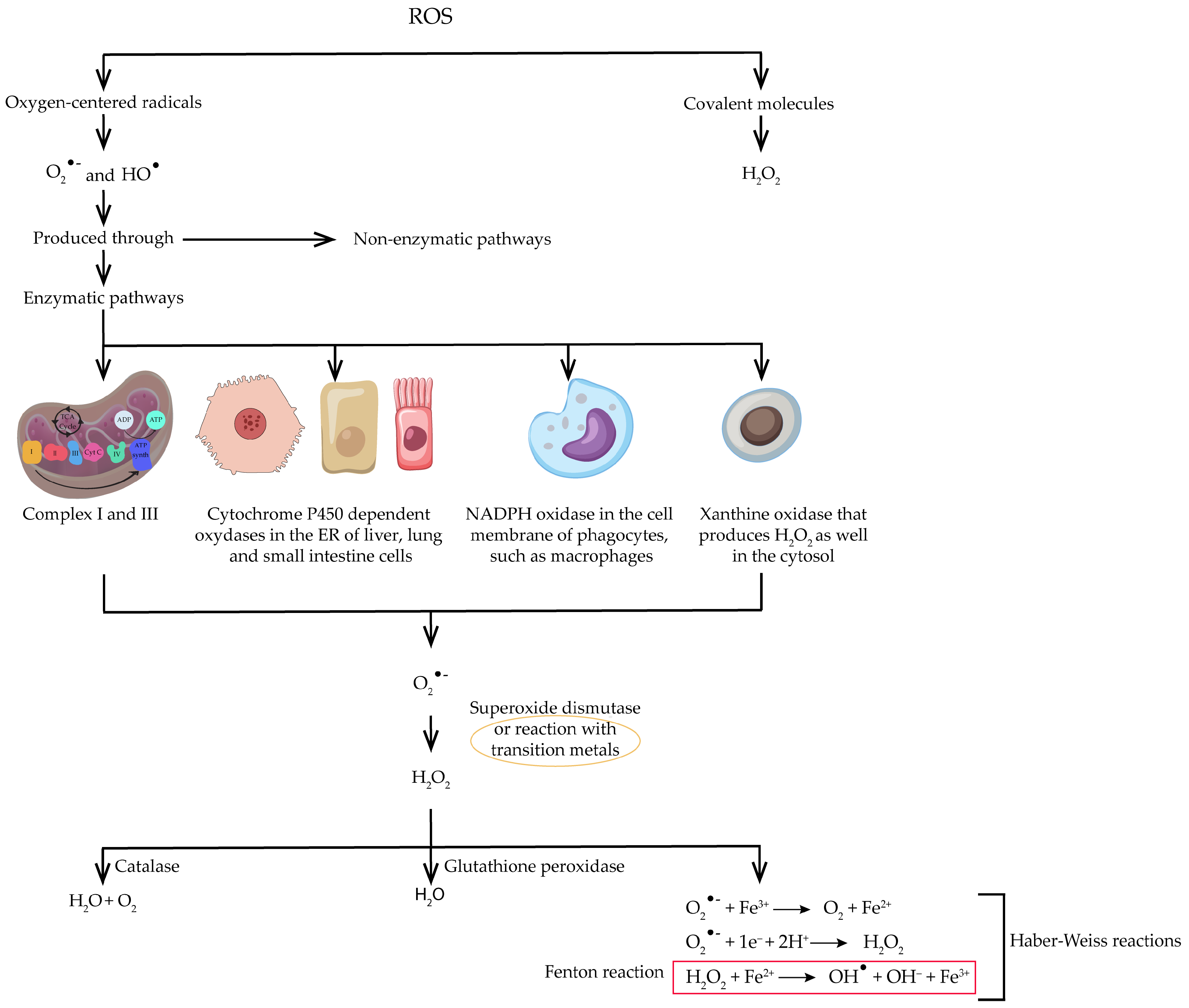
2. Neurodegenerative Diseases and Oxidative Stress
| AD | PD | HD | ALS | |
|---|---|---|---|---|
| Mitochondrial dysfunction |
|
|
|
|
| Metal ion imbalance |
|
|
|
|
| Inflammation |
|
|
|
|
| Reduced antioxidant defenses |
|
|
|
|
| Genetic factors |
|
|
|
|
| Environmental factors |
|
|
|
|
| Protein aggregation and accumulation |
|
|
|
|
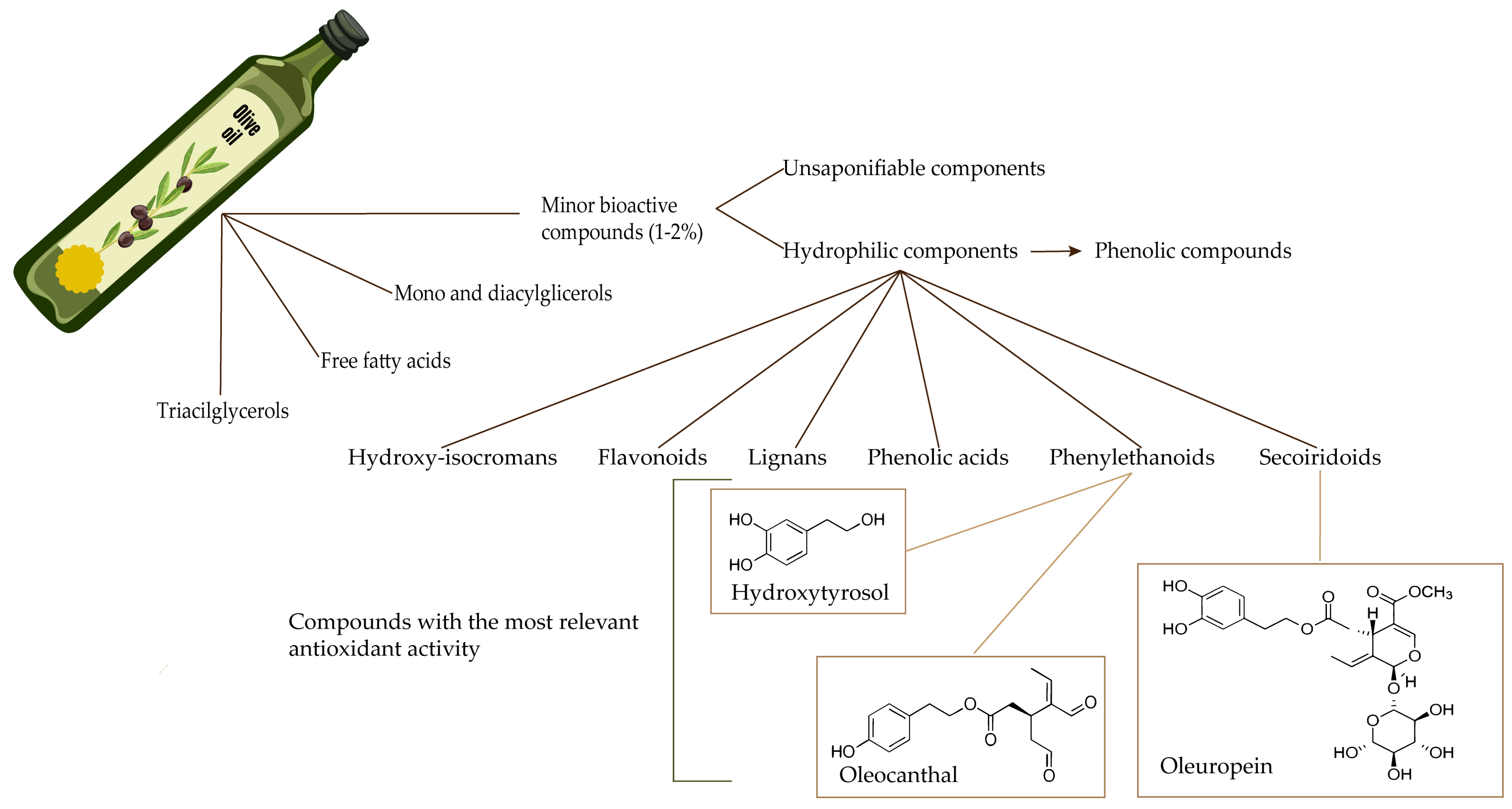
3. Olive Oil Composition
3.1. Detailed Description of Olive Oil’s Chemical Composition, Focusing on Antioxidants like Oleuropein, Hydroxytyrosol, and Oleocanthal
3.1.1. Oleuropein

3.1.2. Hydroxytyrosol
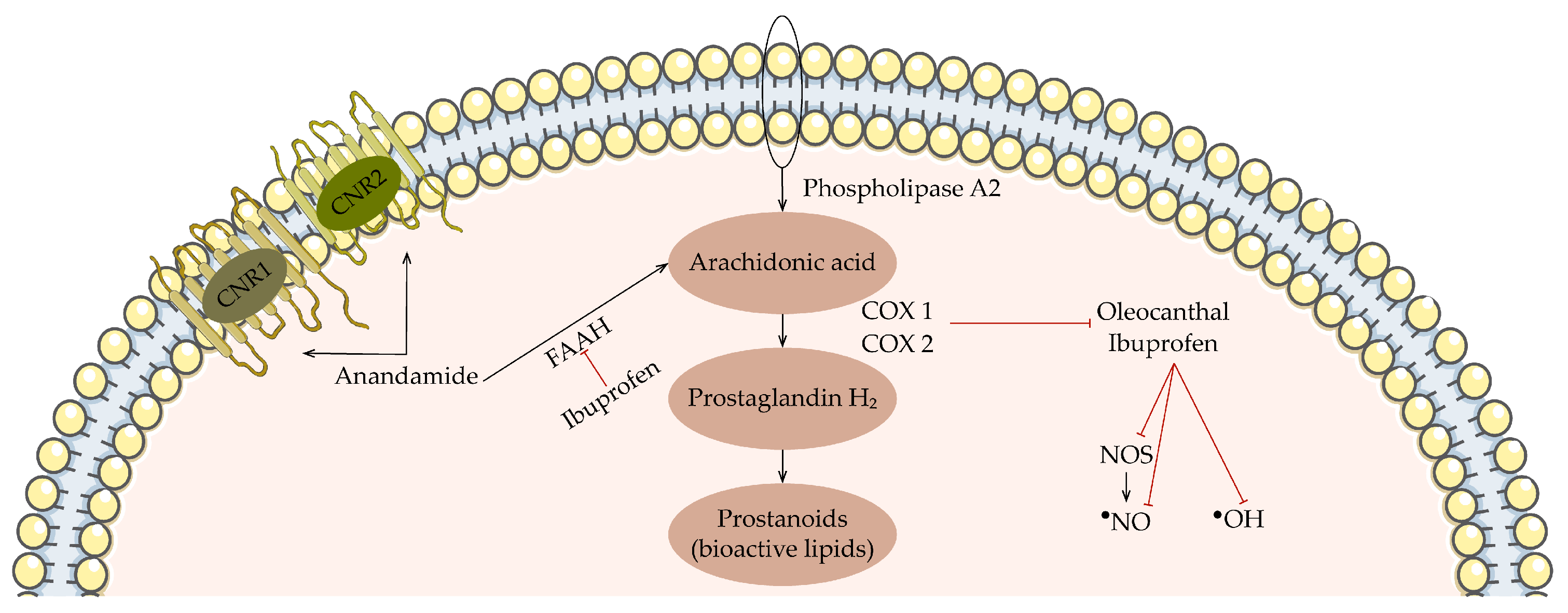
3.1.3. Oleocanthal
3.2. Discussion on the Different Types of Olive Oil and Their Relative Antioxidant Capacities
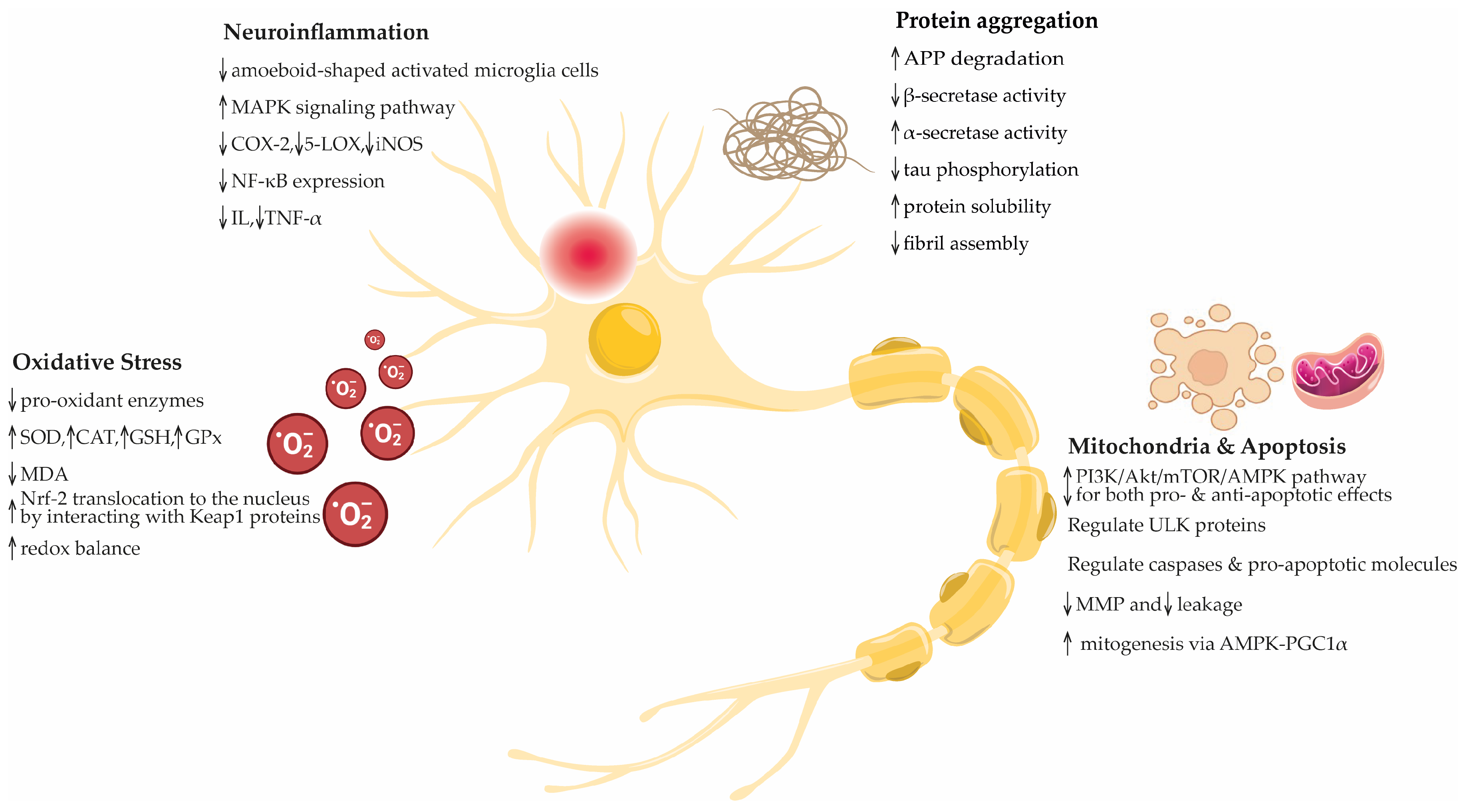
4. Explore How Olive Oil’s Antioxidants Can Potentially Counteract Oxidative Stress in the Brain
4.1. In Vitro Studies
4.2. In Vivo Studies
4.3. Clinical Trials
5. Challenges and Future Directions
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hannan, M.A.; Dash, R.; Sohag, A.A.M.; Haque, M.N.; Moon, I.S. Neuroprotection Against Oxidative Stress: Phytochemicals Targeting TrkB Signaling and the Nrf2-ARE Antioxidant System. Front. Mol. Neurosci. 2020, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Farooqui, A.A. Chapter 1—Molecular aspects of neurodegeneration and classification of neurological disorders. In Molecular Aspects of Neurodegeneration, Neuroprotection, and Regeneration in Neurological Disorders; Farooqui, A.A., Ed.; Academic Press: Cambridge, MA, USA, 2021; pp. 1–40. [Google Scholar]
- Casado, M.E.; Collado-Pérez, R.; Frago, L.M.; Barrios, V. Recent Advances in the Knowledge of the Mechanisms of Leptin Physiology and Actions in Neurological and Metabolic Pathologies. Int. J. Mol. Sci. 2023, 24, 1422. [Google Scholar] [CrossRef] [PubMed]
- Zamanian, M.Y.; Ivraghi, M.S.; Gupta, R.; Prasad, K.D.V.; Alsaab, H.O.; Hussien, B.M.; Ahmed, H.; Ramadan, M.F.; Golmohammadi, M.; Nikbakht, N.; et al. miR-221 and Parkinson’s disease: A biomarker with therapeutic potential. Eur. J. Neurosci. 2024, 59, 283–297. [Google Scholar] [CrossRef]
- Erkkinen, M.G.; Kim, M.-O.; Geschwind, M.D. Clinical Neurology and Epidemiology of the Major Neurodegenerative Diseases. Cold Spring Harb. Perspect. Biol. 2018, 10, a033118. [Google Scholar] [CrossRef] [PubMed]
- Bellou, V.; Belbasis, L.; Tzoulaki, I.; Middleton, L.T.; Ioannidis, J.P.A.; Evangelou, E. Systematic evaluation of the associations between environmental risk factors and dementia: An umbrella review of systematic reviews and meta-analyses. Alzheimers Dement. 2017, 13, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Li, Y.; Pan, H.; Han, L. Global, regional, and national burden of neurological disorders in 204 countries and territories worldwide. J. Glob. Health 2023, 13, 04160. [Google Scholar] [CrossRef]
- Ferini-Strambi, L.; Salsone, M. COVID-19 and neurological disorders: Are neurodegenerative or neuroimmunological diseases more vulnerable? J. Neurol. 2021, 268, 409–419. [Google Scholar] [CrossRef]
- Salis, C.; Papageorgiou, L.; Papakonstantinou, E.; Hagidimitriou, M.; Vlachakis, D. Olive Oil Polyphenols in Neurodegenerative Pathologies. Adv. Exp. Med. Biol. 2020, 1195, 77–91. [Google Scholar] [CrossRef]
- Mohd Sairazi, N.S.; Sirajudeen, K.N.S. Natural Products and Their Bioactive Compounds: Neuroprotective Potentials against Neurodegenerative Diseases. Evid. Based Complement. Alternat. Med. 2020, 2020, 6565396. [Google Scholar] [CrossRef]
- Lamptey, R.N.L.; Chaulagain, B.; Trivedi, R.; Gothwal, A.; Layek, B.; Singh, J. A Review of the Common Neurodegenerative Disorders: Current Therapeutic Approaches and the Potential Role of Nanotherapeutics. Int. J. Mol. Sci. 2022, 23, 1851. [Google Scholar] [CrossRef]
- Park, H.W.; Park, C.G.; Park, M.; Lee, S.H.; Park, H.R.; Lim, J.; Paek, S.H.; Choy, Y.B. Intrastriatal administration of coenzyme Q10 enhances neuroprotection in a Parkinson’s disease rat model. Sci. Rep. 2020, 10, 9572. [Google Scholar] [CrossRef] [PubMed]
- Sheykhhasan, M.; Amini, R.; Soleimani Asl, S.; Saidijam, M.; Hashemi, S.M.; Najafi, R. Neuroprotective effects of coenzyme Q10-loaded exosomes obtained from adipose-derived stem cells in a rat model of Alzheimer’s disease. Biomed. Pharmacother. 2022, 152, 113224. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.; Rodríguez-Pérez, M.; Burgos-Ramos, E. Zebrafish Model Insights into Mediterranean Diet Liquids: Olive Oil and Wine. Antioxidants 2023, 12, 1843. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.; Rodríguez-Pérez, M.; Gómez-Torres, Ó.; Burgos-Ramos, E. Olive oil and wine as source of multi-target agents in the prevention of Alzheimer disease. Nutr. Res. Rev. 2023, 36, 140–154. [Google Scholar] [CrossRef] [PubMed]
- Silva, P.; Vauzour, D. Wine Polyphenols and Neurodegenerative Diseases: An Update on the Molecular Mechanisms Underpinning Their Protective Effects. Beverages 2018, 4, 96. [Google Scholar] [CrossRef]
- Bringas Vega, M.L.; Pedroso Ibáñez, I.; Razzaq, F.A.; Zhang, M.; Morales Chacón, L.; Ren, P.; Galan Garcia, L.; Gan, P.; Virues Alba, T.; Lopez Naranjo, C.; et al. The Effect of Neuroepo on Cognition in Parkinson’s Disease Patients Is Mediated by Electroencephalogram Source Activity. Front. Neurosci. 2022, 16, 841428. [Google Scholar] [CrossRef]
- Peña, G.F.; Hernández, C.L.P.; Guerra, O.I.R.; Romero, T.F. Evidence of the neuroprotective potential of NeuroEPO in preclinical studies and clinical trials: A systematic review. Rev. Habanera Cienc. Med. 2023, 22, 1. [Google Scholar]
- Simpson, D.S.A.; Oliver, P.L. ROS Generation in Microglia: Understanding Oxidative Stress and Inflammation in Neurodegenerative Disease. Antioxidants 2020, 9, 743. [Google Scholar] [CrossRef]
- Shchepinov, M.S. Polyunsaturated Fatty Acid Deuteration against Neurodegeneration. Trends Pharmacol. Sci. 2020, 41, 236–248. [Google Scholar] [CrossRef]
- Ren, J.-X.; Sun, X.; Yan, X.-L.; Guo, Z.-N.; Yang, Y. Ferroptosis in Neurological Diseases. Front. Cell. Neurosci. 2020, 14, 218. [Google Scholar] [CrossRef]
- Misrani, A.; Tabassum, S.; Yang, L. Mitochondrial Dysfunction and Oxidative Stress in Alzheimer’s Disease. Front. Aging Neurosci. 2021, 13, 617588. [Google Scholar] [CrossRef]
- Alqahtani, T.; Deore, S.L.; Kide, A.A.; Shende, B.A.; Sharma, R.; Dadarao Chakole, R.; Nemade, L.S.; Kishor Kale, N.; Borah, S.; Shrikant Deokar, S.; et al. Mitochondrial dysfunction and oxidative stress in Alzheimer’s disease, and Parkinson’s disease, Huntington’s disease and Amyotrophic Lateral Sclerosis—An updated review. Mitochondrion 2023, 71, 83–92. [Google Scholar] [CrossRef]
- Chang, K.-H.; Chen, C.-M. The Role of Oxidative Stress in Parkinson’s Disease. Antioxidants 2020, 9, 597. [Google Scholar] [CrossRef]
- Jurcau, A. Molecular Pathophysiological Mechanisms in Huntington’s Disease. Biomedicines 2022, 10, 1432. [Google Scholar] [CrossRef]
- Cunha-Oliveira, T.; Montezinho, L.; Mendes, C.; Firuzi, O.; Saso, L.; Oliveira, P.J.; Silva, F.S.G. Oxidative Stress in Amyotrophic Lateral Sclerosis: Pathophysiology and Opportunities for Pharmacological Intervention. Oxid. Med. Cell. Longev. 2020, 2020, 5021694. [Google Scholar] [CrossRef]
- Sun, A.Y.; Chen, Y.M. Oxidative stress and neurodegenerative disorders. J. Biomed. Sci. 1998, 5, 401–414. [Google Scholar] [CrossRef]
- Li, J.; Wuliji, O.; Li, W.; Jiang, Z.-G.; Ghanbari, H.A. Oxidative Stress and Neurodegenerative Disorders. Int. J. Mol. Sci. 2013, 14, 24438–24475. [Google Scholar] [CrossRef]
- Cobley, J.N.; Fiorello, M.L.; Bailey, D.M. 13 reasons why the brain is susceptible to oxidative stress. Redox Biol. 2018, 15, 490–503. [Google Scholar] [CrossRef]
- Ballard, C.; Gauthier, S.; Corbett, A.; Brayne, C.; Aarsland, D.; Jones, E. Alzheimer’s disease. Lancet 2011, 377, 1019–1031. [Google Scholar] [CrossRef]
- Blesa, J.; Trigo-Damas, I.; Quiroga-Varela, A.; Jackson-Lewis, V.R. Oxidative stress and Parkinson’s disease. Front. Neuroanat. 2015, 9, 91. [Google Scholar] [CrossRef]
- Dexter, D.T.; Jenner, P. Parkinson disease: From pathology to molecular disease mechanisms. Free Radic. Biol. Med. 2013, 62, 132–144. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Morató, J.; Xicota, L.; Fitó, M.; Farré, M.; Dierssen, M.; De la Torre, R. Potential role of olive oil phenolic compounds in the prevention of neurodegenerative diseases. Molecules 2015, 20, 4655–4680. [Google Scholar] [CrossRef]
- Imarisio, S.; Carmichael, J.; Korolchuk, V.; Chen, C.-W.; Saiki, S.; Rose, C.; Krishna, G.; Davies, J.E.; Ttofi, E.; Underwood, B.R.; et al. Huntington’s disease: From pathology and genetics to potential therapies. Biochem. J. 2008, 412, 191–209. [Google Scholar] [CrossRef]
- Mejzini, R.; Flynn, L.L.; Pitout, I.L.; Fletcher, S.; Wilton, S.D.; Akkari, P.A. ALS Genetics, Mechanisms, and Therapeutics: Where Are We Now? Front. Neurosci. 2019, 13, 1310. [Google Scholar] [CrossRef]
- Dhasmana, S.; Dhasmana, A.; Narula, A.S.; Jaggi, M.; Yallapu, M.M.; Chauhan, S.C. The panoramic view of amyotrophic lateral sclerosis: A fatal intricate neurological disorder. Life Sci. 2022, 288, 120156. [Google Scholar] [CrossRef] [PubMed]
- López-Pingarrón, L.; Almeida, H.; Soria-Aznar, M.; Reyes-Gonzales, M.C.; Terrón, M.P.; García, J.J. Role of Oxidative Stress on the Etiology and Pathophysiology of Amyotrophic Lateral Sclerosis (ALS) and Its Relation with the Enteric Nervous System. Curr. Issues Mol. Biol. 2023, 45, 3315–3332. [Google Scholar] [CrossRef]
- Aran, K.R.; Singh, S. Mitochondrial dysfunction and oxidative stress in Alzheimer’s disease–A step towards mitochondria based therapeutic strategies. Aging Health Res. 2023, 3, 100169. [Google Scholar] [CrossRef]
- Al Shahrani, M.; Heales, S.; Hargreaves, I.; Orford, M. Oxidative Stress: Mechanistic Insights into Inherited Mitochondrial Disorders and Parkinson’s Disease. J. Clin. Med. 2017, 6, 100. [Google Scholar] [CrossRef]
- Bose, A.; Beal, M.F. Mitochondrial dysfunction and oxidative stress in induced pluripotent stem cell models of Parkinson’s disease. Eur. J. Neurosci. 2019, 49, 525–532. [Google Scholar] [CrossRef]
- Kung, H.-C.; Lin, K.-J.; Kung, C.-T.; Lin, T.-K. Oxidative Stress, Mitochondrial Dysfunction, and Neuroprotection of Polyphenols with Respect to Resveratrol in Parkinson’s Disease. Biomedicines 2021, 9, 918. [Google Scholar] [CrossRef]
- Huang, M.; Bargues-Carot, A.; Riaz, Z.; Wickham, H.; Zenitsky, G.; Jin, H.; Anantharam, V.; Kanthasamy, A.; Kanthasamy, A.G. Impact of Environmental Risk Factors on Mitochondrial Dysfunction, Neuroinflammation, Protein Misfolding, and Oxidative Stress in the Etiopathogenesis of Parkinson’s Disease. Int. J. Mol. Sci. 2022, 23, 10808. [Google Scholar] [CrossRef]
- Tobore, T.O. Towards a comprehensive understanding of the contributions of mitochondrial dysfunction and oxidative stress in the pathogenesis and pathophysiology of Huntington’s disease. J. Neurosci. Res. 2019, 97, 1455–1468. [Google Scholar] [CrossRef]
- Chen, C.M. Mitochondrial dysfunction, metabolic deficits, and increased oxidative stress in huntington’s disease. Chang. Gung Med. J. 2011, 34, 135–152. [Google Scholar]
- Roy, R.G.; Mandal, P.K.; Maroon, J.C. Oxidative Stress Occurs Prior to Amyloid Aβ Plaque Formation and Tau Phosphorylation in Alzheimer’s Disease: Role of Glutathione and Metal Ions. ACS Chem. Neurosci. 2023, 14, 2944–2954. [Google Scholar] [CrossRef]
- Plascencia-Villa, G.; Perry, G. Preventive and Therapeutic Strategies in Alzheimer’s Disease: Focus on Oxidative Stress, Redox Metals, and Ferroptosis. Antioxid. Redox Signal. 2021, 34, 591–610. [Google Scholar] [CrossRef]
- Götz, M.E.; Double, K.; Gerlach, M.; Youdim, M.B.H.; Riederere, P. The Relevance of Iron in the Pathogenesis of Parkinson’s Disease. Ann. N. Y. Acad. Sci. 2004, 1012, 193–208. [Google Scholar] [CrossRef]
- Carrì, M.T.; Ferri, A.; Cozzolino, M.; Calabrese, L.; Rotilio, G. Neurodegeneration in amyotrophic lateral sclerosis: The role of oxidative stress and altered homeostasis of metals. Brain Res. Bull. 2003, 61, 365–374. [Google Scholar] [CrossRef]
- Verdile, G.; Keane, K.N.; Cruzat, V.F.; Medic, S.; Sabale, M.; Rowles, J.; Wijesekara, N.; Martins, R.N.; Fraser, P.E.; Newsholme, P. Inflammation and Oxidative Stress: The Molecular Connectivity between Insulin Resistance, Obesity, and Alzheimer’s Disease. Mediat. Inflamm. 2015, 2015, 105828. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Gutierrez, E.; Muñoz-Arenas, G.; Treviño, S.; Espinosa, B.; Chavez, R.; Rojas, K.; Flores, G.; Díaz, A.; Guevara, J. Alzheimer’s disease and metabolic syndrome: A link from oxidative stress and inflammation to neurodegeneration. Synapse 2017, 71, e21990. [Google Scholar] [CrossRef]
- Bisht, K.; Sharma, K.; Tremblay, M.È. Chronic stress as a risk factor for Alzheimer’s disease: Roles of microglia-mediated synaptic remodeling, inflammation, and oxidative stress. Neurobiol. Stress. 2018, 9, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.; Dong, X.; Chen, M.; Zou, Z. Efficacy of probiotics on cognition, and biomarkers of inflammation and oxidative stress in adults with Alzheimer’s disease or mild cognitive impairment-A meta-analysis of randomized controlled trials. Aging 2020, 12, 4010–4039. [Google Scholar] [CrossRef]
- Hendrickx, J.O.; Martinet, W.; Van Dam, D.; De Meyer, G.R.Y. Inflammation, Nitro-Oxidative Stress, Impaired Autophagy, and Insulin Resistance as a Mechanistic Convergence Between Arterial Stiffness and Alzheimer’s Disease. Front. Mol. Biosci. 2021, 8, 651215. [Google Scholar] [CrossRef] [PubMed]
- Shabbir, U.; Tyagi, A.; Elahi, F.; Aloo, S.O.; Oh, D.H. The potential role of polyphenols in oxidative stress and inflammation induced by gut microbiota in alzheimer’s disease. Antioxidants 2021, 10, 1370. [Google Scholar] [CrossRef] [PubMed]
- Das, T.K.; Ganesh, B.P. Interlink between the gut microbiota and inflammation in the context of oxidative stress in Alzheimer’s disease progression. Gut Microbes 2023, 15, 2206504. [Google Scholar] [CrossRef] [PubMed]
- Valverde-Salazar, V.; Ruiz-Gabarre, D.; García-Escudero, V. Alzheimer’s Disease and Green Tea: Epigallocatechin-3-Gallate as a Modulator of Inflammation and Oxidative Stress. Antioxidants 2023, 12, 1460. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, K.; Rahimmi, A. Oxidative stress and neuroinflammation in the story of Parkinson’s disease: Could targeting these pathways write a good ending? J. Cell. Physiol. 2019, 234, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Vallée, A.; Lecarpentier, Y.; Guillevin, R.; Vallée, J.-N. Circadian rhythms, Neuroinflammation and Oxidative Stress in the Story of Parkinson’s Disease. Cells 2020, 9, 314. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, S.; Bisaglia, M. Oxidative Stress and Neuroinflammation in Parkinson’s Disease: The Role of Dopamine Oxidation Products. Antioxidants 2023, 12, 955. [Google Scholar] [CrossRef] [PubMed]
- Park, H.R.; Yang, E.J. Oxidative Stress as a Therapeutic Target in Amyotrophic Lateral Sclerosis: Opportunities and Limitations. Diagnostics 2021, 11, 1546. [Google Scholar] [CrossRef]
- Chang, Y.T.; Chang, W.N.; Tsai, N.W.; Huang, C.C.; Kung, C.T.; Su, Y.J.; Lin, W.C.; Cheng, B.C.; Su, C.M.; Chiang, Y.F.; et al. The roles of biomarkers of oxidative stress and antioxidant in alzheimer’s disease: A systematic review. BioMed Res. Int. 2014, 2014, 182303. [Google Scholar] [CrossRef]
- Ferreira, M.E.S.; de Vasconcelos, A.S.; da Costa Vilhena, T.; da Silva, T.L.; da Silva Barbosa, A.; Gomes, A.R.Q.; Dolabela, M.F.; Percário, S. Oxidative Stress in Alzheimer’s Disease: Should We Keep Trying Antioxidant Therapies? Cell. Mol. Neurobiol. 2015, 35, 595–614. [Google Scholar] [CrossRef] [PubMed]
- Hallam, R.D. Bolstered Neuronal Antioxidant Response May Confer Resistance to Development of Dementia in Individuals with Alzheimer’s Neuropathology by Ameliorating Amyloid-β-Induced Oxidative Stress. J. Neurosci. 2021, 41, 6187–6189. [Google Scholar] [CrossRef] [PubMed]
- Percário, S.; Da Silva Barbosa, A.; Varela, E.L.P.; Gomes, A.R.Q.; Ferreira, M.E.S.; De Nazaré Araújo Moreira, T.; Dolabela, M.F. Oxidative Stress in Parkinson’s Disease: Potential Benefits of Antioxidant Supplementation. Oxid. Med. Cell. Longev. 2020, 2020, 2360872. [Google Scholar] [CrossRef]
- Gil-Mohapel, J.; Brocardo, P.S.; Christie, B.R. The role of oxidative stress in Huntington’s disease: Are antioxidants good therapeutic candidates? Curr. Drug Targets 2014, 15, 454–468. [Google Scholar] [CrossRef] [PubMed]
- Hemerková, P.; Vališ, M. Role of oxidative stress in the pathogenesis of amyotrophic lateral sclerosis: Antioxidant metalloenzymes and therapeutic strategies. Biomolecules 2021, 11, 437. [Google Scholar] [CrossRef] [PubMed]
- Velez-Pardo, C.; Del Rio, M.J.; Lopera, F. Familial Alzheimer’s disease: Oxidative stress, β-amyloid, presenilins, and cell death. Gen. Pharmacol. 1998, 31, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Butterfield, D.A.; Mattson, M.P. Apolipoprotein E and oxidative stress in brain with relevance to Alzheimer’s disease. Neurobiol. Dis. 2020, 138, 104795. [Google Scholar] [CrossRef] [PubMed]
- Candore, G.; Bulati, M.; Caruso, C.; Castiglia, L.; Colonna-Romano, G.; Di Bona, D.; Duro, G.; Lio, D.; Matranga, D.; Pellicanò, M.; et al. Inflammation, cytokines, immune response, apolipoprotein E, cholesterol, and oxidative stress in alzheimer disease: Therapeutic implications. Rejuvenation Res. 2010, 13, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Botchway, B.O.; Okoye, F.C.; Chen, Y.; Arthur, W.E.; Fang, M. Alzheimer Disease: Recent Updates on Apolipoprotein E and Gut Microbiome Mediation of Oxidative Stress, and Prospective Interventional Agents. Aging Dis. 2022, 13, 87. [Google Scholar] [CrossRef] [PubMed]
- Goncharova, Z.A.; Kolmakova, T.S.; Gelpei, M.A. Alpha-synuclein and oxidative stress enzymes as biomarkers of Parkinson’s disease. Neurochem. J. 2017, 11, 121–128. [Google Scholar] [CrossRef]
- Luk, K.C. Oxidative stress and α-synuclein conspire in vulnerable neurons to promote Parkinson’s disease progression. J. Clin. Investig. 2019, 129, 3530–3531. [Google Scholar] [CrossRef] [PubMed]
- Kahle, P.J.; Waak, J.; Gasser, T. DJ-1 and prevention of oxidative stress in Parkinson’s disease and other age-related disorders. Free Radic. Biol. Med. 2009, 47, 1354–1361. [Google Scholar] [CrossRef]
- Pyatha, S.; Kim, H.; Lee, D.; Kim, K. Association between Heavy Metal Exposure and Parkinson’s Disease: A Review of the Mechanisms Related to Oxidative Stress. Antioxidants 2022, 11, 2467. [Google Scholar] [CrossRef] [PubMed]
- Mo, C.; Hannan, A.J.; Renoir, T. Environmental factors as modulators of neurodegeneration: Insights from gene-environment interactions in Huntington’s disease. Neurosci. Biobehav. Rev. 2015, 52, 178–192. [Google Scholar] [CrossRef] [PubMed]
- Motataianu, A.; Serban, G.; Barcutean, L.; Balasa, R. Oxidative Stress in Amyotrophic Lateral Sclerosis: Synergy of Genetic and Environmental Factors. Int. J. Mol. Sci. 2022, 23, 9339. [Google Scholar] [CrossRef] [PubMed]
- Behl, C. Amyloid β-protein toxicity and oxidative stress in Alzheimer’s disease. Cell Tissue Res. 1997, 290, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Abramov, A.Y.; Potapova, E.V.; Dremin, V.V.; Dunaev, A.V. Interaction of Oxidative Stress and Misfolded Proteins in the Mechanism of Neurodegeneration. Life 2020, 10, 101. [Google Scholar] [CrossRef]
- Inglese, P.; Famiani, F.; Galvano, F.; Servili, M.; Esposto, S.; Urbani, S. 3 factors affecting extra-virgin olive oil composition. Hortic. Rev. 2011, 38, 83. [Google Scholar]
- Boskou, D.; Blekas, G.; Tsimidou, M. 4—Olive Oil Composition. In Olive Oil, 2nd ed.; Boskou, D., Ed.; AOCS Press: Urbana, IL, USA, 2006; pp. 41–72. [Google Scholar]
- Covas, M.-I.; Ruiz-Gutiérrez, V.; de la Torre, R.; Kafatos, A.; Lamuela-Raventós, R.M.; Osada, J.; Owen, R.W.; Visioli, F. Minor Components of Olive Oil: Evidence to Date of Health Benefits in Humans. Nutr. Rev. 2006, 64, S20–S30. [Google Scholar] [CrossRef]
- Alonso-Salces, R.M.; Segebarth, N.; Garmón-Lobato, S.; Holland, M.V.; Moreno-Rojas, J.M.; Fernández-Pierna, J.A.; Baeten, V.; Fuselli, S.R.; Gallo, B.; Berrueta, L.A.; et al. 1H-NMR and isotopic fingerprinting of olive oil and its unsaponifiable fraction: Geographical origin of virgin olive oils by pattern recognition. Eur. J. Lipid Sci. Technol. 2015, 117, 1991–2006. [Google Scholar] [CrossRef]
- Sánchez, J.; Harwood, J.L. Biosynthesis of triacylglycerols and volatiles in olives. Eur. J. Lipid Sci. Technol. 2002, 104, 564–573. [Google Scholar] [CrossRef]
- Conde, C.; Delrot, S.; Gerós, H. Physiological, biochemical and molecular changes occurring during olive development and ripening. J. Plant Physiol. 2008, 165, 1545–1562. [Google Scholar] [CrossRef]
- Gomes, T.; Caponio, F.; Bruno, G.; Summo, C.; Paradiso, V.M. Effects of monoacylglycerols on the oxidative stability of olive oil. J. Sci. Food Agric. 2010, 90, 2228–2232. [Google Scholar] [CrossRef]
- Senbagalakshmi, P.; Muthukrishnan, S.; Jebasingh, T.; Kumar, T.S.; Rao, M.; Kumar, T.S.; Rao, M. Squalene, biosynthesis and its role in production of bioactive compounds, a proper scientific challenge—A review. J. Emerg. Technol. Innov. Res. 2019, 6, 505–526. [Google Scholar]
- Serreli, G.; Deiana, M. Biological Relevance of Extra Virgin Olive Oil Polyphenols Metabolites. Antioxidants 2018, 7, 170. [Google Scholar] [CrossRef]
- Seray, K. Olive Oil: Antioxidant Compounds and Their Potential Effects over Health. In Funct Foods; Vasiliki, L., Ed.; IntechOpen: Rijeka, Croatia, 2018; p. Ch. 2. [Google Scholar]
- Gonçalves, M.; Rodríguez-Pérez, M.; Calabrò, A.; Burgos-Ramos, E.; Accardi, G.; Silva, P. A Narrative Review of Metabolomic Insights into Olive Oil’s Nutritional Value. Appl. Sci. 2024, 14, 4203. [Google Scholar] [CrossRef]
- Carrera-González, M.P.; Ramírez-Expósito, M.J.; Mayas, M.D.; Martínez-Martos, J.M. Protective role of oleuropein and its metabolite hydroxytyrosol on cancer. Trends Food Sci. Technol. 2013, 31, 92–99. [Google Scholar] [CrossRef]
- Ozdemir, Y.; Guven, E.; Ozturk, A. Understanding the characteristics of oleuropein for table olive processing. J. Food Process. Technol. 2014, 5, 5. [Google Scholar]
- Cavaca, L.A.S.; López-Coca, I.M.; Silvero, G.; Afonso, C.A.M. Chapter 5—The olive-tree leaves as a source of high-added value molecules: Oleuropein. In Studies in Natural Products Chemistry; Atta Ur, R., Ed.; Elsevier: Amsterdam, The Netherlands, 2020; Volume 64, pp. 131–180. [Google Scholar]
- Bulotta, S.; Celano, M.; Lepore, S.M.; Montalcini, T.; Pujia, A.; Russo, D. Beneficial effects of the olive oil phenolic components oleuropein and hydroxytyrosol: Focus on protection against cardiovascular and metabolic diseases. J. Transl. Med. 2014, 12, 219. [Google Scholar] [CrossRef]
- Fantini, M.; Benvenuto, M.; Masuelli, L.; Frajese, G.V.; Tresoldi, I.; Modesti, A.; Bei, R. In Vitro and in Vivo Antitumoral Effects of Combinations of Polyphenols, or Polyphenols and Anticancer Drugs: Perspectives on Cancer Treatment. Int. J. Mol. Sci. 2015, 16, 9236–9282. [Google Scholar] [CrossRef]
- Keceli, T.M.; Kamiloglu, S.; Capanoglu, E. Phenolic Compounds of Olives and Olive Oil and their Bioavailability. In Olives and Olive Oil as Functional Foods; Wiley: Hoboken, NJ, USA, 2017; pp. 457–470. [Google Scholar]
- Ruzzolini, J.; Peppicelli, S.; Andreucci, E.; Bianchini, F.; Scardigli, A.; Romani, A.; La Marca, G.; Nediani, C.; Calorini, L. Oleuropein, the Main Polyphenol of Olea europaea Leaf Extract, Has an Anti-Cancer Effect on Human BRAF Melanoma Cells and Potentiates the Cytotoxicity of Current Chemotherapies. Nutrients 2018, 10, 1950. [Google Scholar] [CrossRef]
- Lemonakis, N.; Mougios, V.; Halabalaki, M.; Skaltsounis, A.L.; Gikas, E. A novel bioanalytical method based on UHPLC-HRMS/MS for the quantification of oleuropein in human serum. Application to a pharmacokinetic study. Biomed. Chromatogr. 2016, 30, 2016–2023. [Google Scholar] [CrossRef] [PubMed]
- Obied, H.K.; Prenzler, P.D.; Ryan, D.; Servili, M.; Taticchi, A.; Esposto, S.; Robards, K. Biosynthesis and biotransformations of phenol-conjugated oleosidic secoiridoids from Olea europaea L. Nat. Prod. Rep. 2008, 25, 1167–1179. [Google Scholar] [CrossRef]
- Hassen, I.; Casabianca, H.; Hosni, K. Biological activities of the natural antioxidant oleuropein: Exceeding the expectation–A mini-review. J. Funct. Foods 2015, 18, 926–940. [Google Scholar] [CrossRef]
- Yoon, S.K. Oleuropein as an antioxidant and liver protect. Liver 2018, 323–335. [Google Scholar] [CrossRef]
- Wani, T.A.; Masoodi, F.; Gani, A.; Baba, W.N.; Rahmanian, N.; Akhter, R.; Wani, I.A.; Ahmad, M. Olive oil and its principal bioactive compound: Hydroxytyrosol–A review of the recent literature. Trends Food Sci. Technol. 2018, 77, 77–90. [Google Scholar] [CrossRef]
- Robles-Almazan, M.; Pulido-Moran, M.; Moreno-Fernandez, J.; Ramirez-Tortosa, C.; Rodriguez-Garcia, C.; Quiles, J.L.; Ramirez-Tortosa, M. Hydroxytyrosol: Bioavailability, toxicity, and clinical applications. Food Res. Int. 2018, 105, 654–667. [Google Scholar] [CrossRef]
- Chen, C.; Ai, Q.-d.; Wei, Y.-h. Potential role of hydroxytyrosol in neuroprotection. J. Funct. Foods 2021, 82, 104506. [Google Scholar] [CrossRef]
- Charoenprasert, S.; Mitchell, A. Factors Influencing Phenolic Compounds in Table Olives (Olea europaea). J. Agric. Food Chem. 2012, 60, 7081–7095. [Google Scholar] [CrossRef]
- Sánchez, R.; García-Vico, L.; Sanz, C.; Pérez, A.G. An Aromatic Aldehyde Synthase Controls the Synthesis of Hydroxytyrosol Derivatives Present in Virgin Olive Oil. Antioxidants 2019, 8, 352. [Google Scholar] [CrossRef]
- Zhang, B.; Zhang, Y.; Xing, X.; Wang, S. Health benefits of dietary polyphenols: Insight into interindividual variability in absorption and metabolism. Curr. Opin. Food Sci. 2022, 48, 100941. [Google Scholar] [CrossRef]
- Suárez, M.; Valls, R.M.; Romero, M.-P.; Macià, A.; Fernández, S.; Giralt, M.; Solà, R.; Motilva, M.-J. Bioavailability of phenols from a phenol-enriched olive oil. Br. J. Nutr. 2011, 106, 1691–1701. [Google Scholar] [CrossRef]
- Echeverría, F.; Ortiz, M.; Valenzuela, R.; Videla, L.A. Hydroxytyrosol and Cytoprotection: A Projection for Clinical Interventions. Int. J. Mol. Sci. 2017, 18, 930. [Google Scholar] [CrossRef]
- López de las Hazas, M.-C.; Piñol, C.; Macià, A.; Romero, M.-P.; Pedret, A.; Solà, R.; Rubió, L.; Motilva, M.-J. Differential absorption and metabolism of hydroxytyrosol and its precursors oleuropein and secoiridoids. J. Funct. Foods 2016, 22, 52–63. [Google Scholar] [CrossRef]
- Aydar, A.; Öner, T.Ö.; Ücok, E. Effects of hydroxytyrosol on human health. EC Nutr. 2017, 11, 147–157. [Google Scholar]
- Montedoro, G.F.; Servili, M.; Baldioli, M.; Selvaggini, R.; Miniati, E.; Macchioni, A. Simple and hydrolyzable compounds in virgin olive oil. 3. Spectroscopic characterizations of the secoiridoid derivatives. J. Agric. Food Chem. 1993, 41, 2228–2234. [Google Scholar] [CrossRef]
- Scotece, M.; Conde, J.; Abella, V.; Lopez, V.; Pino, J.; Lago, F.; Smith, A.B.; Gómez-Reino, J.J.; Gualillo, O. New drugs from ancient natural foods. Oleocanthal, the natural occurring spicy compound of olive oil: A brief history. Drug Discov. Today 2015, 20, 406–410. [Google Scholar] [CrossRef]
- Francisco, V.; Ruiz-Fernández, C.; Lahera, V.; Lago, F.; Pino, J.; Skaltsounis, L.; González-Gay, M.A.; Mobasheri, A.; Gómez, R.; Scotece, M.; et al. Natural Molecules for Healthy Lifestyles: Oleocanthal from Extra Virgin Olive Oil. J. Agric. Food Chem. 2019, 67, 3845–3853. [Google Scholar] [CrossRef]
- Valli, M.; Peviani, E.G.; Porta, A.; D’Alfonso, A.; Zanoni, G.; Vidari, G. A Concise and Efficient Total Synthesis of Oleocanthal. Eur. J. Org. Chem. 2013, 2013, 4332–4336. [Google Scholar] [CrossRef]
- Sarikaki, G.; Christoforidou, N.; Gaboriaud-Kolar, N.; Smith, A.B., III; Kostakis, I.K.; Skaltsounis, A.-L. Biomimetic Synthesis of Oleocanthal, Oleacein, and Their Analogues Starting from Oleuropein, A Major Compound of Olive Leaves. J. Nat. Prod. 2020, 83, 1735–1739. [Google Scholar] [CrossRef]
- Martins, B.T.; Bronze, M.R.; Ventura, M.R. Asymmetric Synthesis of Oleocanthal and Oleacein. Available online: https://webstorage.cienciaviva.pt/public/pt.encontrociencia.www/2021/posters/582_20210614103103_poster_BM.pdf (accessed on 25 May 2024).
- López-Yerena, A.; Vallverdú-Queralt, A.; Jáuregui, O.; Garcia-Sala, X.; Lamuela-Raventós, R.M.; Escribano-Ferrer, E. Tissue Distribution of Oleocanthal and Its Metabolites after Oral Ingestion in Rats. Antioxidants 2021, 10, 688. [Google Scholar] [CrossRef]
- Cuffaro, D.; Pinto, D.; Silva, A.M.; Bertolini, A.; Bertini, S.; Saba, A.; Macchia, M.; Rodrigues, F.; Digiacomo, M. Insights into the Antioxidant/Antiradical Effects and In Vitro Intestinal Permeation of Oleocanthal and Its Metabolites Tyrosol and Oleocanthalic Acid. Molecules 2023, 28, 5150. [Google Scholar] [CrossRef]
- Nikou, T.; Karampetsou, K.V.; Koutsoni, O.S.; Skaltsounis, A.-L.; Dotsika, E.; Halabalaki, M. Pharmacokinetics and Metabolism Investigation of Oleocanthal. J. Nat. Prod. 2024, 87, 530–543. [Google Scholar] [CrossRef]
- Lozano-Castellón, J.; López-Yerena, A.; Rinaldi de Alvarenga, J.F.; Romero del Castillo-Alba, J.; Vallverdú-Queralt, A.; Escribano-Ferrer, E.; Lamuela-Raventós, R.M. Health-promoting properties of oleocanthal and oleacein: Two secoiridoids from extra-virgin olive oil. Crit. Rev. Food Sci. Nutr. 2020, 60, 2532–2548. [Google Scholar] [CrossRef]
- Kiritsakis, A.; Shahidi, F.; Anousakis, C. Antioxidants of Olive Oil, Olive Leaves, and their Bioactivity. In Olives and Olive Oil as Functional Foods; Wiley: Hoboken, NJ, USA, 2017; pp. 367–382. [Google Scholar]
- Lucas, L.; Russell, A.; Keast, R. Molecular mechanisms of inflammation. Anti-inflammatory benefits of virgin olive oil and the phenolic compound oleocanthal. Curr. Pharm. Des. 2011, 17, 754–768. [Google Scholar] [CrossRef]
- Mazaleuskaya, L.L.; Theken, K.N.; Gong, L.; Thorn, C.F.; FitzGerald, G.A.; Altman, R.B.; Klein, T.E. PharmGKB summary: Ibuprofen pathways. Pharmacogenet Genom. 2015, 25, 96–106. [Google Scholar] [CrossRef]
- Rainsford, K.D. Ibuprofen: Pharmacology, efficacy and safety. Inflammopharmacology 2009, 17, 275–342. [Google Scholar] [CrossRef]
- Commission, E. Council Regulation (EC) No 1234/2007 of 22 October 2007 establishing a common organisation of agricultural markets and on specific provisions for certain agricultural products (Single CMO Regulation). Off. J. L 2007, 299, 1–149. [Google Scholar]
- Schwingshackl, L.; Krause, M.; Schmucker, C.; Hoffmann, G.; Rücker, G.; Meerpohl, J.J. Impact of different types of olive oil on cardiovascular risk factors: A systematic review and network meta-analysis. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 1030–1039. [Google Scholar] [CrossRef]
- Kiritsakis, A.; Markakis, P. Olive oil: A review. Adv. Food Res. 1988, 31, 453–482. [Google Scholar]
- Jimenez-Lopez, C.; Carpena, M.; Lourenço-Lopes, C.; Gallardo-Gomez, M.; Lorenzo, J.M.; Barba, F.J.; Prieto, M.A.; Simal-Gandara, J. Bioactive Compounds and Quality of Extra Virgin Olive Oil. Foods 2020, 9, 1014. [Google Scholar] [CrossRef]
- Fanali, C.; Della Posta, S.; Vilmercati, A.; Dugo, L.; Russo, M.; Petitti, T.; Mondello, L.; de Gara, L. Extraction, Analysis, and Antioxidant Activity Evaluation of Phenolic Compounds in Different Italian Extra-Virgin Olive Oils. Molecules 2018, 23, 3249. [Google Scholar] [CrossRef]
- Ramos-Escudero, F.; Morales, M.T.; Asuero, A.G. Characterization of Bioactive Compounds from Monovarietal Virgin Olive Oils: Relationship Between Phenolic Compounds-Antioxidant Capacities. Int. J. Food Prop. 2015, 18, 348–358. [Google Scholar] [CrossRef]
- Frangipane, M.T.; Costantini, L.; Merendino, N.; Massantini, R. Antioxidant Profile and Sensory Analysis in Olive Oils of Different Quality Grades. Agriculture 2023, 13, 993. [Google Scholar] [CrossRef]
- Szydłowska-Czerniak, A.; Karlovits, G.; Dianoczki, C.; Recseg, K.; Szłyk, E. Comparison of Two Analytical Methods for Assessing Antioxidant Capacity of Rapeseed and Olive Oils. J. Am. Oil Chem. Soc. 2008, 85, 141–149. [Google Scholar] [CrossRef]
- Gallardo-Fernandez, M.; Garcia, A.R.; Hornedo-Ortega, R.; Troncoso, A.M.; Garcia-Parrilla, M.C.; Brito, M.A. In vitro study of the blood–brain barrier transport of bioactives from Mediterranean foods. Food Funct. 2024, 15, 3420–3432. [Google Scholar] [CrossRef] [PubMed]
- Karković Marković, A.; Torić, J.; Barbarić, M.; Jakobušić Brala, C. Hydroxytyrosol, Tyrosol and Derivatives and Their Potential Effects on Human Health. Molecules 2019, 24, 2001. [Google Scholar] [CrossRef] [PubMed]
- Butt, M.S.; Tariq, U.; Iahtisham-Ul-Haq; Naz, A.; Rizwan, M. Neuroprotective effects of oleuropein: Recent developments and contemporary research. J. Food Biochem. 2021, 45, e13967. [Google Scholar] [CrossRef]
- Angeloni, C.; Malaguti, M.; Barbalace, M.C.; Hrelia, S. Bioactivity of Olive Oil Phenols in Neuroprotection. Int. J. Mol. Sci. 2017, 18, 2230. [Google Scholar] [CrossRef]
- Mohagheghi, F.; Bigdeli, M.R.; Rasoulian, B.; Hashemi, P.; Pour, M.R. The neuroprotective effect of olive leaf extract is related to improved blood–brain barrier permeability and brain edema in rat with experimental focal cerebral ischemia. Phytomedicine 2011, 18, 170–175. [Google Scholar] [CrossRef]
- Qosa, H.; Batarseh, Y.S.; Mohyeldin, M.M.; El Sayed, K.A.; Keller, J.N.; Kaddoumi, A. Oleocanthal Enhances Amyloid-β Clearance from the Brains of TgSwDI Mice and in Vitro across a Human Blood-Brain Barrier Model. ACS Chem. Neurosci. 2015, 6, 1849–1859. [Google Scholar] [CrossRef]
- Ontario, M.; Siracusa, R.; Modafferi, S.; Scuto, M.; Sciuto, S.; Greco, V.; Bertuccio, M.; Trovato, A.; Crea, R.; Calabrese, E.; et al. Potential prevention and treatment of neurodegenerative disorders by olive polyphenols and hidrox. Mech. Ageing Dev. 2022, 203, 111637. [Google Scholar] [CrossRef]
- Johnson, D.A.; Johnson, J.A. Nrf2--a therapeutic target for the treatment of neurodegenerative diseases. Free Radic. Biol. Med. 2015, 88, 253–267. [Google Scholar] [CrossRef]
- Carito, V.; Ceccanti, M.; Tarani, L.; Ferraguti, G.; Chaldakov, G.N.; Fiore, M. Neurotrophins’ Modulation by Olive Polyphenols. Curr. Med. Chem. 2016, 23, 3189–3197. [Google Scholar] [CrossRef]
- Li, C.; Jackson, R.M. Reactive species mechanisms of cellular hypoxia-reoxygenation injury. Am. J. Physiol. Cell Physiol. 2002, 282, C227–C241. [Google Scholar] [CrossRef]
- C Correia, S.; Carvalho, C.; Cardoso, S.; X Santos, R.; I Plácido, A.; Candeias, E.; I Duarte, A.; I Moreira, P. Defective HIF signaling pathway and brain response to hypoxia in neurodegenerative diseases: Not an “iffy” question! Curr. Pharm. Des. 2013, 19, 6809–6822. [Google Scholar] [CrossRef]
- González-Correa, J.A.; Muñoz-Marín, J.; Arrebola, M.M.; Guerrero, A.; Narbona, F.; López-Villodres, J.A.; De La Cruz, J.P. Dietary virgin olive oil reduces oxidative stress and cellular damage in rat brain slices subjected to hypoxia-reoxygenation. Lipids 2007, 42, 921–929. [Google Scholar] [CrossRef]
- Abdallah, I.M.; Al-Shami, K.M.; Yang, E.; Wang, J.; Guillaume, C.; Kaddoumi, A. Oleuropein-rich olive leaf extract attenuates neuroinflammation in the Alzheimer’s disease mouse model. ACS Chem. Neurosci. 2022, 13, 1002–1013. [Google Scholar] [CrossRef]
- Khalatbary, A.R. Olive oil phenols and neuroprotection. Nutr. Neurosci. 2013, 16, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Al Rihani, S.B.; Darakjian, L.I.; Kaddoumi, A. Oleocanthal-Rich Extra-Virgin Olive Oil Restores the Blood-Brain Barrier Function through NLRP3 Inflammasome Inhibition Simultaneously with Autophagy Induction in TgSwDI Mice. ACS Chem. Neurosci. 2019, 10, 3543–3554. [Google Scholar] [CrossRef] [PubMed]
- Peng, S.; Zhang, B.; Yao, J.; Duan, D.; Fang, J. Dual protection of hydroxytyrosol, an olive oil polyphenol, against oxidative damage in PC12 cells. Food Funct. 2015, 6, 2091–2100. [Google Scholar] [CrossRef]
- Zheng, A.; Li, H.; Xu, J.; Cao, K.; Li, H.; Pu, W.; Yang, Z.; Peng, Y.; Long, J.; Liu, J.; et al. Hydroxytyrosol improves mitochondrial function and reduces oxidative stress in the brain of db/db mice: Role of AMP-activated protein kinase activation. Br. J. Nutr. 2015, 113, 1667–1676. [Google Scholar] [CrossRef]
- Crespo, M.C.; Tomé-Carneiro, J.; Pintado, C.; Dávalos, A.; Visioli, F.; Burgos-Ramos, E. Hydroxytyrosol restores proper insulin signaling in an astrocytic model of Alzheimer’s disease. BioFactors 2017, 43, 540–548. [Google Scholar] [CrossRef]
- Gallardo-Fernández, M.; Hornedo-Ortega, R.; Alonso-Bellido, I.M.; Rodríguez-Gómez, J.A.; Troncoso, A.M.; García-Parrilla, M.C.; Venero, J.L.; Espinosa-Oliva, A.M.; de Pablos, R.M. Hydroxytyrosol decreases lps-and α-synuclein-induced microglial activation in vitro. Antioxidants 2020, 9, 36. [Google Scholar] [CrossRef]
- González-Correa, J.A.; Navas, M.D.; Lopez-Villodres, J.A.; Trujillo, M.; Espartero, J.L.; De La Cruz, J.P. Neuroprotective effect of hydroxytyrosol and hydroxytyrosol acetate in rat brain slices subjected to hypoxia-reoxygenation. Neurosci. Lett. 2008, 446, 143–146. [Google Scholar] [CrossRef]
- Gallardo-Fernández, M.; Hornedo-Ortega, R.; Cerezo, A.B.; Troncoso, A.M.; Garcia-Parrilla, M.C. Hydroxytyrosol and dopamine metabolites: Anti-aggregative effect and neuroprotective activity against α-synuclein-induced toxicity. Food Chem. Toxicol. 2023, 171, 113542. [Google Scholar] [CrossRef]
- Guerrero, A.; De La Cruz, J.P.; Muñoz-Marín, J.; López-Villodres, J.A.; Madrona, A.; Espartero, J.L.; González-Correa, J.A. Neuroprotective effect of alkyl hydroxytyrosyl ethers in rat brain slices subjected to a hypoxia-reoxygenation model. Food Chem. 2012, 134, 2176–2183. [Google Scholar] [CrossRef]
- Hernández-García, S.; García-Cano, B.; Martínez-Rodríguez, P.; Henarejos-Escudero, P.; Gandía-Herrero, F. Olive oil tyrosols reduce α-synuclein aggregation in vitro and in vivo after ingestion in a Caenorhabditis elegans Parkinson’s model. Food Funct. 2024. [Google Scholar] [CrossRef]
- De La Cruz, J.P.; Ruiz-Moreno, M.I.; Guerrero, A.; López-Villodres, J.A.; Reyes, J.J.; Espartero, J.L.; Labajos, M.T.; González-Correa, J.A. Role of the catechol group in the antioxidant and neuroprotective effects of virgin olive oil components in rat brain. J. Nutr. Biochem. 2015, 26, 549–555. [Google Scholar] [CrossRef]
- Giacomazza, D.; D’Andrea, D.; Provenzano, A.; Picone, P.; Provenzano, F.; Guarrasi, V.; Raimondo, M.; San Biagio, P.L.; Passantino, R.; Mangione, M.R.; et al. The precious content of the olive mill wastewater: The protective effect of the antioxidant fraction in cell cultures. CYTA—J. Food 2018, 16, 658–666. [Google Scholar] [CrossRef]
- De La Cruz Cortés, J.P.; Pérez de Algaba, I.; Martín-aurioles, E.; Arrebola, M.M.; Ortega-hombrados, L.; Rodríguez-pérez, M.D.; Fernández-prior, M.Á.; Bermúdez-oria, A.; Verdugo, C.; González-correa, J.A. Extra virgin oil polyphenols improve the protective effects of hydroxytyrosol in an in vitro model of hypoxia–reoxygenation of rat brain. Brain Sci. 2021, 11, 1133. [Google Scholar] [CrossRef] [PubMed]
- Lambert de Malezieu, M.; Courtel, P.; Sleno, L.; Abasq, M.L.; Ramassamy, C. Synergistic properties of bioavailable phenolic compounds from olive oil: Electron transfer and neuroprotective properties. Nutr. Neurosci. 2021, 24, 660–673. [Google Scholar] [CrossRef] [PubMed]
- Debbabi, M.; Zarrouk, A.; Bezine, M.; Meddeb, W.; Nury, T.; Badreddine, A.; Karym, E.M.; Sghaier, R.; Bretillon, L.; Guyot, S.; et al. Comparison of the effects of major fatty acids present in the Mediterranean Diet (oleic acid, docosahexaenoic acid) and in hydrogenated oils (elaidic acid) on 7-ketocholesterol-induced oxiapoptophagy in microglial BV-2 cells. Chem. Phys. Lipids 2017, 207, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Abuznait, A.H.; Qosa, H.; Busnena, B.A.; El Sayed, K.A.; Kaddoumi, A. Olive-oil-derived oleocanthal enhances β-amyloid clearance as a potential neuroprotective mechanism against Alzheimer’s disease: In vitro and in vivo studies. ACS Chem. Neurosci. 2013, 4, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Batarseh, Y.S.; Mohamed, L.A.; Al Rihani, S.B.; Mousa, Y.M.; Siddique, A.B.; El Sayed, K.A.; Kaddoumi, A. Oleocanthal ameliorates amyloid-β oligomers’ toxicity on astrocytes and neuronal cells: In vitro studies. Neuroscience 2017, 352, 204–215. [Google Scholar] [CrossRef]
- Kucukgul, A.; Isgor, M.M.; Duzguner, V.; Atabay, M.N.; Kucukgul, A. Antioxidant effects of oleuropein on hydrogen peroxide-induced neuronal stress-an in vitro study. Anti-Inflamm. Anti-Allergy Agents Med. Chem. 2020, 19, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Pasban-Aliabadi, H.; Esmaeili-Mahani, S.; Sheibani, V.; Abbasnejad, M.; Mehdizadeh, A.; Yaghoobi, M.M. Inhibition of 6-hydroxydopamine-induced PC12 cell apoptosis by olive (Olea europaea L.) leaf extract is performed by its main component oleuropein. Rejuvenation Res. 2013, 16, 134–142. [Google Scholar] [CrossRef] [PubMed]
- de Malezieu, M.L.; Ferron, S.; Sauvager, A.; Courtel, P.; Ramassamy, C.; Tomasi, S.; Abasq, M.L. UV-Vis spectroelectrochemistry of oleuropein, tyrosol, and p-coumaric acid individually and in an equimolar combination. differences in LC-ESI-MS2 profiles of oxidation products and their neuroprotective properties. Biomolecules 2019, 9, 802. [Google Scholar] [CrossRef] [PubMed]
- Palazzi, L.; Bruzzone, E.; Bisello, G.; Leri, M.; Stefani, M.; Bucciantini, M.; De Laureto, P.P. Oleuropein aglycone stabilizes the monomeric α-synuclein and favours the growth of non-toxic aggregates. Sci. Rep. 2018, 8, 8337. [Google Scholar] [CrossRef]
- Kumar, R.; Khursheed, R.; Kumar, R.; Awasthi, A.; Sharma, N.; Khurana, S.; Kapoor, B.; Khurana, N.; Singh, S.K.; Gowthamarajan, K.; et al. Self-nanoemulsifying drug delivery system of fisetin: Formulation, optimization, characterization and cytotoxicity assessment. J. Drug Deliv. Sci. Technol. 2019, 54, 101252. [Google Scholar] [CrossRef]
- De Paola, M.; Sestito, S.E.; Mariani, A.; Memo, C.; Fanelli, R.; Freschi, M.; Bendotti, C.; Calabrese, V.; Peri, F. Synthetic and natural small molecule TLR4 antagonists inhibit motoneuron death in cultures from ALS mouse model. Pharmacol. Res. 2016, 103, 180–187. [Google Scholar] [CrossRef] [PubMed]
- St-Laurent-Thibault, C.; Arseneault, M.; Longpré, F.; Ramassamy, C. Tyrosol and hydroxytyrosol two main components of olive oil, protect N2a cells against amyloid-ß-induced toxicity. involvement of the NF-KB signaling. Curr. Alzheimer Res. 2011, 8, 543–551. [Google Scholar] [CrossRef]
- Qusa, M.H.; Abdelwahed, K.S.; Meyer, S.A.; El Sayed, K.A. Olive Oil Lignan (+)-Acetoxypinoresinol Peripheral Motor and Neuronal Protection against the Tremorgenic Mycotoxin Penitrem A Toxicity via STAT1 Pathway. ACS Chem. Neurosci. 2020, 11, 3575–3589. [Google Scholar] [CrossRef]
- Oliván, S.; Martínez-Beamonte, R.; Calvo, A.C.; Surra, J.C.; Manzano, R.; Arnal, C.; Osta, R.; Osada, J. Extra virgin olive oil intake delays the development of amyotrophic lateral sclerosis associated with reduced reticulum stress and autophagy in muscle of SOD1G93A mice. J. Nutr. Biochem. 2014, 25, 885–892. [Google Scholar] [CrossRef]
- Qosa, H.; Mohamed, L.A.; Batarseh, Y.S.; Alqahtani, S.; Ibrahim, B.; LeVine, H.; Keller, J.N.; Kaddoumi, A. Extra-virgin olive oil attenuates amyloid-β and tau pathologies in the brains of TgSwDI mice. J. Nutr. Biochem. 2015, 26, 1479–1490. [Google Scholar] [CrossRef] [PubMed]
- Farfán-García, E.D.; Abad-García, A.; Alatorre, A.; Pérez-Capistran, T.; Querejeta, E.; Soriano-Ursúa, M.A. Olive oil limited motor disruption and neuronal damage in parkinsonism induced by MPTP administration. Toxicol. Res. Appl. 2020, 4, 2397847320922939. [Google Scholar] [CrossRef]
- Debbabi, M.; Nury, T.; Zarrouk, A.; Mekahli, N.; Bezine, M.; Sghaier, R.; Grégoire, S.; Martine, L.; Durand, P.; Camus, E.; et al. Protective effects of α-tocopherol, γ-tocopherol and oleic acid, three compounds of olive oils, and no effect of trolox, on 7-ketocholesterol-induced mitochondrial and peroxisomal dysfunction in microglial BV-2 cells. Int. J. Mol. Sci. 2016, 17, 1973. [Google Scholar] [CrossRef] [PubMed]
- Lauretti, E.; Iuliano, L.; Praticò, D. Extra-virgin olive oil ameliorates cognition and neuropathology of the 3xTg mice: Role of autophagy. Ann. Clin. Transl. Neurol. 2017, 4, 564–574. [Google Scholar] [CrossRef]
- Lauretti, E.; Nenov, M.; Dincer, O.; Iuliano, L.; Praticò, D. Extra virgin olive oil improves synaptic activity, short-term plasticity, memory, and neuropathology in a tauopathy model. Aging Cell 2020, 19, e13076. [Google Scholar] [CrossRef]
- Kandiş, S.; Altintaş, L.; Kizildağ, S.; Şimşek, F.; Ateş, M.; Alaçam, H.; Uysal, N. Comparison anti-oxidant and neuroprotective effects of extra-virgin olive oil, donepezil and rosmarinic acid on aluminum chloride-induced Alzheimer’s in rat models. Ank. Univ. Vet. Fak. Derg. 2022, 69, 171–181. [Google Scholar] [CrossRef]
- Machin, A.; Kalanjati, V.P.; Abidah, A.N.; Sugianto, P.; Susanto, J.; Firdha, A.A. The effect of extra virgin olive oil on HSP27 expression in the cerebral cortex of male Rattus norvegicus middle cerebral artery occlusion model. Food Nutr. Res. 2024, 68. [Google Scholar] [CrossRef]
- Tasset, I.; Pontes, A.J.; Hinojosa, A.J.; de la Torre, R.; Túnez, I. Olive oil reduces oxidative damage in a 3-nitropropionic acid-induced huntington’s disease-like rat model. Nutr. Neurosci. 2011, 14, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Grossi, C.; Ed Dami, T.; Rigacci, S.; Stefani, M.; Luccarini, I.; Casamenti, F. Employing alzheimer disease animal models for translational research: Focus on dietary components. Neurodegener. Dis. 2014, 13, 131–134. [Google Scholar] [CrossRef]
- Abdallah, I.M.; Al-Shami, K.M.; Alkhalifa, A.E.; Al-Ghraiybah, N.F.; Guillaume, C.; Kaddoumi, A. Comparison of Oleocanthal-Low EVOO and Oleocanthal against Amyloid-β and Related Pathology in a Mouse Model of Alzheimer’s Disease. Molecules 2023, 28, 1249. [Google Scholar] [CrossRef] [PubMed]
- Amel, N.; Wafa, T.; Samia, D.; Yousra, B.; Issam, C.; Cheraif, I.; Attia, N.; Mohamed, H. Extra virgin olive oil modulates brain docosahexaenoic acid level and oxidative damage caused by 2,4-Dichlorophenoxyacetic acid in rats. J. Food Sci. Technol. 2016, 53, 1454–1464. [Google Scholar] [CrossRef]
- Rodríguez-Pérez, M.D.; de Algaba, I.P.; Martín-Aurioles, E.; Arrebola, M.M.; Ortega-Hombrados, L.; Verdugo, C.; Fernández-Prior, M.Á.; Bermúdez-Oria, A.; De La Cruz, J.P.; González-Correa, J.A. Neuroprotective Effect of 3′,4′-Dihydroxyphenylglycol in Type-1-like Diabetic Rats—Influence of the Hydroxytyrosol/3′,4′-dihydroxyphenylglycol Ratio. Nutrients 2022, 14, 1146. [Google Scholar] [CrossRef]
- Romero-Márquez, J.M.; Navarro-Hortal, M.D.; Jiménez-Trigo, V.; Muñoz-Ollero, P.; Forbes-Hernández, T.Y.; Esteban-Muñoz, A.; Giampieri, F.; Noya, I.D.; Bullón, P.; Vera-Ramírez, L.; et al. An Olive-Derived Extract 20% Rich in Hydroxytyrosol Prevents β-Amyloid Aggregation and Oxidative Stress, Two Features of Alzheimer Disease, via SKN-1/NRF2 and HSP-16.2 in Caenorhabditis elegans. Antioxidants 2022, 11, 629. [Google Scholar] [CrossRef]
- Arunsundar, M.; Shanmugarajan, T.S.; Ravichandran, V. 3,4-Dihydroxyphenylethanol Attenuates Spatio-Cognitive Deficits in an Alzheimer’s Disease Mouse Model: Modulation of the Molecular Signals in Neuronal Survival-Apoptotic Programs. Neurotox. Res. 2015, 27, 143–155. [Google Scholar] [CrossRef] [PubMed]
- De La Cruz, J.P.; Ruiz-Moreno, M.I.; Guerrero, A.; Reyes, J.J.; Benitez-Guerrero, A.; Espartero, J.L.; González-Correa, J.A. Differences in the Neuroprotective Effect of Orally Administered Virgin Olive Oil (Olea europaea) Polyphenols Tyrosol and Hydroxytyrosol in Rats. J. Agric. Food Chem. 2015, 63, 5957–5963. [Google Scholar] [CrossRef]
- Gallardo, E.; Madrona, A.; Palma-Valdés, R.; Trujillo, M.; Espartero, J.L.; Santiago, M. The effect of hydroxytyrosol and its nitroderivatives on catechol-O-methyl transferase activity in rat striatal tissue. RSC Adv. 2014, 4, 61086–61091. [Google Scholar] [CrossRef]
- Qin, C.; Hu, S.; Zhang, S.; Zhao, D.; Wang, Y.; Li, H.; Peng, Y.; Shi, L.; Xu, X.; Wang, C.; et al. Hydroxytyrosol Acetate Improves the Cognitive Function of APP/PS1 Transgenic Mice in ERβ-dependent Manner. Mol. Nutr. Food Res. 2021, 65, e2000797. [Google Scholar] [CrossRef] [PubMed]
- Batarseh, Y.S.; Kaddoumi, A. Oleocanthal-rich extra-virgin olive oil enhances donepezil effect by reducing amyloid-β load and related toxicity in a mouse model of Alzheimer’s disease. J. Nutr. Biochem. 2018, 55, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Mete, M.; Aydemir, I.; Unsal, U.U.; Collu, F.; Vatandas, G.; Gurcu, B.; Duransoy, Y.K.; Taneli, F.; Tuglu, M.I.; Selcuki, M. Neuroprotective effects of oleocanthal, a compound in virgin olive oil, in a rat model of traumatic brain injury. Turk. Neurosurg. 2018, 28, 858–865. [Google Scholar] [CrossRef]
- Khalatbary, A.R.; Ahmadvand, H. Neuroprotective effect of oleuropein following spinal cord injury in rats. Neurol. Res. 2012, 34, 44–51. [Google Scholar] [CrossRef]
- Luccarini, I.; Pantano, D.; Nardiello, P.; Cavone, L.; Lapucci, A.; Miceli, C.; Nediani, C.; Berti, A.; Stefani, M.; Casamenti, F. The Polyphenol Oleuropein Aglycone Modulates the PARP1-SIRT1 Interplay: An in Vitro and in Vivo Study. J. Alzheimers Dis. 2016, 54, 737–750. [Google Scholar] [CrossRef]
- Diomede, L.; Rigacci, S.; Romeo, M.; Stefani, M.; Salmona, M. Oleuropein Aglycone Protects Transgenic C. elegans Strains Expressing Aβ42 by Reducing Plaque Load and Motor Deficit. PLoS ONE 2013, 8, e58893. [Google Scholar] [CrossRef]
- Luccarini, I.; Ed Dami, T.; Grossi, C.; Rigacci, S.; Stefani, M.; Casamenti, F. Oleuropein aglycone counteracts Aβ42 toxicity in the rat brain. Neurosci. Lett. 2014, 558, 67–72. [Google Scholar] [CrossRef]
- Zamani, M.; Hassanshahi, J.; Soleimani, M.; Zamani, F. Neuroprotective effect of olive oil in the hippocampus CA1 neurons following ischemia: Reperfusion in mice. J. Neurosci. Rural Pract. 2013, 4, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Mardookhi, J.; Bigdeli, M.R.; Khaksar, S. The effect of pre-treatment with olive oil on TNFR1/NF-kB inflammatory pathway in rat ischemic stroke model. Physiol. Pharmacol. 2016, 20, 246–255. [Google Scholar]
- Maj, M.A.; Gehani, T.R.; Immoos, C.; Medrano, M.S.; Fanter, R.K.; Strand, C.R.; Glanz, H.; Piccolo, B.D.; Abo-Ismail, M.K.; La Frano, M.R.; et al. Olive- and Coconut-Oil-Enriched Diets Decreased Secondary Bile Acids and Regulated Metabolic and Transcriptomic Markers of Brain Injury in the Frontal Cortexes of NAFLD Pigs. Brain Sci. 2022, 12, 1193. [Google Scholar] [CrossRef]
- Lee, A.Y.; Choi, J.M.; Lee, J.; Lee, M.H.; Lee, S.; Cho, E.J. Effects of Vegetable Oils with Different Fatty Acid Compositions on Cognition and Memory Ability in Aβ25-35-Induced Alzheimer’s Disease Mouse Model. J. Med. Food 2016, 19, 912–921. [Google Scholar] [CrossRef]
- Koppal, A.; Sivanesan, S.; Ramachandra, V.H.; Sukumar, E.; Vijayaraghavan, R. Embelin and levodopa combination therapy mitigates parkinson’s disease complications in mice. Indian J. Pharm. Educ. Res. 2021, 55, S468–S478. [Google Scholar] [CrossRef]
- Yu, J.; Kwon, H.; Cho, E.; Jeon, J.; Kang, R.H.; Youn, K.; Jun, M.; Lee, Y.C.; Ryu, J.H.; Kim, D.H. The effects of pinoresinol on cholinergic dysfunction-induced memory impairments and synaptic plasticity in mice. Food Chem. Toxicol. 2019, 125, 376–382. [Google Scholar] [CrossRef]
- García-Moreno, J.C.; Porta de la Riva, M.; Martínez-Lara, E.; Siles, E.; Cañuelo, A. Tyrosol, a simple phenol from EVOO, targets multiple pathogenic mechanisms of neurodegeneration in a C. elegans model of Parkinson’s disease. Neurobiol. Aging 2019, 82, 60–68. [Google Scholar] [CrossRef]
- Mohagheghi, F.; Bigdeli, M.R.; Rasoulian, B.; Zeinanloo, A.A.; Khoshbaten, A. Dietary virgin olive oil reduces blood brain barrier permeability, brain edema, and brain injury in rats subjected to ischemia-reperfusion. Sci. World J. 2010, 10, 1180–1191. [Google Scholar] [CrossRef]
- Cruz, J.P.D.L.; Río, S.D.; Arrebola, M.M.; López-Villodres, J.A.; Jebrouni, N.; González-Correa, J.A. Effect of virgin olive oil plus acetylsalicylic acid on brain slices damage after hypoxia-reoxygenation in rats with type 1-like diabetes mellitus. Neurosci. Lett. 2010, 471, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Berr, C.; Portet, F.; Carriere, I.; Akbaraly, T.N.; Feart, C.; Gourlet, V.; Combe, N.; Barberger-Gateau, P.; Ritchie, K. Olive Oil and Cognition: Results from the Three-City Study. Dement. Geriatr. Cogn. Disord. 2009, 28, 357–364. [Google Scholar] [CrossRef]
- Martínez-Lapiscina, E.H.; Clavero, P.; Toledo, E.; Estruch, R.; Salas-Salvadó, J.; San Julián, B.; Sanchez-Tainta, A.; Ros, E.; Valls-Pedret, C.; Martinez-Gonzalez, M. Mediterranean Diet improves cognition: The PREDIMED-NAVARRA randomised trial. J. Neurol. Neurosurg. Psychiatry 2013, 84, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Tsolaki, M.; Lazarou, E.; Kozori, M.; Petridou, N.; Tabakis, I.; Lazarou, I.; Karakota, M.; Saoulidis, I.; Melliou, E.; Magiatis, P. A Randomized Clinical Trial of Greek High Phenolic Early Harvest Extra Virgin Olive Oil in Mild Cognitive Impairment: The MICOIL Pilot Study. J. Alzheimers Dis. 2020, 78, 801–817. [Google Scholar] [CrossRef]
- Kaddoumi, A.; Denney, T.S.; Deshpande, G.; Robinson, J.L.; Beyers, R.J.; Redden, D.T.; Praticò, D.; Kyriakides, T.C.; Lu, B.; Kirby, A.N.; et al. Extra-Virgin Olive Oil Enhances the Blood–Brain Barrier Function in Mild Cognitive Impairment: A Randomized Controlled Trial. Nutrients 2022, 14, 5102. [Google Scholar] [CrossRef]
- Management of Dementia with Olive Oil Leaves—GOLDEN. 2019. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT0444002 (accessed on 25 May 2024).
- Masonic Cancer Center. Study of Nutraceutical Intervention with High Phenolic Extra Virgin Olive Oil and Curcumin for Neurofibromatosis, Type 1 (NF1). 2022. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05363267 (accessed on 25 May 2024).
- Auburn University. Does EVOO Induce Gene and Metabolic Changes in Healthy Subjects. 2023. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT05929924 (accessed on 25 May 2024).
- de la Torre, R. Bioavailability of olive oil phenolic compounds in humans. Inflammopharmacology 2008, 16, 245–247. [Google Scholar] [CrossRef] [PubMed]

| Reasons for the Brain’s Susceptibility for Oxidative Stress | Examples and Consequences of Radical Formation |
|---|---|
| Radicals are important in fundamental biological processes. |
|
| The brain relies on Ca2+ signaling, which in turn can trigger several neurotoxic cascades that produce reactive species. |
|
| Glutamate, a fundamental neurotransmitter, can result in decreased endogenous antioxidant defenses and excessive Ca2+ influx, which activates harmful neurotoxic pathways that produce radicals. |
|
| Neurons have limited capacity to metabolize toxic byproducts of glucose metabolism, which can generate toxicity and cause alterations in proteins, RNA and DNA, leading to OS. |
|
| Mitochondria are involved in respiration and signaling pathways, both of which produce reactive species. |
|
| The metabolism of neurotransmitters might generate H2O2 |
|
| Neurotransmitters, particularly those with catechol groups, can undergo auto-oxidation. |
|
| The brain has relatively low endogenous antioxidant defense mechanisms. |
|
| Transition metals, which are abundant in the brain, can lead to increased levels of reactive species. |
|
| The high content of unsaturated lipids in the brain makes it susceptible to lipid peroxidation and OS. |
|
| NOS and NOX are used for signaling. |
|
| RNA can undergo oxidation, generating damaging molecules. |
|
| Sample | In Vitro Model | Treatment | Biological Activity | Reference |
|---|---|---|---|---|
| HT | PC12 cells | PC12 cells were pre-treated with HT at concentrations ranging from 1 to 50 μM for 12 h before being exposed to either H2O2 or 6-OHDA to induce oxidative damage. Cell viability and other assays were conducted after treatment with H2O2 or 6-OHDA for various durations, typically 12 to 24 h. | HT scavenged free radicals in vitro, displaying better activity than resveratrol in DPPH assays and protecting erythrocyte ghosts from lipid peroxidation and hemolysis induced by AAPH. HT protected PC12 cells from H2O2 and 6-OHDA-induced cell damage, maintaining cell viability and reducing LDH leakage. HT decreased the population of apoptotic nuclei and significantly reduced the activation of caspase-3, a key enzyme in the execution phase of apoptosis. HT prevented intracellular ROS accumulation and loss of cellular thiols in PC12 cells treated with H2O2 or 6-OHDA. HT activated the Nrf2/ARE signaling pathway, leading to the upregulation of cytoprotective enzymes such as HO-1, NQO1, TrxR1, and GCLC and GCLM. The activation of Nrf2 and its translocation to the nucleus were essential for HT’s protective effects, as knockdown of Nrf2 significantly reduced HT’s cytoprotective actions. | [148] |
| HT | SH-SY-5Y cells | SH-SY-5Y cells were treated with HT at various concentrations (2, 5, and 10 μM) and exposed to high glucose (45 mM) to induce OS. The cells were pre-treated with HT for 24 h before glucose exposure. | HT significantly enhanced cell viability and reduced OS-induced apoptosis in SH-SY-5Y cells. HT increased the expression of HO-1 and complex IV in SH-SY-5Y cells and prevented high glucose-induced ROS production and mitochondrial dysfunction. | [149] |
| HT | Astrocytic cell line (C6) (AD model) | The astrocytic cell line was exposed to Aβ (25–35) and co-incubated with HT for different periods. | Aβ (25–35) exposure significantly decreased astrocyte viability compared to controls. Both pre-treatment and post-treatment with HT prevented this decrease in viability. HT’s preventive role on Aβ (25–35)-induced cytotoxicity in astrocytes was mediated by an increased HT-induced activation of Akt, part of the insulin signaling pathway. HT prevented the pronounced activation of mTOR, thereby restoring proper insulin signaling. HT protects Aβ (25–35)-treated astrocytes by improving insulin sensitivity and restoring proper insulin signaling. | [150] |
| HT | BV 2 cells | BV 2 cells were treated with HT at various concentrations (1, 10, 25, and 50 µM) and stimulated with LPS or aggregated α-Syn. | HT demonstrated anti-inflammatory effects by reducing microglial activation. HT decreased the expression of pro-inflammatory markers (TNF-α, iNOS, IL-1β, IL-6, and CXCL10), inhibited the nuclear translocation of NF-κB, and reduced the ROS production via the inhibition of NADPH oxidase. Additionally, HT modulated the MAPK pathways (JNK 1/2, p38, and AKT) involved in the inflammatory response. | [151] |
| HT and HT-AC (VOO) | Rat brain slices | Brain slices were pre-incubated with HT and HT-AC at various concentrations (1, 5, 10, 50, and 100 µM) during hypoxia and reoxygenation periods. | Both HT and HT-AC significantly reduced LDH efflux, a marker of brain cell death, in a concentration-dependent manner. The IC50 values were 77.78 µM for HT and 28.18 µM for HT-AC. | [152] |
| HT and its metabolites, which include DOPAL, MOPET, and MOPAL | PC12 cells | The type of administration involves treating PC12 cells with various concentrations of the metabolites (DOPAL, MOPET, and MOPAL) either alone or in combination with α-Syn fibrils. The specific concentrations tested for each metabolite ranged from 0.5 μM to 150 μM. | DOPAL: Exhibits the greatest effect in preventing aggregation and α-Syn-induced neurotoxicity, with a potent destabilizing effect on α-Syn fibrils and a significant increase in cell viability. MOPET: Effective in inhibiting α-Syn fibril formation and reducing α-Syn-induced toxicity in PC12 cells, though less potent than DOPAL. MOPAL: No significant effect on α-Syn fibril formation or destabilization and showed toxicity at higher concentrations. Gene expression: Both DOPAL and MOPET significantly increased SIRT-1 and Hsp70 gene expression, and inhibited SIRT-2 gene expression, which are involved in neuroprotective mechanisms. | [153] |
| HT, Alkyl HT ethers including ethyl, butyl, hexyl, octyl, and dodecyl derivatives | Rat brain slices | Brain slices were incubated with HT and its alkyl ether derivatives at concentrations ranging from 0.5 to 1000 μM. The experimental protocol included:
| Neuroprotective effects: All alkyl HT ethers demonstrated neuroprotective effects by reducing LDH efflux. The butyl derivative was the most potent, showing the lowest IC50 values for LDH efflux and lipid peroxidation (TBARS). Antioxidant effects: All compounds inhibited lipid peroxidation in a concentration-dependent manner, with the butyl ether being the most effective. Compounds also mitigated GSH depletion induced by diethylmaleate and prevented OS induced by hypoxia/reoxygenation. HT and its derivatives reduced the levels of PGE2, nitrites plus nitrates (NO2 + NO3), and IL-1β, indicating anti-inflammatory properties. | [154] |
| HT, HT-AC, Tyr, DOPAC, DA, and sodium ascorbate | Biomolecular fluorescence complementation technology using E. coli BL21 cells | Sodium ascorbate was used to supplement, as it allowed for stabilization by avoiding autoxidation. Specific dosages of HT, HT-AC, Tyr, DOPAC, and DA were administered. | Reduction in α-syn aggregation: At low concentrations, most molecules were mildly effective, likely due to oxidation. Increasing the concentration, along with supplementation with sodium ascorbate, improved their effectiveness. In fact, HT-AC and DOPAC were able to inhibit aggregation entirely and DA decreased the aggregation by 28.7%. | [155] |
| HT, Tyr, and MET | Rat brain tissue | OS was induced with ferrous salts (lipid peroxidation induction), diethyl maleate (depletion of GSH), and hypoxia/reoxygenation in brain slices. The study involved comparing the effects of HT, Tyr, and MET on OS and neuroprotection. | Lipid peroxidation was inhibited in direct proportion to the number of OH groups: HT > Tyr > MET. Exposure to HT led to partial recovery of the GSH system after chemical inhibition or hypoxia/reoxygenation. All three compounds inhibited cell death in hypoxia/reoxygenation experiments, with HT being the most effective. ONOO- formation (3-nitrotyrosine) and inflammatory mediators (PGE2 and IL-1β) were inhibited by all three compounds. The presence of OH groups in these phenolic compounds from VOO is a determinant factor in their antioxidant effect in brain tissue, though this antioxidant effect is not the only explanation for their neuroprotective effect. | [156] |
| HT, Tyr, CA, and CU extracted from olive mill wastewater derived from the production of four Sicilian EVOOs | Human neuroblastoma LAN5 cells | LAN5 cells were treated with the biophenols (HT, Tyr, CA, and CU) at concentrations of 12.5, 25, 50, and 100 μM for 24 h. Cells were also treated with 40 μM Aβ oligomers alone or in combination with 25 or 50 μM of the biophenols. | Antioxidant activity: The antioxidant ability of the biophenols was determined using the ORAC assay. The ORAC values were HT (24,000 μmol TE/g), Tyr (25,000 μmol TE/g), CA (16,000 μmol TE/g), and CU (21,000 μmol TE/g). Cytotoxicity: The biophenols were not cytotoxic to LAN5 cells at concentrations up to 50 μM. At 100 μM, a slight decrease in cell viability was observed for HT and CU. Neuroprotective effects: The biophenols (HT, Tyr, and CA) demonstrated a neuroprotective role by significantly reducing the oxidative damage induced by Aβ oligomers. CA was the most effective in preserving cell viability and morphology. The biophenols reduced ROS and mitochondrial superoxide production induced by Aβ oligomers. CA showed the most significant reduction in ROS and superoxide levels compared to HT and Tyr. | [157] |
| HT, Tyr, 3′,4′DHPG, and OLC | Rat brain slices | The brain slices were incubated with HT, Tyr, DHPG, and OLC at various concentrations mimicking those found in EVOO. The polyphenols were administered from the beginning of the experiment (pre-hypoxia) and maintained until the end of the reoxygenation period. | Cytoprotective effects: The polyphenol mixture showed significantly greater cytoprotective effects compared to HT alone. The combination reduced LDH efflux. Antioxidant effects: The polyphenols demonstrated potent antioxidant effects by reducing lipid peroxidation (TBARS) and inhibiting ONOO- production. HT and OLC: Showed the highest antioxidant and cytoprotective potency. DHPG: Increased the antioxidant effects of HT at higher concentrations and enhanced its inhibitory effect on ONOO- formation. Tyr: Did not significantly modify the antioxidant variables inhibited by HT but showed some synergistic effects in combination. | [158] |
| Mix 1—OLE, ρ-coumaric, and Tyr; Mix 2—HT, ρ-coumaric, and Tyr | Neuroblastoma cell line (SK-N-SH) | The neuronal cells were exposed to H2O2 (200 μM) or paraquat and treatment with the mixes at various concentrations followed. | Radical scavenging capacity: Mix 1 presented higher capacity of scavenging free radicals, when comparing with Mix 2. Hence, for cellular studies, only Mix 1 was used. Cytoprotective effects: Mix 1 at the concentrations of 0.1 and 1 μM allowed for protection of the neuronal cells challenged with H2O2, while the compounds that constituted it did not have similar effects when used individually. The results were comparable when cells were treated with paraquat, a pesticide that induces OS and is related with PD etiology. Antioxidant effects: At 1 μM, Mix 1 reduced the level of ROS by 15% and protected cells from OS related damage, observed through diminished protein carbonyl levels. Moreover, treatment with Mix 1 leads to reduced activation of NF-κB and Nrf2. | [159] |
| OA | BV 2 cells | BV 2 cells were treated with 7KC at concentrations of 25–50 μM to induce cytotoxic effects, including OS, apoptosis, and autophagy. OA was administered at concentrations of 50, 100, 200, 300, and 600 μM, either alone or in combination with 7KC. Treatments with OA, EA, and DHA were added to the culture medium simultaneously with 7KC for 24 h. | Cell viability and proliferation: OA significantly attenuated 7KC-induced inhibition of cell proliferation. Oxidative stress: OA reduced 7KC-induced ROS overproduction and lipid peroxidation, as indicated by reduced 4-HNE levels. Mitochondrial protection: OA mitigated 7KC-induced loss of mitochondrial transmembrane potential (Δψm) and decreased the percentage of cells with depolarized mitochondria. Plasma membrane integrity: OA reduced 7KC-induced plasma membrane permeability, assessed by propidium iodide staining, indicating reduced cell death. Membrane fluidity: OA prevented 7KC-induced increase in plasma membrane fluidity, as measured by fluorescence anisotropy using TMA-DPH. Apoptosis: OA significantly reduced 7KC-induced apoptosis, evidenced by decreased caspase-3 activation and lower percentage of cells with condensed/fragmented nuclei. Autophagy: OA modulated 7KC-induced autophagy, indicated by changes in the LC3-II/LC3-I ratio. OA reduced the autophagic response. | [160] |
| OLC | Mouse brain endothelial cells (bEnd3 cells) were used as a representative model of BBB | Cells were treated with OLC at concentrations ranging from 0.5 to 50 μM for 72 h. | OLC treatment increased the expression and activity P-gp and LRP1, which are major Aβ transport proteins at the BBB. A significant increase in 125I-Aβ40 degradation due to the upregulation of Aβ-degrading enzymes was observed following OLC treatment. | [161] |
| OLC | Human astrocytoma cell line (CCF-STTG1). SH-SY5Y cell line, transfected with APP695 (SH-SY5Y-APP) and non-transfected SH-SY5Y cells | Astrocytes were treated with 100 nM of Aβo, 5 μM OLC, or a combination of both for 3 or 7 days. Neuronal cells (SH-SY5Y-APP and SH-SY5Y) were treated with 100 nM Aβo, 5 μM OLC, or a combination for 3 or 7 days. ACM from treated astrocytes was also used to treat neurons. | Astrocytes: OLC reduced the baseline and Aβo-induced levels of IL-6 and GFAP in astrocytes. OLC restored the Aβo-induced downregulation of GLT1 and GLUT1 in astrocytes. Astrocytes efficiently took up Aβ monomers and oligomers, with OLC not significantly altering the degradation of Aβ monomers. Neuronal cells: OLC prevented the Aβo-induced downregulation of synaptic proteins PSD-95 and SNAP-25 in SH-SY5Y-APP cells and increased their baseline expression. OLC directly induced the expression of synaptic proteins in neurons without mediation by astrocytes, as ACM from OLC-treated astrocytes did not alter synaptic protein levels in neurons. | [162] |
| OLE | Human glioblastoma cells (U87) | U87 cells were pre-treated with OLE essential oil at a concentration of 10 µM. After 30 min of OLE pre-treatment, 100 µM H2O2 was added to induce OS, and the cells were incubated for 3 h. | Cell viability: OLE pre-treatment significantly prevented cell losses caused by H2O2. GSH levels: OLE regenerated total antioxidant capacity and GSH levels, which were decreased by H2O2 exposure. Nitric oxide and total oxidant capacity: OLE administration decreased NO and total oxidant capacity levels in treated cells. iNOS expression: The relative gene expression level of inducible iNOS was reduced by OLE pre-treatment. | [163] |
| OLE and olive leaf extract | PC12 cells | PC12 cells were treated with 6-OHDA at a concentration of 150 μM to induce cell damage. Olive leaf extract was administered at doses of 400 and 600 µg/mL. OLE was administered at doses of 20 and 25 µg/mL. Olive leaf extract and OLE were added to the cells 20 min before 6-OHDA treatment and incubated for 24 h. | Olive leaf extract and OLE significantly increased cell viability and reduced 6-OHDA-induced cytotoxicity in PC12 cells. Treatment with olive leaf extract and OLE reduced intracellular ROS levels in 6-OHDA-treated cells. OLE decreased the activation of caspase-3 and balanced the Bax/Bcl-2 ratio, indicating inhibition of apoptosis. Olive leaf extract and OLE also prevented DNA fragmentation induced by 6-OHDA, further confirming their protective effects against apoptosis. | [164] |
| OLE, Tyr, and CU | SK-N-SH cells | SK-N-SH cells were treated with H₂O₂ to induce OS. Cells were then treated with very low concentrations (1 and 5 nM) of oxidized OLE and oxidized mixtures (Mix) of the three polyphenols for 24 h to evaluate their neuroprotective properties. | Antioxidant activity: Significant neuroprotection by oxidized OLE and the oxidized mix against H₂O₂-induced toxicity was observed in SK-N-SH cells. Neuroprotective effects: Oxidized OLE and the oxidized polyphenol mix significantly reduced intracellular ROS levels and protein carbonyl levels in neuronal cells exposed to OS. The combination of OLE with Tyr and CU acid showed enhanced neuroprotective effects compared to the individual polyphenols, suggesting synergistic interactions among the compounds. Mechanism of action: The neuroprotective effects of the oxidized polyphenols were attributed to their ability to modulate redox signaling pathways and reduce oxidative damage. The presence of oxidized products, such as quinones and dimers, formed during the oxidation process, contributed to the enhanced antioxidant and neuroprotective properties of the mixtures. | [165] |
| OleA | SH-SY5Y cells | SH-SY5Y cells were treated with α-Syn aggregates in the presence or absence of OleA at a ratio of 1:10 (α-Syn/OleA) for various incubation times (24 h and 5 days). | Anti-amyloidogenic effects: OleA interfered with α-Syn aggregation, stabilizing monomeric α-Syn and hampering the growth of toxic oligomers. OleA favored the formation of stable and harmless α-Syn aggregates, reducing the formation of cytotoxic amyloid fibrils. Reduction in cytotoxicity: OleA-treated α-Syn aggregates showed reduced cytotoxicity in SH-SY5Y cells compared to untreated aggregates. Higher cell viability was observed when cells were treated with α-Syn aggregates formed in the presence of OleA. Oxidative stress reduction: OleA decreased the ability of α-Syn aggregates to induce ROS production in SH-SY5Y cells. ROS levels were significantly lower in cells treated with OleA-formed aggregates compared to those treated with untreated α-Syn aggregates. Interaction with cell membrane: OleA reduced the binding of α-Syn aggregates to cell membrane components, particularly to lipid raft-associated ganglioside GM1. This reduction in membrane interaction likely contributes to the decreased cytotoxicity in OleA-treated aggregates. | [166] |
| OleA | SH-SY5Y cells | OleA was dissolved in DMSO and used in various assays to investigate its effect on protein aggregation and cytotoxicity. | OleA was found to interfere with the aggregation of Syn by stabilizing Syn monomers and preventing the formation of cytotoxic oligomers. It reduced the cytotoxicity of Syn aggregates by preventing their binding to cell membranes and reducing oxidative damage to cells. | [167] |
| OleA | SH-SY5Y cells | OleA was used to investigate its effect on pE3-Aβ aggregation and cytotoxicity in SH-SY5Y cells. | OleA was shown to reduce the burden of pE3-Aβ by interfering with its aggregation path, reducing its cytotoxicity, and promoting the formation of non-toxic aggregates. | [167] |
| Phenol fraction extracted from commercial EVOO | HEK cells expressing TLR4 (HEK-Blue-4™ cells). Spinal cord primary cultures from SOD1 mutated (SOD1 G93A) mice | The phenolic extract from EVOO was added to the cell cultures to inhibit TLR4 activation. The dose-dependent inhibition of TLR4 activation was determined with concentrations resulting in an IC50 of about 20 μg/mL. | EVOO phenols inhibited the activation of TLR4 in HEK cells and reduced the release of NO from activated glia. They protected motoneurons from LPS-induced lethality in spinal cord cultures and counteracted motoneuron death induced by SOD1 mutant glia. EVOO phenols demonstrated recognized antioxidant properties, which contributed to their anti-inflammatory and neuroprotective effects. | [168] |
| Ty and OH-Tyr | N2a cells | Tyr and OH-Tyr were applied to cultured N2a cells in vitro. Aβ was used to induce toxicity in the cells (100 μg/mL). | Neuroprotection: Tyr and OH-Tyr decreased cell death when co-treated with Aβ. Mechanism of Action: Both compounds attenuated the increase in nuclear translocation of the NF-κB subunits after Aβ exposure. GSH Levels: Neither Tyr and OH-Tyr prevented the decrease in GSH induced by H2O2 or Aβ. Transcription Factor Activation: The activation of NF-κB by Aβ was reduced in the presence of Tyr and OH-Tyr. | [169] |
| Tyr, HT, (−)-OLC, (−)-hydroxyoleocanthal, ligstroside aglycone, OleA, OLE, and (+)-1-acetoxypinoresinol (AC), PN | Schwann cells | The administration involved treating Schwann cells with penitrem A at its IC50 value (20 μM) and then adding the tested olive phenolics. | Tyr: No protective activity against Penitrem A at any dose. HT: Moderate protective activity, showing 32% toxicity recovery at 10 μM. Secoiridoids: (−)-OLC, (−)-hydroxyoleocanthal, and ligstroside aglycone did not show any protective activity. OleA and OLE had modest recovery (10%) at 10 μM. Lignans: Consistent and significant protection ratios at different doses. AC and PN significantly increased Schwann cells’ survival rates with notable dose-dependent protection against penitrem A toxicity. | [170] |
| Sample | In Vivo Model | Treatment | Biological Activity | Reference |
|---|---|---|---|---|
| EVOO | Transgenic SOD1G93A mice (ALS model). | Mice were fed a chow diet enriched with 20% (w/w) EVOO. | Mice fed an EVOO diet showed significantly higher survival and better motor performance compared to control mice. EVOO group mice also had larger muscle fiber areas than those receiving palm oil. The study found a decrease in markers of ER stress, such as Atf6 and Grp78, in mice receiving the EVOO diet. The beneficial effects of EVOO were associated with improved ER stress response and autophagy in muscle tissues. | [171] |
| EVOO | TgSwDI mice: A transgenic mouse model used to study AD and cerebral amyloid angiopathy. | Mice were fed an EVOO-enriched diet for either 3 or 6 months. | Reduction in Aβ and Tau pathologies: Long-term consumption of an EVOO-enriched diet (6 months) significantly reduced total Aβ and tau levels in the brain. Cognitive improvement: There was a significant improvement in mouse cognitive behavior with long-term EVOO consumption. Enhanced clearance and reduced production of Aβ: The reduction in brain Aβ was attributed to enhanced clearance pathways and reduced production via modulation of APP processing. Time-dependent effects: Short-term EVOO consumption (3 months) improved Aβ clearance and reduced Aβ levels but did not affect tau levels or cognitive functions. | [172] |
| EVOO | Acute parkinsonism murine model in C57BL6 mice induced by MPTP. | EVOO, corn oil, and levodopa were administered to the mice. | MPTP allowed for motor disruption in the mice. Enhanced locomotor activity: Mice treated with EVOO showed an increase in motor activity, compared to that registered when levodopa was used. Increased neural survival in the substantia nigra and striatum: Through immunohistochemistry, it was possible to observe that the group treated with EVOO had lower levels of neuronal loss, compared to the levels registered in the group treated with levodopa. Corn oil did not exhibit similar motor and neuroprotective effects. | [173] |
| EVOO OOLF OOHF | Rat | 2,4-D pesticide, EVOO, and its fractions were administered to rats by gavage for four consecutive weeks. | OS reduction: EVOO and its fractions partly reversed the OS caused by 2,4-D pesticide, as indicated by changes in brain lipid peroxide levels, AChE activity, and antioxidant enzyme activities. Restoration of fatty acid composition: EVOO enhanced neuroprotection by restoring brain fatty acid composition, especially the level of DHA. | [174] |
| EVOO | 3xTg mice (AD model) | Mice were fed a regular chow diet supplemented with EVOO starting at 6 months of age for 6 months. | Amelioration of behavioral deficits: Mice receiving the EVOO-rich diet showed improvements in their behavioral deficits. Increase in synaptophysin levels: There was a significant increase in the steady-state levels of synaptophysin, a protein marker of synaptic integrity. Reduction in Aβ and tau pathologies: Significant reduction in insoluble Aβ peptide levels and deposition. Lower amounts of phosphorylated tau protein at specific epitopes. Activation of cell autophagy: The reduction in Aβ and tau pathology was secondary to the activation of cell autophagy. | [175] |
| EVOO | The in vivo model used in this study is the hTau mouse model, which is a mouse model of tauopathy. | The treatment involved dietary administration of eEVOO. | The study found that EVOO directly improves synaptic activity, short-term plasticity, and memory while decreasing tau neuropathology in the hTau mice. Specifically, EVOO consumption ameliorated spatial learning and recognition memory ability, as well as enhanced hippocampal synaptic function and plasticity. | [176] |
| EVOO | Sprague–Dawley adult male rats Condition: AD model induced by aluminum chloride (AlCl₃) | AlCl₃ at 100 mg/kg administered orally for 15 days to induce AD pathology. Treatments administered for 21 days following the induction of AD: EVOO Rosmarinic acid Donepezil (used as a reference treatment) | Cognitive impairment: Cognitive impairment was observed after 15 days of AlCl₃ administration. Preventive effects: Treatment protocols with EVOO, rosmarinic acid, and donepezil prevented the occurrence of AD pathology histopathologically. Oxidative damage: The study demonstrated that oxidative damage was mitigated by the treatments. Neuroprotection: EVOO and rosmarinic acid showed neuroprotective effects similar to donepezil. | [177] |
| EVOO | Wistar rat strain | EVOO was administered in two dosages: 0.5 mL/kg body weight 2 mL/kg body weight The treatment was conducted over a period of 14 days. | Neuroprotection: EVOO showed potential neuroprotective effects by inhibiting ROS. Modulation of Hsp27: EVOO significantly downregulated the expression of Hsp27 in the cerebral cortex. Cellular composition: There were significant differences in neuron and glia nuclei numbers between groups treated with EVOO and control groups. OS reduction: The bioactive components in EVOO, including tocopherols and phenolic compounds, contribute to its antioxidant properties, reducing OS in brain tissue. | [178] |
| EVOO and HT | Rat model where HD-like conditions were induced using 3NP. | EVOO was administered orally to the rats. The study compares different timing of EVOO administration (before or after 3NP exposure) to assess the optimal protective effects against OS. | EVOO demonstrated significant antioxidative effects, evidenced by an increase in cellular GSH levels and a decrease in oxidative damage. The administration of EVOO both before and after 3NP exposure showed a protective effect against the OS induced in the brain, particularly in the striatum. | [179] |
| EVOO and OleA | TgCRND8 mice (AD model) | Continuous intake: High doses of OleA were administered, potentially as a nutraceutical or food integrator. | The study supports the beneficial effects of EVOO and highlights that continuous intake of high doses of OleA may prevent or delay the onset of AD and reduce the severity of its symptoms. Mechanisms of action includes autophagy and adult hippocampal neurogenesis, potentially leading to neuroprotective effects. | [180] |
| EVOO OLC | 5xFAD (AD model) | The administration method involved feeding the homozygous 5xFAD mice with refined olive oil, OLC-low EVOO (0.5 mg total phenolic content/kg), and OLC (0.5 mg OLC/kg) for three months. | Both EVOO and OLC significantly reduced the levels of soluble APP and increased the expression of synaptic markers (PSD-95, SNAP-25, and synapsin-1) in the 5xFAD mouse brains. EVOO and OLC demonstrated significant reductions in astrocyte activation, suggesting a reduction in neuroinflammation. The findings suggest that both EVOO and OLC have neuroprotective effects in reducing Aβ production and neuroinflammation while enhancing synaptic health in the context of AD. | [181] |
| HT | Rat model, specifically focusing on the offspring of rats that were exposed to prenatal stress. | HT was administered at doses of 10 and 50 mg/kg/day. | Neurogenesis and cognitive function: HT supplementation improved learning capacity and memory performance in prenatally stressed offspring. HT prevented the stress-induced downregulation of neural proteins, including BDNF, GAP43, synaptophysin, NMDAR1, NMDANR2A, and NMDANR2B. HT increased the expression of the glucocorticoid receptor in prenatally stressed rats. OS and mitochondrial dysfunction: HT alleviated OS and mitochondrial dysfunction in prenatally stressed rats. HT significantly increased transcription factors FOXO1 and FOXO3, as well as phase II enzyme-related proteins, including Nrf2 and HO-1. | [182] |
| HT | Type-1-like diabetic rats | Specific dosages of DHPG and HT were administered. | Neuroprotective effects: HT demonstrated significant neuroprotective effects in the rat model of type-1 diabetes. Antioxidant activity: HT exerted strong antioxidant effects, helping to reduce OS in brain tissue. Anti-nitrosative stress: HT also contributed to reducing nitrosative stress, which is crucial for protecting neuronal cells. Synergistic effects: The combination of HT and DHPG showed enhanced neuroprotective effects compared to each compound alone. This synergy likely results from their combined antioxidant and anti-nitrosative properties. Protection against retinal damage: The study found that the combination of HT and DHPG helped mitigate retinal nerve cell damage, which is important for preventing diabetic retinopathy. | [183] |
| HT | Caenorhabditis elegans | The treatment involved administering 100 µg/mL of the HT-rich olive extract to Caenorhabditis elegans. | The study demonstrated that the HT-rich olive extract prevents oxidative stress and delays Aβ-induced paralysis in Caenorhabditis elegans. The extract reduced the presence of Aβ aggregates and showed the ability to mitigate proteotoxicity associated with tau protein aggregation. Additionally, the extract exhibited antioxidant properties and enhanced stress resistance in the nematodes, contributing to prolonged longevity and improved health span. Gene reporter strains of Caenorhabditis elegans indicated that the extract influenced various stress-related pathways, such as those involving the DAF-16/FOXO, SKN-1/NRF2, and Hsp-16.2 proteins. | [184] |
| HT | C57BL/6 mice (AD model) | AD-like neurotoxicity was induced in mice by intracerebroventricular injection of soluble oligomeric amyloid β1-42 plus ibotenic acid (oA42i). Treatment: HT was administered orally at a dose of 10 mg/kg/day for 14 days. The administration was performed via oral gavage, and the treatment was initiated 4 days post-surgery for inducing AD-like pathology. | Neuroprotective and cognitive enhancing effects: Spatial memory improvement: HT treatment significantly improved spatial reference and working memory in oA42i-intoxicated mice, as assessed by radial arm maze performance. Molecular mechanisms: MAPK signaling pathways: HT reversed oA42i-induced downregulation of ERK1/2 and RSK2 phosphorylation and inhibited the activation of JNK and p38, which are associated with neuronal death. PI3K/Akt and JAK2/STAT3 pathways: HT restored the phosphorylation levels of Akt1, JAK2, and STAT3, promoting neuronal survival. Apoptosis inhibition: HT treatment modulated the Bcl-2/Bad ratio, reduced cytochrome c release, and decreased the activation of caspase-9 and caspase-3, thereby inhibiting mitochondria-mediated apoptosis. Gene expression: HT upregulated the expression of SIRT1, CREB, and CREB-target genes (BDNF, c-Fos, Nurr1, and Egr1), which are involved in neuronal survival and memory functions. Mitochondrial protection: HT preserved mitochondrial integrity, preventing the structural damage observed in the oA42i group. | [185] |
| HT | Male db/db mice on a C57BL/6J | Mice were divided into three groups: control, low-dose HT (10 mg/kg/day), and high-dose HT (50 mg/kg/day). HT was administered orally for 8 weeks. | Mitochondrial function: HT improved the expression and activity of mitochondrial respiratory chain complexes I, II, and IV in the brain of db/db mice. Specifically, complex I activity was significantly increased. HT treatment enhanced mitochondrial biogenesis and function, indicated by increased expression of PGC-1α and activation of AMPK and SIRT1 pathways. Antioxidant activity: HT induced phase II antioxidant enzymes, including HO-1, SOD1, and SOD2, in the brain of db/db mice. This was associated with a significant reduction in protein oxidation levels. HT improved neuronal survival and function in db/db mice, as evidenced by increased mRNA levels of neuronal markers such as activity-regulated cytoskeleton-associated protein, NMDAR1, and NGF. | [149] |
| HTEE, tTEE MHTEE | Rat | Rats were treated orally with doses of 10 or 20 mg/kg/day of HTEE, TEE, or MHTEE. | Lipid peroxidation was inhibited by HTEE, TEE, and MHTEE. All three compounds showed similar neuroprotective effects, reducing arbitrary units from baseline measurements. Inhibition of 3-nitrotyrosine production was observed for all three compounds. PGE2 production was reduced in the treated groups. Only HTEE inhibited IL-1β production. | [186] |
| HT, HT-AC, Tyr, DOPAC, DA, and sodium ascorbate | Caenorhabditis elegans NL5901 mutant strain | Sodium ascorbate was used to supplement, as it allowed for stabilization by avoiding autoxidation. Specific dosages of HT, HT-AC, Tyr, DOPAC, and DA were administered. | Reduction in α-Syn aggregation: DOPAC and HT-AC were able to decrease the aggregation by 79.2% and 76.2%, respectively. These compounds exhibited a positive effect on the longevity of Caenorhabditis elegans, as well. DA was also able to reduce the aggregation. | [155] |
| HT, nitrohydroxytyrosol, nitrohydroxytyrosol acetate, and ethyl nitrohydroxytyrosol ether | Rat model | The animals received either an acute (single dose; 20 mg/kg, intraperitoneally) or a chronic (one daily dose for 5 days; 20 mg/kg) treatment of HT and its nitro derivatives. | The treatments produced a significant increase in the intracellular levels of DA and its metabolite, DOPAC. The increase in DA levels was similar to that seen with the commercial COMT inhibitor, Ro41-0960. Chronic treatment effects were stronger than acute treatment effects. Unlike Ro41-0960, HT and its derivatives did not produce a significant decrease in the intracellular level of homovanillic acid, although the chronic treatment effect was stronger than the acute treatment effect. These results suggest that these compounds could inhibit catechol-O-methyltransferase activity. | [187] |
| HT-AC | APP/PS1 (AD model). | The administration method involved oral administration of HT-AC to the transgenic mice. | The study found that HT-AC improved cognitive functions in AD mice, specifically enhancing escape latency, escape distance, and the number of platform crossings in the water maze test. The beneficial effects included amelioration of neuronal apoptosis and reduction in inflammatory cytokine levels. HT-AC stimulated the transcription of ERβ, enhancing neuronal viability and electrophysiological activity in primary neurons. These effects were abolished when ERβ was deficient, indicating the involvement of ERβ in mediating the neuroprotective effects of HT-AC. | [188] |
| OLC | TgSwDI mice (AD model). | The mice were treated with OLC for 4 weeks. | Amyloid load: OLC treatment significantly decreased amyloid load in the hippocampal parenchyma and microvessels. Cerebral clearance: This reduction was associated with enhanced cerebral clearance of Aβ across the BBB. Proteins involved in clearance: OLC increased the expression of important amyloid clearance proteins at the BBB, including P-gp and LRP1. It also activated the ApoE-dependent amyloid clearance pathway in the mice’s brains. Anti-inflammatory effects: OLC reduced astrocyte activation and IL-1β levels in the brains of these mice. Mechanistic studies: Demonstrated OLC’s ability to increase P-gp and LRP1 expression, and to enhance the ApoE-dependent clearance pathway. | [138] |
| OLC | 5xFAD mouse (AD model) | Dietary intake: EVOO was consumed as a medical food. Combination treatment: EVOO was combined with donepezil, an acetylcholine esterase inhibitor approved for all stages of AD. | EVOO consumption combined with donepezil significantly reduced Aβ load and related pathological changes. Enhancement in Aβ clearance pathways, including BBB clearance and enzymatic degradation. Shifting APP processing toward the non-amyloidogenic pathway. Improved synaptic function. Strengthened BBB integrity. Decreased inflammation associated with Aβ pathology. | [189] |
| OLC | Wistar albino rat model of traumatic brain injury. | The study used 26 adults male Wistar albino rats. The rats were divided into four groups: Group 1: Sham group (n = 5). Group 2: Trauma group treated with 10 mg/kg saline intraperitoneally (IP) twice a day (n = 5). Group 3: Rats treated with 10 mg/kg OLC IP twice a day (n = 8). Group 4: Rats treated with 30 mg/kg OLC IP twice a day (n = 8). Brain samples were collected 72 h after injury. | OLC treatment showed neuroprotective effects by targeting secondary injury mechanisms, reducing OS, and inflammation, and promoting tissue repair and recovery in a dose-dependent manner. | [190] |
| OLC | Wild-type C57BL/6 mice | Wild-type C57BL/6 mice were administered OLC intraperitoneally at a dose of 10 mg/kg twice daily for 2 weeks. | Enhanced clearance of 125I-Aβ40 from the brain was observed in OLC-treated mice, with an increase in brain efflux index(%) from 62.0 ± 3.0% (control) to 79.9 ± 1.6% (OLC-treated). OLC has anti-inflammatory properties similar to ibuprofen, inhibiting inflammatory markers and reducing OS. | [161] |
| OLC-rich EVOO. | TgSwDI (AD model) | OLC-rich EVOO was administered starting at the age of 6 months for a treatment duration of 3 months. | Neuroinflammation: OC-rich EVOO reduced neuroinflammation by inhibiting the NLRP3 inflammasome. Autophagy: OC-rich EVOO induced autophagy through activation of the AMPK/ULK1 pathway. BBB: OC-rich EVOO restored BBB function, reducing AD-associated pathology. | [147] |
| OLE | Experimental spinal cord injury model in rats | The treatment involved administering OLE at a dosage of 20 mg/kg intraperitoneally, immediately and 1 h after the spinal cord injury. | MDA levels were significantly decreased in the OLE treatment groups. GSH levels were significantly increased in the OLE treatment groups. Apoptosis: There was a greater Bcl-2 expression and attenuated Bax expression in the OLE-treated rats. TUNEL-positive reactions were significantly reduced in the OLE treatment groups. The treatment with OLE also improved behavioral function compared to the trauma group. | [191] |
| OLE | TgCRND8 (AD model) | OLE was administered at 50 mg/kg of diet for 8 weeks to 6-month-old TgCRND8 mice. | PARP1 activation and PAR formation: OLE treatment rescued PARP1 activation and the levels of its product, PAR, to control values. Neurodegeneration: The beneficial effects of OLE against neurodegeneration were highlighted the TgCRND8 mouse model. | [192] |
| OLE | 5xFAD (AD model) | The administration method involved feeding the mice an OLE-enriched diet at a dosage of 695 mg/kg body weight per day for three months, starting when the mice were three months old. | The study found that OLE reduced neuroinflammation by inhibiting the NF-κB pathway and suppressing the activation of NLRP3 inflammasomes and RAGE/HMGB1 pathways. OLE reduced total Aβ brain levels by increasing clearance and reducing production of Aβ, enhancing BBB integrity and function. These effects collectively improved memory function in the mice. The results suggest that the consumption of OLE as a dietary supplement may stop or slow the progression of AD. | [145] |
| OleA | Transgenic Caenorhabditis elegans strains CL2006 and CL4176, which are simplified models of AD and sporadic inclusion body myositis | The OleA was administered to Caenorhabditis elegans, with the CL2006 strain being fed OleA and the CL4176 strain receiving OleA before the induction of the Aβ transgene expression. | OleA-fed CL2006 worms: Reduced Aβ plaque deposition. Fewer toxic Aβo. Remarkably decreased paralysis. Increased lifespan compared to untreated animals. OleA-treated CL4176 worms: Protective effect observed when OleA was administered before the induction of the Aβ transgene expression. These effects were specific, dose-related, and not mediated by the known polyphenolic antioxidant activity. | [193] |
| OleA | Rat model | The administration involved injecting a 1.5 µL solution containing the following: OleA (450 µM) or Aggregated Aβ42 peptide (50 µM) in the presence or absence of OleA (450 µM). Control rats were injected with a vehicle (1.5 µL). | Co-administration of OleA counteracted Aβ42 toxicity. The number of choline acetyltransferase-positive neurons in the nucleus basalis magnocellularis was preserved. The number of A11-positive oligomers was lower in the Aβ42-OleA-injected nucleus basalis of Meynert. Glia reaction was lower in the Aβ42-OleA-injected nucleus basalis magnocellularis. | [194] |
| Olive oil | Mice with induced ischemia-reperfusion | Pre-treatment with olive oil for a week. | Significantly reduced cell death and decreased memory loss. | [195] |
| Olive oil | Wistar rats | Rats were divided into groups and administered different doses of olive oil (0.25, 0.5, and 0.75 mL/kg/day) by gavage for a specific period. | Reduction in neurological deficits and infarct volume: Olive oil administration significantly reduced total neurological deficit scores in rats subjected to middle cerebral artery occlusion. Olive oil at a dose of 0.75 mL/kg/day significantly decreased infarct volume in total, cortex, and striatum areas of the brain. Molecular effects: The study measured TNFR1 and NF-κB protein expression in the cortex and striatum regions, indicating involvement in the inflammatory pathway modulation. Antioxidant and anti-inflammatory effects: Olive oil contains compounds with these effects, which are beneficial in reducing ischemic damages. | [196] |
| Olive oil | NAFLD pig model | The administration method involved feeding the pigs diets enriched with olive oil and coconut oil. | The study found that olive- and coconut-oil-enriched diets decreased secondary bile acids. These diets regulated metabolic and transcriptomic markers of brain injury in the frontal cortexes of NAFLD pigs. The results included improvements in various biochemical markers related to inflammation and brain function, suggesting potential neuroprotective effects. | [197] |
| Olive oil | Mice were injected intracerebroventricularly with Aβ25–35 to induce AD-like pathology | Olive oil was administered orally at a dose of 500 mg/kg/day for 14 days. | Cognitive function: Olive oil did not significantly improve performance in the T-maze and novel object recognition tests compared to the control group, indicating limited effect on spatial and recognition memory. In the Morris water maze test, olive oil did not significantly reduce the escape latency or increase the time spent in the target quadrant, suggesting limited improvement in spatial learning and memory. OS: Olive oil treatment resulted in a significant decrease in MDA levels in the brain, kidney, and liver, indicating reduced lipid peroxidation. Olive oil reduced NO production in the liver but not significantly in the brain. Enzyme activity and protein expression: Olive oil did not significantly inhibit AChE activity in the brain. Olive oil administration slightly reduced the expression levels of iNOS and COX-2, which are markers of inflammation, but the reduction was not as significant as that observed with perilla oil. Olive oil did not significantly upregulate BDNF expression compared to the control group. | [198] |
| Olive oil | PD induced by rotenone in Swiss albino male adult mice. | Control Group: 2 mL/kg olive oil by oral route. Experimental Groups: 2.5 mg/kg rotenone by intraperitoneal route. Group 3: 7.5 mg/kg Levodopa p.o. Groups 4 and 5: 20 mg/kg and 40 mg/kg embelin p.o., respectively. Groups 6 and 7: 20 mg/kg and 40 mg/kg embelin p.o. respectively, combined with 7.5 mg/kg Levodopa p.o. | The combination of embelin (40 mg/kg) and levodopa (7.5 mg/kg) showed superior neuroprotective activity compared to other treatment groups. This conclusion was based on biochemical parameters, histopathological observations, and immunohistochemical analysis of α-Syn protein in the brain. | [199] |
| PN | Mice: Cholinergic dysfunction-induced memory impairments, a model for dementia and AD | PN administered at 25 mg/kg orally in a dose-dependent manner. | Memory improvement: PN ameliorated memory impairment in the dementia model induced by cholinergic blockade in the passive avoidance test. Synaptic plasticity: Facilitated induction of hippocampal long-term potentiation, a cellular model of learning and memory. Enzyme inhibition: Blocked AchE activity in a concentration-dependent manner. | [200] |
| Tyr | Caenorhabditis elegans (PD model) | Tyr treatment: Administered to Caenorhabditis elegans to study its effects on α-Syn aggregation, neurodegeneration, and OS. | Reduction in α-Syn aggregation: Tyr is effective in reducing α-Syn inclusions. Decreased toxicity and extended lifespan: Treated nematodes showed lower toxicity and extended lifespan. Neuroprotection: Tyr delayed α-Syn-dependent degeneration of dopaminergic neurons in vivo. Reduction in OS: Tyr treatment reduced reactive ROS levels. Promotion of chaperone and antioxidant enzyme expression: Tyr promoted the expression of specific chaperones and antioxidant enzymes. | [201] |
| VOO. The composition of VOO included fatty acids such as oleic acid (68.822%), linoleic acid (9.951%), palmitic acid (15.99%), stearic acid (1.815%), alpha-linolenic acid (0.602%), and minor components like alpha-tocopherol (210 mg/kg) and total polyphenols (320 mg/kg) | Male Wistar rats (200–300 g) | The treatments administered were: Control group: Rats received saline via gastric gavage. Treatment groups: Rats received 0.25, 0.5, or 0.75 mL/kg/day of VOO via gastric gavage. Treatments were administered daily for 30 days before inducing ischemia-reperfusion injury. | Reduction in infarct volume: VOO treatment significantly reduced infarct volumes in the brain compared to controls, with the most significant reduction observed at the highest dose (0.75 mL/kg/day). Reduction in brain edema: VOO treatment reduced brain water content in the infarcted hemisphere, indicating reduced brain edema. The doses of 0.5 and 0.75 mL/kg/day were effective, while the lower dose (0.25 mL/kg/day) had no significant effect. Improvement in BBB integrity: VOO treatment reduced BBB permeability. The higher doses (0.5 and 0.75 mL/kg/day) significantly reduced BBB permeability compared to the control group. Improvement in neurological deficit scores: VOO treatment improved neurological outcomes, with lower neurological deficit scores observed in treated groups compared to controls. Lipid profile modulation: VOO treatment reduced the LDL/HDL ratio and increased HDL levels, indicating a favorable effect on blood lipid profiles. | [202] |
| VOO. The main components of VOO include fatty acids such as oleic acid (C18:1, 76.5%) and linoleic acid (C18:2, 9.9%), along with minor components like alpha-tocopherol (173 mg/kg) and total phenolic compounds (250 mg/kg) | Adult male Wistar rats (200–250 g). Experimental diabetes was induced in the rats using a single femoral intravenous injection of 50 mg/kg streptozotocin | The treatments administered were:
| Neuroprotective effects: Both VOO and aspirin significantly reduced LDH) efflux after reoxygenation, indicating reduced cell damage (−54.1% for aspirin, −51.3% for VOO, and −72.9% for aspirin plus VOO). Reduction in lipid peroxides: Lipid peroxides in brain slices were reduced following treatment with aspirin (−17.9%), VOO (−37.3%), and the combination of both (−49.2%). Inhibition of nitric oxide production: The treatments inhibited the production of NO after reoxygenation (−46.5% for aspirin, −48.2% for VOO, and −75.8% for aspirin plus VOO). The activity of inducible iNOS was also reduced (−31.8% for aspirin, −29.1% for VOO, and −56.0% for aspirin plus VOO). Enhanced antioxidant defense: The combined treatment of aspirin and VOO resulted in higher GSH levels and increased activities of antioxidant enzymes such as GPx and GSH reductase | [203] |
| Status | Study | Key Findings/Aim | Reference |
|---|---|---|---|
| Complete | Three-city study | Olive oil consumption associated with lower odds of cognitive deficits and decline. | [204] |
| PREDIMED-NAVARRA | Mediterranean diet with EVOO or nuts improves global cognition independently of potential confounders. | [205] | |
| MICOIL Pilot Study | High and moderate phenolic EVOO linked to improved cognitive performance, potentially preventing MCI progression to Alzheimer’s. | [206] | |
| AU-ROOAD | EVOO reduces blood–brain barrier permeability, lowers amyloid-B levels, and improves dementia symptoms. | [207] | |
| Ongoing | GOLDENNCT04440020 | Investigates the effects of a Mediterranean diet and olive leaf beverages on memory and cognitive function. | [208] |
| NCT05363267 | Studies the combined effects of high-phenolic EVOO and curcumin on neurofibromatosis, Type 1. | [209] | |
| NCT05929924 | Assess whether EVOO has a protective effect against AD in healthy individuals whose family history includes the disease. | [210] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonçalves, M.; Vale, N.; Silva, P. Neuroprotective Effects of Olive Oil: A Comprehensive Review of Antioxidant Properties. Antioxidants 2024, 13, 762. https://doi.org/10.3390/antiox13070762
Gonçalves M, Vale N, Silva P. Neuroprotective Effects of Olive Oil: A Comprehensive Review of Antioxidant Properties. Antioxidants. 2024; 13(7):762. https://doi.org/10.3390/antiox13070762
Chicago/Turabian StyleGonçalves, Marta, Nuno Vale, and Paula Silva. 2024. "Neuroprotective Effects of Olive Oil: A Comprehensive Review of Antioxidant Properties" Antioxidants 13, no. 7: 762. https://doi.org/10.3390/antiox13070762
APA StyleGonçalves, M., Vale, N., & Silva, P. (2024). Neuroprotective Effects of Olive Oil: A Comprehensive Review of Antioxidant Properties. Antioxidants, 13(7), 762. https://doi.org/10.3390/antiox13070762










