Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants and Data Collection
2.2. Assessment of Vaccination Attitude
2.3. Sociodemographic Variables
2.4. Health-Related Behavior and COVID-19-Related Psychological Constructs
2.5. Anti-Scientific Attitude
2.6. Pseudoscientific Belief
2.7. General Anxiety
2.8. Misinformation on Vaccines
2.9. Analysis
2.10. Ethical Issues
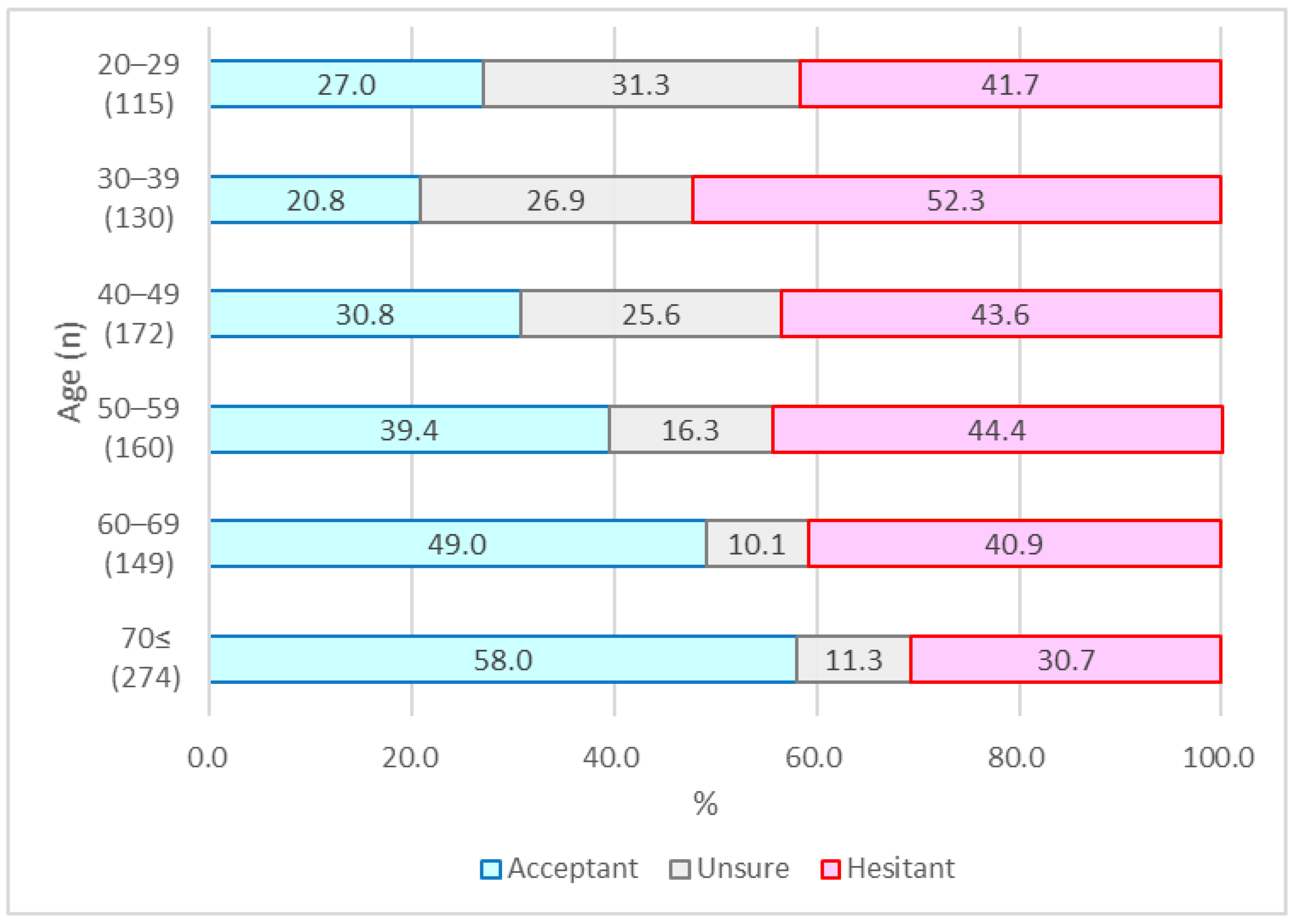
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fadda, M.; Albanese, E.; Suggs, L.S. When a COVID-19 vaccine is ready, will we all be ready for it? Int. J. Public Health 2020, 65, 711–712. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 25 November 2021).
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy: An overview. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Dubé, E. Restoring confidence in vaccines in the COVID-19 era. Expert Rev. Vaccines 2020, 19, 991–993. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Larson, H.J.; De Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights through a 67-Country Survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Harrison, E.A.; Wu, J.W. Vaccine confidence in the time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef] [Green Version]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33 (Suppl. 4), D66–D71. [Google Scholar] [CrossRef]
- Viswanath, K.; Bekalu, M.; Dhawan, D.; Pinnamaneni, R.; Lang, J.; McLoud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 2021, 21, 818. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dube, E.; Schuster, M.; MacDonald, N.E.; Wilson, R.; The SAGE Working Group on Vaccine Hesitancy. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Matsui, Y. Why high school students believe in paranormal phenomena? In Mysterious Phenomena: Children’s Mind and Education; Kinoshita, K.S., Ed.; Kitaohji Publishing: Kyoto, Japan, 1997; pp. 15–35. [Google Scholar]
- Nakajima, S.; Tatsuya, S.; Watanabe, Y. Development of the paranormal phenomena belief scale. J. Jpn. Skept. 1993, 2, 69–79. [Google Scholar]
- Iwanaga, M.; Sakata, K. Preliminary research on the dominant factors in paranormal beliefs (1): Effects of personal factors. Mem. Fac. Integr. Arts Sci. Hiroshima Univ. Sci. Rep. 1998, 24, 75–85. [Google Scholar]
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; et al. Acceptance of a COVID-19 Vaccine in Japan during the COVID-19 Pandemic. Vaccines 2021, 9, 210. [Google Scholar] [CrossRef]
- Okubo, R.; Yoshioka, T.; Ohfuji, S.; Matsuo, T.; Tabuchi, T. COVID-19 Vaccine Hesitancy and Its Associated Factors in Japan. Vaccines 2021, 9, 662. [Google Scholar] [CrossRef]
- Our World in Data. 2021. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 25 November 2021).
- Ministry of Health, Labour and Welfare. Situation Report. 2021. Available online: https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou_00006.html (accessed on 25 November 2021).
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef]
- Larson, H.J.; Smith, D.M.D.; Paterson, P.; Cumming, M.; Eckersberger, E.; Freifeld, C.C.; Ghinai, I.; Jarrett, C.; Paushter, L.; Brownstein, J.S.; et al. Measuring vaccine confidence: Analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect. Dis. 2013, 13, 606–613. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Hickler, B.; Guirguis, S.; Obregon, R. Vaccine Special Issue on Vaccine Hesitancy. Vaccine 2015, 33, 4155–4156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eskola, J.; Duclos, P.; Schuster, M.; MacDonald, N.E.; The SAGE Working Group on Vaccine Hesitancy. How to deal with vaccine hesitancy? Vaccine 2015, 33, 4215–4217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomson, A.; Vallée-Tourangeau, G.; Suggs, L.S. Strategies to increase vaccine acceptance and uptake: From behavioral insights to context-specific, culturally-appropriate, evidence-based communications and interventions. Vaccine 2018, 36, 6457–6458. [Google Scholar] [CrossRef] [PubMed]
- Nyhan, B.; Reifler, J.; Richey, S.; Freed, G.L. Effective Messages in Vaccine Promotion: A Randomized Trial. Pediatrics 2014, 133, e835–e842. [Google Scholar] [CrossRef] [Green Version]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; The SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biasio, L.R. Vaccine hesitancy and health literacy. Hum. Vaccines Immunother. 2017, 13, 701–702. [Google Scholar] [CrossRef] [PubMed]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 vaccine literacy: A preliminary online survey. Hum. Vaccines Immunother. 2021, 17, 1304–1312. [Google Scholar] [CrossRef] [PubMed]
- Lorini, C.; Santomauro, F.; Donzellini, M.; Capecchi, L.; Bechini, A.; Boccalini, S.; Bonanni, P.; Bonaccorsi, G. Health literacy and vaccination: A systematic review. Hum. Vaccines Immunother. 2018, 14, 478–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]

| Vaccination Attitude | |||||
|---|---|---|---|---|---|
| Total | Acceptant (%) | Unsure (%) | Hesitant (%) | p | |
| Gender | 1000 | 406 (40.6) | 187 (18.7) | 407 (40.7) | |
| Female | 520 | 202 (38.9) | 104 (20.0) | 214 (41.2) | 0.3956 |
| Male | 480 | 204 (42.5) | 83 (17.3) | 193 (40.2) | |
| Other | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Residential area | |||||
| Tokyo metropolitan area | 421 | 176 (41.8) | 78 (18.5) | 167 (39.7) | 0.9038 |
| Northern Japan | 121 | 48 (39.7) | 23 (19.0) | 50 (41.3) | |
| Central Japan | 129 | 53 (41.1) | 25 (19.4) | 51 (39.5) | |
| Western Japan | 264 | 106 (40.2) | 52 (19.7) | 106 (40.2) | |
| Southern Japan | 65 | 23 (35.4) | 9 (13.9) | 33 (50.8) | |
| Education | |||||
| University-level education | 594 | 246 (41.4) | 119 (20.0) | 229 (38.6) | 0.1931 |
| Below university level | 406 | 160 (39.4) | 68 (16.8) | 178 (43.8) | |
| Annual income (in JPY) | |||||
| <JPY 2,000,000 | 107 | 32 (29.9) | 18 (16.8) | 57 (53.3) | 0.0373 |
| JPY 2,000,000–JPY 4,000,000 | 239 | 105 (43.9) | 39 (16.3) | 95 (39.8) | |
| JPY 4,000,000–JPY 6,000,000 | 278 | 105 (37.8) | 53 (19.1) | 120 (43.2) | |
| >JPY 6,000,000 | 376 | 164 (43.6) | 77 (20.5) | 135 (35.9) | |
| Underlying condition | |||||
| One or more | 237 | 116 (49.0) | 31 (13.1) | 90 (38.0) | 0.0038 |
| None | 763 | 290 (38.0) | 156 (20.5) | 317 (41.6) | |
| Vaccination Attitude | |||||
|---|---|---|---|---|---|
| Total | Acceptant (%) | Unsure (%) | Hesitant (%) | p | |
| Gender | 1000 | 855 (85.5) | 56 (5.6) | 89 (8.9) | |
| Female | 520 | 451 (86.7) | 28 (5.4) | 41 (7.9) | 0.464 |
| Male | 480 | 404 (84.2) | 28 (5.7) | 48 (10.0) | |
| Other | 0 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Residential area | |||||
| Tokyo metropolitan area | 421 | 367 (87.2) | 24 (5.7) | 30 (7.1) | 0.204 |
| Northern Japan | 121 | 96 (79.3) | 10 (8.3) | 15 (12.4) | |
| Central Japan | 129 | 117 (90.7) | 3 (2.3) | 9 (7.0) | |
| Western Japan | 264 | 223 (84.5) | 14 (5.3) | 27 (10.2) | |
| Southern Japan | 65 | 52 (80.0) | 5 (7.7) | 8 (12.3) | |
| Education | |||||
| University-level education | 594 | 531 (89.4) | 27 (4.6) | 36 (6.1) | <0.000 |
| Below university level | 406 | 324 (79.8) | 29 (7.1) | 53 (13.1) | |
| Annual income (in JPY) | |||||
| <JPY 2,000,000 | 107 | 91 (85.1) | 7 (6.5) | 9 (8.4) | 0.2464 |
| JPY 2,000,000–JPY 4,000,000 | 239 | 208 (87.0) | 11 (4.6) | 20 (8.4) | |
| JPY 4,000,000–JPY 6,000,000 | 278 | 228 (82.0) | 15 (5.4) | 35 (12.6) | |
| >JPY 6,000,000 | 376 | 328 (87.2) | 23 (6.1) | 25 (6.7) | |
| Underlying condition | |||||
| One or more | 237 | 206 (86.9) | 13 (5.5) | 20 (8.4) | 0.9543 |
| None | 703 | 651 (85.3) | 43 (5.6) | 69 (9.0) | |
| Vaccination Attitude | |||||
|---|---|---|---|---|---|
| Health Behavior | Total (IQR) | Acceptant (IQR) | Unsure (IQR) | Hesitant (IQR) | p |
| Influenza vaccination | 3.0 (1.0, 5.0) | 4.0 (1.0, 5.0) | 1.0 (1.0, 3.0) | 1.0 (1.0, 2.0) | <0.0001 |
| Medical checkups | 5.0 (3.0, 5.0) | 5.0 (4.0, 5.0) | 3.0 (2.0, 5.0) | 3.0 (1.0, 5.0) | <0.0001 |
| Exercise | 3.0 (2.0, 4.0) | 3.0 (2.0, 4.0) | 3.0 (1.3, 4.0) | 2.0 (1.0, 4.0) | 0.0655 |
| Smoking | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 1.0 (1.0, 3.0) | 1.0 (1.0, 1.0) | 0.1355 |
| COVID-19-related anxiety | 3.0 (3.0, 4.0) | 3.0 (3.0, 4.0) | 3.0 (3.0, 4.0) | 3.0 (2.0, 4.0) | <0.0001 |
| Risk perception | 2.0 (2.0, 3.0) | 2.0 (2.0, 3.0) | 2.0 (2.0, 3.0) | 2.0 (1.0, 2.0) | 0.0002 |
| Concerns for adverse effects | 3.0 (2.0, 3.0) | 3.0 (2.0, 3.0) | 3.0 (3.0, 4.0) | 4.0 (3.0, 4.0) | <0.0001 |
| Trust in the government | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 2.0 (1.0, 2.0) | 0.0070 |
| Vaccination Attitude | |||||
|---|---|---|---|---|---|
| Total (IQR) | Acceptant (IQR) | Unsure (IQR) | Hesitant (IQR) | p | |
| Vaccination attitude | 37.0 (32.0, 41.0) | 38.0 (34.0, 42.0) | 30.0 (27.0, 32.3) | 26.0 (17.5, 30.0) | <0.0001 |
| General anxiety | 28.0 (21.0, 33.0) | 28.0 (20.0, 33.0) | 30.0 (26.3, 32.0) | 29.0 (22.0, 33.0) | 0.1070 |
| Anti-science | 15.0 (14.0, 17.0) | 15.0 (13.0, 17.0) | 16.0 (15.0, 18.0) | 16.0 (15.0, 18.5) | 0.0003 |
| Pseudoscience | 39.0 (29.0, 45.8) | 39.0 (29.0, 45.0) | 40.0 (34.3, 46.8) | 38.0 (29.0, 49.0) | 0.1360 |
| Misinformation | 9.0 (6.0, 12.0) | 8.0 (6.0, 12.0) | 12.0 (10.0, 13.0) | 12.0 (10.5, 17.0) | <0.0001 |
| AOR | 95% CI | p | ||
|---|---|---|---|---|
| Gender | Male | 0.817 | 0.633–1.053 | 0.119 |
| Age group (years) | 20–29 | Ref | ||
| 30–39 | 0.682 | 0.421–1.105 | 0.120 | |
| 40–49 | 1.019 | 0.647–1.606 | 0.936 | |
| 50–59 | 1.270 | 0.795–2.031 | 0.317 | |
| 60–69 | 1.572 | 0.970–2.549 | 0.066 | |
| ≥70 | 2.150 | 1.388–3.330 | 0.001 | |
| Residential area | Tokyo metropolitan area | Ref | ||
| Northern Japan | 1.004 | 0.671–1.505 | 0.982 | |
| Central Japan | 0.984 | 0.606–1.598 | 0.948 | |
| Western Japan | 1.043 | 0.81–1.598 | 0.846 | |
| Southern Japan | 0.907 | 0.495–1.661 | 0.752 | |
| Education | University-level education | 0.976 | 0.748–1.274 | 0.859 |
| Annual income (in JPY) | <JPY 2,000,000 | Ref | ||
| JPY 2,000,000–JPY 4,000,000 | 1.539 | 0.967–2.449 | 0.069 | |
| JPY 4,000,000–JPY 6,000,000 | 1.588 | 1.003–2.514 | 0.049 | |
| >JPY 6,000,000 | 1.846 | 1.176–2.900 | 0.008 | |
| Underlying condition | One or more | 0.974 | 0.783–1.213 | 0.816 |
| Influenza vaccination | 1 point | 1.331 | 1.230–1.441 | <0.000 |
| Medical checkups | 1 point | 1.102 | 0.997–1.218 | 0.056 |
| Exercise | 1 point | 1.100 | 1.006–1.203 | 0.036 |
| Smoking | 1 point | 0.974 | 0.783–1.213 | 0.253 |
| AOR | 95% CI | p | ||
|---|---|---|---|---|
| Gender | Male | 1.282 | 0.791–2.077 | 0.313 |
| Age group (years) | 20–29 | Ref | ||
| 30–39 | 0.675 | 0.322–1.418 | 0.300 | |
| 40–49 | 1.128 | 0.540–2.355 | 0.749 | |
| 50–59 | 1.501 | 0.671–3.383 | 0.320 | |
| 60–69 | 2.087 | 0.763–5.711 | 0.152 | |
| ≥70 | 0.920 | 0.409–2.067 | 0.839 | |
| Residential area | Tokyo metropolitan area | Ref | ||
| Northern Japan | 1.772 | 0.900–3.487 | 0.098 | |
| Central Japan | 2.219 | 0.898–5.479 | 0.084 | |
| Western Japan | 1.592 | 0.787–3.219 | 0.196 | |
| Southern Japan | 1.281 | 0.495–3.318 | 0.609 | |
| Education | University-level education | 1.629 | 1.094–2.743 | 0.019 |
| Annual income (in JPY) | <JPY 2,000,000 | Ref | 0.790–1.216 | 0.854 |
| JPY 2,000,000–JPY 4,000,000 | 0.781 | 0.349–1.747 | 0.547 | |
| JPY 4,000,000–JPY 6,000,000 | 0.783 | 0.362–1.694 | 0.535 | |
| >JPY 6,000,000 | 0.813 | 0.377–1.754 | 0.598 | |
| Underlying condition | One or more | 0.905 | 0.617–1.327 | 0.609 |
| Influenza vaccination | 1 point | 1.450 | 1.230–1.710 | <0.000 |
| Medical checkups | 1 point | 1.349 | 1.158–1.572 | <0.000 |
| Exercise | 1 point | 1.060 | 0.901–1.246 | 0.485 |
| Smoking | 1 point | 0.919 | 0.765–1.103 | 0.364 |
| COVID-19-related anxiety | 1 point | 1.882 | 1.374–2.579 | <0.000 |
| Risk perception | 1 point | 1.578 | 1.128–2.206 | 0.008 |
| Concern for adverse effects | 1 point | 0.293 | 0.213–0.404 | <0.000 |
| Trust in the government | 1 point | 1.080 | 0.803–1.451 | 0.626 |
| General anxiety | 1 point | 1.048 | 1.013–1.084 | 0.008 |
| Anti-science | 1 point | 0.950 | 0.875–1.030 | 0.208 |
| Pseudoscience | 1 point | 1.014 | 0.993–1.036 | 0.199 |
| Misinformation | 1 point | 0.821 | 0.770–0.875 | <0.000 |
| β | 95% CI | p | ||
|---|---|---|---|---|
| Gender | Male | −0.176 | −0.508–0.155 | 0.2973 |
| Age group (years) | 20–29 | −0.747 | −1.594–0.100 | 0.0839 |
| 30–39 | −1.630 | −2.438–−0.821 | <0.0001 | |
| 40–49 | −0.196 | −0.908–0.516 | 0.5893 | |
| 50–59 | 0.369 | −0.347–1.084 | 0.3120 | |
| 60–69 | 0.780 | 0.020–1.541 | 0.0443 | |
| ≥70 | 1.424 | 0.744–2.103 | <0.0001 | |
| Residential area | Tokyo metropolitan area | 0.197 | −0.347–0.740 | 0.4782 |
| Northern Japan | −0.681 | −1.474–0.111 | 0.0919 | |
| Central Japan | 0.467 | −0.306–1.240 | 0.2364 | |
| Western Japan | −0.053 | −0.655–0.538 | 0.8617 | |
| Southern Japan | 0.072 | −0.946–1.089 | 0.8900 | |
| Education | University-level education | −0.016 | −0.352–0.321 | 0.9270 |
| Annual income (in JPY) | <JPY 2,000,000 | −0.152 | −0.921–0.617 | 0.6985 |
| JPY 2,000,000–JPY 4,000,000 | −0.511 | −1.093–0.070 | 0.0845 | |
| JPY 4,000,000–JPY 6,000,000 | 0.494 | −0.053–1.041 | 0.0766 | |
| >JPY 6,000,000 | 0.169 | −0.357–0.695 | 0.5277 | |
| Underlying condition | One or more | −0.076 | −0.467–0.316 | 0.7049 |
| Influenza vaccination | 1 point | 0.563 | 0.356–0.769 | <0.0001 |
| Medical checkups | 1 point | 0.431 | 0.177–0.684 | 0.0009 |
| Exercise | 1 point | 0.323 | 0.095–0.551 | 0.0055 |
| Smoking | 1 point | −0.020 | −0.301–0.260 | 0.8868 |
| COVID-19-related anxiety | 1 point | 1.763 | 1.314–2.212 | <0.0001 |
| Concerns for adverse effects | 1 point | −2.400 | −2.809–−1.991 | <0.0001 |
| Risk perception | 1 point | 0.446 | −0.019–0.911 | 0.0602 |
| Trust in the government | 1 point | 1.634 | 1.226–2.041 | <0.0001 |
| General anxiety | 1 point | 0.006 | −0.039–0.052 | 0.7806 |
| Anti-science | 1 point | −0.131 | −0.240–−0.021 | 0.0194 |
| Pseudoscience | 1 point | 0.066 | 0.036–0.095 | <0.0001 |
| Misinformation | 1 point | −0.788 | −0.884–−0.692 | <0.0001 |
| AOR | 95% CI | p | ||
|---|---|---|---|---|
| Age group (years) | 20–29 | Ref | - | - |
| 30–39 | 1.173 | 0.284–4.843 | 0.8251 | |
| 40–49 | 1.028 | 0.271–3.908 | 0.9672 | |
| 50–59 | 0.567 | 0.139–2.322 | 0.4305 | |
| 60–69 | 1.309 | 0.227–7.539 | 0.7629 | |
| ≥70 | 0.217 | 0.048–0.987 | 0.0481 | |
| Education | University-level education | 3.408 | 1.345–8.636 | 0.0098 |
| Annual income (in JPY) | <JPY 2,000,000 | Ref | - | - |
| JPY 2,000,000–JPY 4,000,000 | 0.226 | 0.056–0.921 | 0.0381 | |
| JPY 4,000,000–JPY 6,000,000 | 0.182 | 0.047–0.702 | 0.0134 | |
| >JPY 6,000,000 | 0.253 | 0.065–0.985 | 0.0475 | |
| Influenza vaccination | 1 point | 1.104 | 0.788–1.546 | 0.5663 |
| Medical checkups | 1 point | 1.389 | 1.047–1.842 | 0.0225 |
| COVID-19-related anxiety | 1 point | 2.123 | 1.285–3.508 | 0.0033 |
| Concerns for adverse effects | 1 point | 0.335 | 0.195–0.574 | <0.0001 |
| Misinformation | 1 point | 0.879 | 0.789–0.978 | 0.0183 |
| n (%) | |
|---|---|
| Current infection status including emergence of variants. | 20 (29.9) |
| People around me got vaccinated. | 17 (25.4) |
| Hoping to get back to a normal life. | 15 (22.4) |
| Family members encouraged me to get a vaccine. | 12 (17.9) |
| Understood the effects of the vaccines. | 2 (3.0) |
| The specialists encouraged a vaccination. | 1 (1.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harada, T.; Watanabe, T. Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors. Vaccines 2022, 10, 25. https://doi.org/10.3390/vaccines10010025
Harada T, Watanabe T. Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors. Vaccines. 2022; 10(1):25. https://doi.org/10.3390/vaccines10010025
Chicago/Turabian StyleHarada, Takayuki, and Takaaki Watanabe. 2022. "Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors" Vaccines 10, no. 1: 25. https://doi.org/10.3390/vaccines10010025
APA StyleHarada, T., & Watanabe, T. (2022). Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors. Vaccines, 10(1), 25. https://doi.org/10.3390/vaccines10010025





