Level of Knowledge Regarding Mpox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study
Abstract
1. Introduction
2. Methodology
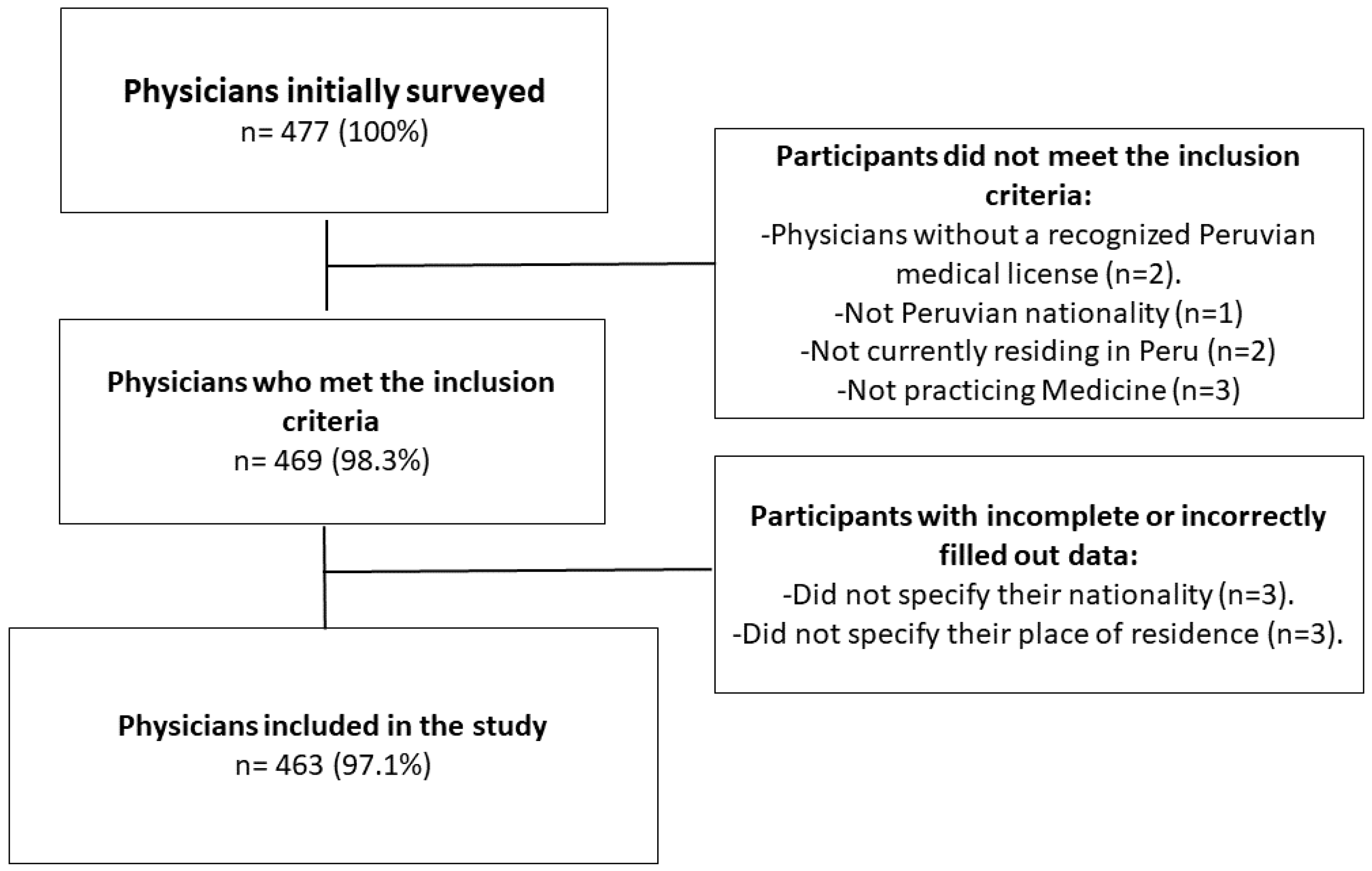
2.1. Study Design, Setting, and Participants
2.2. Sample and Diffusion
2.3. Questionnaire
2.4. Independent Variables
2.5. Dependent Variable: Knowledge of Mpox
2.6. Statistical Analysis
2.7. Ethical Aspects
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Monkeypox. WHO. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/monkeypox (accessed on 10 October 2022).
- Bunge, E.M.; Hoet, B.; Chen, L.; Lienert, F.; Weidenthaler, H.; Baer, L.R.; Steffen, R. The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLOS Negl. Trop. Dis. 2022, 16, e0010141. [Google Scholar] [CrossRef] [PubMed]
- Breman, J.G.; Kalisa-Ruti Steniowski, M.V.; Zanotto, E.; Gromyko, A.I.; Arita, I. Human monkeypox, 1970–1979. Bull World Health Organ 1980, 58, 165–182. [Google Scholar] [PubMed]
- Breman, J.G.; Henderson, D.A. Poxvirus dilemmas--monkeypox, smallpox, and biologic terrorism. N. Engl. J. Med. 1998, 339, 556–559. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Monkeypox in the U.S. CDC. 2022. Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html (accessed on 10 October 2022).
- World Health Organization. Multi-Country Monkeypox Outbreak: Situation Update. WHO. 2022. Available online: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON396 (accessed on 10 October 2022).
- Rodriguez-Morales, A.J.; Lopardo, G.; Verbanaz, S.; Orduna, T.; Lloveras, S.; Azeñas-Burgoa, J.M.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Barbosa, A.N.; Diaz-Quijano, F.; et al. Latin America: Situation and preparedness facing the multi-country human monkeypox outbreak. Lancet Reg. Health—Am. 2022, 13, 100318. [Google Scholar] [CrossRef] [PubMed]
- Cimerman, S.; Chebabo, A.; Cunha CA da Barbosa, A.N.; Rodríguez-Morales, A.J. Human monkeypox preparedness in Latin America—Are we ready for the next viral zoonotic disease outbreak after COVID-19? Braz. J. Infect. Dis. 2022, 26, 102372. [Google Scholar] [CrossRef]
- Ministry of Health. Minsa Confirms First Case of Monkeypox in Peru. MINSA. 2022. Available online: https://www.gob.pe/institucion/minsa/noticias/627040-minsa-confirma-primer-caso-de-la-viruela-del-mono-en-el-peru (accessed on 10 October 2022).
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S.; et al. Knowledge of human monkeypox viral infection among general practitioners: A cross-sectional study in Indonesia. Pathog. Glob. Health 2020, 114, 68–75. [Google Scholar] [CrossRef]
- Philpott, D. Epidemiologic and Clinical Characteristics of Monkeypox Cases—United States, May 17–July 22, 2022. MMWR Morb. Mortal Wkly Rep. 2022, 71, 1018–1022. [Google Scholar] [CrossRef]
- Adalja, A.; Inglesby, T. A Novel International Monkeypox Outbreak. Ann. Intern Med. 2022, 175, 1175–1176. [Google Scholar] [CrossRef]
- Tutu van Furth, A.M.; van der Kuip, M.; van Els, A.L.; Fievez, L.C.; van Rijckevorsel, G.G.; van den Ouden, A.; Jonges, M.; Welkers, M.R. Paediatric monkeypox patient with unknown source of infection, the Netherlands, June 2022. Euro. Surveill 2022, 27, 2200552. [Google Scholar] [CrossRef]
- Dye, C.; Kraemer, M.U.G. Investigating the monkeypox outbreak. BMJ 2022, 377, o1314. [Google Scholar] [CrossRef]
- Omrani, A.S.; Shalhoub, S. Middle East respiratory syndrome coronavirus (MERS-CoV): What lessons can we learn? J. Hosp. Infect. 2015, 91, 188–196. [Google Scholar] [CrossRef] [PubMed]
- McEachan, R.; Taylor, N.; Harrison, R.; Lawton, R.; Gardner, P.; Conner, M. Meta-Analysis of the Reasoned Action Approach (RAA) to Understanding Health Behaviors. Ann. Behav. Med. 2016, 50, 592–612. [Google Scholar] [CrossRef]
- Wilkason, C.; Lee, C.; Sauer, L.M.; Nuzzo, J.; McClelland, A. Assessing and Reducing Risk to Healthcare Workers in Outbreaks. Health Secur. 2020, 18, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Elm E von Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Ministry of Health. Monkeypox. MINSA. 2022. Available online: https://www.dge.gob.pe/portalnuevo/vigilancia-epidemiologica/subsistema-de-vigilancia/zoonoticas/viruela-del-mono/ (accessed on 10 October 2022).
- Medical Colleage of Peru. Registered Physicians. CMP. 2022. Available online: https://www.cmp.org.pe/medicos-colegiados-cmp/ (accessed on 10 October 2022).
- National Epidemiology Prevention and Infection Control Center of Peru. Ministry of Health. MINSA. 2023. Available online: https://www.dge.gob.pe/portalnuevo/ (accessed on 8 January 2023).
- World Health Organization. Monkeypox. WHO. 2018. Available online: https://www.who.int/emergencies/emergency-events/item/monkeypox (accessed on 10 October 2022).
- Alsanafi, M.; Al-Mahzoum, K.; Sallam, M. Monkeypox Knowledge and Confidence in Diagnosis and Management with Evaluation of Emerging Virus Infection Conspiracies among Health Professionals in Kuwait. Pathogens 2022, 11, 994. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Al-Mahzoum, K.; Al-Tammemi, A.B.; Alkurtas, M.; Mirzaei, F.; Kareem, N.; Al-Naimat, H.; Jardaneh, L.; Al-Majali, L.; AlHadidi, A.; et al. Assessing Healthcare Workers’ Knowledge and Their Confidence in the Diagnosis and Management of Human Monkeypox: A Cross-Sectional Study in a Middle Eastern Country. Healthcare (Basel) 2022, 10, 1722. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, N.Z.; Algethami, M.R.; Alarifi, A.M.; Alzahrani, F.; Sheerah, H.A.; Abdelaal, A.; Sah, R.; Rodriguez-Morales, A.J. Knowledge and attitude regarding monkeypox virus among physicians in Saudi Arabia, a cross-sectional study. Res. Sq. [Prepr.]. 2022, 10, 2099. [Google Scholar] [CrossRef]
- Zalcman, E.; Peru confirms first monkeypox-related death. In The Brazilian Report, Brazil. 2022. Available online: https://brazilian.report/liveblog/2022/08/02/peru-monkeypox-related-death/ (accessed on 10 October 2022).
- World Health Organization. Multi-Country Outbreak of Monkeypox, External Situation Report #3–10. WHO. 2022. Available online: https://www.who.int/publications/m/item/multi-country-outbreak-of-monkeypox--external-situation-report--3---10-august-2022 (accessed on 10 October 2022).
- World Health Organization. Multi-Country Outbreak of Monkeypox, External Situation Report #5–7. WHO. 2022. Available online: https://www.who.int/publications/m/item/multi-country-outbreak-of-monkeypox--external-situation-report--5---7-september-2022 (accessed on 10 October 2022).
- World Health Organization. 2022 Monkeypox Outbreak: Global Trends. WHO. 2022. Available online: https://worldhealthorg.shinyapps.io/mpx_global/ (accessed on 10 October 2022).
- JCR/RMB. Peru: Government Promotes Campaign to Prevent Monkeypox. Andina. 2022. Available online: https://andina.pe/ingles/noticia-peru-government-promotes-campaign-to-prevent-monkeypox-902910.aspx (accessed on 10 October 2022).
- Pittman, P.R.; Hahn, M.; Lee, H.S.; Koca, C.; Samy, N.; Schmidt, D.; Hornung, J.; Weidenthaler, H.; Heery, C.R.; Meyer, T.P.; et al. Phase 3 Efficacy Trial of Modified Vaccinia Ankara as a Vaccine against Smallpox. N. Engl. J. Med. 2019, 381, 1897–1908. [Google Scholar] [CrossRef]
- Food and Drug Administration. Monkeypox Update: FDA Authorizes Emergency Use of JYNNEOS Vaccine to Increase Vaccine Supply. FDA. 2022. Available online: https://www.fda.gov/news-events/press-announcements/monkeypox-update-fda-authorizes-emergency-use-jynneos-vaccine-increase-vaccine-supply (accessed on 10 October 2022).
- Riccò, M.; Ferraro, P.; Camisa, V.; Satta, E.; Zaniboni, A.; Ranzieri, S.; Baldassarre, A.; Zaffina, S.; Marchesi, F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop Med. Infect. Dis. 2022, 7, 135. [Google Scholar] [CrossRef]
- Salim, N.A.; Septadina, I.S.; Permata, M.; Hudari, H. Knowledge, attitude, and perception of anticipating 2022 global human monkeypox infection among internal medicine residents at palembang indonesia: An online survey. J. Kedokt. Dan Kesehat. Publ. Ilm. Fak. Kedokt. Univ. Sriwijaya. 2022, 9, 253–262. [Google Scholar] [CrossRef]
- BBC News. What Vaccines and Treatments Are Being Used against Monkeypox. 2022. Available online: https://www.bbc.com/mundo/noticias-62306701 (accessed on 11 October 2022).
- Reuters. Factbox: Countries Offering Vaccine for Monkeypox. 2022. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/countries-offering-vaccine-monkeypox-2022-05-24/ (accessed on 11 October 2022).
- Thornhill, J.P.; Barkati, S.; Walmsley, S.; Rockstroh, J.; Antinori, A.; Harrison, L.B.; Palich, R.; Nori, A.; Reeves, I.; Habibi, M.S.; et al. Monkeypox Virus Infection in Humans across 16 Countries—April–June 2022. N. Engl. J. Med. 2022, 387, 679–691. [Google Scholar] [CrossRef]
- Tarín-Vicente, E.J.; Alemany, A.; Agud-Dios, M.; Ubals, M.; Suñer, C.; Antón, A.; Arando, M.; Arroyo-Andrés, J.; Calderón-Lozano, L.; Casañ, C.; et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: A prospective observational cohort study. Lancet 2022, 400, 661–669. [Google Scholar] [CrossRef]
- Gedela, K.; Da Silva Fontoura, D.; Salam, A.; Gorman, G.; Golden, J.; O’Hara, G.; Elowaidy, A.; Tittle, V.; Girometti, N.; Whitlock, G.; et al. Infectious proctitis due to human monkeypox. Clin. Infect Dis. 2022, ciac713. [Google Scholar] [CrossRef]
- Lucar, J.; Roberts, A.; Saardi, K.M.; Yee, R.; Siegel, M.O.; Palmore, T.N. Monkeypox Virus-Associated Severe Proctitis Treated With Oral Tecovirimat: A Report of Two Cases. Ann. Intern Med. 2022, 175, 1626–1627. [Google Scholar] [CrossRef]
- De Nicolas-Ruanes, B.; Vivancos, M.; Azcarraga-Llobet, C.; Moreno, A.; Rodriguez-Dominguez, M.; Berna-Rico, E.; Garcia-Mouronte, E.; Carron-Herrero, A.; McGee, A.; Galan, J.; et al. Monkeypox virus case with maculopapular exanthem and proctitis during the Spanish outbreak in 2022. J. Eur. Acad. Dermatol. Venereol. 2022, 36, e658–e660. [Google Scholar] [CrossRef]
- Haller, S.L.; Peng, C.; McFadden, G.; Rothenburg, S. Poxviruses and the Evolution of Host Range and Virulence. Infect Genet. Evol. 2014, 21, 15–40. [Google Scholar] [CrossRef]
- Antinori, A.; Mazzotta, V.; Vita, S.; Carletti, F.; Tacconi, D.; Lapini, L.E.; D’Abramo, A.; Cicalini, S.; Lapa, D.; Pittalis, S.; et al. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro. Surveill 2022, 27, 2200421. [Google Scholar] [CrossRef]
- Girometti, N.; Byrne, R.; Bracchi, M.; Heskin, J.; McOwan, A.; Tittle, V.; Gedela, K.; Scott, C.; Patel, S.; Gohil, J.; et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: An observational analysis. Lancet Infect Dis. 2022, 22, 1321–1328. [Google Scholar] [CrossRef]
- Yardley, S.; Teunissen, P.W.; Dornan, T. Experiential learning: AMEE Guide No. 63. Med. Teach. 2012, 34, e102–e115. [Google Scholar] [CrossRef]
- Tanaka, K.; Son, D. Experiential learning for junior residents as a part of community-based medical education in Japan. Educ. Prim. Care 2019, 30, 282–288. [Google Scholar] [CrossRef]
- Schiel, K.; Everard, K. Active Learning Versus Traditional Teaching Methods in the Family Medicine Clerkship. Fam. Med. 2021, 53, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Ellington, L.E.; Becerra, R.; Mallma, G.; Tantaleán da Fieno, J.; Nair, D.; Onchiri, F.; Nielsen, K.R. Knowledge acquisition and retention after a high flow training programme in Peru: A quasi-experimental single group pre–post design. BMJ Open 2020, 10, e035125. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Monkeypox situation in Peru. MINSA. 2022. Available online: https://www.dge.gob.pe/sala-monkeypox/ (accessed on 10 October 2022).
- Riad, A.; Drobov, A.; Rozmarinová, J.; Drapáčová, P.; Klugarová, J.; Dušek, L.; Pokorná, A.; Klugar, M. Monkeypox Knowledge and Vaccine Hesitancy of Czech Healthcare Workers: A Health Belief Model (HBM)-Based Study. Vaccines 2022, 10, 2022. [Google Scholar] [CrossRef]
- Vu, M.; Huynh, V.N.; Bednarczyk, R.A.; Escoffery, C.; Ta, D.; Nguyen, T.T.; Berg, C.J. Experience and lessons learned from multi-modal internet-based recruitment of U.S. Vietnamese into research. PLoS ONE 2021, 16, e0256074. [Google Scholar] [CrossRef] [PubMed]
- Haddad, C.; Sacre, H.; Zeenny, R.M.; Hajj, A.; Akel, M.; Iskandar, K.; Salameh, P. Should samples be weighted to decrease selection bias in online surveys during the COVID-19 pandemic? Data from seven datasets. BMC Med Res Methodol. 2022, 22, 63. [Google Scholar] [CrossRef]

| Characteristic | N = 463 |
|---|---|
| Gender | |
| Female | 194 (41.9%) |
| Male | 269 (58.1%) |
| Age, mean (SD) | 36.6 (10.3) |
| Macro-region | |
| Lima and Callao | 263 (56.8%) |
| Central | 27 (5.8%) |
| North | 44 (9.5%) |
| Eastern | 58 (12.5%) |
| South | 71 (15.3%) |
| Undergraduate University | |
| Private University | 201 (43.4%) |
| Public University | 262 (56.6%) |
| Years from medical school graduation, mean (SD) | 9.9 (9.5) |
| Medical position | |
| Medical Specialist | 189 (40.8%) |
| General Practitioner | 234 (50.5%) |
| Resident Physician (in training) | 40 (8.6%) |
| Postgraduate degree | |
| Doctorate | 4 (0.9%) |
| Master’s degree | 117 (25.3%) |
| None | 342 (73.9%) |
| Area of work | |
| Rural Zone | 73 (15.8%) |
| Urban Zone | 390 (84.2%) |
| Awareness about the current mpox virus | |
| No | 5 (1.1%) |
| Yes | 458 (98.9%) |
| Experience in taking care of a patient with mpox | |
| No | 396 (85.5%) |
| Yes | 67 (14.5%) |
| Knowledge score, median (IQR) | 14.00 (13.0, 15.0) |
| Knowledge percentile | |
| ≤p50, 0–14 points | 247 (53.3%) |
| >p50, >14 points | 216 (46.7%) |
| % of correct answers | |
| <70% | 33 (7.1%) |
| >70% | 430 (92.9%) |
| Questions: Correct Answer | N = 463 | |
|---|---|---|
| Mpox is caused by: A virus | 99.6% | 461 |
| Cases of mpox have been reported in Peru: True | 99.1% | 459 |
| Mpox can be transmitted from person to person: True | 98.7% | 457 |
| What treatment would you use for people with mild symptoms of mpox? Symptomatic treatment. | 96.5% | 447 |
| Mpox has a mortality rate of approximately 80%: False | 96.1% | 445 |
| People with symptoms of mpox require isolation to limit the spread of the infection: True | 95.0% | 440 |
| Vesicles are one of the classic lesions of mpox: True | 91.6% | 424 |
| Patients with mpox may present with influenza-like symptoms in the first few days of illness: True | 90.9% | 421 |
| It is not a route of transmission of mpox: Mosquito bite | 89.6% | 415 |
| What is the incubation period of mpox? 5–21 days | 89.4% | 414 |
| Mpox is a disease endemic to Central and West Africa: True | 86.0% | 398 |
| Mpox lesions do not occur on the genitals: False | 83.8% | 388 |
| What is the population most affected by mpox in the present outbreak? Men who have sex with men | 83.6% | 387 |
| Which test is used to confirm the diagnosis of mpox? PCR of the lesions | 81.4% | 377 |
| There is an FDA-approved vaccine to prevent mpox: True | 60.7% | 281 |
| Proctitis is one of the manifestations of mpox: True | 49.0% | 227 |
| Mpox can be transmitted to a person by the bite of an infected rodent: True | 33.3% | 154 |
| Characteristic | ≤P50, | >P50, | cPR [95% CI] * | p-Value |
|---|---|---|---|---|
| N = 247 | N = 216 | |||
| Gender | ||||
| Female | 109 (56.2%) | 85 (43.8%) | Ref. | Ref. |
| Male | 138 (51.3%) | 131 (48.7%) | 1.11 [0.91 to 1.36] | 0.301 |
| Age, mean (SD) | 36.4 (10.2) | 36.8 (10.5) | 1.00 [0.99 to 1.01] | 0.678 |
| Macro-region | ||||
| Lima and Callao | 130 (49.4%) | 133 (50.6%) | Ref. | Ref. |
| Central | 18 (66.7%) | 9 (33.3%) | 0.66 [0.38 to 1.14] | 0.093 |
| North | 20 (45.5%) | 24 (54.5%) | 1.08 [0.80 to 1.45] | 0.060 |
| East | 40 (69.0%) | 18 (31.0%) | 0.61 [0.41 to 0.92] | 0.007 |
| South | 39 (54.9%) | 32 (45.1%) | 0.89 [0.67 to 1.18] | 0.415 |
| Undergraduate University | ||||
| Private University | 116 (57.7%) | 85 (42.3%) | Ref. | Ref. |
| Public University | 131 (50.0%) | 131 (50.0%) | 1.18 [0.97 to 1.45] | 0.101 |
| Years from medical school graduation, mean (SD) | 9.64 (9.13) | 10.2 (9.86) | 1.00 [0.99 to 1.01] | 0.488 |
| Medical position | ||||
| Medical Specialist | 97 (51.3%) | 92 (48.7%) | Ref. | Ref. |
| General Practitioner | 130 (55.6%) | 104 (44.4%) | 0.91 [0.74 to 1.12] | 0.388 |
| Resident Physician (in training) | 20 (50.0%) | 20 (50.0%) | 1.03 [0.73 to 1.45] | 0.880 |
| Postgraduate degree | ||||
| Doctorate | 3 (75.0%) | 1 (25.0%) | Ref. | Ref. |
| Master’s degree | 67 (57.3%) | 50 (42.7%) | 1.71 [0.31 to 9.45] | 0.544 |
| None | 177 (51.8%) | 165 (48.2%) | 1.93 [0.35 to 10.6] | 0.415 |
| Area of work | ||||
| Rural Zone | 42 (57.5%) | 31 (42.5%) | Ref. | Ref. |
| Urban Zone | 205 (52.6%) | 185 (47.4%) | 1.12 [0.84 to 1.49] | 0.439 |
| Awareness about the current mpox outbreak | ||||
| No | 3 (60.0%) | 2 (40.0%) | Ref. | Ref. |
| Yes | 244 (53.3%) | 214 (46.7%) | 1.17 [0.40 to 3.43] | 0.794 |
| Experience in taking care of a patient with mpox | ||||
| No | 222 (56.1%) | 174 (43.9%) | Ref. | Ref. |
| Yes | 25 (37.3%) | 42 (62.7%) | 1.43 [1.15 to A1.77] | 0.005 |
| Variables | aPR * | CI 95% | p | |
|---|---|---|---|---|
| Macro-region | ||||
| Lima and Callao | Ref. | |||
| Central | 0.67 | 0.39 | 1.15 | 0.148 |
| North | 1.09 | 0.81 | 1.46 | 0.566 |
| East | 0.62 | 0.42 | 0.93 | 0.022 |
| South | 0.91 | 0.69 | 1.20 | 0.504 |
| Experience in taking care of a patient with mpox | ||||
| No | ||||
| Yes | 1.40 | 1.13 | 1.73 | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonzales-Zamora, J.A.; Soriano-Moreno, D.R.; Soriano-Moreno, A.N.; Ponce-Rosas, L.; Sangster-Carrasco, L.; De-Los-Rios-Pinto, A.; Benito-Vargas, R.M.; Murrieta-Ruiz, V.; Morocho-Alburqueque, N.; Caira-Chuquineyra, B.; et al. Level of Knowledge Regarding Mpox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study. Vaccines 2023, 11, 167. https://doi.org/10.3390/vaccines11010167
Gonzales-Zamora JA, Soriano-Moreno DR, Soriano-Moreno AN, Ponce-Rosas L, Sangster-Carrasco L, De-Los-Rios-Pinto A, Benito-Vargas RM, Murrieta-Ruiz V, Morocho-Alburqueque N, Caira-Chuquineyra B, et al. Level of Knowledge Regarding Mpox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study. Vaccines. 2023; 11(1):167. https://doi.org/10.3390/vaccines11010167
Chicago/Turabian StyleGonzales-Zamora, Jose A., David R. Soriano-Moreno, Anderson N. Soriano-Moreno, Linda Ponce-Rosas, Lucero Sangster-Carrasco, Abraham De-Los-Rios-Pinto, Raysa M. Benito-Vargas, Valentina Murrieta-Ruiz, Noelia Morocho-Alburqueque, Brenda Caira-Chuquineyra, and et al. 2023. "Level of Knowledge Regarding Mpox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study" Vaccines 11, no. 1: 167. https://doi.org/10.3390/vaccines11010167
APA StyleGonzales-Zamora, J. A., Soriano-Moreno, D. R., Soriano-Moreno, A. N., Ponce-Rosas, L., Sangster-Carrasco, L., De-Los-Rios-Pinto, A., Benito-Vargas, R. M., Murrieta-Ruiz, V., Morocho-Alburqueque, N., Caira-Chuquineyra, B., Fernandez-Guzman, D., Ccami-Bernal, F., Quispe-Vicuña, C., Alarcon-Parra, M., Pinedo-Soria, A., & Alave, J. (2023). Level of Knowledge Regarding Mpox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study. Vaccines, 11(1), 167. https://doi.org/10.3390/vaccines11010167







