Social Support Mediates the Relationship between COVID-19-Related Burnout and Booster Vaccination Willingness among Fully Vaccinated Nurses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measures
2.2.1. Demographic and COVID-19-Related Variables
2.2.2. Booster Vaccination Willingness
2.2.3. Social Support
2.2.4. Burnout
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Descriptive Statistics and Correlations
3.3. Linear Regression Analysis
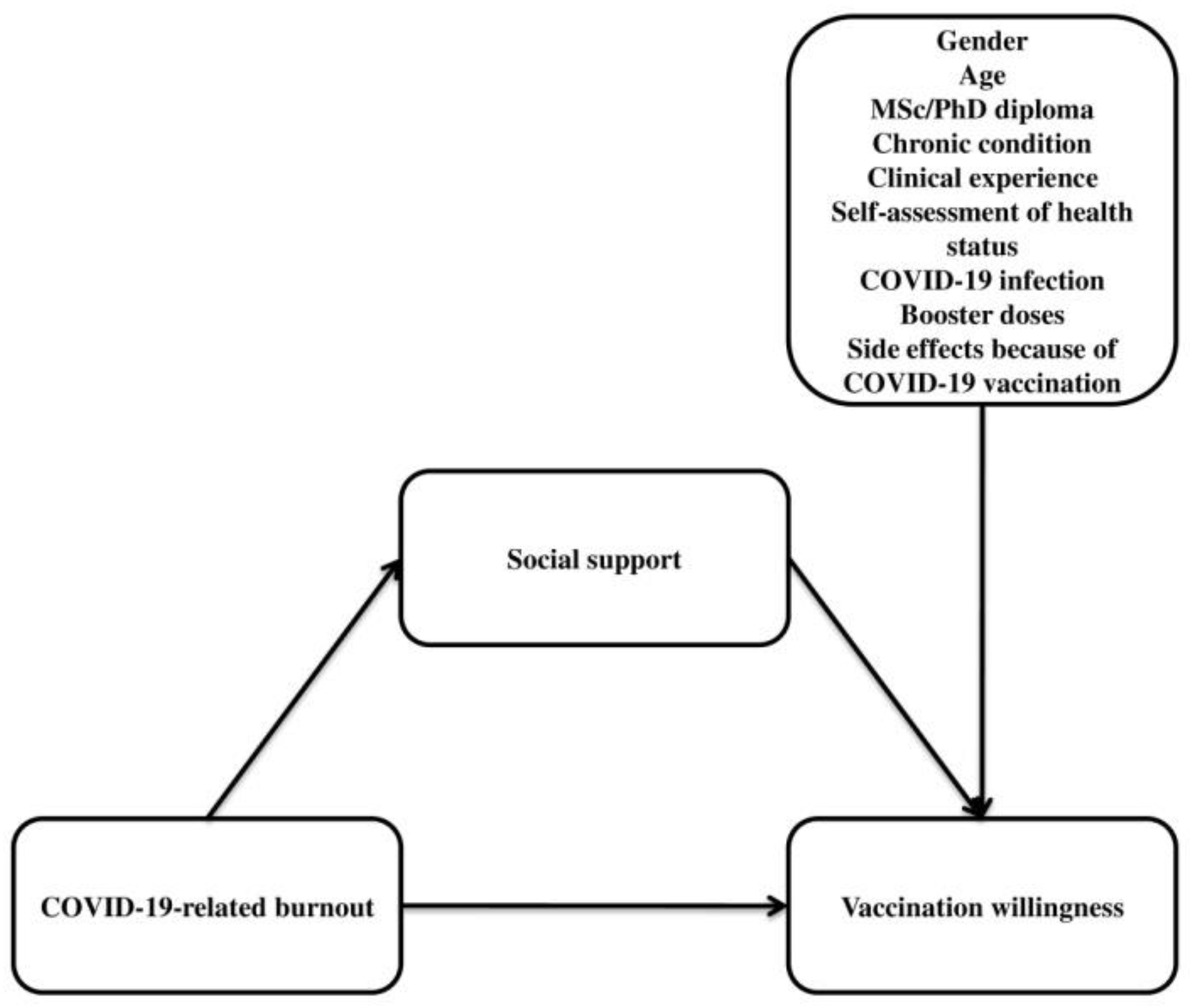
3.4. Mediation Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Worldometer. COVID-19 Coronavirus Pandemic 2022. Available online: https://www.worldometers.info/coronavirus/ (accessed on 27 November 2022).
- Abdel-Gawad, M.; Zaghloul, M.S.; Abd-Elsalam, S.; Hashem, M.; Lashen, S.A.; Mahros, A.M.; Mohammed, A.Q.; Hassan, A.M.; Bekhit, A.N.; Mohammed, W.; et al. Post-COVID-19 Syndrome Clinical Manifestations: A Systematic Review. Anti-Inflamm. Anti-Allergy Agents Med. Chem. 2022, 21, 115–120. [Google Scholar] [CrossRef]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and Cognitive Impairment in Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef] [PubMed]
- Jennings, G.; Monaghan, A.; Xue, F.; Mockler, D.; Romero-Ortuño, R. A Systematic Review of Persistent Symptoms and Residual Abnormal Functioning Following Acute COVID-19: Ongoing Symptomatic Phase vs. Post-COVID-19 Syndrome. J. Clin. Med. 2021, 10, 5913. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Coronavirus (COVID-19) Vaccinations 2022. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 27 November 2022).
- Chavda, V.P.; Bezbaruah, R.; Deka, K.; Nongrang, L.; Kalita, T. The Delta and Omicron Variants of SARS-CoV-2: What We Know So Far. Vaccines 2022, 10, 1926. [Google Scholar] [CrossRef] [PubMed]
- Zeng, B.; Gao, L.; Zhou, Q.; Yu, K.; Sun, F. Effectiveness of COVID-19 Vaccines against SARS-CoV-2 Variants of Concern: A Systematic Review and Meta-Analysis. BMC Med. 2022, 20, 200. [Google Scholar] [CrossRef]
- Zarębska-Michaluk, D.; Hu, C.; Brzdęk, M.; Flisiak, R.; Rzymski, P. COVID-19 Vaccine Booster Strategies for Omicron SARS-CoV-2 Variant: Effectiveness and Future Prospects. Vaccines 2022, 10, 1223. [Google Scholar] [CrossRef]
- Zhu, Y.; Liu, S.; Zhang, D. Effectiveness of COVID-19 Vaccine Booster Shot Compared with Non-Booster: A Meta-Analysis. Vaccines 2022, 10, 1396. [Google Scholar] [CrossRef]
- Khong, K.-W.; Zhang, R.; Hung, I.F.-N. The Four Ws of the Fourth Dose COVID-19 Vaccines: Why, Who, When and What. Vaccines 2022, 10, 1924. [Google Scholar] [CrossRef]
- Lee, A.R.Y.B.; Wong, S.Y.; Tay, S.H. Booster COVID-19 Vaccines for Immune-Mediated Inflammatory Disease Patients: A Systematic Review and Meta-Analysis of Efficacy and Safety. Vaccines 2022, 10, 668. [Google Scholar] [CrossRef]
- Tenforde, M.W.; Patel, M.M.; Gaglani, M.; Ginde, A.A.; Douin, D.J.; Talbot, H.K.; Casey, J.D.; Mohr, N.M.; Zepeski, A.; McNeal, T.; et al. Effectiveness of a Third Dose of Pfizer-BioNTech and Moderna Vaccines in Preventing COVID-19 Hospitalization Among Immunocompetent and Immunocompromised Adults—United States, August–December 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Dzinamarira, T.; Nkambule, S.J.; Hlongwa, M.; Mhango, M.; Iradukunda, P.G.; Chitungo, I.; Dzobo, M.; Mapingure, M.P.; Chingombe, I.; Mashora, M.; et al. Risk Factors for COVID-19 Infection Among Healthcare Workers. A First Report From a Living Systematic Review and Meta-Analysis. Saf. Health Work 2022, 13, 263–268. [Google Scholar] [CrossRef]
- International Council of Nurses. ICN Says 115,000 Healthcare Worker Deaths from COVID-19 Exposes Collective Failure of Leaders to Protect Global Workforce. Available online: https://www.icn.ch/news/icn-says-115000-healthcare-worker-deaths-covid-19-exposes-collective-failure-leaders-protect (accessed on 1 June 2022).
- World Health Organization. The Impact of COVID-19 on Health and Care Workers: A Closer Look at Deaths; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- National Nurses United. Registered Nurses Call on CDC to Prioritize Health Care Workers for Second COVID-19 Booster Shot. Available online: https://www.nationalnursesunited.org/press/nurses-call-on-cdc-to-prioritize-health-care-workers-with-second-booster-shot (accessed on 1 June 2022).
- Wise, J. COVID-19: JCVI Advises Further Booster for Vulnerable Adults and Health and Care Workers. BMJ 2022, 377, o1277. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Dashboard Officially Reporting COVID-19 Vaccination Data. Available online: https://app.powerbi.com/view?r=eyJrIjoiMWNjNzZkNjctZTNiNy00YmMzLTkxZjQtNmJiZDM2MTYxNzEwIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed on 27 November 2022).
- Katzman, J.G.; Katzman, J.W. Primary Care Clinicians as COVID-19 Vaccine Ambassadors. J. Prim. Care Community Health 2021, 12, 215013272110070. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Katsiroumpa, A.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Mariolis-Sapsakos, T.; Kaitelidou, D. Predictors of Second COVID-19 Booster Dose or New COVID-19 Vaccine Hesitancy among Nurses: A Cross-Sectional Study. J. Clin. Nurs. 2022, jocn.16576. [Google Scholar] [CrossRef]
- Abdelmoneim, S.A.; Sallam, M.; Hafez, D.M.; Elrewany, E.; Mousli, H.M.; Hammad, E.M.; Elkhadry, S.W.; Adam, M.F.; Ghobashy, A.A.; Naguib, M.; et al. COVID-19 Vaccine Booster Dose Acceptance: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2022, 7, 298. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ Burnout and Associated Risk Factors during the COVID-19 Pandemic: A Systematic Review and Meta-analysis. J. Adv. Nurs. 2021, 77, 3286–3302. [Google Scholar] [CrossRef]
- Hur, G.; Cinar, N.; Suzan, O.K. Impact of COVID-19 Pandemic on Nurses’ Burnout and Related Factors: A Rapid Systematic Review. Arch. Psychiatr. Nurs. 2022, 41, 248–263. [Google Scholar] [CrossRef]
- Ramírez-Elvira, S.; Romero-Béjar, J.L.; Suleiman-Martos, N.; Gómez-Urquiza, J.L.; Monsalve-Reyes, C.; Cañadas-De la Fuente, G.A.; Albendín-García, L. Prevalence, Risk Factors and Burnout Levels in Intensive Care Unit Nurses: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11432. [Google Scholar] [CrossRef]
- Sullivan, D.; Sullivan, V.; Weatherspoon, D.; Frazer, C. Comparison of Nurse Burnout, Before and During the COVID-19 Pandemic. Nurs. Clin. N. Am. 2022, 57, 79–99. [Google Scholar] [CrossRef]
- World Health Organization. ICD-11: International Classification of Diseases, 11th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Chen, C.; Meier, S.T. Burnout and Depression in Nurses: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021, 124, 104099. [Google Scholar] [CrossRef] [PubMed]
- Jun, J.; Ojemeni, M.M.; Kalamani, R.; Tong, J.; Crecelius, M.L. Relationship between Nurse Burnout, Patient and Organizational Outcomes: Systematic Review. Int. J. Nurs. Stud. 2021, 119, 103933. [Google Scholar] [CrossRef] [PubMed]
- Khatatbeh, H.; Pakai, A.; Al-Dwaikat, T.; Onchonga, D.; Amer, F.; Prémusz, V.; Oláh, A. Nurses’ Burnout and Quality of Life: A Systematic Review and Critical Analysis of Measures Used. Nurs. Open 2022, 9, 1564–1574. [Google Scholar] [CrossRef] [PubMed]
- Membrive-Jiménez, M.J.; Gómez-Urquiza, J.L.; Suleiman-Martos, N.; Velando-Soriano, A.; Ariza, T.; De la Fuente-Solana, E.I.; Cañadas-De la Fuente, G.A. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare 2022, 10, 954. [Google Scholar] [CrossRef] [PubMed]
- Lin, N.; Ensel, W.M.; Simeone, R.S.; Kuo, W. Social Support, Stressful Life Events, and Illness: A Model and an Empirical Test. J. Health Soc. Behav. 1979, 20, 108. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Sayin Kasar, K.; Karaman, E. Life in Lockdown: Social Isolation, Loneliness and Quality of Life in the Elderly during the COVID-19 Pandemic: A Scoping Review. Geriatr. Nurs. 2021, 42, 1222–1229. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Zhang, X.; Bai, S.; Minhat, H.S.; Nazan, A.I.N.M.; Feng, J.; Li, X.; Luo, G.; Zhang, X.; Feng, J.; et al. Assessing Social Support Impact on Depression, Anxiety, and Stress among Undergraduate Students in Shaanxi Province during the COVID-19 Pandemic of China. PLoS ONE 2021, 16, e0253891. [Google Scholar] [CrossRef] [PubMed]
- Hou, T.; Zhang, T.; Cai, W.; Song, X.; Chen, A.; Deng, G.; Ni, C. Social Support and Mental Health among Health Care Workers during Coronavirus Disease 2019 Outbreak: A Moderated Mediation Model. PLoS ONE 2020, 15, e0233831. [Google Scholar] [CrossRef] [PubMed]
- Kaya, H.; Ayık, B.; Tasdelen, R.; Ercis, M.; Ertekin, E. Social Support Promotes Mental Health During the COVID-19 Outbreak: A Cross-Sectional Study from Turkey. Psychiatr. Danub. 2021, 33, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Qi, M.; Zhou, S.-J.; Guo, Z.-C.; Zhang, L.-G.; Min, H.-J.; Li, X.-M.; Chen, J.-X. The Effect of Social Support on Mental Health in Chinese Adolescents During the Outbreak of COVID-19. J. Adolesc. Health 2020, 67, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Luo, S.; Mu, W.; Li, Y.; Ye, L.; Zheng, X.; Xu, B.; Ding, Y.; Ling, P.; Zhou, M.; et al. Effects of Sources of Social Support and Resilience on the Mental Health of Different Age Groups during the COVID-19 Pandemic. BMC Psychiatry 2021, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Huang, N.; Fu, M.; Zhang, H.; Feng, X.L.; Guo, J. Relationship Between Risk Perception, Social Support, and Mental Health Among General Chinese Population During the COVID-19 Pandemic. Risk Manag. Healthc. Policy 2021, 14, 1843–1853. [Google Scholar] [CrossRef] [PubMed]
- Szkody, E.; Stearns, M.; Stanhope, L.; McKinney, C. Stress-Buffering Role of Social Support during COVID-19. Fam. Proc. 2021, 60, 1002–1015. [Google Scholar] [CrossRef] [PubMed]
- Jaspal, R.; Breakwell, G.M. Social Support, Perceived Risk and the Likelihood of COVID-19 Testing and Vaccination: Cross-Sectional Data from the United Kingdom. Curr. Psychol. 2022, 41, 492–504. [Google Scholar] [CrossRef] [PubMed]
- Stickley, A.; Matsubayashi, T.; Ueda, M. Loneliness and COVID-19 Preventive Behaviours among Japanese Adults. J. Public Health 2021, 43, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Yan, J.; Wu, C.; He, C.; Lin, Y.; He, S.; Du, Y.; Cao, B.; Lang, H. The Social Support, Psychological Resilience and Quality of Life of Nurses in Infectious Disease Departments in China: A Mediated Model. J. Nurs. Manag. 2022, jonm.13889. [Google Scholar] [CrossRef] [PubMed]
- Du, J.; Liu, Z.; Zhang, X.; Shao, P.; Hua, Y.; Li, Y.; Lang, H.; Ni, C. Occupational Stress and Insomnia Symptoms Among Nurses During the Outbreak of COVID-19 in China: The Chain Mediating Effect of Perceived Organizational Support and Psychological Capital. Front. Psychiatry 2022, 13, 882385. [Google Scholar] [CrossRef] [PubMed]
- Fronda, D.C.; Labrague, L.J. Turnover Intention and Coronaphobia among Frontline Nurses during the Second Surge of COVID-19: The Mediating Role of Social Support and Coping Skills. J. Nurs. Manag. 2022, 30, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Hou, T.; Yin, Q.; Xu, Y.; Gao, J.; Bin, L.; Li, H.; Cai, W.; Liu, Y.; Dong, W.; Deng, G.; et al. The Mediating Role of Perceived Social Support Between Resilience and Anxiety 1 Year After the COVID-19 Pandemic: Disparity Between High-Risk and Low-Risk Nurses in China. Front. Psychiatry 2021, 12, 666789. [Google Scholar] [CrossRef] [PubMed]
- Patelarou, A.; Saliaj, A.; Galanis, P.; Pulomenaj, V.; Prifti, V.; Sopjani, I.; Mechili, E.A.; Laredo-Aguilera, J.A.; Kicaj, E.; Kalokairinou, A.; et al. Predictors of Nurses’ Intention to Accept COVID-19 Vaccination: A Cross-sectional Study in Five European Countries. J. Clin. Nurs. 2022, 31, 1258–1266. [Google Scholar] [CrossRef] [PubMed]
- Rabi, R.; Maraqa, B.; Nazzal, Z.; Zink, T. Factors Affecting Nurses’ Intention to Accept the COVID-19 Vaccine: A Cross-Sectional Study. Public Health Nurs. 2021, 38, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Fontenot, H.B.; Mattheus, D.; Lim, E.; Michel, A.; Ryan, N.; Davis, K.F.; Zimet, G. Assessing Licensed Nurses COVID-19 Vaccine Attitudes and Intentions: A Cross-Sectional Survey in the State of Hawaii. Hum. Vaccin. Immunother. 2021, 17, 3933–3940. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Editor’s Choice: Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Trabucco Aurilio, M.; Mennini, F.S.; Gazzillo, S.; Massini, L.; Bolcato, M.; Feola, A.; Ferrari, C.; Coppeta, L. Intention to Be Vaccinated for COVID-19 among Italian Nurses during the Pandemic. Vaccines 2021, 9, 500. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.; Hult, T.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Pachi, A.; Sikaras, C.; Ilias, I.; Panagiotou, A.; Zyga, S.; Tsironi, M.; Baras, S.; Tsitrouli, L.A.; Tselebis, A. Burnout, Depression and Sense of Coherence in Nurses during the Pandemic Crisis. Healthcare 2022, 10, 134. [Google Scholar] [CrossRef] [PubMed]
- Sikaras, C.; Ilias, I.; Tselebis, A.; Pachi, A.; Zyga, S.; Tsironi, M.; Gil, A.P.R.; Panagiotou, A. Nursing Staff Fatigue and Burnout during the COVID-19 Pandemic in Greece. AIMS Public Health 2022, 9, 94–105. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Theofilou, P. Translation and Cultural Adaptation of the Multidimensional Scale of Perceived Social Support for Greece. Health Psychol. Res. 2015, 3, 1061. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Katsiroumpa, A.; Sourtzi, P.; Siskou, O.; Konstantakopoulou, O.; Kaitelidou, D. The COVID-19 Burnout Scale: Development and Initial Validation. medrxiv 2022. [Google Scholar] [CrossRef]
- Seber, G.; Lee, A. Linear Regression Analysis, 2nd ed.; Wiley: Hoboken, NJ, USA, 2003. [Google Scholar]
- Hayes, A. Introduction to Mediation, Moderation, and Conditional Process Analysis; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.; Cheshmehzangi, A.; McDonnell, D.; da Veiga, C.P.; Xiang, Y.-T. Mind the “Vaccine Fatigue”. Front. Immunol. 2022, 13, 839433. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.-R.; Hong, H.-J.; Chang, J.-J.; Shin, S.-H. The Association between Korean Clinical Nurses’ Workplace Bullying, Positive Psychological Capital, and Social Support on Burnout. Int. J. Environ. Res. Public Health 2021, 18, 11583. [Google Scholar] [CrossRef] [PubMed]
- Liao, H.; Liang, R.; He, H.; Huang, Y.; Liu, M. Work Stress, Burnout, Occupational Commitment, and Social Support among Chinese Pediatric Nurses: A Moderated Mediation Model. J. Pediatr. Nurs. 2022, 67, e16–e23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Guan, C.; Jiang, J.; Zhu, C.; Hu, X. Mediating Effect of Resilience on the Relationship between Perceived Social Support and Burnout among Chinese Palliative Nurses. J. Clin. Nurs. 2022, jocn.16532. [Google Scholar] [CrossRef] [PubMed]
- Velando-Soriano, A.; Ortega-Campos, E.; Gómez-Urquiza, J.L.; Ramírez-Baena, L.; De La Fuente, E.I.; Cañadas-De La Fuente, G.A. Impact of Social Support in Preventing Burnout Syndrome in Nurses: A Systematic Review. Jpn. J. Nurs. Sci. 2020, 17, e12269. [Google Scholar] [CrossRef] [PubMed]
- Han, H.-Y.; Lee, J.-Y.; Jang, I. The Moderating Effects of Social Support between Emotional Labor and Job Satisfaction in Clinical Nurses. Korean J. Occup. Health Nurs. 2015, 24, 331–339. [Google Scholar] [CrossRef][Green Version]
- Bradley, J.R.; Cartwright, S. Social Support, Job Stress, Health, and Job Satisfaction Among Nurses in the United Kingdom. Int. J. Stress Manag. 2002, 9, 163–182. [Google Scholar] [CrossRef]
- Khattak, S.R.; Saeed, I.; Rehman, S.U.; Fayaz, M. Impact of Fear of COVID-19 Pandemic on the Mental Health of Nurses in Pakistan. J. Loss Trauma 2021, 26, 421–435. [Google Scholar] [CrossRef]
- Song, J.; McDonald, C. Experiences of New Zealand Registered Nurses of Chinese Ethnicity during the COVID-19 Pandemic. J. Clin. Nurs. 2021, 30, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Izcovich, A.; Ragusa, M.A.; Tortosa, F.; Lavena Marzio, M.A.; Agnoletti, C.; Bengolea, A.; Ceirano, A.; Espinosa, F.; Saavedra, E.; Sanguine, V.; et al. Prognostic Factors for Severity and Mortality in Patients Infected with COVID-19: A Systematic Review. PLoS ONE 2020, 15, e0241955. [Google Scholar] [CrossRef] [PubMed]
- Shang, W.; Wang, Y.; Yuan, J.; Guo, Z.; Liu, J.; Liu, M. Global Excess Mortality during COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 1702. [Google Scholar] [CrossRef] [PubMed]
- Dadras, O.; SeyedAlinaghi, S.; Karimi, A.; Shamsabadi, A.; Qaderi, K.; Ramezani, M.; Mirghaderi, S.P.; Mahdiabadi, S.; Vahedi, F.; Saeidi, S.; et al. COVID-19 Mortality and Its Predictors in the Elderly: A Systematic Review. Health Sci. Rep. 2022, 5, e657. [Google Scholar] [CrossRef] [PubMed]
- Oueijan, R.I.; Hill, O.R.; Ahiawodzi, P.D.; Fasinu, P.S.; Thompson, D.K. Rare Heterogeneous Adverse Events Associated with MRNA-Based COVID-19 Vaccines: A Systematic Review. Medicines 2022, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Dighriri, I.M.; Alhusayni, K.M.; Mobarki, A.Y.; Aljerary, I.S.; Alqurashi, K.A.; Aljuaid, F.A.; Alamri, K.A.; Mutwalli, A.A.; Maashi, N.A.; Aljohani, A.M.; et al. Pfizer-BioNTech COVID-19 Vaccine (BNT162b2) Side Effects: A Systematic Review. Cureus 2022, 14, e23526. [Google Scholar] [CrossRef] [PubMed]
- Kouhpayeh, H.; Ansari, H. Adverse Events Following COVID-19 Vaccination: A Systematic Review and Meta-Analysis. Int. Immunopharmacol. 2022, 109, 108906. [Google Scholar] [CrossRef] [PubMed]

| Variable | N | % |
|---|---|---|
| Gender | ||
| Females | 851 | 88.4 |
| Males | 112 | 11.6 |
| MSc/PhD diploma | ||
| No | 437 | 45.4 |
| Yes | 526 | 54.6 |
| Chronic condition | ||
| No | 722 | 75.0 |
| Yes | 241 | 25.0 |
| Self-assessment of health status | ||
| Very poor | 26 | 2.7 |
| Poor | 16 | 1.7 |
| Moderate | 70 | 7.3 |
| Good | 580 | 60.2 |
| Very good | 271 | 28.1 |
| COVID-19 infection | ||
| No | 272 | 28.2 |
| Yes | 691 | 71.8 |
| Booster doses | ||
| No | 102 | 10.6 |
| Yes | 861 | 89.4 |
| Variable | Mean | SD | Median |
|---|---|---|---|
| Age | 37.9 | 9.6 | 37.0 |
| Clinical experience (years) | 12.0 | 9.2 | 11.0 |
| Side-effects because of COVID-19 vaccination | 3.1 | 2.6 | 2.0 |
| COVID-19 vaccination willingness | 5.3 | 3.6 | 5.0 |
| COVID-19-related burnout | 3.2 | 0.9 | 3.2 |
| Total social support | 6.0 | 1.2 | 6.4 |
| Family support | 6.0 | 1.4 | 6.5 |
| Friends support | 5.9 | 1.4 | 6.3 |
| Significant others support | 6.1 | 1.3 | 6.8 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | 0.878 *** | 0.010 | 0.152 *** | −0.015 | −0.098 ** | −0.025 | −0.127 *** | −0.108 ** |
| 2. Clinical experience (years) | - | 0.075 * | 0.137 *** | 0.006 | −0.087 * | −0.028 | −0.091 ** | −0.112 *** | |
| 3. Side-effects because of COVID-19 vaccination | - | −0.240 *** | 0.274 *** | −0.047 | −0.056 | −0.019 | −0.049 | ||
| 4. COVID-19 vaccination willingness | - | −0.291 *** | 0.136 *** | 0.114** | 0.141 *** | 0.165 *** | |||
| 5. COVID-19-related burnout | - | −0.183 *** | −0.145 *** | −0.159 *** | −0.175 *** | ||||
| 6. Total social support | - | 0.862 *** | 0.853 *** | 0.892 *** | |||||
| 7. Family support | - | 0.554 *** | 0.680 *** | ||||||
| 8. Friend support | - | 0.669 *** | |||||||
| 9. Significant other support | - |
| Independent Variable | Adjusted Coefficient Beta | 95% CI for Beta | p-Value | Tolerance | VIF |
|---|---|---|---|---|---|
| Males vs. females | 1.882 | 1.227 to 2.538 | <0.001 | 0.923 | 1.083 |
| Age | 0.040 | 0.018 to 0.062 | <0.001 | 0.906 | 1.104 |
| MSc/PhD diploma | 0.274 | −0.138 to 0.686 | 0.193 | 0.967 | 1.034 |
| Chronic condition | 0.722 | 0.232 to 1.211 | 0.004 | 0.907 | 1.103 |
| Very poor/poor/moderate health status vs. good/very good | 0.614 | 0.035 to 1.263 | 0.064 | 0.941 | 1.062 |
| Non-COVID-19 infection | 0.699 | 0.233 to 1.164 | 0.003 | 0.928 | 1.077 |
| Booster dose | 2.014 | 1.346 to 2.682 | <0.001 | 0.964 | 1.037 |
| Side effects because of COVID-19 vaccination | −0.210 | −0.293 to −0.126 | <0.001 | 0.879 | 1.137 |
| COVID-19-related burnout | −0.878 | −1.102 to −0.653 | <0.001 | 0.884 | 1.131 |
| Total social support | 0.194 | 0.040 to 0.348 | 0.013 | 0.902 | 1.109 |
| b | SE | t | p | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||
| Direct effects | ||||||
| COVID-19-RB → SS | −0.2205 | 0.0404 | −5.46 | <0.0001 | −0.2998 | −0.1412 |
| COVID-19-RB → VW | −0.8922 | 0.1125 | −7.93 | <0.0001 | −1.1129 | −0.6715 |
| Indirect effect | ||||||
| COVID-19-RB → SS → VW | 0.0437 | 0.0223 | 2.33 | <0.05 | 0.0041 | 0.0922 |
| Total effect | −0.8485 | 0.1110 | -7.65 | <0.0001 | −1.0663 | −0.6307 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galanis, P.; Katsiroumpa, A.; Sourtzi, P.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Kaitelidou, D. Social Support Mediates the Relationship between COVID-19-Related Burnout and Booster Vaccination Willingness among Fully Vaccinated Nurses. Vaccines 2023, 11, 46. https://doi.org/10.3390/vaccines11010046
Galanis P, Katsiroumpa A, Sourtzi P, Siskou O, Konstantakopoulou O, Katsoulas T, Kaitelidou D. Social Support Mediates the Relationship between COVID-19-Related Burnout and Booster Vaccination Willingness among Fully Vaccinated Nurses. Vaccines. 2023; 11(1):46. https://doi.org/10.3390/vaccines11010046
Chicago/Turabian StyleGalanis, Petros, Aglaia Katsiroumpa, Panayota Sourtzi, Olga Siskou, Olympia Konstantakopoulou, Theodoros Katsoulas, and Daphne Kaitelidou. 2023. "Social Support Mediates the Relationship between COVID-19-Related Burnout and Booster Vaccination Willingness among Fully Vaccinated Nurses" Vaccines 11, no. 1: 46. https://doi.org/10.3390/vaccines11010046
APA StyleGalanis, P., Katsiroumpa, A., Sourtzi, P., Siskou, O., Konstantakopoulou, O., Katsoulas, T., & Kaitelidou, D. (2023). Social Support Mediates the Relationship between COVID-19-Related Burnout and Booster Vaccination Willingness among Fully Vaccinated Nurses. Vaccines, 11(1), 46. https://doi.org/10.3390/vaccines11010046








