The Multidimensional Vaccine Hesitancy Scale: A Validation Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Translation and Adaptation of MVHS into Romanian
2.3. Measures
- Multidimensional vaccine hesitancy scale–MVHS [17] measures vaccination hesitancy behaviour, and it has 32 items assessed on a scale from 1 (strongly disagree) to 7 (strongly agree).
- The scale of COVID-19 vaccine willingness has two items assessed on a scale from 1 (extremely disinterested) to 7 (extremely willing): Please show how willing you are to get an anti-COVID-19 vaccine next year if (1) the vaccine is free and if (2) it costs 2500 lei (Romanian currency). The internal consistency coefficients are Cronbach’α = 0.71 (95%CI: 0.66–0.76) and McDonald’ s ω = 0.71 (95%CI: 0.67–0.75).
- The scale of flu vaccine willingness. Similarly, two items were used on a scale from 1 (extremely disinterested) to 7(extremely willing): Please show how willing you are to get a flu vaccine next year if (1) it is free and if (2) it costs 2500 lei (Romanian currency). For the respective coefficients, the acceptable value, Cronbach’s α 0.67 (95%CI: 0.60–0.72) and McDonald’ s ω = 0.66 (95%CI: 0.60–0.70). The two scales were inspired by the studies of Howard [17], Perez et al. [24], and Shapiro et al. [25].
2.4. The Sociodemographic and Vaccination Data
2.5. Statistical Strategies
3. Results
3.1. The Sociodemographic Analysis of the Sample
3.2. Vaccination Data
3.3. The Factorial Structure
3.4. Gender Invariance
3.5. The Descriptive Analysis of the Data Obtained
3.6. The Convergent and Discriminant Validity
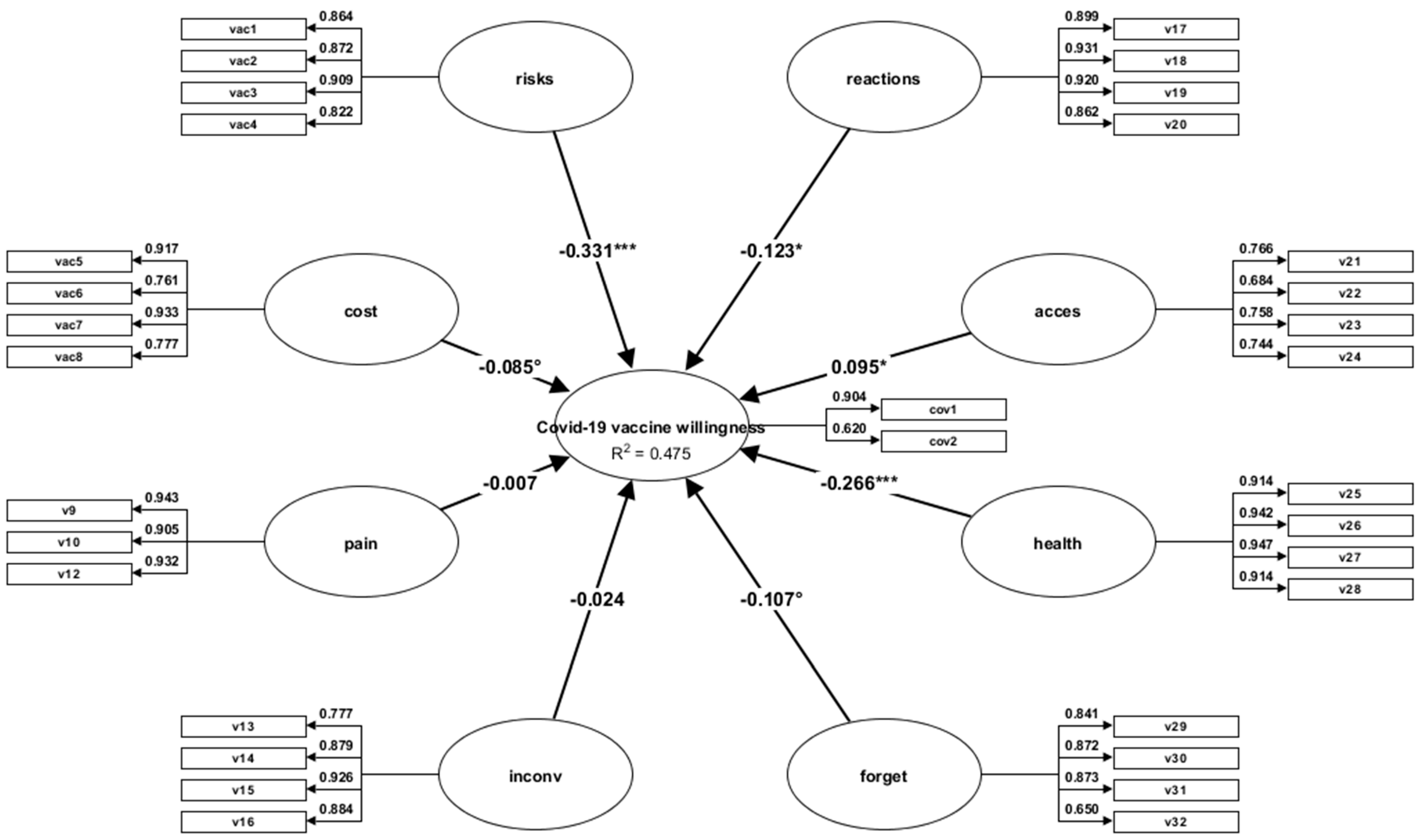
3.7. Predictive Validity
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacDonald, N.E.; SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Dudley, M.Z.; Privor-Dumm, L.; Dubé, È.; MacDonald, N.E. Words matter: Vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine 2020, 38, 709–711. [Google Scholar] [CrossRef] [PubMed]
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Medar, C.; et al. COVID-19 Parental Vaccine Hesitancy in Romania: Nationwide Cross-Sectional Study. Vaccines 2022, 10, 493. [Google Scholar] [CrossRef]
- Citu, I.M.; Citu, C.; Gorun, F.; Motoc, A.; Gorun, O.M.; Burlea, B.; Bratosin, F.; Tudorache, E.; Margan, M.-M.; Hosin, S.; et al. Determinants of COVID-19 Vaccination Hesitancy among Romanian Pregnant Women. Vaccines 2022, 10, 275. [Google Scholar] [CrossRef]
- Mărcău, F.C.; Purec, S.; Niculescu, G. Study on the Refusal of Vaccination against COVID-19 in Romania. Vaccines 2022, 10, 261. [Google Scholar] [CrossRef]
- Assante, G.M.; Candel, O.S. Do Vaccination Attitudes Mediate the Link between Critical Consciousness and COVID-19 Vaccination Behaviour? A Cross-Sectional Study. Sustainability 2022, 14, 7623. [Google Scholar] [CrossRef]
- Dascalu, S.; Geambasu, O.; Covaciu, O.; Chereches, R.M.; Diaconu, G.; Dumitra, G.G.; Gheorghita, V.; Popovici, E.D. Prospects of COVID-19 Vaccination in Romania: Challenges and Potential Solutions. Front. Public Health 2021, 9, 644538. [Google Scholar] [CrossRef]
- Dandolov, P. What’s Behind Vaccine Hesitancy in Bulgaria and Romania? Geopolitical Monitor. 2021. Available online: https://www.geopoliticalmonitor.com/whats-behind-vaccine-hesitancy-in-bulgaria-and-romania/ (accessed on 13 October 2022).
- Kluge, H.; McKee, M. COVID-19 vaccines for the European region: An unprecedented challenge. Lancet 2021, 397, 1689–1691. [Google Scholar] [CrossRef]
- CNN Analysis. 2022. Available online: https://www.digi24.ro/stiri/externe/cnn-cum-au-ajuns-romania-si-bulgaria-sa-aiba-cele-mai-mici-rate-de-vaccinare-din-ue-trecutul-comunist-este-una-din-cauze-1687669 (accessed on 13 October 2022).
- Gallup. Wellcome Global Monitor—First Wave Findings. 2019. Available online: https://wellcome.org/reports/wellcome-globalmonitor/2018 (accessed on 20 February 2022).
- Popa, A.D.; Enache, A.I.; Popa, I.V.; Antoniu, S.A.; Dragomir, R.A.; Burlacu, A. Determinants of the Hesitancy toward COVID-19 Vaccination in Eastern European Countries and the Relationship with Health and Vaccine Literacy: A Literature Review. Vaccines 2022, 10, 672. [Google Scholar] [CrossRef]
- Miko, D.; Costache, C.; Colosi, H.A.; Neculicioiu, V.; Colosi, I.A. Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina 2019, 55, 282. [Google Scholar] [CrossRef]
- Martin, L.R.; Petrie, K.J. Understanding the dimensions of anti-vaccination attitudes: The vaccination attitudes examination (VAX) scale. Ann. Behav. Med. 2017, 51, 652–660. [Google Scholar] [CrossRef]
- Mărcău, F.C. Survey on COVID-19 Vaccination of the Population in the Oltenia Region. Revista Universitară de Sociologie 2021, XVI, 306–318. Available online: http://www.sociologiecraiova.ro/revista/wp-content/uploads/2022/01/RUS-3_2021-306-318.pdf (accessed on 12 October 2022).
- Voidăzan, T.S.; Budianu, M.A.; Rozsnyai, F.F.; Kovacs, Z.; Uzun, C.C.; Neagu, N. Assessing the Level of Knowledge, Beliefs and Acceptance of HPV Vaccine: A Cross-Sectional Study in Romania. Int. J. Environ. Res. Public Health 2022, 19, 6939. [Google Scholar] [CrossRef]
- Howard, M.C. A more comprehensive measure of vaccine hesitancy: Creation of the Multidimensional Vaccine Hesitancy Scale (MVHS). J. Health Psychol. 2021, 27, 2402–2419. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef]
- Gilkey, M.B.; Reiter, P.L.; Magnus, B.E.; McRee, A.L.; Dempsey, A.F.; Brewer, N.T. Validation of the vaccination confidence scale: A brief measure to identify parents at risk for refusing adolescent vaccines. Acad. Pediatr. 2016, 16, 42–49. [Google Scholar] [CrossRef] [Green Version]
- Sarathchandra, D.; Navin, M.C.; Largent, M.A.; McCright, A.M. A survey instrument for measuring vaccine acceptance. Prev. Med. 2018, 109, 1–7. [Google Scholar] [CrossRef]
- Howard, M.C.; Davis, M.M. The mediating role of vaccine hesitancy in the relations of COVID-19 conspiracy beliefs and vaccination outcomes: Which dimensions matter? J. Health Psychol. 2022; Epub ahead of print. [Google Scholar] [CrossRef]
- Howard, M.C. The good, the bad, and the neutral: Vaccine hesitancy mediates the relations of Psychological Capital, the Dark Triad, and the Big Five with vaccination willingness and behaviors. Pers. Individ. Dif. 2022, 190, 111523. [Google Scholar] [CrossRef]
- World Health Organization. Process of Translation and Adaptation of Instruments. 2020. Available online: http://www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 29 August 2022).
- Perez, S.; Tatar, O.; Shapiro, G.K.; Dubé, E.; Ogilvie, G.; Guichon, J.; Gilca, V.; Rosberger, Z. Psychosocial determinants of parental human papillomavirus (HPV) vaccine decision-making for sons: Methodological challenges and initial results of a pan-Canadian longitudinal study. BMC Public Health 2016, 16, 1223. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, G.K.; Holding, A.; Perez, S.; Amsel, R.; Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016, 2, 167–172. [Google Scholar] [CrossRef]
- Schermelleh-Engel, K.; Moosbrugger, H.; Müller, H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol. Res. 2003, 8, 23–74. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon/Pearson Education: Boston, MA, USA, 2007. [Google Scholar]
- Wang, J.; Wang, X. Structural Equation Modeling, 2nd ed.; John Wiley & Son Ltd.: Hoboken, NJ, USA, 2020. [Google Scholar]
- Rutkowski, L.; Svetina, D. Measurement Invariance in International Surveys: Categorical Indicators and Fit Measure Performance. Appl. Meas. Educ. 2017, 30, 39–51. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Modeling Structural Equations, 4th ed.; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Chin, W.W. How to Write Up and Report PLS Analyses. In Handbook of Partial Least Squares; Vinzi, V.E., Chin, W.W., Henseler, J., Wang, H., Eds.; Springer: Berlin, Germany, 2010; pp. 655–690. [Google Scholar]
- Henseler, J. Composite-Based Structural Equation Modeling: Analyzing Latent and Emergent Variables; Guilford Press: New York, NY, USA, 2020. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2015, 43, 115–135. [Google Scholar] [CrossRef] [Green Version]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 3rd ed.; Sage: Thousand Oaks, CA, USA, 2022. [Google Scholar]
- Wagenmakers, E.J.; Farrell, S. AIC model selection using Akaike weights. Psychon Bull Rev. 2004, 11, 192–196. [Google Scholar] [CrossRef]
- Pituch, K.A.; Stevens, J.P. Applied Multivariate Statistics for the Social Sciences Analyses with SAS and IBM’s SPSS, 6th ed.; Routledge Taylor & Frances Group: London, UK, 2016. [Google Scholar]
- Fornell, C.; Larcker, D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981, 18, 382–388. [Google Scholar] [CrossRef]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef] [Green Version]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Mbombi, M.O.; Muthelo, L.; Mphekgwane, P.; Dhau, I.; Tlouyamma, J.; Nemuramba, R.; Mashaba, R.G.; Mothapo, K.; Maimela, E. Prevalence of COVID-19 Vaccine Hesitancy in a Rural Setting: A Case Study of DIMAMO Health and Demographic Surveillance Site, Limpopo Province of South Africa. J. Respir. 2022, 2, 101–110. [Google Scholar] [CrossRef]
- Cesaroni, G.; Calandrini, E.; Balducci, M.; Cappai, G.; Di Martino, M.; Sorge, C.; Nicastri, E.; Agabiti, N.; Davoli, M. Educational inequalities in COVID-19 vaccination: A cross-sectional study of the adult population in the Lazio Region, Italy. Vaccines 2022, 10, 364. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Block, S.; Sood, S. What determines Vaccine Hesitancy: Recommendations from childhood Vaccine Hesitancy to address COVID-19 Vaccine Hesitancy. Vaccines 2022, 10, 80. [Google Scholar] [CrossRef] [PubMed]

| Variables | n = 528 | |
|---|---|---|
| Age | 18–76 years | Mean age: 30.57 years; |
| Gender | Males Females | 40.70% 59.30% |
| Residence | Urban Rural | 83.70% 16.30% |
| Education | Secondary studies University studies Post-university studies | 13.40% 61.60% 25.00% |
| Work sector | Public Private Freelance Unemployed | 42.00% 46.27% 9.46% 2.27% |
| Geographic region | Capital South-East South-West North-West | 55.30% 29.20% 12.30% 3.20% |
| Models | χ2 | df | χ2/df | CFI | IFI | RMSEA (90%CI) | SRMR | AIC |
|---|---|---|---|---|---|---|---|---|
| M1 | 1256.309 | 436 | 2.88 | 0.93 | 0.93 | 0.060 [0.056–0.064] | 0.061 | 1504.309 |
| M2 | 1122.739 | 406 | 2.76 | 0.94 | 0.94 | 0.058 [0.054–0.062] | 0.053 | 1364.739 |
| M3 | 994.810 | 400 | 2.48 | 0.95 | 0.95 | 0.053 [0.049–0.057] | 0.051 | 1248.810 |
| Items | Factor Loading | M | S.D. |
|---|---|---|---|
| 1. Vaccines can cause long-term health issues. | 0.81 | 2.84 | 1.85 |
| 2. Vaccines are unsafe. | 0.86 | 2.53 | 1.66 |
| 3. Vaccines can cause illness. | 0.86 | 2.65 | 1.71 |
| 4. Vaccines can cause certain disorders. | 0.73 | 3.45 | 1.85 |
| 5. Vaccines cost too much. | 0.88 | 2.33 | 1.64 |
| 6. I am unable to get vaccines because they cost too much. | 0.68 | 1.66 | 1.26 |
| 7.Vaccines are too expensive. | 0.94 | 2.17 | 1.60 |
| 8. Without health insurance, vaccines cost too much. | 0.68 | 2.66 | 1.85 |
| 9. Needles bother me when receiving a vaccine. | 0.95 | 2.23 | 1.89 |
| 10. I worry about needles when getting a vaccine. | 0.80 | 2.20 | 1.85 |
| 11. Getting a vaccine hurts. | 0.30 | 4.24 | 1.69 |
| 12. I have a phobia of needles when receiving a vaccine. | 0.92 | 2.18 | 1.90 |
| 13. I am too busy to get a vaccine. | 0.66 | 1.63 | 1.16 |
| 14. Getting a vaccine is too much of a hassle. | 0.87 | 1.77 | 1.33 |
| 15. Getting a vaccine is too much trouble. | 0.88 | 1.76 | 1.35 |
| 16. I do not have the time to get a vaccine. | 0.77 | 1.53 | 1.09 |
| 17. I have allergic reactions to most vaccines. | 0.85 | 1.78 | 1.37 |
| 18. I am a high-risk person for having a negative reaction to vaccines. | 0.92 | 1.69 | 1.42 |
| 19. I am allergic to certain ingredients in vaccines. | 0.89 | 1.77 | 1.46 |
| 20. I have a medical condition that prevents me from getting vaccines. | 0.80 | 1.63 | 1.38 |
| 21. Vaccines are unavailable where I live. | 0.58 | 1.30 | 0.98 |
| 22. There is nowhere to get a vaccine. | 0.62 | 1.25 | 0.81 |
| 23. It is difficult to get a vaccine where I live. | 0.71 | 1.26 | 0.82 |
| 24. It is difficult to know where to get a vaccine. | 0.64 | 1.50 | 1.11 |
| 25. I do not need vaccines because I rarely get sick. | 0.87 | 2.20 | 1.70 |
| 26. My strong immune system eliminates any need for vaccines. | 0.91 | 2.10 | 1.65 |
| 27. I do not need vaccines because I am a low-risk person. | 0.93 | 2.01 | 1.54 |
| 28. People in my physical condition do not need vaccines | 0.87 | 1.77 | 1.43 |
| 29. Getting vaccines often slips my memory. | 0.81 | 1.90 | 1.45 |
| 30. I just forget about getting vaccines. | 0.85 | 1.73 | 1.47 |
| 31. I just never get around to getting vaccines. | 0.80 | 2.02 | 1.66 |
| 32. I accidentally skip getting vaccines. | 0.51 | 1.49 | 1.10 |
| Model Invariance | Overall Fit Indices | Comparative Fit Indices | |||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | χ2/df | CFI | RMSEA | Δχ2 | Δdf | ΔCFI | ΔRMSEA | |
| Configural | 1699.449 | 800 | 2.12 | 0.928 | 0.046 | – | – | – | – |
| Metric | 1787.958 | 823 | 2.17 | 0.922 | 0.047 | 88.509 | 23 | 0.006 | −0.001 |
| Scalar | 1843.737 | 854 | 2.15 | 0.920 | 0.047 | 144.288 | 54 | 0.002 | 0.000 |
| Strict | 1941.946 | 890 | 2.18 | 0.915 | 0.047 | 242.497 | 90 | 0.005 | 0.000 |
| Variables | M | S.D. | Min-Max | Skewness | Kurtosis | α | ω |
|---|---|---|---|---|---|---|---|
| Risks | 11.50 | 6.14 | 4–28 | 0.77 | −0.14 | 0.88 | 0.89 |
| Costs | 8.84 | 5.43 | 4–28 | 1.21 | 0.86 | 0.86 | 0.87 |
| Pain | 6.63 | 5.23 | 3–21 | 1.42 | 0.85 | 0.91 | 0.92 |
| Inconvenience | 6.70 | 4.30 | 4–26 | 1.94 | 3.55 | 0.89 | 0.89 |
| Reactions | 6.88 | 5.10 | 4–28 | 2.16 | 4.20 | 0.95 | 0.92 |
| Access | 5.32 | 2.77 | 4–22 | 2.80 | 8.77 | 0.71 | 0.72 |
| Healthy | 8.09 | 5.88 | 4–28 | 1.72 | 2.34 | 0.94 | 0.94 |
| Forget | 7.15 | 4.68 | 4–25 | 1.76 | 2.63 | 0.83 | 0.85 |
| Vaccine hesitancy | 65.39 | 27.50 | 31–155 | 1.10 | 0.55 | 0.93 | 0.93 |
| Age Group (Years) | |||
|---|---|---|---|
| Vaccine Hesitancy (%) | 18–29 | 30–49 | >50 |
| low | 11.90 | 11.50 | 61.30 |
| moderate | 74.40 | 69.50 | 61.30 |
| high | 13.80 | 19.11 | 22.70 |
| Factors | CR | AVE | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| Risks | 0.88 | 0.66 | 0.81 * | |||||||
| Costs | 0.87 | 0.64 | 0.35 | 0.80 * | ||||||
| Pain | 0.92 | 0.79 | 0.24 | 0.20 | 0.88 * | |||||
| Inconvenience | 0.87 | 0.64 | 0.44 | 0.39 | 0.34 | 0.80 * | ||||
| Reactions | 0.92 | 0.75 | 0.52 | 0.26 | 0.24 | 0.57 | 0.86 * | |||
| Access | 0.73 | 0.41 | 0.25 | 0.32 | 0.17 | 0.48 | 0.36 | 0.64 * | ||
| Healthy | 0.94 | 0.80 | 0.54 | 0.27 | 0.23 | 0.57 | 0.51 | 0.33 | 0.89 * | |
| Forget | 0.83 | 0.57 | 0.35 | 0.29 | 0.25 | 0.62 | 0.36 | 0.49 | 0.58 | 0.75 * |
| Constructs | β | SE | t-Value | p-Value |
|---|---|---|---|---|
| Risks→COVID-19 vaccine | −0.33 | 0.05 | −5.74 | 0.000 |
| Costs→COVID-19 vaccine | −0.08 | 0.04 | 1.81 | 0.069 |
| Pain→COVID-19 vaccine | −0.00 | 0.04 | −0.14 | 0.882 |
| Inconvenience→COVID-19 vaccine | −0.02 | 0.06 | −0.36 | 0.716 |
| Reactions→COVID-19 vaccine | −0.12 | 0.06 | −1.99 | 0.045 |
| Access→COVID-19 vaccine | 0.09 | 0.04 | 2.07 | 0.038 |
| Healthy→COVID-19 vaccine | −0.26 | 0.05 | −4.98 | 0.000 |
| Forget→COVID-19 vaccine | −0.10 | 0.05 | −1.94 | 0.053 |
| Constructs | β | SE | t-Value | p-Value |
|---|---|---|---|---|
| Risks→flu vaccine | −0.20 | 0.06 | −3.36 | 0.000 |
| Costs→flu vaccine | −0.04 | 0.05 | −0.77 | 0.435 |
| Pain→flu vaccine | −0.01 | 0.04 | −0.35 | 0.721 |
| Inconvenience→flu vaccine | −0.04 | 0.06 | −0.62 | 0.531 |
| Reactions→flu vaccine | −0.04 | 0.06 | −0.75 | 0.48 |
| Access→flu vaccine | 0.11 | 0.04 | 2.22 | 0.026 |
| Healthy→flu vaccine | −0.34 | 0.05 | −6.07 | 0.000 |
| Forget→flu vaccine | −0.05 | 0.05 | −0.88 | 0.377 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balgiu, B.A.; Sfeatcu, R.; Țâncu, A.M.C.; Imre, M.; Petre, A.; Tribus, L. The Multidimensional Vaccine Hesitancy Scale: A Validation Study. Vaccines 2022, 10, 1755. https://doi.org/10.3390/vaccines10101755
Balgiu BA, Sfeatcu R, Țâncu AMC, Imre M, Petre A, Tribus L. The Multidimensional Vaccine Hesitancy Scale: A Validation Study. Vaccines. 2022; 10(10):1755. https://doi.org/10.3390/vaccines10101755
Chicago/Turabian StyleBalgiu, Beatrice Adriana, Ruxandra Sfeatcu, Ana Maria Cristina Țâncu, Marina Imre, Ana Petre, and Laura Tribus. 2022. "The Multidimensional Vaccine Hesitancy Scale: A Validation Study" Vaccines 10, no. 10: 1755. https://doi.org/10.3390/vaccines10101755







