COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome
Abstract
1. Introduction
2. Materials and Methods
2.1. Measures
2.2. Analyses
2.2.1. Measurement Models
2.2.2. Latent Profile Analyses
2.2.3. Predictors and Outcome of Profiles
2.3. Ethical Aspects
3. Results
3.1. Preliminary Analyses
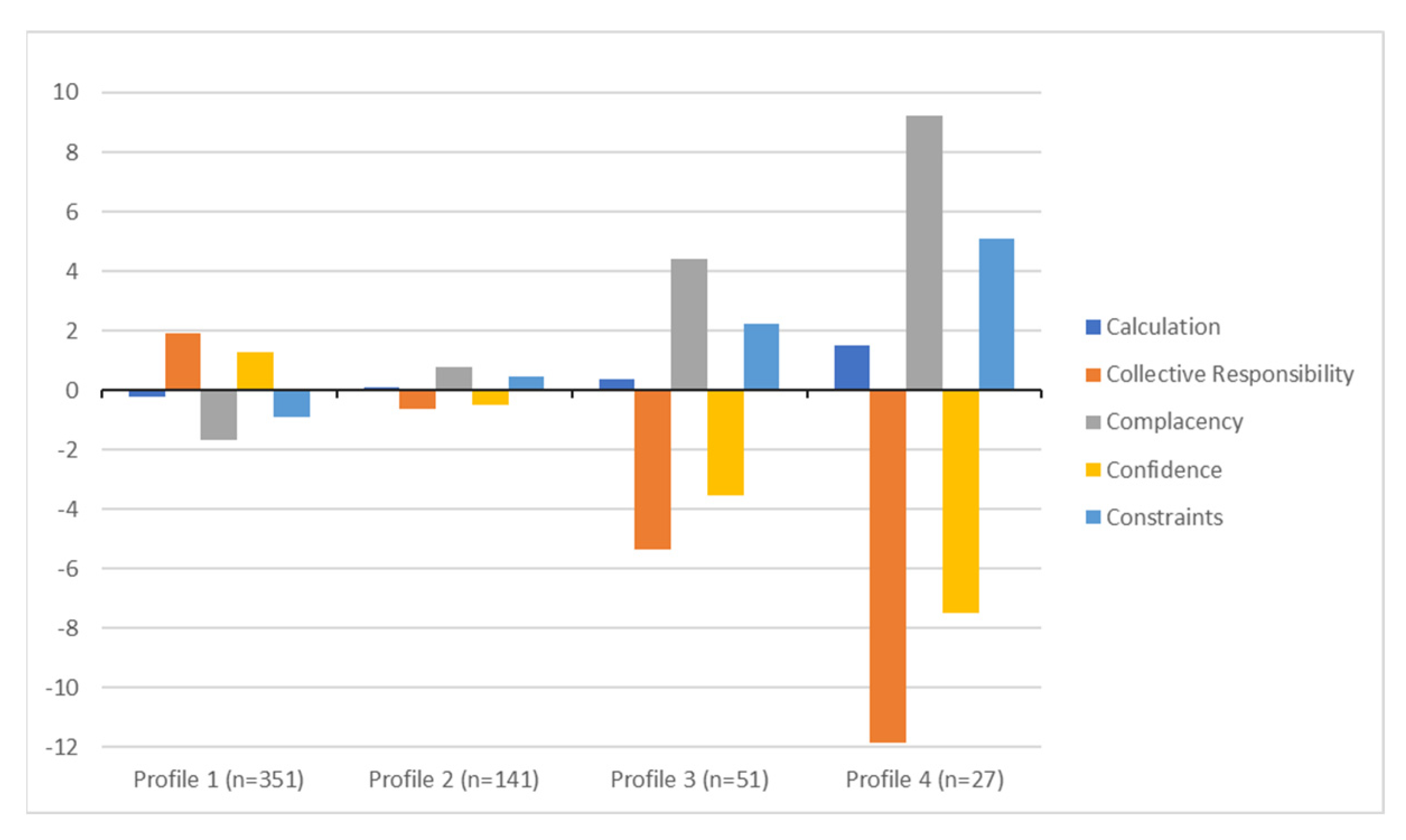
3.2. Latent Profile Analysis
3.3. Predictors and Profile Outcomes
4. Discussion
4.1. Implications
4.2. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. The Global Vaccine Action Plan 2011–2020: Review and Lessons Learned: Strategic Advisory Group of Experts on Immunization; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-World Effectiveness of COVID-19 Vaccines: A Literature Review and Meta-Analysis. Int. J. Infect. Dis. 2022, 114, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Katerelos, P.; Poufta, S.; Pavli, A.; Maragos, A.; Theodoridou, M. Attitudes toward Mandatory Occupational Vaccinations and Vaccination Coverage against Vaccine-Preventable Diseases of Health Care Workers in Primary Health Care Centers. Am. J. Infect. Control 2013, 41, 66–70. [Google Scholar] [CrossRef]
- Theodoridou, M. Professional and Ethical Responsibilities of Health-Care Workers in Regard to Vaccinations. Vaccine 2014, 32, 4866–4868. [Google Scholar] [CrossRef] [PubMed]
- Razai, M.S.; Chaudhry, U.A.; Doerholt, K.; Bauld, L.; Majeed, A. COVID-19 Vaccination Hesitancy. BMJ 2021, 373, n1138. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Hu, S.; Du, F.; Zang, S.; Xing, Y.; Qu, Z.; Zhang, X.; Lin, L.; Hou, Z. Mapping Global Acceptance and Uptake of COVID-19 Vaccination: A Systematic Review and Meta-Analysis. Commun. Med. 2022, 2, 113. [Google Scholar] [CrossRef] [PubMed]
- Desye, B. Prevalence and Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers: A Systematic Review. Front. Public Health 2022, 10, 941206. [Google Scholar] [CrossRef]
- World Health Organization. Global COVID-19 Vaccination Strategy in a Changing World: July 2022 Update. 2022. Available online: https://www.who.int/publications/m/item/global-covid-19-159vaccination-strategy-in-a-changing-world—july-2022-update (accessed on 21 January 2023).
- Abdelmoneim, S.A.; Sallam, M.; Hafez, D.M.; Elrewany, E.; Mousli, H.M.; Hammad, E.M.; Elkhadry, S.W.; Adam, M.F.; Ghobashy, A.A.; Naguib, M.; et al. COVID-19 Vaccine Booster Dose Acceptance: Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2022, 7, 298. [Google Scholar] [CrossRef]
- Dziedzic, A.; Issa, J.; Hussain, S.; Tanasiewicz, M.; Wojtyczka, R.; Kubina, R.; Konwinska, M.D.; Riad, A. COVID-19 Vaccine Booster Hesitancy (VBH) of Healthcare Professionals and Students in Poland: Cross-Sectional Survey-Based Study. Front. Public Health 2022, 10, 938067. [Google Scholar] [CrossRef]
- Bussink-Voorend, D.; Hautvast, J.L.A.; Vandeberg, L.; Visser, O.; Hulscher, M.E.J.L. A Systematic Literature Review to Clarify the Concept of Vaccine Hesitancy. Nat. Hum. Behav. 2022, 6, 1634–1648. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Böhm, R. Beyond Confidence: Development of a Measure Assessing the 5C Psychological Antecedents of Vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef]
- Jolley, D.; Douglas, K.M. Prevention Is Better than Cure: Addressing Anti-Vaccine Conspiracy Theories. J. Appl. Soc. Psychol. 2017, 47, 459–469. [Google Scholar] [CrossRef]
- Anakpo, G.; Mishi, S. Hesitancy of COVID-19 Vaccines: Rapid Systematic Review of the Measurement, Predictors, and Preventive Strategies. Hum. Vaccines Immunother. 2022, 18, 2074716. [Google Scholar] [CrossRef] [PubMed]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. [Google Scholar] [CrossRef] [PubMed]
- Al-Sanafi, M.; Sallam, M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines 2021, 9, 701. [Google Scholar] [CrossRef]
- Chen, Y.-L.; Lin, Y.-J.; Chang, Y.-P.; Chou, W.-J.; Yen, C.-F. Differences in the Protection Motivation Theory Constructs between People with Various Latent Classes of Motivation for Vaccination and Preventive Behaviors against COVID-19 in Taiwan. Int. J. Environ. Res. Public. Health 2021, 18, 7042. [Google Scholar] [CrossRef]
- Lee, C.H.; Sibley, C.G. Attitudes toward Vaccinations Are Becoming More Polarized in New Zealand: Findings from a Longitudinal Survey. EClinicalMedicine 2020, 23, 100387. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Neufeind, J.; Betsch, C.; Habersaat, K.B.; Eckardt, M.; Schmid, P.; Wichmann, O. Barriers and Drivers to Adult Vaccination among Family Physicians–Insights for Tailoring the Immunization Program in Germany. Vaccine 2020, 38, 4252–4262. [Google Scholar] [CrossRef]
- Leung, C.L.K.; Li, K.-K.; Wei, V.W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S.; Kwok, K.O. Profiling Vaccine Believers and Skeptics in Nurses: A Latent Profile Analysis. Int. J. Nurs. Stud. 2022, 126, 104142. [Google Scholar] [CrossRef] [PubMed]
- Kopsidas, I.; Tsopela, G.-C.; Maroudi-Manta, S.; Kourkouni, E.; Charalampopoulos, D.; Sirogianni, A.; Collins, M.E.; Lourida, A.; Kourlaba, G.; Zaoutis, T.E. Increasing Healthcare Workers’ Uptake of Seasonal Influenza Vaccination in a Tertiary-Care Pediatric Hospital in Greece with a Low-Cost, Tailor-Made, Multifaceted Strategy. Vaccine 2020, 38, 4609–4615. [Google Scholar] [CrossRef] [PubMed]
- Zhang, E.; Dai, Z.; Wang, C.; Hu, J.; Wang, S.; Zhang, L.; Fang, Q. Targeting COVID-19 Vaccine Hesitancy among Nurses in Shanghai: A Latent Profile Analysis. Front. Public Health 2022, 10, 953850. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.J.; Lee, B.; Nugent, K. COVID-19 Vaccination Hesitancy among Healthcare Workers-A Review. Vaccines 2022, 10, 948. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Leung, C.L.K.; Tang, A.; Chan, E.Y.Y.; Tsoi, M.T.F.; Wei, W.I.; McNeil, E.B.; Wong, S.Y.S. The Way Forward to Achieve High COVID-19 Vaccination and Revaccination Coverage in a City amid a Period of Tranquility. Front. Public Health 2022, 10, 935243. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, G.K.; Holding, A.; Perez, S.; Amsel, R.; Rosberger, Z. Validation of the Vaccine Conspiracy Beliefs Scale. Papillomavirus Res. 2016, 2, 167–172. [Google Scholar] [CrossRef]
- Brislin, R.W. Back-Translation for Cross-Cultural Research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Muthén, B.; Muthén, L. Mplus. In Handbook of Item Response Theory; CRC Press: Boca Raton, FL, USA, 2017; Volume 3, pp. 507–517. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Gillet, N.; Morin, A.J.S.; Choisay, F.; Fouquereau, E. A Person-Centered Representation of Basic Need Satisfaction Balance at Work. J. Pers. Psychol. 2019, 18, 113–128. [Google Scholar] [CrossRef]
- Hipp, J.R.; Bauer, D.J. Local Solutions in the Estimation of Growth Mixture Models. Psychol. Methods 2006, 11, 36. [Google Scholar] [CrossRef]
- Masyn, K.E. Latent Class Analysis and Finite Mixture Modeling. In The Oxford Handbook of Quantitative Methods: Statistical Analysis; Oxford Library of Psychology; Oxford University Press: New York, NY, USA, 2013; Volume 2, pp. 551–611. [Google Scholar]
- Marsh, H.W.; Lüdtke, O.; Trautwein, U.; Morin, A.J.S. Classical Latent Profile Analysis of Academic Self-Concept Dimensions: Synergy of Person- and Variable-Centered Approaches to Theoretical Models of Self-Concept. Struct. Equ. Model. 2009, 16, 191–225. [Google Scholar] [CrossRef]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Lanza, S.T.; Bray, B.C.; Collins, L.M. An Introduction to Latent Class and Latent Transition Analysis. In Handbook of Psychology: Research Methods in Psychology, 2nd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013; Volume 2, pp. 691–716. [Google Scholar]
- Morin, A.J.S.; Morizot, J.; Boudrias, J.-S.; Madore, I. A Multifoci Person-Centered Perspective on Workplace Affective Commitment: A Latent Profile/Factor Mixture Analysis. Organ. Res. Methods 2011, 14, 58–90. [Google Scholar] [CrossRef]
- Lo, Y.; Mendell, N.R.; Rubin, D.B. Testing the Number of Components in a Normal Mixture. Biometrika 2001, 88, 767–778. [Google Scholar] [CrossRef]
- Celeux, G.; Soromenho, G. An Entropy Criterion for Assessing the Number of Clusters in a Mixture Model. J. Classif. 1996, 13, 195–212. [Google Scholar] [CrossRef]
- Asparouhov, T.; Muthén, B. Auxiliary Variables in Mixture Modeling: Three-Step Approaches Using Mplus. Struct. Equ. Model. 2014, 21, 329–341. [Google Scholar] [CrossRef]
- Vermunt, J.K. Latent Class Modeling with Covariates: Two Improved Three-Step Approaches. Polit. Anal. 2017, 18, 450–469. [Google Scholar] [CrossRef]
- Smith, T.C. Vaccine Rejection and Hesitancy: A Review and Call to Action. Open Forum Infect. Dis. 2017, 4, ofx146. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Katsiroumpa, A.; Siskou, O.; Konstantakopoulou, O.; Katsoulas, T.; Mariolis-Sapsakos, T.; Kaitelidou, D. Predictors of Second COVID-19 Booster Dose or New COVID-19 Vaccine Hesitancy among Nurses: A Cross-Sectional Study. medRxiv 2022. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Intention of Healthcare Workers to Accept COVID-19 Vaccination and Related Factors: A Systematic Review and Meta-Analysis. Asian Pac. J. Trop. Med. 2021, 14, 543. [Google Scholar] [CrossRef]
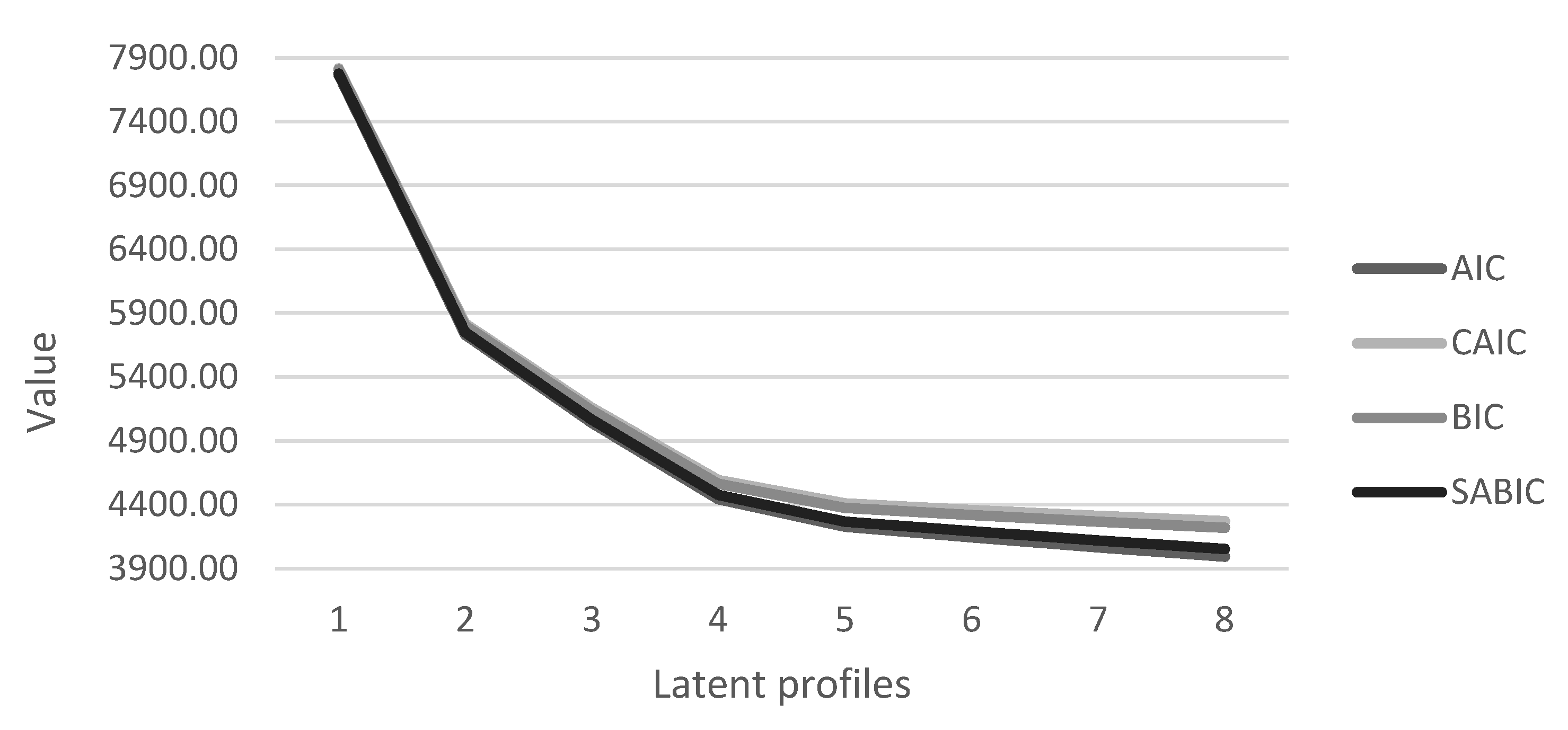
| Model | LL | #fp | Scaling | AIC | CAIC | BIC | SABIC | Entropy | aLMR | BLRT | AWE |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Profile | −3871.94 | 10 | 1.739 | 7763.88 | 7817.33 | 7807.33 | 7775.59 | 11,721.00 | |||
| 2 Profiles | −2849.95 | 16 | 1.775 | 5731.89 | 5817.42 | 5801.42 | 5750.63 | 0.989 | <0.001 | <0.001 | 8718.13 |
| 3 Profiles | −2497.97 | 22 | 2.194 | 5039.93 | 5157.53 | 5135.53 | 5065.69 | 0.972 | ns | <0.001 | 7725.30 |
| 4 Profiles | −2193.23 | 28 | 1.730 | 4442.46 | 4592.14 | 4564.14 | 4475.25 | 0.948 | <0.001 | <0.001 | 6874.21 |
| 5 Profiles | −2079.77 | 34 | 1.624 | 4227.55 | 4409.30 | 4375.30 | 4267.37 | 0.946 | <0.001 | <0.001 | 6596.95 |
| 6 Profiles | −2032.34 | 40 | 1.519 | 4144.68 | 4358.51 | 4318.51 | 4191.52 | 0.891 | <0.001 | <0.001 | 6517.76 |
| 7 Profiles | −1986.93 | 46 | 1.560 | 4065.87 | 4311.77 | 4265.77 | 4119.74 | 0.901 | ns | <0.001 | 6444.65 |
| 8 Profiles | −1944.86 | 52 | 1.634 | 3993.73 | 4271.70 | 4219.70 | 4054.62 | 0.899 | ns | <0.001 | 6381.55 |
| 1 vs. 4 | 2 vs. 4 | 3 vs. 4 | 2 vs. 1 | 3 vs. 1 | 3 vs. 2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | (S.E.) | OR | Coef. | (S.E.) | OR | Coef. | (S.E.) | OR | Coef. | (S.E.) | OR | Coef. | (S.E.) | OR | Coef. | (S.E.) | OR | |
| FLU (No vs. Yes) | −1.17 | 1.26 | 0.31 | −0.87 | 1.22 | 0.42 | 0.04 | 1.14 | 1.04 | 0.30 | 0.34 | 1.35 | −1.21 * | 0.61 | 3.36 | 0.91 | 0.53 | 2.48 |
| HBV (No vs. Yes) | 2.49 * | 1.01 | 12.05 | 2.00 * | 0.93 | 7.41 | 1.61 | 0.82 | 4.99 | −0.49 | 0.42 | 0.62 | −0.88 | 0.60 | 0.41 | −0.40 | 0.47 | 0.67 |
| SIER (No vs. Yes) | 0.84 | 0.99 | 2.32 | 0.49 | 0.94 | 1.62 | 1.11 | 0.85 | 3.04 | 0.80 * | 0.37 | 2.23 | 0.98 | 0.58 | 2.67 | 0.18 | 0.47 | 1.20 |
| DEATH (No vs. Yes) | 0.82 | 0.89 | 2.28 | 1.62 * | 0.82 | 5.07 | 1.80 * | 0.72 | 6.08 | −0.36 | 0.34 | 0.70 | 0.27 | 0.58 | 1.31 | 0.63 | 0.50 | 1.87 |
| VCBS | −6.90 ** | 0.75 | 0.00 | −3.73 * | 0.61 | 0.02 | −2.14 * | 0.54 | 0.12 | 3.17 * | 0.42 | 23.81 | 4.76 * | 0.53 | 116.96 | 1.59 ** | 0.29 | 4.91 |
| Probability (%) | S.E. | ||
|---|---|---|---|
| Profile 1: Believer (n = 351) | |||
| Intention to get vaccine: | No | 0.084 | 0.02 |
| Does not know | 0.112 | 0.02 | |
| Yes | 0.804 | 0.03 | |
| Profile 2: Middler (n = 141) | |||
| Intention to get vaccine: | No | 0.279 | 0.04 |
| Does not know | 0.237 | 0.04 | |
| Yes | 0.483 | 0.04 | |
| Profile 3: Hesitant (n = 51) | |||
| Intention to get vaccine: | No | 0.678 | 0.07 |
| Does not know | 0.211 | 0.06 | |
| Yes | 0.111 | 0.04 | |
| Profile 4: Rejector (n = 27) | |||
| Intention to get vaccine: | No | 1 | 0 |
| Does not know | 0 | 0 | |
| Yes | 0 | 0 | |
| Chi-Square | p-Value | df | |
|---|---|---|---|
| Overall test | 3365.89 | <0.001 | 6 |
| Profile 1 vs. 2 | 34.67 | <0.001 | 2 |
| Profile 1 vs. 3 | 182.81 | <0.001 | 2 |
| Profile 1 vs. 4 | 2725.76 | <0.001 | 2 |
| Profile 2 vs. 3 | 41.63 | <0.001 | 2 |
| Profile 2 vs. 4 | 333.00 | <0.001 | 2 |
| Profile 3 vs. 4 | 24.42 | <0.001 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Portoghese, I.; Siddi, M.; Chessa, L.; Costanzo, G.; Garcia-Larsen, V.; Perra, A.; Littera, R.; Sambugaro, G.; Giacco, S.D.; Campagna, M.; et al. COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome. Vaccines 2023, 11, 273. https://doi.org/10.3390/vaccines11020273
Portoghese I, Siddi M, Chessa L, Costanzo G, Garcia-Larsen V, Perra A, Littera R, Sambugaro G, Giacco SD, Campagna M, et al. COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome. Vaccines. 2023; 11(2):273. https://doi.org/10.3390/vaccines11020273
Chicago/Turabian StylePortoghese, Igor, Melinda Siddi, Luchino Chessa, Giulia Costanzo, Vanessa Garcia-Larsen, Andrea Perra, Roberto Littera, Giada Sambugaro, Stefano Del Giacco, Marcello Campagna, and et al. 2023. "COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome" Vaccines 11, no. 2: 273. https://doi.org/10.3390/vaccines11020273
APA StylePortoghese, I., Siddi, M., Chessa, L., Costanzo, G., Garcia-Larsen, V., Perra, A., Littera, R., Sambugaro, G., Giacco, S. D., Campagna, M., & Firinu, D. (2023). COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome. Vaccines, 11(2), 273. https://doi.org/10.3390/vaccines11020273







