Generation of a Live-Attenuated Strain of Chikungunya Virus from an Indian Isolate for Vaccine Development
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture and Viruses
2.2. Immunofluorescence Staining
2.3. Animal Experiments
2.3.1. Ethics Statement
2.3.2. CHIKV Virus Infection in Mouse Models
2.3.3. Mice Immunization
2.3.4. Enzyme Linked Immunosorbent Assay
2.3.5. Plaque Reduction Neutralization Tests
2.3.6. Passive Protection Assays
2.4. Whole-Genome Sequencing
2.5. Statistics
3. Results
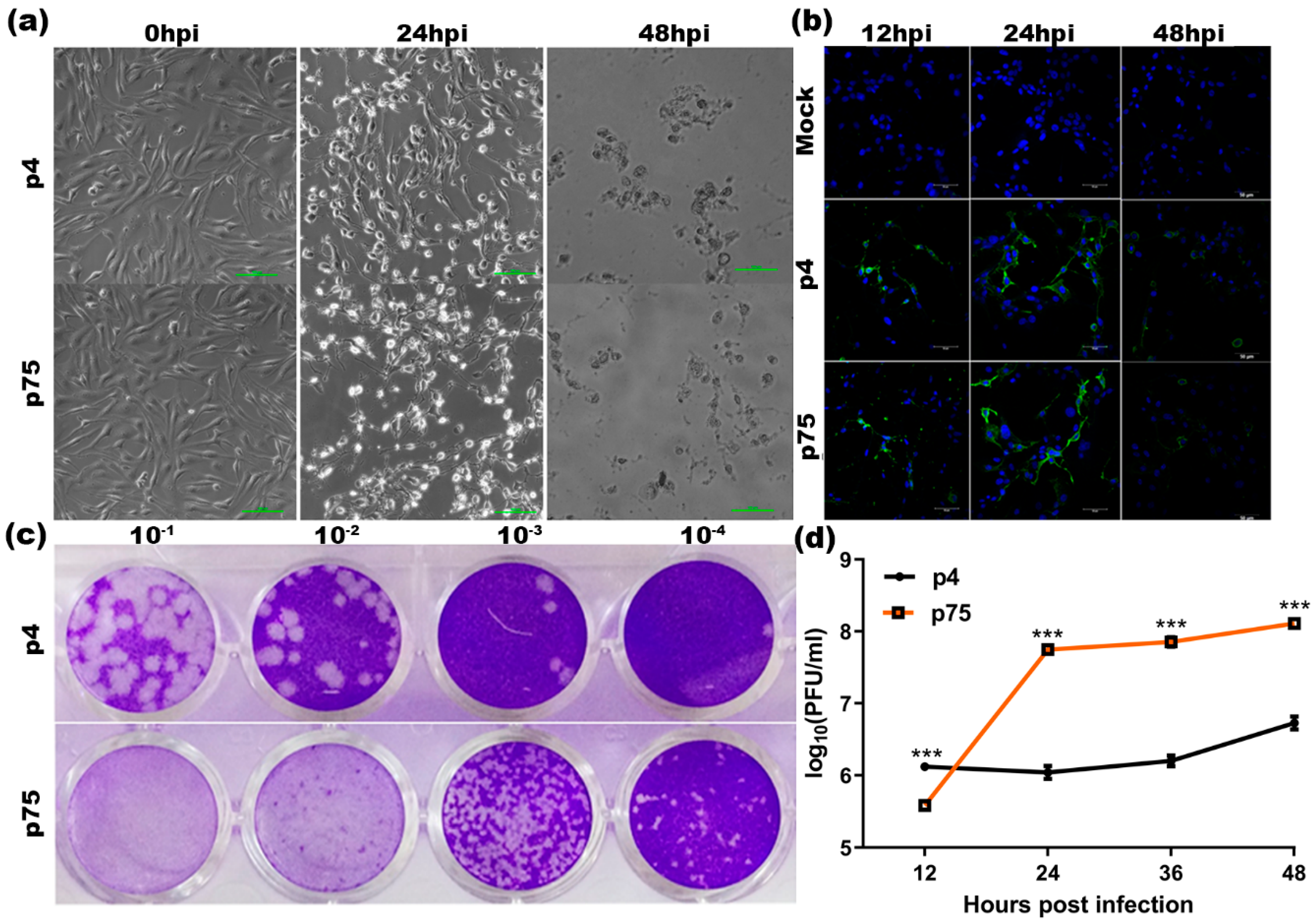
3.1. Infectivity Phenotype of the Wild-Type and Attenuated CHIKV Strains
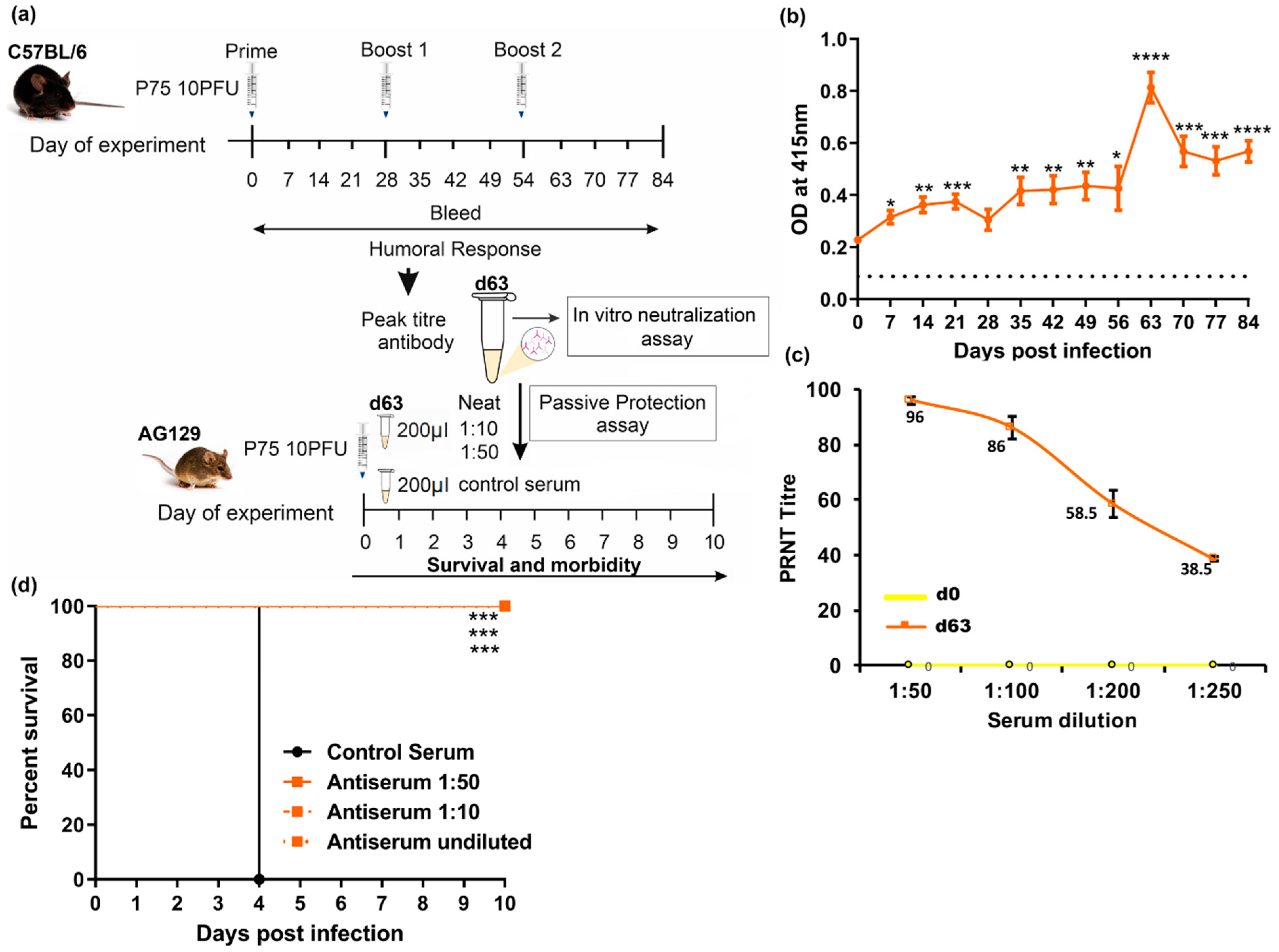
3.2. Evaluation of CHIKV p75 Attenuation in Mouse Models
3.3. Passive Protection in AG129 Mice
3.4. Comparative Whole-Genome Sequence Analysis of the Wild-Type and Attenuated CHIKV Strains to Identify Adaptive Mutations
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Solignat, M.; Gay, B.; Higgs, S.; Briant, L.; Devaux, C. Replication cycle of chikungunya: A re-emerging arbovirus. Virology 2009, 393, 183–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasque, P.; Couderc, T.; Lecuit, M.; Roques, P.; Ng, L.F. Chikungunya virus pathogenesis and immunity. Vector Borne Zoonotic Dis. 2015, 15, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Queyriaux, B.; Simon, F.; Grandadam, M.; Michel, R.; Tolou, H.; Boutin, J.P. Clinical burden of chikungunya virus infection. Lancet Infect. Dis. 2008, 1, 2–3. [Google Scholar] [CrossRef]
- Rao, T.R. Recent epidemics caused by Chikungunya virus in India. Sci. Cult. 1966, 32, 215. [Google Scholar]
- Carey, D.E.; Myers, R.M.; Deranitz, C.M.; Jadhav, M.; Reuben, R. The 1964 chikungunya epidemic at Vellore, South India, including observations on concurrent dengue. Trans. R. Soc. Trop. Med. Hyg. 1969, 63, 434–445. [Google Scholar] [CrossRef]
- Arankalle, V.A.; Shrivastava, S.; Cherian, S.; Gunjikar, R.S.; Walimbe, A.; Jadhav, S.M.; Sudeep, A.B.; Mishra, A.C. Genetic divergence of Chikungunya viruses in India (1963–2006) with special reference to the 2005–2006 explosive epidemic. J. Gen. Virol. 2007, 88, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Volk, S.M.; Chen, R.; Tsetsarkin, K.A.; Adams, A.P.; Garcia, T.I.; Sall, A.A.; Nasar, F.; Schuh, A.J.; Holmes, E.C.; Higgs, S.; et al. Genome-scale phylogenetic analyses of chikungunya virus reveal independent emergences of recent epidemics and various evolutionary rates. J. Virol. 2010, 84, 6497–6504. [Google Scholar] [CrossRef] [Green Version]
- Alvarez, M.; Mejía, B.A.; Morales, R.; Ramirez-Vallejo, E. Cardiovascular involvement and manifestations of systemic Chikungunya virus infection: A systematic review. F1000Research 2017, 6, 390. [Google Scholar] [CrossRef]
- Pinheiro, T.J.; Guimarães, L.F.; Silva, M.T.; Soares, C.N. Neurological manifestations of Chikungunya and Zika infections. Arq. Neuro-Psiquiatr. 2016, 74, 937–943. [Google Scholar] [CrossRef] [Green Version]
- Das, T.; Jaffar-Bandjee, M.C.; Hoarau, J.J.; Trotot, P.K.; Denizot, M.; Lee-Pat-Yuen, G.; Sahoo, R.; Guiraud, P.; Ramful, D.; Robin, S.; et al. Chikungunya fever: CNS infection and pathologies of a re-emerging arbovirus. Prog. Neurobiol. 2010, 91, 121–129. [Google Scholar] [CrossRef]
- Puntasecca, C.J.; King, C.H.; LaBeaud, A.D. Measuring the global burden of chikungunya and Zika viruses: A systematic review. PLoS Negl. Trop. Dis. 2021, 15, e0009055. [Google Scholar] [CrossRef]
- Harrison, V.R.; Eckels, K.H.; Bartelloni, P.J.; Hampton, C. Production and evaluation of a formalin-killed Chikungunya vaccine. J. Immunol. 1971, 107, 643–647. [Google Scholar] [PubMed]
- Levitt, N.H.; Ramsburg, H.H.; Hasty, S.; Repik, P.M.; Cole, F.E., Jr.; Lupton, H.W. Development of an attenuated strain of chikungunya virus for use in vaccine production. Vaccine 1986, 4, 157–162. [Google Scholar] [CrossRef]
- Edelman, R.; Tacket, C.O.; Wasserman, S.S.; Bodison, S.A.; Perry, J.G.; Mangiafico, J.A. Phase II safety and immunogenicity study of live chikungunya virus vaccine. Am. J. Trop. Med. Hyg. 2000, 62, 681–685. [Google Scholar] [CrossRef] [PubMed]
- Gorchakov, R.; Wang, E.; Leal, G.; Forrester, N.L.; Plante, K.; Rossi, S.L.; Partidos, C.D.; Adams, A.P.; Seymour, R.L.; Weger, J.; et al. Attenuation of Chikungunya Virus Vaccine Strain 181/Clone 25 Is Determined by Two Amino Acid Substitutions in the E2 Envelope Glycoprotein. J. Virol. 2012, 86, 6084–6096. [Google Scholar] [CrossRef] [Green Version]
- Akahata, W.; Yang, Z.Y.; Andersen, H.; Sun, S.; Holdaway, H.A.; Kong, W.P.; Lewis, M.G.; Higgs, S.; Rossmann, M.G.; Rao, S.; et al. A virus-like particle vaccine for epidemic Chikungunya virus protects nonhuman primates against infection. Nat. Med. 2010, 16, 334–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akahata, W.; Nabel, G.J. A specific domain of the Chikungunya virus E2 protein regulates particle formation in human cells: Implications for alphavirus vaccine design. J. Virol. 2012, 86, 8879–8883. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, L.J.; Dowd, K.A.; Mendoza, F.H.; Saunders, J.G.; Sitar, S.; Plummer, S.H.; Yamshchikov, G.; Sarwar, U.N.; Hu, Z.; Enama, M.E.; et al. Safety and tolerability of chikungunya virus-like particle vaccine in healthy adults: A phase 1 dose-escalation trial. Lancet 2014, 384, 2046–2052. [Google Scholar] [CrossRef]
- Chen, G.L.; Coates, E.E.; Plummer, S.H.; Carter, C.A.; Berkowitz, N.; Conan-Cibotti, M.; Cox, J.H.; Beck, A.; Callahan, M.O.; Andrews, C.; et al. Effect of a Chikungunya Virus-Like Particle Vaccine on Safety and Tolerability Outcomes: A Randomized Clinical Trial. JAMA 2020, 323, 1369–1377. [Google Scholar] [CrossRef]
- Bennett, S.R.; McCarty, J.M.; Ramanathan, R.; Mendy, J.; Richardson, J.S.; Smith, J.; Alexander, J.; Ledgerwood, J.E.; Lame, P.A.; Tredo, S.R.; et al. Safety and immunogenicity of PXVX0317, an aluminium hydroxide-adjuvanted chikungunya virus-like particle vaccine: A randomised, double-blind, parallel-group, phase 2 trial. Lancet Infect. Dis. 2022, 9, 1343–1355. [Google Scholar] [CrossRef]
- Hallengärd, D.; Kakoulidou, M.; Lulla, A.; Kümmerer, B.M.; Johansson, D.X.; Mutso, M.; Lulla, V.; Fazakerley, K.J.; Roques, P.; Le Grand, R.; et al. Novel attenuated Chikungunya vaccine candidates elicit protective immunity in C57BL/6 mice. J. Virol. 2014, 88, 2858–2866. [Google Scholar] [CrossRef] [PubMed]
- Hallengärd, D.; Lum, F.M.; Kümmerer, B.M.; Lulla, A.; Lulla, V.; García-Arriaza, J.; Fazakerley, J.K.; Roques, P.; Le Grand, R.; Merits, A.; et al. Prime-boost immunization strategies against Chikungunya virus. J. Virol. 2014, 88, 13333–13343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roques, P.; Ljungberg, K.; Kümmerer, B.M.; Gosse, L.; Dereuddre-Bosquet, N.; Tchitchek, N.; Hallengärd, D.; García-Arriaza, J.; Meinke, A.; Esteban, M.; et al. Attenuated and vectored vaccines protect nonhuman primates against Chikungunya virus. JCI Insight 2017, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Wressnigg, N.; Hochreiter, R.; Zoihsl, O.; Fritzer, A.; Bézay, N.; Klingler, A.; Lingnau, K.; Schneider, M.; Lundberg, U.; Meinke, A.; et al. Single-shot live-attenuated chikungunya vaccine in healthy adults: A phase 1, randomised controlled trial. Lancet Infect. Dis. 2020, 20, 1193–1203. [Google Scholar] [CrossRef]
- Kumar, M.; Sudeep, A.B.; Arankalle, V.A. Evaluation of recombinant E2 protein-based and whole-virus inactivated candidate vaccines against chikungunya virus. Vaccine 2012, 30, 6142–6149. [Google Scholar] [CrossRef]
- Brandler, S.; Ruffié, C.; Combredet, C.; Brault, J.B.; Najburg, V.; Prevost, M.C.; Habel, A.; Tauber, E.; Desprès, P.; Tangy, F. A recombinant measles vaccine expressing chikungunya virus-like particles is strongly immunogenic and protects mice from lethal challenge with chikungunya virus. Vaccine 2013, 31, 3718–3725. [Google Scholar] [CrossRef]
- Ramsauer, K.; Schwameis, M.; Firbas, C.; Müllner, M.; Putnak, R.J.; Thomas, S.J.; Desprès, P.; Tauber, E.; Jilma, B.; Tangy, F. Immunogenicity, safety, and tolerability of a recombinant measles-virus-based chikungunya vaccine: A randomised, double-blind, placebo-controlled, active-comparator, first-in-man trial. Lancet Infect. Dis. 2015, 15, 519–527. [Google Scholar] [CrossRef]
- Reisinger, E.C.; Tschismarov, R.; Beubler, E.; Wiedermann, U.; Firbas, C.; Loebermann, M.; Pfeiffer, A.; Muellner, M.; Tauber, E.; Ramsauer, K. Immunogenicity, safety, and tolerability of the measles-vectored chikungunya virus vaccine MV-CHIK: A double-blind, randomised, placebo-controlled and active-controlled phase 2 trial. Lancet 2018, 392, 2718–2727. [Google Scholar] [CrossRef]
- Rossi, S.L.; Comer, J.E.; Wang, E.; Azar, S.R.; Lawrence, W.S.; Plante, J.A.; Ramsauer, K.; Schrauf, S.; Weaver, S.C. Immunogenicity and Efficacy of a Measles Virus-Vectored Chikungunya Vaccine in Nonhuman Primates. J. Infect. Dis. 2019, 220, 735–742. [Google Scholar] [CrossRef]
- Tschismarov, R.; Zellweger, R.M.; Koh, M.J.; Leong, Y.S.; Low, J.; Ooi, E.; Mandl, C.; Ramsauer, K.; de Alwis, R. Antibody effector analysis of prime versus prime-boost immunizations with a recombinant measles-vectored chikungunya virus vaccine. JCI Insight 2021, 6, e151095. [Google Scholar] [CrossRef]
- Smalley, C.; Erasmus, J.H.; Chesson, C.B.; Beasley, D.W. Status of research and development of vaccines for chikungunya. Vaccine 2016, 34, 2976–2981. [Google Scholar] [CrossRef] [PubMed]
- Translational Research Consortia (TRC) for Chikungunya Virus in India. Current Status of Chikungunya in India. Front. Microbiol. 2021, 12, 695173. [Google Scholar] [CrossRef]
- Torres-Ruesta, A.; Ling Chee, R.S.; Ng, L.F. Insights into Antibody-Mediated Alphavirus Immunity and Vaccine Development Landscape. Microorganisms 2021, 9, 899. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Sandoval, A. 51 years in of Chikungunya clinical vaccine development: A historical perspective. Hum. Vaccines Immunother. 2019, 15, 2351–2358. [Google Scholar] [CrossRef] [PubMed]
- López-Camacho, C.; Kim, Y.C.; Blight, J.; Moreli, M.L.; Montoya-Diaz, E.; Huiskonen, J.T.; Kümmerer, B.M.; Reyes-Sandoval, A. Assessment of immunogenicity and neutralisation efficacy of viral-vectored vaccines against chikungunya virus. Viruses 2019, 11, 322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campos, R.K.; Preciado-Llanes, L.; Azar, S.R.; Lopez-Camacho, C.; Reyes-Sandoval, A.; Rossi, S.L. A single and un-adjuvanted dose of a chimpanzee adenovirus-vectored vaccine against chikungunya virus fully protects mice from lethal disease. Pathogens 2019, 8, 231. [Google Scholar] [CrossRef] [Green Version]
- Campos, R.K.; Preciado-Llanes, L.; Azar, S.R.; Kim, Y.C.; Brandon, O.; López-Camacho, C.; Reyes-Sandoval, A.; Rossi, S.L. Adenoviral-vectored Mayaro and Chikungunya virus vaccine candidates afford partial cross-protection from lethal challenge in A129 mouse model. Front. Immunol. 2020, 11, 591885. [Google Scholar] [CrossRef]
- Folegatti, P.M.; Harrison, K.; Preciado-Llanes, L.; Ramos Lope, F.; Bittaye, M.; Kim, Y.C.; Flaxman, A.; Bellamy, D.; Makinson, R.; Sheridan, J.; et al. A single dose of ChAdOx1 Chik vaccine induces neutralizing antibodies against four chikungunya virus lineages in a phase 1 clinical trial. Nat. Commun. 2021, 12, 4636. [Google Scholar] [CrossRef]
- Shaw, C.; Panther, L.; August, A.; Zaks, T.; Smolenov, I.; Bart, S.; Watson, M. Safety and immunogenicity of a mRNA-based chikungunya vaccine in a phase 1 dose-ranging trial. Int. J. Infect. Dis. 2019, 79, 17. [Google Scholar] [CrossRef] [Green Version]
- Kose, N.; Fox, J.M.; Sapparapu, G.; Bombardi, R.; Tennekoon, R.N.; De Silva, A.D.; Elbashir, S.M.; Theisen, M.A.; Humphris-Narayanan, E.; Ciaramella, G.; et al. A lipid-encapsulated mRNA encoding a potently neutralizing human monoclonal antibody protects against chikungunya infection. Sci. Immunol. 2019, 4, eaaw6647. [Google Scholar] [CrossRef]
- August, A.; Attarwala, H.Z.; Himansu, S.; Kalidindi, S.; Lu, S.; Pajon, R.; Han, S.; Lecerf, J.; Tomassini, J.; Hard, M.; et al. A phase 1 trial of lipid-encapsulated mRNA encoding a monoclonal antibody with neutralizing activity against Chikungunya virus. Nat. Med. 2021, 27, 2224–2233. [Google Scholar] [CrossRef] [PubMed]
- Plante, K.; Wang, E.; Partidos, C.D.; Weger, J.; Gorchakov, R.; Tsetsarkin, K.; Borland, E.M.; Powers, A.M.; Seymour, R.; Stinchcomb, D.T.; et al. Novel chikungunya attenuated strain with an IRES-based attenuation and host range alteration mechanism. PLoS Pathog. 2011, 7, e1002142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Partidos, C.D.; Paykel, J.; Weger, J.; Borland, E.M.; Powers, A.M.; Seymour, R.; Weaver, S.C.; Stinchcomb, D.T.; Osorio, J.E. Cross-protective immunity against o‘nyong-nyong virus afforded by a novel recombinant chikungunya vaccine. Vaccine 2012, 30, 4638–4643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, H.; Das, S.C.; Fuchs, J.F.; Suresh, M.; Weaver, S.C.; Stinchcomb, D.T.; Partidos, C.D.; Osorio, J.E. Deciphering the protective role of adaptive immunity to CHIKV/IRES a novel candidate vaccine against Chikungunya in the A129 mouse model. Vaccine 2013, 31, 3353–3360. [Google Scholar] [CrossRef] [Green Version]
- Roy, C.J.; Adams, A.P.; Wang, E.; Plante, K.; Gorchakov, R.; Seymour, R.L.; Vinet-Oliphant, H.; Weaver, S.C. Chikungunya vaccine candidate is highly attenuated and protects nonhuman primates against telemetrically monitored disease following a single dose. J. Infect. Dis. 2014, 209, 1891–1899. [Google Scholar] [CrossRef]
- Muthumani, K.; Lankaraman, K.M.; Laddy, D.J.; Sundaram, S.G.; Chung, C.W.; Sako, E.; Wu, L.; Khan, A.; Sardesai, N.; Kim, J.J.; et al. Immunogenicity of novel consensus-based DNA vaccines against Chikungunya virus. Vaccine 2008, 26, 5128–5134. [Google Scholar] [CrossRef] [Green Version]
- Mallilankaraman, K.; Shedlock, D.J.; Bao, H.; Kawalekar, O.U.; Fagone, P.; Ramanathan, A.A.; Ferraro, B.; Stabenow, J.; Vijayachari, P.; Sundaram, S.G.; et al. A DNA vaccine against chikungunya virus is protective in mice and induces neutralizing antibodies in mice and nonhuman primates. PLoS Negl. Trop. Dis. 2011, 5, e928. [Google Scholar] [CrossRef] [Green Version]
- Bao, H.; Ramanathan, A.; Kawalakar, O.; Sundaram, S.G.; Tingey, C.; Bian, C.B.; Muruganandam, N.; Vijayachari, P.; Sardesai, N.Y.; Weiner, D.B.; et al. Nonstructural protein 2 (nsP2) of Chikungunya virus (CHIKV) enhances protective immunity mediated by a CHIKV envelope protein expressing DNA Vaccine. Viral Immunol. 2013, 6, 75–83. [Google Scholar] [CrossRef]
- Erasmus, J.H.; Auguste, A.J.; Kaelber, J.T.; Luo, H.; Rossi, S.L.; Fenton, K.; Leal, G.; Kim, D.Y.; Chiu, W.; Wang, T.; et al. A chikungunya fever vaccine utilizing an insect-specific virus platform. Nat. Med. 2017, 23, 192–199. [Google Scholar] [CrossRef]
- Chan, Y.H.; Teo, T.H.; Utt, A.; Tan, J.J.; Amrun, S.N.; Bakar, F.A.; Yee, W.X.; Becht, E.; Pin Lee, C.Y.; Lee, B.; et al. Mutating chikungunya virus non-structural protein produces potent live-attenuated vaccine candidate. EMBO Mol. Med. 2019, 11, e10092. [Google Scholar] [CrossRef]
- Taylor, A.; Liu, X.; Zaid, A.; Goh, L.Y.H.; Hobson-Peters, J.; Hall, R.A.; Merits, A.; Mahalingam, S. Mutation of the n-terminal region of chikungunya virus capsid protein: Implications for vaccine design. MBio 2017, 8, e01970-16. [Google Scholar] [CrossRef] [PubMed]
- Carrau, L.; Rezelj, V.V.; Noval, M.G.; Levi, L.I.; Megrian, D.; Blanc, H.; Weger-Lucarelli, J.; Moratorio, G.; Stapleford, K.A.; Vignuzzi, M. Chikungunya virus vaccine candidates with decreased mutational robustness are attenuated in vivo and have compromised transmissibility. J. Virol. 2019, 93, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piper, A.; Ribeiro, M.; Smith, K.M.; Briggs, C.M.; Huitt, E.; Nanda, K.; Spears, C.J.; Quiles, M.; Cullen, J.; Thomas, M.E.; et al. Chikungunya virus host range E2 transmembrane deletion mutants induce protective immunity against challenge in C57BL/6J mice. J. Virol. 2013, 87, 6748–6757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gardner, C.L.; Hritz, J.; Sun, J.H.; Vanlandingham, D.L.; Song, T.Y.; Ghedin, E.; Higgs, S.; Klimstra, W.B.; Ryman, K.D. Deliberate attenuation of chikungunya virus by adaptation to heparan sulfate-dependent infectivity: A model for rational arboviral vaccine design. PLoS Negl. Trop. Dis. 2014, 8, e2719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiwari, M.; Parida, M.; Santhosh, S.R.; Khan, M.; Dash, P.K.; Rao, P.L. Assessment of immunogenic potential of Vero adapted formalin inactivated vaccine derived from novel ECSA genotype of Chikungunya virus. Vaccine 2009, 27, 2513–2522. [Google Scholar] [CrossRef]
- Metz, S.W.; Gardner, J.; Geertsema, C.; Le, T.T.; Goh, L.; Vlak, J.M.; Suhrbier, A.; Pijlman, G.P. Effective chikungunya virus-like particle vaccine produced in insect cells. PLoS Negl. Trop. Dis. 2013, 7, e2124. [Google Scholar] [CrossRef]
- Metz, S.W.; Martina, B.E.; Van den Doel, P.; Geertsema, C.; Osterhaus, A.D.; Vlak, J.M.; Pijlman, G.P. Chikungunya virus-like particles are more immunogenic in a lethal AG129 mouse model compared to glycoprotein E1 or E2 subunits. Vaccine 2013, 31, 6092–6096. [Google Scholar] [CrossRef]
- Wagner, J.M.; Pajerowski, J.; Daniels, C.L.; McHugh, P.M.; Flynn, J.A.; Balliet, J.W.; Casimiro, D.R.; Subramanian, S. Enhanced production of Chikungunya virus-like particles using a high-pH adapted spodopterafrugiperda insect cell line. PLoS ONE 2014, 9, e94401. [Google Scholar] [CrossRef] [Green Version]
- Saraswat, S.; Athmaram, T.N.; Parida, M.; Agarwal, A.; Saha, A.; Dash, P.K. Expression and characterization of yeast derived chikungunya virus like particles (CHIK-VLPs) and its evaluation as a potential vaccine candidate. PLoS Negl. Trop. Dis. 2016, 10, e0004782. [Google Scholar] [CrossRef] [Green Version]
- Abeyratne, E.; Tharmarajah, K.; Freitas, J.R.; Mostafavi, H.; Mahalingam, S.; Zaid, A.; Zaman, M.; Taylor, A. Liposomal delivery of the RNA genome of a live-attenuated chikungunya virus vaccine candidate provides local, but not systemic protection after one dose. Front. Immunol. 2020, 11, 304. [Google Scholar] [CrossRef]
- Tretyakova, I.; Hearn, J.; Wang, E.; Weaver, S.; Pushko, P. DNA vaccine initiates replication of live attenuated chikungunya virus in vitro and elicits protective immune response in mice. J. Infect. Dis. 2014, 209, 1882–1890. [Google Scholar] [CrossRef] [PubMed]
- Szurgot, I.; Ljungberg, J.; Kümmerer, B.M.; Liljeström, P. Infectious RNA vaccine protects mice against chikungunya virus infection. Sci. Rep. 2020, 10, 21076. [Google Scholar] [CrossRef] [PubMed]
- Metz, S.W.; Geertsema, C.; Martina, B.E.; Andrade, P.; Heldens, J.G.; Oers, M.M.; Goldbach, R.W.; Vlak, J.M.; Pijlman, G.P. Functional processing and secretion of Chikungunya virus E1 and E2 glycoproteins in insect cells. Virology 2011, 8, 353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.; Dhanwani, R.; Rao, P.V.; Parida, M. Subunit vaccine formulations based on recombinant envelope proteins of Chikungunya virus elicit balanced Th1/Th2 response and virus-neutralizing antibodies in mice. Virus Res. 2012, 167, 236–246. [Google Scholar] [CrossRef]
- Wang, E.; Volkova, E.; Adams, A.P.; Forrester, N.; Xiao, S.Y.; Frolov, I.; Weaver, S.C. Chimeric alphavirus attenuated strains for chikungunya. Vaccine 2007, 26, 5030–5039. [Google Scholar] [CrossRef] [Green Version]
- Wang, E.; Kim, D.Y.; Weaver, S.C.; Ilya Frolov, I. Chimeric Chikungunya viruses are nonpathogenic in highly sensitive mouse models but efficiently induce a protective immune response. J. Virol. 2011, 85, 9249–9252. [Google Scholar] [CrossRef] [Green Version]
- Chattopadhyay, A.; Wang, E.; Seymour, R.; Weaver, S.C.; Rose, J.K. A chimeric vesiculo/alphavirus is an effective alphavirus vaccine. J. Virol. 2013, 87, 395–402. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Suhrbier, A.; Penn-Nicholson, A.; Woraratanadharm, J.; Gardner, J.; Luo, M.; Le, T.T.; Anraku, I.; Sakalian, M.; Einfeld, D.; et al. A complex adenovirus vaccine against chikungunya virus provides complete protection against viraemia and arthritis. Vaccine 2011, 29, 2803–2809. [Google Scholar] [CrossRef] [Green Version]
- Weger-Lucarelli, J.; Chu, H.; Aliota, M.T.; Partidos, C.D.; Osorio, J.E. A novel MVA vectored Chikungunya virus vaccine elicits protective immunity in mice. PLoS Negl. Trop. Dis. 2014, 8, e2970. [Google Scholar] [CrossRef]
- García-Arriaza, J.; Cepeda, V.; Hallengärd, D.; Sorzano, C.Ó.; Kümmerer, B.M.; Liljeström, P.; Esteban, M. A novel poxvirus-based vaccine, MVA-CHIKV, is highly immunogenic and protects mice against chikungunya infection. J. Virol. 2014, 88, 3527–3547. [Google Scholar] [CrossRef] [Green Version]
- Van Den Doel, P.; Volz, A.; Roose, J.M.; Sewbalaksing, V.D.; Pijlman, G.; Middelkoop, I.V.; Duiverman, V.; Van de Wetering, E.; Sutter, G.; Osterhaus, A.; et al. Recombinant modified vaccinia virus Ankara expressing glycoprotein E2 of Chikungunya virus protects AG129 mice against lethal challenge. PLoS Negl. Trop. Dis. 2014, 8, e3101. [Google Scholar] [CrossRef] [PubMed]
- Kam, Y.W.; Lum, F.M.; Teo, T.H.; Lee, W.W.; Simarmata, D.; Harjanto, S.; Chua, C.L.; Chan, Y.F.; Wee, J.K.; Chow, A.; et al. Early neutralizing IgG response to Chikungunya virus in infected patients targets a dominant linear epitope on the E2 glycoprotein. EMBO Mol. Med. 2012, 4, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Voigt, E.A.; Fuerte-Stone, J.; Granger, B.; Archer, J.; Hoeven, N.V. Live-attenuated RNA hybrid vaccine technology provides single-dose protection against Chikungunya virus. Mol. Ther. 2021, 29, 2782–2793. [Google Scholar] [CrossRef] [PubMed]
- Slifka, D.K.; Raué, H.P.; Weber, W.C.; Andoh, T.F.; Kreklywich, C.N.; DeFilippis, V.R.; Streblow, D.N.; Slifka, M.K.; Amanna, I.J. Development of a next-generation chikungunya virus vaccine based on the HydroVax platform. PLoS Pathog. 2022, 18, e1010695. [Google Scholar] [CrossRef]
- Schmidt, C.; Haefner, E.; Gerbeth, J.; Beissert, T.; Sahin, U.; Perkovic, M.; Schnierle, B.S. A taRNA vaccine candidate induces a specific immune response that protects mice against Chikungunya virus infections. Mol. Ther. Nucleic Acids 2022, 28, 743–754. [Google Scholar] [CrossRef]
- Ge, N.; Sun, J.; Liu, Z.; Shu, J.; Yan, H.; Kou, Z.; Wei, Y.; Jin, X. An mRNA vaccine encoding Chikungunya virus E2-E1 protein elicits robust neutralizing antibody responses and CTL immune responses. Virol. Sin. 2022, 37, 266–276. [Google Scholar] [CrossRef]
- Powers, A.M.; Brault, A.C.; Tesh, R.B.; Weaver, S.C. Re-emergence of Chikungunya and O’nyong-nyong viruses: Evidence for distinct geographical lineages and distant evolutionary relationships. J. Gen. Virol. 2000, 81, 471–479. [Google Scholar] [CrossRef]
- Chen, R.; Puri, V.; Fedorova, N.; Lin, D.; Hari, K.L.; Jain, R.; Rodas, J.D.; Das, S.R.; Shabman, R.S.; Weaver, S.C. Comprehensive Genome Scale Phylogenetic Study Provides New Insights on the Global Expansion of Chikungunya Virus. J. Virol. 2016, 90, 10600–10611. [Google Scholar] [CrossRef] [Green Version]
- Xavier, J.; Giovanetti, M.; Fonseca, V.; Thézé, J.; Gräf, T.; Fabri, A.; Goes de Jesus, J.; Lima de Mendonça, M.C.; Damasceno dos Santos Rodrigues, C.; Mares-Guia, M.A.; et al. Circulation of chikungunya virus East/Central/South African lineage in Rio de Janeiro, Brazil. PLoS ONE 2019, 14, e0217871. [Google Scholar] [CrossRef] [Green Version]
- Sahadeo, N.; Mohammed, H.; Allicock, O.; Auguste, A.J.; Widen, S.G.; Badal, K.; Pulchan, K.; Foster, J.E.; Weaver, S.C.; Carrington, C. Molecular Characterisation of Chikungunya Virus Infections in Trinidad and Comparison of Clinical and Laboratory Features with Dengue and Other Acute Febrile Cases. PLoS ONE Negl. Trop. Dis. 2015, 9, e0004199. [Google Scholar]
- Kautz, T.F.; Díaz-González, E.E.; Erasmus, J.H.; Malo-García, I.R.; Langsjoen, R.M.; Patterson, E.I.; Auguste, D.I.; Forrester, N.L.; Sanchez-Casas, R.M.; Hernández-Ávila, M.; et al. Chikungunya Virus as Cause of Febrile Illness Outbreak, Chiapas, Mexico, 2014. Emerg. Infect. Dis. 2015, 21, 2070–2073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langsjoen, R.M.; Haller, S.L.; Roy, C.J.; Vinet-Oliphant, H.; Bergren, N.A.; Erasmus, J.H.; Livengoo, J.A.; Powell, T.D.; Weaver, S.C. Chikungunya Virus Strains Show Lineage-Specific Variations in Virulence and Cross-Protective Ability in Murine and Nonhuman Primate Models. MBio 2018, 9, e02449-17. [Google Scholar] [CrossRef] [PubMed]
- Auerswald, H.; Boussioux, C.; In, S.; Mao, S.; Ong, S.; Huy, R.; Leang, R.; Chan, M.; Duong, V.; Ly, S.; et al. Broad and long-lasting immune protection against various Chikungunya genotypes demonstrated by participants in a cross-sectional study in a Cambodian rural community. Emerg. Microbes Infect. 2018, 7, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Chua, C.L.; Sam, I.C.; Merits, A.; Chan, Y.F. Antigenic Variation of East/Central/South African and Asian Chikungunya Virus Genotypes in Neutralization by Immune Sera. PLoS Negl. Trop. Dis. 2016, 10, e0004960. [Google Scholar] [CrossRef] [Green Version]
- Abraham, R.; Mudaliar, P.; Padmanabhan, A.; Sreekumar, E. Induction of Cytopathogenicity in Human Glioblastoma Cells by Chikungunya Virus. PLoS ONE 2013, 8, e75854. [Google Scholar] [CrossRef]
- Sreekumar, E.; Issac, A.; Nair, S.; Hariharan, R.; Janki, M.B.; Arathy, D.S.; Regu, R.; Mathew, T.; Anoop, M.; Niyas, K.P.; et al. Genetic characterization of 2006–2008 isolates of Chikungunya virus from Kerala, South India, by whole genome sequence analysis. Virus Genes 2009, 40, 14–27. [Google Scholar] [CrossRef]
- Nair, S.R.; Abraham, R.; Sreekumar, E. Interferon-gamma and IL-1beta activation precede death in neonatal mice models of central nervous system (CNS) infection by Chikungunya virus. Int. J. Infect. Dis. 2016, 45, 449–450. [Google Scholar] [CrossRef] [Green Version]
- Nair, S.R.; Abraham, R.; Sundaram, S.; Sreekumar, E. Interferon regulated gene (IRG) expression-signature in a mouse model of chikungunya virus neurovirulence. J. Neurovirol. 2017, 23, 886–902. [Google Scholar] [CrossRef]
- Cook, L.E.; Locke, M.C.; Young, A.R.; Monte, K.; Hedberg, M.L.; Shimak, R.M.; Sheehan, K.C.; Veis, D.J.; Diamond, M.S.; Lenschow, D.J. Distinct Roles of Interferon Alpha and Beta in Controlling Chikungunya Virus Replication and Modulating Neutrophil-Mediated Inflammation. J. Virol. 2019, 94, e00841-19. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Vanlandingham, D.L.; McGee, C.E.; Higgs, S. A single mutation in chikungunya virus affects vector specificity and epidemic potential. PLoS Pathog. 2007, 3, e201. [Google Scholar] [CrossRef]
- Bettis, A.A.; L’Azou Jackson, M.; Yoon, I.K.; Breugelmans, J.G.; Goio, A.; Gubler, D.J.; Powers, A.M. The global epidemiology of chikungunya from 1999 to 2020: A systematic literature review to inform the development and introduction of vaccines. PLoS Negl. Trop. Dis. 2022, 16, e0010069. [Google Scholar] [CrossRef] [PubMed]
- Olopade, O.L.; Jenkins, R.B.; Ransom, D.T.; Malik, K.; Pomykala, H.; Nobori, T.; Cowan, J.M.; Rowley, J.D.; Diaz, M.O. Molecular Analysis of Deletions of the Short Arm of Chromosome 9 in Human Gliomas. Cancer Res. 1992, 52, 2523–2529. [Google Scholar] [PubMed]
- Sgorbissa, A.; Tomasella, A.; Potu, H.; Manini, I.; Brancolini, C. Type I IFNs signaling and apoptosis resistance in glioblastoma cells. Apoptosis 2011, 16, 1229–1244. [Google Scholar] [CrossRef] [PubMed]
- Wollmann, G.; Tattersall, P.; Van den Pol, A.N. Targeting human glioblastoma cells: Comparison of nine viruses with oncolytic potential. J. Virol. 2005, 79, 6005–6022. [Google Scholar] [CrossRef] [Green Version]
- Silva, L.A.; Khomandiak, S.; Ashbrook, A.W.; Weller, R.; Heise, M.T.; Morrison, T.E.; Dermody, T.S. A single-amino-acid polymorphism in Chikungunya virus E2 glycoprotein influences glycosaminoglycan utilization. J. Virol. 2013, 88, 2385–2397. [Google Scholar] [CrossRef] [Green Version]
- Ashbrook, A.W.; Burrack, K.S.; Silva, L.A.; Montgomery, S.A.; Heise, M.T.; Morrison, T.E.; Dermody, T.S. Residue 82 of the Chikungunya Virus E2 Attachment Protein Modulates Viral Dissemination and Arthritis in Mice. J. Virol. 2014, 88, 12180–12192. [Google Scholar] [CrossRef] [Green Version]
- Lentscher, A.J.; McAllister, N.; Griswold, K.A.; Martin, J.L.; Welsh, O.L.; Sutherland, D.M.; Silva, L.A.; Dermody, T.S. Chikungunya virus vaccine candidate incorporating synergistic mutations is attenuated and protects against virulent virus challenge. J. Infect.Dis. 2022. [Google Scholar] [CrossRef]
- Cunha, M.S.; Cruz, N.V.G.; Schnellrath, L.C.; Medaglia, M.L.G.; Casotto, M.E.; Albano, R.M.; Costa, L.J.; Damaso, C.R. Autochthonous Transmission of East/Central/South African Genotype Chikungunya Virus, Brazil. Emerg. Infect. Dis. 2017, 23, 1737–1739. [Google Scholar] [CrossRef] [Green Version]
- Abraham, R.; Mudaliar, P.; Joseph, I.; Sivakumar, K.C.; Nair, R.R.; Sreekumar, E. Correlation of phylogenetic clade diversification and in vitro infectivity differences among Cosmopolitan genotype strains of Chikungunya virus. Infect. Genet. Evol. 2016, 37, 174–184. [Google Scholar] [CrossRef]
- Moyen, N.; Thiberville, S.D.; Pastorino, B.; Nougairede, A.; Thirion, L.; Mombouli, J.V.; Dimi, Y.; Gofart, I.L.; Capobianchi, M.R.; Lepfoundzou, A.D.; et al. First reported chikungunya fever outbreak in the republic of Congo, 2011. PLoS ONE 2014, 12, e115938. [Google Scholar] [CrossRef] [Green Version]
- Lim, C.-K.; Nishibori, T.; Watanabe, K.; Ito, M.; Kotaki, A.; Tanaka, K.; Kurane, I.; Takasaki, T. Chikungunya virus isolated from a returnee to Japan from Sri Lanka: Isolation of two sub-strains with different characteristics. Am. J. Trop. Med. Hyg. 2009, 81, 865–868. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juthamas, P.; Imad, H.A.; Rahman, M.; Nakayama, E.E.; Kludkleeb, S.; Ponam, T.; Rahim, R.; Rasel, A.B.; Poltep, K.; Yamanaka, A.; et al. A novel sub-lineage of chikungunya virus East/Central/South African Genotype Indian ocean lineage caused sequential outbreaks in Bangladesh and Thailand. Viruses 2020, 2, 1319. [Google Scholar]
- Njenga, M.; Kariuki, L.; Ledermann, N.J.; Ndirangu, A.; Logue, C.H.; Kelly, C.H.L.; Sang, R.; Sergon, K.; Breiman, R.; Powers, A.M. Tracking epidemic chikungunya virus into the Indian Ocean from East Africa. J. Gen. Virol. 2008, 89, 2754–2760. [Google Scholar] [CrossRef]
- Valerie, M.J.; Noval, M.B.; Chen, R.; Weaver, S.C.; Vignuzzi, M.; Stapleford, K.A.; Turner, P.E. Chikungunya virus evolution following a large 3′ UTR deletion results in host-specific molecular changes in protein-coding regions. Virus Evol. 2018, 4, vey012. [Google Scholar]
- Kovacikova, K.; Bas, M.M.; Tas, A.; Albulescu, I.C.; Rijswijk, R.V.; Jarhad, D.B.; Shin, Y.S.; Jang, M.H.; Kim, G.; Lee, H.W.; et al. 6′-β-Fluoro-homoaristeromycin and 6′-fluoro-homoneplanocin A are potent inhibitors of chikungunya virus replication through their direct effect on viral nonstructural protein 1. Antimicrob. Agents Chemother. 2020, 64, e02532-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albulescu, I.C.; White-Scholten, L.; Tas, A.; Hoornweg, T.E.; Ferla, S.; Kovacikova, K.; Smit, J.M.; Brancale, A.; Snijder, E.J.; van Hemert, M.J. Suramin inhibits chikungunya virus replication by interacting with virions and blocking the early steps of infection. Viruses 2020, 12, 314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sangwoo, N.; Ga, Y.J.; Lee, J.Y.; Hwang, W.Y.; Jung, E.; Shin, J.S.; Chen, W.; Choi, G.; Zhou, B.; Yeh, J.Y.; et al. Radicicol Inhibits Chikungunya Virus Replication by Targeting Nonstructural Protein 2. Antimicrob. Agents Chemother. 2021, 65, e00135-21. [Google Scholar]
- De Caluwé, L.; Heyndrickx, L.; Coppens, S.; Vereecken, K.; Quiñones-Mateu, M.E.; Merits, A.; Ariën, K.K.; Bartholomeeusen, K. Chikungunya Virus’ High Genomic Plasticity Enables Rapid Adaptation to Restrictive A549 Cells. Viruses 2022, 14, 282. [Google Scholar] [CrossRef]
- Broeckel, R.; Fox, J.M.; Haese, N.; Kreklywich, C.N.; Sukulpovi-Petty, S.; Legasse, A.; Smith, P.P.; Denton, M.; Corvey, C.; Krishnan, S.; et al. Therapeutic administration of a recombinant human monoclonal antibody reduces the severity of chikungunya virus disease in rhesus macaques. PLoS Negl. Trop. Dis. 2017, 11, e0005637. [Google Scholar] [CrossRef] [Green Version]
- Pankaj, P.; Dowd, K.A.; Brien, J.D.; Edeling, M.A.; Gorlatov, S.; Johnson, S.; Lee, I.; Akahata, W.; Nabel, G.J.; Richter, M.K.S.; et al. Development of a highly protective combination monoclonal antibody therapy against Chikungunya virus. PLoS Pathog. 2013, 9, e1003312. [Google Scholar]
- Suganya, S.; Sexton, N.R.; Kahle, K.M.; Fong, R.H.; Mattia, K.M.; Gardner, J.; Kai, L.; Nathan, L.; Beatriz, S.; David, T.; et al. A neutralizing monoclonal antibody targeting the acid-sensitive region in chikungunya virus E2 protects from disease. PLoS Negl. Trop. Dis. 2013, 7, e2423. [Google Scholar]
- Jing, J.; Liss, N.M.; Chen, D.H.; Liao, M.; Fox, J.M.; Shimak, R.M.; Fong, R.H.; Chafets, D.; Bakkour, S.; Keating, S.; et al. Neutralizing monoclonal antibodies block chikungunya virus entry and release by targeting an epitope critical to viral pathogenesis. Cell Rep. 2015, 13, 2553–2564. [Google Scholar]
- Partidos, C.D.; Weger, J.; Brewoo, J.; Seymour, R.; Borland, E.M.; Ledermann, J.P.; Powers, A.M.; Weaver, S.C.; Stinchcomb, D.T.; Osorio, J.E. Probing the attenuation and protective efficacy of a candidate chikungunya virus vaccine in mice with compromised interferon (IFN) signaling. Vaccine 2011, 29, 3067–3073. [Google Scholar] [CrossRef] [PubMed]

| Sl. No. | Name of Candidate Vaccine | CHIKV Strain | Vaccine Type | Details of the Candidate | Reference |
|---|---|---|---|---|---|
| Clinical Phase 3 | |||||
| 1 | PXVX0317/VRC-CHKVLP059-00-VP | 37,997; West African | VLP | Structural polyprotein CE3E26KE1 was inserted into pseudotyped lentiviral vectors and transfected into HEK293 cell line forms of VLPs. | [16,17,18,19,20] |
| 2 | Δ5nsP3/VLA1553-301 | LR2006 OPY1; ECSA | Live-attenuated | Infectious viruses from cDNA clone with the deletion of 60 amino acids in the hypervariable region of the nsP3. | [21,22,23,24] |
| 3 | BBV87 | IND-06-AP3; ECSA | Inactivated virus | Whole-virus BPL/formalin inactivated vaccine formulated with 0.25 mg aluminum (as aluminum hydroxide). | [25] |
| Clinical Phase 2 | |||||
| 4 | TSI-GSD-218 (181/clone25) Completed | AF15561; Asian | Live-attenuated | Virus strain was attenuated by 11 passages in Vero cells and sequential 18 plaque-to-plaque passages in MRC-5 cells to develop 181/clone 25. | [13,14,15] |
| 5 | MV-CHIKV (V184) | ECSA | Virus vectored, VLP | Measles virus vaccine Schwarz 06-46 strain vector expressing VLPs comprising structural polyprotein. | [26,27,28,29,30] |
| Clinical Phase 1 | |||||
| 6 | Formalin inactivated (15561) | AF15561; Asian | Inactivated whole virus | Standard formalin inactivation protocol on virus strain. | [12] |
| 7 | ChAdOx1 Chik (CHIK001) | NA | Virus vectored | Replication-deficient simian adenoviral vector expressing the CHIKV structural proteins CE3E26KE1 forms VLPs. | [35,36,37,38] |
| 8 | mRNA-1388 (VAL-181388) | NA | mRNA | mRNA encoding CE3E26KE1 | [39] |
| 9 | mRNA-1944 | SL15649; ECSA | mRNA | Lipid nanoparticle-encapsulated mRNA encoding the heavy and light chains of a human CHIKV specific monoclonal-neutralizing antibody, CHKV-24. | [40,41] |
| Preclinical (Non-Human Primate) | |||||
| 10 | CHIKV-IRES | LR2006 OPY1; ECSA | Live-attenuated IRES | Manipulation of the structural protein expression CHIKV infectious cDNA clone by replacing its subgenomic promoter with IRES from encephalomyocarditis virus. | [42,43,44,45] |
| 11 | CHIKV pMCE321 | PC-08; ECSA | DNA | Consensus sequences were optimized for Env expression and inserted into pVax1 expression vector and designated as pMCE321. | [46,47,48] |
| 12 | EILV-CHIKV | 99659; Asian | Chimeric virus | An insect specific alphavirus EILV cDNA clone was designed to a chimeric virus containing the CHIKV structural proteins. | [49] |
| Preclinical (Mouse model) | |||||
| 13 | RH-CHIKV, RHEV-CHIKV | LR2006 OPY1; ECSA | Live-attenuated | CHIKVs with mutations in non-structural proteins –nsP1 R532H, nsP2 E515V and a double mutant, were investigated for their suitability as-attenuated CHIKV vaccines. | [50] |
| 14 | CHIKV-NoLS | LR2006 OPY1; ECSA | Live-attenuated | Mutation in the nucleolar localization sequence (NoLS) in CHIKV capsid protein was characterized for attenuation. | [51] |
| 15 | Stop CHIKV, Superstop CHIKV | LR2006 OPY1; ECSA | Live-attenuated | Live-attenuated CHIKV was designed by applying a rational genomic design based on multiple replacements of synonymous codons. | [52] |
| 16 | Chikv HR (TM17-2) | 37997; West African | Live-attenuated | Host range mutant generated by attenuating cDNA clone of CHIKV via truncating the transmembrane domain of E2. | [53] |
| 17 | Heparin sulfate cell culture adapted | LR2006 OPY1; ECSA | Live-attenuated | Virus stock was serially passaged 10 times in triplicate series on CHOK1, pgsA745 or C6/36 cells for deliberate attenuation through envelope glycoprotein mutation. | [54] |
| 18 | CHIKV DRDE-06 | DRDE-06; ECSA | Inactivated virus | Vero cell culture-derived, formalin-inactivated CHIKV vaccine candidate. | [55] |
| 19 | VLP -CHIKV-S27 | S27; ECSA | VLP | Structural polyprotein was inserted into a recombinant baculovirus vector and transfected in insect cell line (Spodoptera frugiperda cell lines -Sf21 to generate Ac-S27. | [56,57] |
| 20 | VLP–CHIKV-37997 | 37997; West African | VLP | Structural polyprotein was inserted into a recombinant baculovirus vector and is transfected in insect cell line Sf9 to generate AcMNPV-CHIKV37997. | [58] |
| 21 | Yeast expressed VLP | DRDE07; ECSA | VLP | Structural polyprotein was inserted into a yeast expression vector and integrated in GS115 strain of Pichia pastoris by electroporation. | [59] |
| 22 | Δ5nsP3 and Δ6K DNA | LR2006 OPY1; ECSA | DNA | cDNAs of the CHIKV, Δ5nsP3, or Δ6K strain were cloned under the control of the human CMV promoter in DNA-launched Semliki Forest virus replicon (DREP) plasmid which can produce infectious viruses. | [21] |
| 23 | CHIKV-NoLS RNA | LR2006 OPY1; ECSA | RNA | In vivo liposome RNA delivery system delivers the self-replicating RNA genome of CHIKV-NoLS directly into mice, allowing the recipient’s body to produce the live-attenuated vaccine particles—de novo production of live-attenuated vaccine in vivo. | [60] |
| 24 | p181/25-7 iDNA | TSI-GSD-218; Asian | DNA | iDNA vaccine comprising of plasmid DNA that encode the full-length infectious RNA genome of live-attenuated CHIKV clone 181/25. | [61] |
| 25 | iRNA Δ5nsP3; iDNA Δ5nsP3 | LR2006 OPY1; ECSA | RNA, DNA | In vitro transfection of iRNA carrying the deletion of 183 nucleotides in the nsP3 (Δ5nsP3) gene generated infectious viruses. iRNA is under SP6 while iDNA is under CMV promotor. | [21,62] |
| 26 | CHIKV-sE1 and –SE2 | S27; ECSA | Subunit vaccine | C-terminal his-tagged E1 and E2 envelope glycoproteins were produced at high levels in insect cells with baculovirus vectors using their native signal peptides located in CHIKV 6K and E3, respectively. | [56,57,63] |
| 27 | rE2p-CHIK | IND-06-AP3; ECSA | Subunit vaccine | E2 gene of CHIKV isolate was cloned in pET15b vector, expressed and purified (rE2p). | [25] |
| 28 | rCHIK-E1/E2 | DRDE-06; ECSA | Subunit vaccine | The E1 and E2 gene fragment were cloned into a pET28b + vector, expressed and purified. | [64] |
| 29 | VEE/CHIKV EEE/CHIKV SIN/CHIKV | LR2006 OPY1; ECSA | Chimeric virus | Chimeric viruses were constructed with VEEV (TC-83 strain) or EEEV (BeAr436087) or Sindbis virus (AR339) as the backbone and the structural protein genes of CHIKV and passaged on Vero cells. | [65] |
| 30 | VEE/CHIKV/IRES-C VEE/IRES-CHIKV VEE/IRES-C/CHIKV | LR2006 OPY1; ECSA | Chimeric virus | The above chimeric viruses were modified and made replication dependent on the function of the encephalomyocarditis virus (EMCV) internal ribosome entry site (IRES) and tested three different strategies of IRES-mediated CHIKV structural protein expression. | [65,66] |
| 31 | rVSVΔG- CHIKV | S27; ECSA | Chimeric virus | VSVΔG vector expressing CHIKV envelope proteins | [67] |
| 32 | CAdVax-CHIKV | LR2006 OPY1; ECSA | Chimeric virus | Inserting structural polyprotein into non-replicating complex Adenovirus vaccine (CAdVax) vectors. | [68] |
| 33 | MVA-CHIKV | LR2006 OPY1; ECSA | Chimeric virus | Based on the highly attenuated poxvirus vector modified vaccinia virus Ankara (MVA) expressing the CHIKV CE3E26KE1 structural gene. | [69,70] |
| 34 | MVA-6KE1 MVA-E3E2 MVA-6KE1E3E2 | S27; ECSA | Chimeric virus | Recombinant MVA vector expressing E3E2, 6KE1, or the entire CHIKV envelope polyprotein cassette E3E26KE1. | [71] |
| 35 | E2EP3 | NA | Epitope based | KLH-E2EP3 peptide with adjuvant when administered in mice protected against CHIKV. | [72] |
| 36 | CHIKV 181/25 CHIKV 181/25- Δ5nsP3 | TSI-GSD-218; Asian | Live-attenuated RNA hybrid | Full-length replication-competent attenuated CHIKV genomes are delivered to the site of vaccination using cutting-edge thermostable RNA vaccine delivery technology. | [73] |
| 37 | HydroVax-CHIKV | TSI-GSD-218; Asian | Inactivated virus | Site-directed hydrogen peroxide-based inactivation approach which maintains antigenic structures. | [74] |
| 38 | TR-S | LR2006 OPY1; ECSA | Trans-amplifying RNA | A trans-replicon (TR) RNA encoding the CHIKV envelope proteins can be amplified by the replicase (which are formed by a non-replicating mRNA encoding for the CHIKV nonstructural proteins) in trans. | [75] |
| 39 | E2-E1-LNP | Asian strain | mRNA | mRNA-lipid nanoparticle (mRNA-LNP) vaccine expressing CHIKV E2-E1 antigen. | [76] |
| Mutations Identified | |||||
|---|---|---|---|---|---|
| Protein | Amino Acid Positions | RGCB 355/KL08-p4 (Virulent) | RGCB 355/KL08-p75 (Attenuated) | AF15561 Asian Lineage Parent Strain of 181/25 (Virulent) | TSI-GSD-218 181/Clone25 (Attenuated) |
| nsP1 | 171 | R | Q | R | R |
| 301 | T | T | T | I | |
| nsP2 | 740 | V | A | V | V |
| nsP3 | 409 | N | T | N | N |
| Capsid | 15 | Q | L | Q | Q |
| E2 | 12 | T | T | T | I |
| 82 | G | R | G | R | |
| 196 | T | K | T | T | |
| 252 | Q | H | K | K | |
| E1 | 226 | V | A | A | A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nair, S.R.; Abraham, R.; Sreekumar, E. Generation of a Live-Attenuated Strain of Chikungunya Virus from an Indian Isolate for Vaccine Development. Vaccines 2022, 10, 1939. https://doi.org/10.3390/vaccines10111939
Nair SR, Abraham R, Sreekumar E. Generation of a Live-Attenuated Strain of Chikungunya Virus from an Indian Isolate for Vaccine Development. Vaccines. 2022; 10(11):1939. https://doi.org/10.3390/vaccines10111939
Chicago/Turabian StyleNair, Sreeja R., Rachy Abraham, and Easwaran Sreekumar. 2022. "Generation of a Live-Attenuated Strain of Chikungunya Virus from an Indian Isolate for Vaccine Development" Vaccines 10, no. 11: 1939. https://doi.org/10.3390/vaccines10111939
APA StyleNair, S. R., Abraham, R., & Sreekumar, E. (2022). Generation of a Live-Attenuated Strain of Chikungunya Virus from an Indian Isolate for Vaccine Development. Vaccines, 10(11), 1939. https://doi.org/10.3390/vaccines10111939





