Shoulder Injury Related to Vaccine Administration (SIRVA) Is Real: A Case Report
Abstract
:1. Introduction
- Adhesive capsulitis (frozen shoulder)
- Arthralgia
- Axillary nerve palsy
- Neuritis
- Osteonecrosis of the humeral head
- Radial nerve palsy
- Rotator cuff tears
- Rotator cuff tendinopathy
- Shoulder impingement syndrome
- Subdeltoid/subacromial bursitis
- Synovitis
2. Case Presentation
2.1. Patient Details
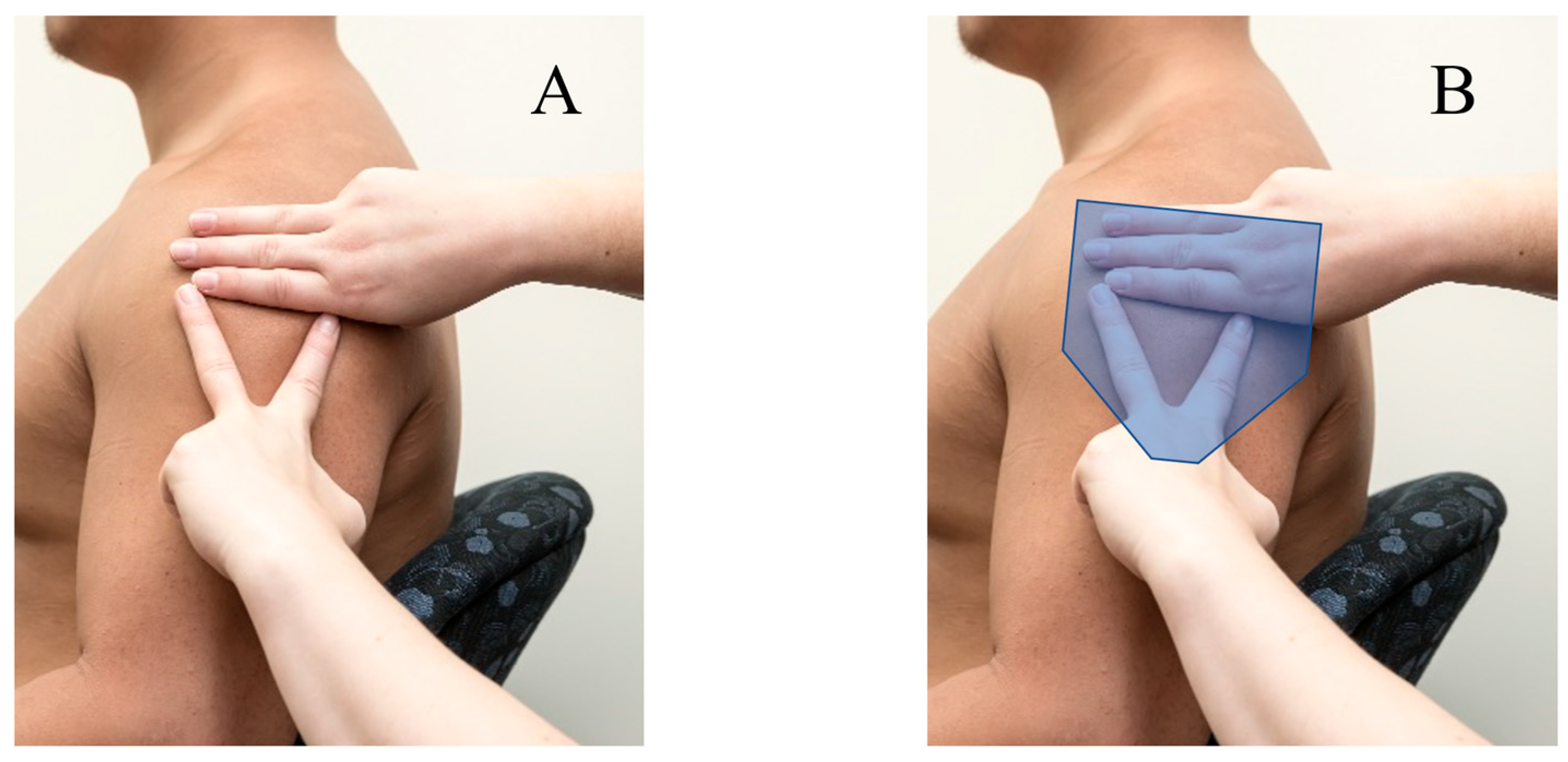
2.2. Clinical Findings
2.3. Timeline
2.4. Diagnostic Assessment
2.5. Differential Diagnosis
2.6. Treatment
2.7. Outcome and Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Pre (20 Months Post-Vaccination) | Post (26 Months Post-Vaccination) | |||||
|---|---|---|---|---|---|---|
| Right | Left | % Difference | Right | Left | % Difference | |
| AROM | ||||||
| Flexion | 180° | 80° | −55.5% | 180° | 140° | −22.2% |
| Abduction | 120° | 55° | −54.2% | 120° | 90° | −25.0% |
| Internal rotation (HBB) | T7 | T9 | NA | T7 | T9 | NA |
| External rotation (HBH) | T3 | TMJ | NA | T3 | C3 | NA |
| External rotation at 90° shoulder abduction | 100° | 0° | −100.0% | 100° | 30° | −70% |
| Dynamometry | ||||||
| Infraspinatus/ teres minor | 7.8 kg | 4.4 kg | −43.6% | 8 kg | 6.8 kg | −15.0% |
| Subscapularis | 6.8 kg | 4.4 kg | −35.7% | 10.2 kg | 9.7 kg | −5.0% |
| Biceps brachii | 17 kg | 15 kg | −11.8% | 16 kg | 14 kg | −12.5% |
| Supraspinatus | 7 kg | 4.8 kg | −31.5% | 7.5 kg | 5.2 kg | −30.7% |
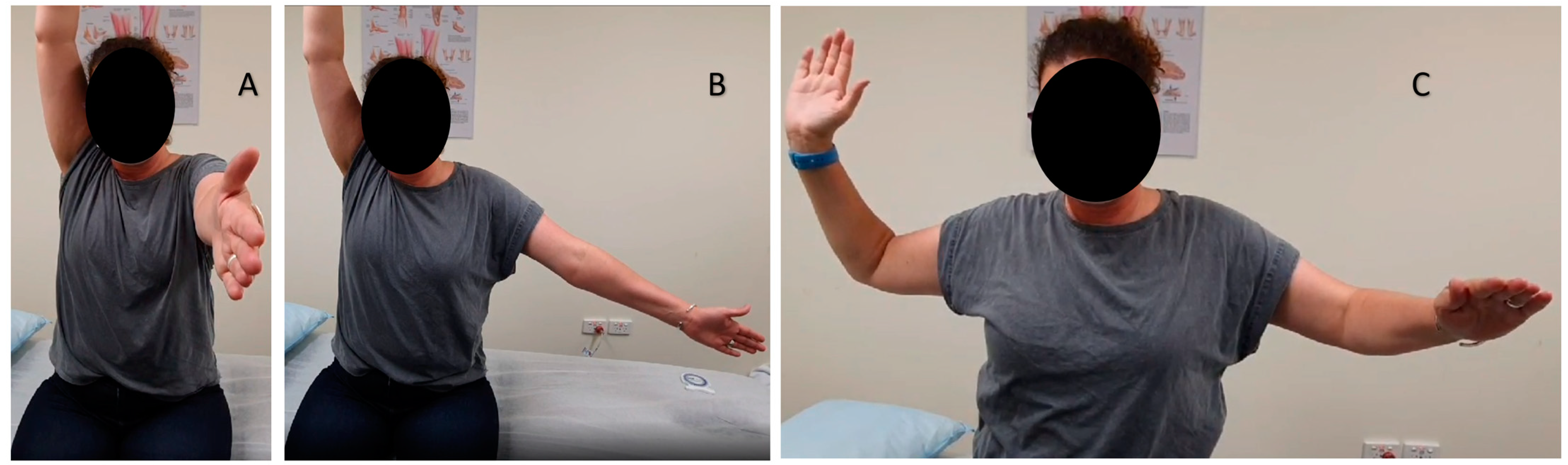
| Supine shoulder flexion stretch |  |
| Supine external shoulder rotation stretch |  |
| Shoulder flexion stretch at wall | 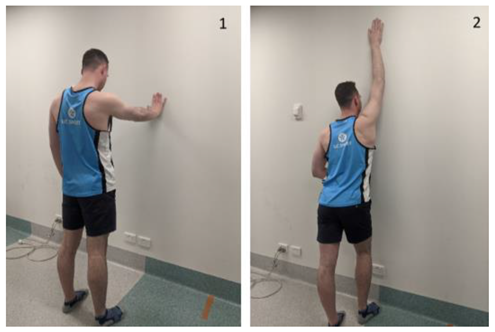 |
| Bilateral supine active assisted range-of-motion external rotation of the shoulder with cane in neutral |  |
| Bilateral supine active assisted range-of-motion shoulder abduction with cane |  |
| Pectoral standing stretch with external rotation of the shoulder | 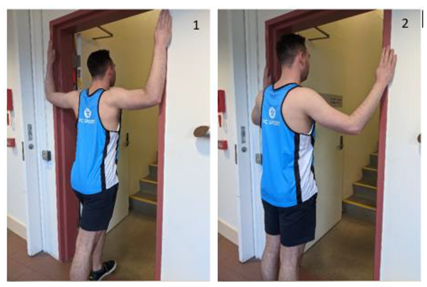 |
References
- Mackenzie, L.; Bousie, J.; Newman, P.; Bushell, M.J. Shoulder Injuries Related to Vaccine Administration. Aust. Pharm. 2022, 40, 60–68. [Google Scholar]
- Lewis, G. Shoulder Injury Related to Vaccine Administration (SIRVA); Murdoch Children’s Research Institute: Melbourne, Australia, 2019. [Google Scholar]
- Cross, G.B.; Moghaddas, J.; Buttery, J.; Ayoub, S.; Korman, T.M. Don’t aim too high: Avoiding shoulder injury related to vaccine administration. Aust. Fam. Physician 2016, 45, 303–306. [Google Scholar] [PubMed]
- Avoiding shoulder injury related to vaccine administration. In Australian Immunisation Handbook; Australian Government, Department of Health: Canberra, Australia, 2021.
- Prevent Shoulder Injuries during COVID-19 Vaccinations. Institute for Same Medication Practices [Internet]. 17 December 2020. Available online: https://www.ismp.org/resources/prevent-shoulder-injuries-during-covid-19-vaccinations (accessed on 10 September 2021).
- Bancsi, A.; Houle, S.K.D.; Grindrod, K.A. Getting it in the right spot: Shoulder injury related to vaccine administration (SIRVA) and other injection site events. Can. Pharm. J. 2018, 151, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Kakati, A.; Bhat, D.; Devi, B.; Shukla, D. Injection nerve palsy. J. Neurosci. Rural. Pract. 2013, 4, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Hibbs, B.F.; Ng, C.S.; Museru, O.; Moro, P.L.; Marquez, P.; Woo, E.J.; Cano, M.V.; Shimabukuro, T.T. Reports of atypical shoulder pain and dysfunction following inactivated influenza vaccine, Vaccine Adverse Event Reporting System (VAERS), 2010–2017. Vaccine 2020, 38, 1137–1143. [Google Scholar] [CrossRef] [PubMed]
- Degreef, I.; Debeer, P. Post-vaccination frozen shoulder syndrome. Report of 3 cases. Acta Chir. Belg. 2012, 112, 447–449. [Google Scholar] [CrossRef] [PubMed]
- Saleh, Z.; Faruqui, S.; Foad, A. Onset of frozen shoulder following pneumococcal and influenza vaccinations. J. Chiropr. Med. 2015, 14, 285–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pandey, V.; Madi, S. Clinical Guidelines in the Management of Frozen Shoulder: An Update! Indian J. Orthop. 2021, 55, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Hand, C.; Clipsham, K.; Rees, J.; Carr, A. Long-term outcome of frozen shoulder. J. Shoulder Elb. Surg. 2008, 17, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Macomb, C.V.; Evans, M.O.; Dockstater, J.E.; Montgomery, J.R.; Beakes, D.E. Treating SIRVA early with corticosteroid injections: A case series. Mil. Med. 2020, 185, e298–e300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Technical Advisory Group on Immunisation. Australian Immunisation Handbook; Australian Government, Department of Health: Canberra, Australia, 2018. [Google Scholar]
- Bancsi, A.; Houle, S.K.D.; Grindrod, K.A. Shoulder injury related to vaccine administration and other injection site events. Can. Fam. Physician 2019, 65, 40–42. [Google Scholar]
- Cocoman, A.; Barron, C. A sure shot. World Ir. Nurs. 2013, 21, 48–49. [Google Scholar]
- Altman, G.; Buchsel, P.; Coxon, V. Delmar’s Fundamental & Advanced Nursing Skills, 3rd ed.; Thomson/Delmar Learning: Washington, UT, USA, 2004. [Google Scholar]
- Fujimoto, E. The problem of using deltoid muscle for intramuscular injection. Aino J. 2007, 6, 49–53. [Google Scholar]
- Cook, I. Best vaccination practice and medically attended injection site events following deltoid intramuscular injection. Hum. Vaccines Immunother. 2015, 11, 1184–1191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroger, A.; Bahta, L.; Hunter, P. General Best Practice Guidelines for Immunization [Internet]. 10 February 2023. Best Practices Guidance of the Advisory Committee on Immunization Practices (ACIP). Available online: https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/index.html (accessed on 15 September 2022).
- Petousis-Harris, H. Vaccine injection technique and reactogenicity- Evidence for Practice. Vaccine 2008, 26, 6299–6304. [Google Scholar] [CrossRef]
- McGarvey, A.; Hooper, C. The Deltoid Intramuscular Injection Site in the Adult—Current Practice Among General Practitioners and Practice Nurses. Ir. Med. J. 2005, 98, 105–107. [Google Scholar] [PubMed]
- Mackenzie, L.; Bousie, J.; Newman, P.; Waghorn, J.; Cunningham, J.; Bushell, M.-J. Healthcare Practitioners Knowledge of Shoulder Injury Related to Vaccine Administration (SIRVA). Vaccines 2022, 10, 1991. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mackenzie, L.J.; Bousie, J.A.; Bushell, M.-J.A.; Newman, P. Shoulder Injury Related to Vaccine Administration (SIRVA) Is Real: A Case Report. Vaccines 2023, 11, 1164. https://doi.org/10.3390/vaccines11071164
Mackenzie LJ, Bousie JA, Bushell M-JA, Newman P. Shoulder Injury Related to Vaccine Administration (SIRVA) Is Real: A Case Report. Vaccines. 2023; 11(7):1164. https://doi.org/10.3390/vaccines11071164
Chicago/Turabian StyleMackenzie, Laura Jane, Jaquelin Anne Bousie, Mary-Jessimine Ann Bushell, and Phillip Newman. 2023. "Shoulder Injury Related to Vaccine Administration (SIRVA) Is Real: A Case Report" Vaccines 11, no. 7: 1164. https://doi.org/10.3390/vaccines11071164
APA StyleMackenzie, L. J., Bousie, J. A., Bushell, M.-J. A., & Newman, P. (2023). Shoulder Injury Related to Vaccine Administration (SIRVA) Is Real: A Case Report. Vaccines, 11(7), 1164. https://doi.org/10.3390/vaccines11071164








