Maternal COVID-19 Vaccine May Reduce the Risk of MIS-C in Infants: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
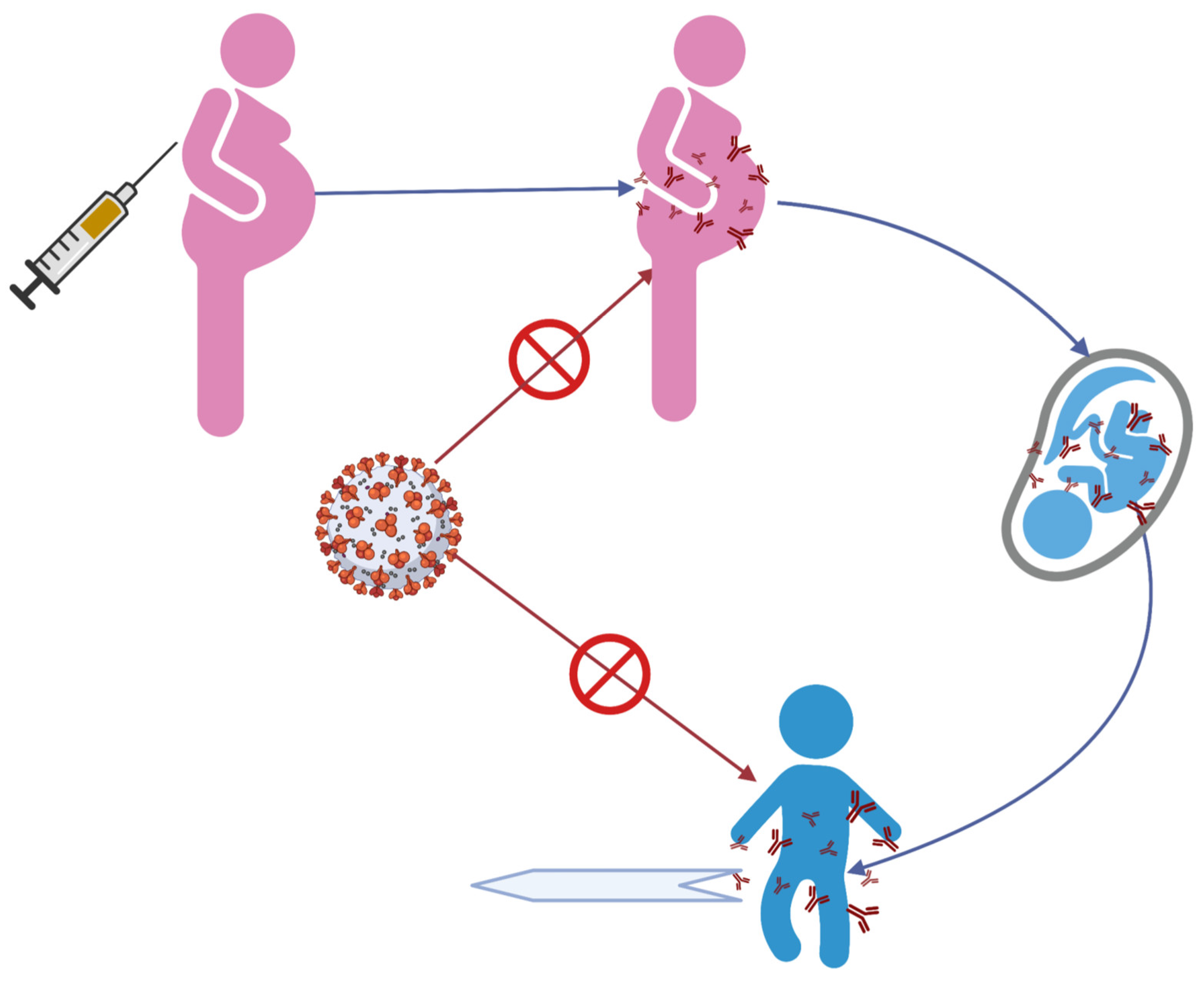
3.1. Studies Evaluating Transplacental Transfer of Antibodies to Newborns and Young Infants after Maternal COVID-19 Vaccination
| Author & Year | Study Type | Location | Type of Vaccine | Study Groups | Time of Vaccine in Pregnancy | Measure | Results |
|---|---|---|---|---|---|---|---|
| Beharier, 2021 [18] | Prospective cohort | Israel | BNT162b2 (2 doses) |
| 34.5 ± 7.5 weeks | Anti-S and RBD antibodies in maternal blood and in umbilical cord blood (Sera Ig G and IgM) |
|
| Collier, 2021 [25] | Prospective cohort | Israel | BNT162b2 or MRNA-1273 (2 doses) |
| 1st trimester (17%), 2nd trimester (50%), 3rd trimester (33%) | Immunogenicity of the mRNA vaccines in pregnant and lactating women: median RBD and anti-S IgG and IgA antibody titers |
|
| Kashani-Ligumsk, 2021 [19] | Prospective cohort | Israel | BNT162b2 (2 doses) |
| 3rd trimester | Titers of anti-S IgG antibodies to SARS-CoV-2 in umbilical cord blood in vaccinated pregnant women | Neonates born to vaccinated parturients had higher antibody titers and prolonged protection compared to those born to infected parturients. |
| Shook, 2022 [27] | Prospective cohort | United States | BNT162b2 or MRNA-1273 |
| 27 weeks | Persistence of anti-S IgG in infants after vaccine vs. natural infection. | Most infants had anti-S IgG persistently positive at 6 months of life. |
| Nir, 2021 [20] | Prospective cohort | Israel | BNT162b2 (2 doses) |
| 33.5 ± 3.2 weeks at second dosage | RBD IgG antibodies in maternal blood and in umbilical cord blood | Antibodies detected in cord blood, newborn dried blood spot, and breast milk samples were higher in vaccinated women than in COVID-19-recovered women. |
| Gray, 2021 [21] | Prospective cohort | United States | BNT162b2 or MRNA-1273 (2 doses) |
| 23.2 weeks(IQR 16.3–32.1) | Titers of severe acute respiratory syndrome coronavirus 2 spike and receptor-binding domain IgG, IgA, and IgM were quantified in participant sera and breastmilk |
|
| Trostle, 2021 [17] | Prospective case series | United States | BNT162b2 or MRNA-1273 (at least 1 dose) | 36 vaccinated pregnant women | 1st trimester (6%), 2nd trimester (83%), 3rd trimester (11%) | Positive Anti-S IgG antibodies and negative anti-N IgG antibodies in maternal blood and umbilical cord blood |
|
| Rottenstreich, 2021 [29] | Prospective case series | Israel | BNT162b2 (at least 1 dose) | 20 vaccinated pregnant women | 3rd trimester | Anti-S and RBD IgG antibodies in maternal blood and umbilical cord blood |
|
| Mithal, 2021 [30] | Prospective case series | United States | BNT162b2 or mRNA-1273 | 27 vaccinated pregnant women | 33 ± 2 weeks | Transfer of SARS-CoV-2 IgG antibodies to infants |
|
| Prabhu, 2021 [31] | Prospective case series | United States | BNT162b2 or MRNA-1273 (at least 1 dose) | 122 vaccinated pregnant women | NA | Anti-S IgG antibodies in maternal blood and umbilical cord blood |
|
| Yang, 2022 [22] | Retrospective cohort | United States | BNT162b2 mRNA-1273 or Johnson | 1359 vaccinated pregnant women | Both in pre-pregnant state and pregnancy | Transfer of maternal anti-S IgG in cord blood.Assess the association of prior infection and vaccine booster on anti-S IgG levels |
|
| Cassaniti, 2021 [24] | Retrospective cohort | Italy | BNT162b2 (2 doses) |
| 31+4 and 27+6 weeks | anti-SARS-CoV-2 spike IgG and IgA antibodies in pregnant women and newborns |
|
| Gloeckner, 2021 [26] | Retrospective cohort | Germany | BNT162b2 or MRNA-1273 after a prime vaccination with Oxford–AstraZeneca ChAdOx1 |
| NA | anti-spike IgG antibody kinetics in pregnant women in comparison to their newborns, as well as to a healthy nonpregnant control group |
|
| Zdanowski, 2021 [32] | Retrospective case series | Poland | BNT162b2 (2 doses) | 16 vaccinated pregnant women | 31.8 ± 2.1 weeks | Anti-S IgG antibodies in maternal blood and umbilical cord blood |
|
| Douxfils, 2021 [23] | Case report | Belgium | BNT162b2 (2 doses) | 1 vaccinated pregnant woman | 25 weeks | anti-S IgG antibodies in umbilical cord blood compared to maternal blood |
|
| Gill, 2021 [33] | Case report | United States | BNT162b2 (2 doses) | 1 vaccinated pregnant woman | 32+6 weeks | IgG SARS-CoV-2 antibodies in maternal blood and umbilical cord blood | Vaccination in pregnancy produced a robust immune response for the patient, with subsequent transplacental transfer of neutralizing antibodies. |
| Mangat, 2021 [28] | Case report | United States | BNT162b2 | 1 vaccinated pregnant woman | 22 and 26 weeks | Serial anti-S IgG antibody titers in infant | Antibodies in preterm infants were persistently positive at 6 months of age. |
| Mehaffey, 2021 [34] | Case report | United States | BNT162b2 (2 doses) | 1 vaccinated pregnant woman | 29 and 32 weeks | IgG SARS-CoV-2 antibodies in maternal and umbilical cord blood | Vertical transmission of IgG SARS-CoV-2-specific antibodies from a vaccinated mother to her son with no evidence of prior infection. |
| Paul, 2021 [35] | Case report | United States | MRNA-1273 (1 dose) | 1 vaccinated pregnant woman | 36+3 weeks | IgG SARS-CoV-2 in umbilical cord blood after maternal vaccination | SARS-CoV-2 IgG antibodies were detectable in a newborn’s cord blood sample after only a single dose of the vaccine. |
3.2. Studies Evaluating the Risk of COVID-19-Related Hospitalization and MIS-C Incidence in Vaccinated Children and Infants Born to Mothers Vaccinated during Pregnancy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bailey, L.C.; Razzaghi, H.; Burrows, E.K.; Bunnell, H.T.; Camacho, P.E.F.; Christakis, D.A.; Eckrich, D.; Kitzmiller, M.; Lin, S.M.; Magnusen, B.C.; et al. Assessment of 135 794 Pediatric Patients Tested for Severe Acute Respiratory Syndrome Coronavirus 2 Across the United States. JAMA Pediatr. 2021, 175, 176–184. [Google Scholar] [CrossRef] [PubMed]
- Wanga, V.; Gerdes, M.E.; Shi, D.S.; Choudhary, R.; Dulski, T.M.; Hsu, S.; Idubor, O.I.; Webber, B.J.; Wendel, A.M.; Agathis, N.T.; et al. Characteristics and Clinical Outcomes of Children and Adolescents Aged <18 Years Hospitalized with COVID-19—Six Hospitals, United States, July-August 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1766–1772. [Google Scholar] [CrossRef] [PubMed]
- Feldstein, L.R.; Tenforde, M.W.; Friedman, K.G.; Newhams, M.; Rose, E.B.; Dapul, H.; Soma, V.L.; Maddux, A.B.; Mourani, P.M.; Bowens, C.; et al. Characteristics and Outcomes of US Children and Adolescents With Multisystem Inflammatory Syndrome in Children (MIS-C) Compared With Severe Acute COVID-19. JAMA 2021, 325, 1074–1087. [Google Scholar] [CrossRef]
- Belay, E.D.; Abrams, J.; Oster, M.E.; Giovanni, J.; Pierce, T.; Meng, L.; Prezzato, E.; Balachandran, N.; Openshaw, J.J.; Rosen, H.E.; et al. Trends in Geographic and Temporal Distribution of US Children With Multisystem Inflammatory Syndrome During the COVID-19 Pandemic. JAMA Pediatr. 2021, 175, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Son, M.B.F.; Murray, N.; Friedman, K.; Young, C.C.; Newhams, M.M.; Feldstein, L.R.; Loftis, L.L.; Tarquinio, K.M.; Singh, A.R.; Heidemann, S.M.; et al. Multisystem Inflammatory Syndrome in Children—Initial Therapy and Outcomes. N. Engl. J. Med. 2021, 385, 23–34. [Google Scholar] [CrossRef]
- Alsaied, T.; Tremoulet, A.H.; Burns, J.C.; Saidi, A.; Dionne, A.; Lang, S.M.; Newburger, J.W.; de Ferranti, S.; Friedman, K.G. Review of Cardiac Involvement in Multisystem Inflammatory Syndrome in Children. Circulation 2021, 143, 78–88. [Google Scholar] [CrossRef]
- CDC, COVID Data Tracker. Centers for Disease Control and Prevention. Available online: https://covid.cdc.gov/covid-data-tracker/#mis-national-surveillance (accessed on 30 April 2022).
- De Rose, D.U.; Pugnaloni, F.; Calì, M.; Ronci, S.; Caoci, S.; Maddaloni, C.; Martini, L.; Santisi, A.; Dotta, A.; Auriti, C. Multisystem Inflammatory Syndrome in Neonates Born to Mothers with SARS-CoV-2 Infection (MIS-N) and in Neonates and Infants Younger Than 6 Months with Acquired COVID-19 (MIS-C): A Systematic Review. Viruses 2022, 14, 750. [Google Scholar] [CrossRef]
- Pawar, R.; Gavade, V.; Patil, N.; Mali, V.; Girwalkar, A.; Tarkasband, V.; Loya, S.; Chavan, A.; Nanivadekar, N.; Shinde, R.; et al. Neonatal Multisystem Inflammatory Syndrome (MIS-N) Associated with Prenatal Maternal SARS-CoV-2: A Case Series. Children 2021, 8, 572. [Google Scholar] [CrossRef]
- Federal Drug Administration. Coronavirus (COVID-19) Update: FDA Authorizes Moderna and Pfizer-BioNTech VCOVID-19 Vaccines for Children Down to 6 Months of Age. 2022. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-moderna-and-pfizer-biontech-covid-19-vaccines-children (accessed on 16 August 2022).
- Zambrano, L.D.; Newhams, M.M.; Olson, S.M.; Halasa, N.B.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Kamidani, S.; Tarquinio, K.M.; Maddux, A.B.; et al. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA Vaccination Against Multisystem Inflammatory Syndrome in Children Among Persons Aged 12-18 Years—United States, July-December 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 52–58. [Google Scholar] [CrossRef]
- Levy, M.; Recher, M.; Hubert, H.; Javouhey, E.; Fléchelles, O.; Leteurtre, S.; Angoulvant, F. Multisystem Inflammatory Syndrome in Children by COVID-19 Vaccination Status of Adolescents in France. JAMA 2022, 327, 281–283. [Google Scholar] [CrossRef]
- Ouldali, N.; Bagheri, H.; Salvo, F.; Antona, D.; Pariente, A.; Leblanc, C.; Tebacher, M.; Micallef, J.; Levy, C.; Cohen, R.; et al. Hyper inflammatory syndrome following COVID-19 mRNA vaccine in children: A national post-authorization pharmacovigilance study. Lancet Reg. Health Eur. 2022, 17, 100393. [Google Scholar] [CrossRef] [PubMed]
- Halasa, N.B.; Olson, S.M.; Staat, M.A.; Newhams, M.M.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Cameron, M.A.; Pannaraj, P.S.; Bline, K.E.; et al. Effectiveness of Maternal Vaccination with mRNA COVID-19 Vaccine During Pregnancy Against COVID-19-Associated Hospitalization in Infants Aged <6 Months—17 States, July 2021-January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Shimabukuro, T.T.; Kim, S.Y.; Myers, T.R.; Moro, P.L.; Oduyebo, T.; Panagiotakopoulos, L.; Marquez, P.L.; Olson, C.K.; Liu, R.; Chang, K.T.; et al. Preliminary Findings of mRNA COVID-19 Vaccine Safety in Pregnant Persons. N. Engl. J. Med. 2021, 384, 2273–2282. [Google Scholar] [CrossRef] [PubMed]
- Marchant, A.; Sadarangani, M.; Garand, M.; Dauby, N.; Verhasselt, V.; Pereira, L.; Bjornson, G.; Jones, C.E.; Halperin, S.A.; Edwards, K.M.; et al. Maternal immunisation: Collaborating with mother nature. Lancet Infect. Dis. 2017, 17, e197–e208. [Google Scholar] [CrossRef]
- Trostle, M.E.; Aguero-Rosenfeld, M.E.; Roman, A.S.; Lighter, J.L. High antibody levels in cord blood from pregnant women vaccinated against COVID-19. Am. J. Obstet. Gynecol. MFM 2021, 3, 100481. [Google Scholar] [CrossRef] [PubMed]
- Beharier, O.; Plitman Mayo, R.; Raz, T.; Nahum Sacks, K.; Schreiber, L.; Suissa-Cohen, Y.; Chen, R.; Gomez-Tolub, R.; Hadar, E.; Gabbay-Benziv, R. Efficient maternal to neonatal transfer of antibodies against SARS-CoV-2 and BNT162b2 mRNA COVID-19 vaccine. J. Clin. Invest. 2021, 131, e150319. [Google Scholar] [CrossRef] [PubMed]
- Kashani-Ligumsky, L.; Lopian, M.; Cohen, R.; Senderovich, H.; Czeiger, S.; Halperin, A.; Chaim, A.B.; Kremer, I.; Lessing, J.B.; Somekh, E.; et al. Titers of SARS-CoV-2 antibodies in cord blood of neonates whose mothers contracted SARS-CoV-2 (COVID-19) during pregnancy and in those whose mothers were vaccinated with mRNA to SARS-CoV-2 during pregnancy. J. Perinatol. 2021, 41, 2621–2624. [Google Scholar] [CrossRef]
- Nir, O.; Schwartz, A.; Toussia-Cohen, S.; Leibovitch, L.; Strauss, T.; Asraf, K.; Doolman, R.; Sharabi, S.; Cohen, C.; Lustig, Y.; et al. Maternal-neonatal transfer of SARS-CoV-2 immunoglobulin G antibodies among parturient women treated with BNT162b2 messenger RNA vaccine during pregnancy. Am. J. Obstet. Gynecol. MFM 2022, 4, 100492. [Google Scholar] [CrossRef]
- Gray, K.J.; Bordt, E.A.; Atyeo, C.; Deriso, E.; Akinwunmi, B.; Young, N.; Baez, A.M.; Shook, L.L.; Cvrk, D.; James, K.; et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: A cohort study. Am. J. Obstet. Gynecol. 2021, 225, e1–e303. [Google Scholar] [CrossRef]
- Yang, Y.J.; Murphy, E.A.; Singh, S.; Sukhu, A.C.; Wolfe, I.; Adurty, S.; Eng, D.; Yee, J.; Mohammed, I.; Zhao, Z.; et al. Association of Gestational Age at Coronavirus Disease 2019 (COVID-19) Vaccination, History of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection, and a Vaccine Booster Dose With Maternal and Umbilical Cord Antibody Levels at Delivery. Obstet. Gynecol. 2022, 139, 373–380. [Google Scholar] [CrossRef]
- Douxfils, J.; Gillot, C.; De Gottal, É.; Vandervinne, S.; Bayart, J.L.; Dogné, J.M.; Favresse, J. Efficient Maternal to Neonate Transfer of Neutralizing Antibodies after SARS-CoV-2 Vaccination with BNT162b2: A Case-Report and Discussion of the Literature. Vaccines 2021, 9, 907. [Google Scholar] [CrossRef] [PubMed]
- Cassaniti, I.; Percivalle, E.; Zelini, P.; Ngaradoumbe Nanhorngue, K.; Parolo, A.; Bernardi, V.; Jorizzo, G.; Santer, P.; Perotti, F.; Spinillo, A.; et al. Both SARS-CoV-2 infection and vaccination in pregnancy elicited neutralizing antibodies in pregnant women and newborns. Clin Microbiol Infect 2021, 27, 1708–1709. [Google Scholar] [CrossRef] [PubMed]
- Collier, A.Y.; McMahan, K.; Yu, J.; Tostanoski, L.H.; Aguayo, R.; Ansel, J.; Chandrashekar, A.; Patel, S.; Apraku Bondzie, E.; Sellers, D.; et al. Immunogenicity of COVID-19 mRNA Vaccines in Pregnant and Lactating Women. JAMA 2021, 325, 2370–2380. [Google Scholar] [CrossRef]
- Gloeckner, S.; Hornung, F.; Heimann, Y.; Schleussner, E.; Deinhardt-Emmer, S.; Loeffler, B.; Zoellkau, J. Newborns’ passive humoral SARS-CoV-2 immunity following heterologous vaccination of the mother during pregnancy. Am. J. Obstet. Gynecol. 2022, 226, 261–262. [Google Scholar] [CrossRef] [PubMed]
- Shook, L.L.; Atyeo, C.G.; Yonker, L.M.; Fasano, A.; Gray, K.J.; Alter, G.; Edlow, A.G. Durability of Anti-Spike Antibodies in Infants After Maternal COVID-19 Vaccination or Natural Infection. JAMA 2022, 327, 1087–1089. [Google Scholar] [CrossRef]
- Mangat, C.; Milosavljevic, N. BNT162b2 Vaccination during Pregnancy Protects Both the Mother and Infant: Anti-SARS-CoV-2 S Antibodies Persistently Positive in an Infant at 6 Months of Age. Case Rep. Pediatr. 2021, 2021, 6901131. [Google Scholar] [CrossRef] [PubMed]
- Rottenstreich, A.; Zarbiv, G.; Oiknine-Djian, E.; Zigron, R.; Wolf, D.G.; Porat, S. Efficient Maternofetal Transplacental Transfer of Anti- Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Antibodies After Antenatal SARS-CoV-2 BNT162b2 Messenger RNA Vaccination. Clin. Infect. Dis. 2021, 73, 1909–1912. [Google Scholar] [CrossRef]
- Mithal, L.B.; Otero, S.; Shanes, E.D.; Goldstein, J.A.; Miller, E.S. Cord blood antibodies following maternal coronavirus disease 2019 vaccination during pregnancy. Am. J. Obstet. Gynecol. 2021, 225, 192–194. [Google Scholar] [CrossRef]
- Prabhu, M.; Murphy, E.A.; Sukhu, A.C.; Yee, J.; Singh, S.; Eng, D.; Zhao, Z.; Riley, L.E.; Yang, Y.J. Antibody Response to Coronavirus Disease 2019 (COVID-19) Messenger RNA Vaccination in Pregnant Women and Transplacental Passage Into Cord Blood. Obstet. Gynecol. 2021, 138, 278–280. [Google Scholar] [CrossRef]
- Zdanowski, W.; Waśniewski, T. Evaluation of SARS-CoV-2 Spike Protein Antibody Titers in Cord Blood after COVID-19 Vaccination during Pregnancy in Polish Healthcare Workers: Preliminary Results. Vaccines 2021, 9, 675. [Google Scholar] [CrossRef]
- Gill, L.; Jones, C.W. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Antibodies in Neonatal Cord Blood After Vaccination in Pregnancy. Obstet. Gynecol. 2021, 137, 894–896. [Google Scholar] [CrossRef] [PubMed]
- Mehaffey, J.H.; Arnold, M.; Huffstetler, E.; Mehaffey, R.L.; Quillian, H.; Mehaffey, J.H. Successful vertical transmission of SARS-CoV-2 antibodies after maternal vaccination. Birth 2021, 48, 451–452. [Google Scholar] [CrossRef] [PubMed]
- Paul, G.; Chad, R. Newborn antibodies to SARS-CoV-2 detected in cord blood after maternal vaccination—A case report. BMC Pediatr. 2021, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Olson, S.M.; Newhams, M.M.; Halasa, N.B.; Price, A.M.; Boom, J.A.; Sahni, L.C.; Irby, K.; Walker, T.C.; Schwartz, S.P.; Pannaraj, P.S.; et al. Effectiveness of Pfizer-BioNTech mRNA Vaccination Against COVID-19 Hospitalization Among Persons Aged 12-18 Years—United States, June-September 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1483–1488. [Google Scholar] [CrossRef]
- Price, A.M.; Olson, S.M.; Newhams, M.M.; Halasa, N.B.; Boom, J.A.; Sahni, L.C.; Pannaraj, P.S.; Irby, K.; Bline, K.E.; Maddux, A.B.; et al. BNT162b2 Protection against the Omicron Variant in Children and Adolescents. N. Engl. J. Med. 2022, 386, 1899–1909. [Google Scholar] [CrossRef]
- Klein, N.P.; Stockwell, M.S.; Demarco, M.; Gaglani, M.; Kharbanda, A.B.; Irving, S.A.; Rao, S.; Grannis, S.J.; Dascomb, K.; Murthy, K.; et al. Effectiveness of COVID-19 Pfizer-BioNTech BNT162b2 mRNA Vaccination in Preventing COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Nonimmunocompromised Children and Adolescents Aged 5-17 Years—VISION Network, 10 States, April 2021-January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 352–358. [Google Scholar]
- Marks, K.J.; Whitaker, M.; Agathis, N.T.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Kirley, P.D.; Kawasaki, B.; Meek, J.; et al. Hospitalization of Infants and Children Aged 0-4 Years with Laboratory-Confirmed COVID-19—COVID-NET, 14 States, March 2020-February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 429–436. [Google Scholar] [CrossRef]
- Food and Drug Administration. FDA Approves First COVID-19 Vaccine. 2021. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccineexternal (accessed on 1 May 2022).
- Oliver, S.E.; Wallace, M.; Link-Gelles, R. COVID-19 Vaccines: Safe and Effective in Children Ages 5-11 Years. Pediatrics 2022, 150, e2022057314. [Google Scholar] [CrossRef]
- Fowlkes, A.L.; Yoon, S.K.; Lutrick, K.; Gwynn, L.; Burns, J.; Grant, L.; Phillips, A.L.; Ellingson, K.; Ferraris, M.V.; LeClair, L.B.; et al. Effectiveness of 2-Dose BNT162b2 (Pfizer BioNTech) mRNA Vaccine in Preventing SARS-CoV-2 Infection Among Children Aged 5-11 Years and Adolescents Aged 12-15 Years—PROTECT Cohort, July 2021-February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 422–428. [Google Scholar] [CrossRef]
- Shi, D.S.; Whitaker, M.; Marks, K.J.; Anglin, O.; Milucky, J.; Patel, K.; Pham, H.; Chai, S.J.; Kawasaki, B.; Meek, J.; et al. Hospitalizations of Children Aged 5-11 Years with Laboratory-Confirmed COVID-19—COVID-NET, 14 States, March 2020-February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 574–581. [Google Scholar] [CrossRef]
- CDC Case Definition for MIS-C. Available online: https://www.cdc.gov/mis/mis-c/hcp/index.html (accessed on 2 May 2022).
- Diggikar, S.; Nanjegowda, R.; Kumar, A.; Kumar, V.; Kulkarni, S.; Venkatagiri, P. Neonatal Multisystem Inflammatory Syndrome secondary to SARS-CoV-2 infection. J. Paediatr. Child Health 2021, 58, 900–902. [Google Scholar] [CrossRef] [PubMed]
- Bohn, M.K.; Yousef, P.; Steele, S.; Sepiashvili, L.; Adeli, K. MultiInflammatory Syndrome in Children: A View into Immune Pathogenesis from a Laboratory Perspective. J. Appl. Lab. Med. 2022, 7, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, A.; Brodsky, N.N.; Sumida, T.S.; Comi, M.; Asashima, H.; Hoehn, K.B.; Li, N.; Liu, Y.; Shah, A.; Ravindra, N.G.; et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity 2021, 54, 1083–1095. [Google Scholar] [CrossRef] [PubMed]
- Moreews, M.; Le Gouge, K.; Khaldi-Plassart, S.; Pescarmona, R.; Mathieu, A.L.; Malcus, C.; Djebali, S.; Bellomo, A.; Dauwalder, O.; Perret, M.; et al. Polyclonal expansion of TCR Vbeta 21.3(+) CD4(+) and CD8(+) T cells is a hallmark of Multisystem Inflammatory Syndrome in Children. Sci. Immunol. 2021, 6, eabh1516. [Google Scholar] [CrossRef]
| Author | Country | Type of Study | n: Study Group vs. Control Group (if Any) | Age | Intervention | Study Period | Measure | Results: |
|---|---|---|---|---|---|---|---|---|
| Olson, 2022 [36] | United States | Case-control | 179 cases (SARS-CoV-2 test positive) vs. 285 controls (SARS-CoV-2 test negative) | 12–18 years | 2 Doses of BNT162b2 | June– September 2021 |
|
|
| Klein, 2022 [38] | United States | Case-control | 9640 cases (SARS-CoV-2 test positive) vs. 31,276 controls (SARS-CoV-2 test negative) | 5–17 years | 2 Doses of BNT162b2 | April 2021–January 2022 |
|
|
| Price, 2022 [37] | United States | Case-control | 1185 cases (SARS-CoV-2 test positive) vs. 1627 controls (SARS-CoV-2 test negative) | 5–18 years | 2 Doses of BNT162b2 m RNA vaccine | July–February 2022 |
|
|
| Halasa, 2022 [14] | United States | Case-control | 176 cases (SARS-CoV-2 test positive) vs. 203 controls (SARS-CoV-2 test negative) | 0–6 months | Maternal 2-dose mRNA vaccination | July 2021–January 2022 |
|
|
| Zambrano, 2022 [11] | United States | Case-control | 102 cases (diagnosed with MIS-C) vs. 181 controls (no evidence of SARS-CoV-2 infection) | 12–18 years | 2 Doses of Pfizer-BioNTech vaccine in 12–18 year-olds | July 2021–January 2022 |
|
|
| Fowlkes, 2022 [42] | United States | Prospective cohort | 1364 participants | 5–15 years | 2 Doses of BNT162b2 | July 2021–February 2022 |
|
|
| Shi, 2022 [43] | United States | Population-based surveillance | 1475 (laboratory- confirmed COVID-19) | 5–11 years | 1–2 Doses of BNT162b2 | March 2020–February 2022 |
|
|
| Ouldali, 2022 [13] | France | Population-based surveillance | NA | 12–17 years | 2 Doses of mRNA vaccine | 15 June 2021 and 1 January 2022 |
|
|
| Marks, 2022 [39] | United States | Population-based Surveillance | 2818 (laboratory- confirmed COVID-19) | 12–17 years | 1–2 Doses of BNT162b2 | July 2021–January 2022 |
|
|
| Levy, 2021 [12] | France | Patient Registry | 107 (diagnosed with MIS-C) | 12–18 years | 1–2 Doses of mRNA vaccine | September 2021 and October 2021 |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangat, C.; Yarrarapu, S.N.S.; Singh, G.; Bansal, P. Maternal COVID-19 Vaccine May Reduce the Risk of MIS-C in Infants: A Narrative Review. Vaccines 2022, 10, 1454. https://doi.org/10.3390/vaccines10091454
Mangat C, Yarrarapu SNS, Singh G, Bansal P. Maternal COVID-19 Vaccine May Reduce the Risk of MIS-C in Infants: A Narrative Review. Vaccines. 2022; 10(9):1454. https://doi.org/10.3390/vaccines10091454
Chicago/Turabian StyleMangat, Chetna, Siva Naga Srinivas Yarrarapu, Gagandeep Singh, and Pankaj Bansal. 2022. "Maternal COVID-19 Vaccine May Reduce the Risk of MIS-C in Infants: A Narrative Review" Vaccines 10, no. 9: 1454. https://doi.org/10.3390/vaccines10091454





