Toxicity and Efficacy Evaluation of Soluble Recombinant Ricin Vaccine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals, Reagents, Cells, and Animals
2.2. In Silico Analysis of Protein Structure
2.3. Construction and Soluble Expression of Truncated R51
2.4. Protein Purification
2.5. Toxicity Assessment
2.6. Efficacy Assessment
2.7. Antibody Titer and TNA
2.8. Statistical Analysis
3. Results
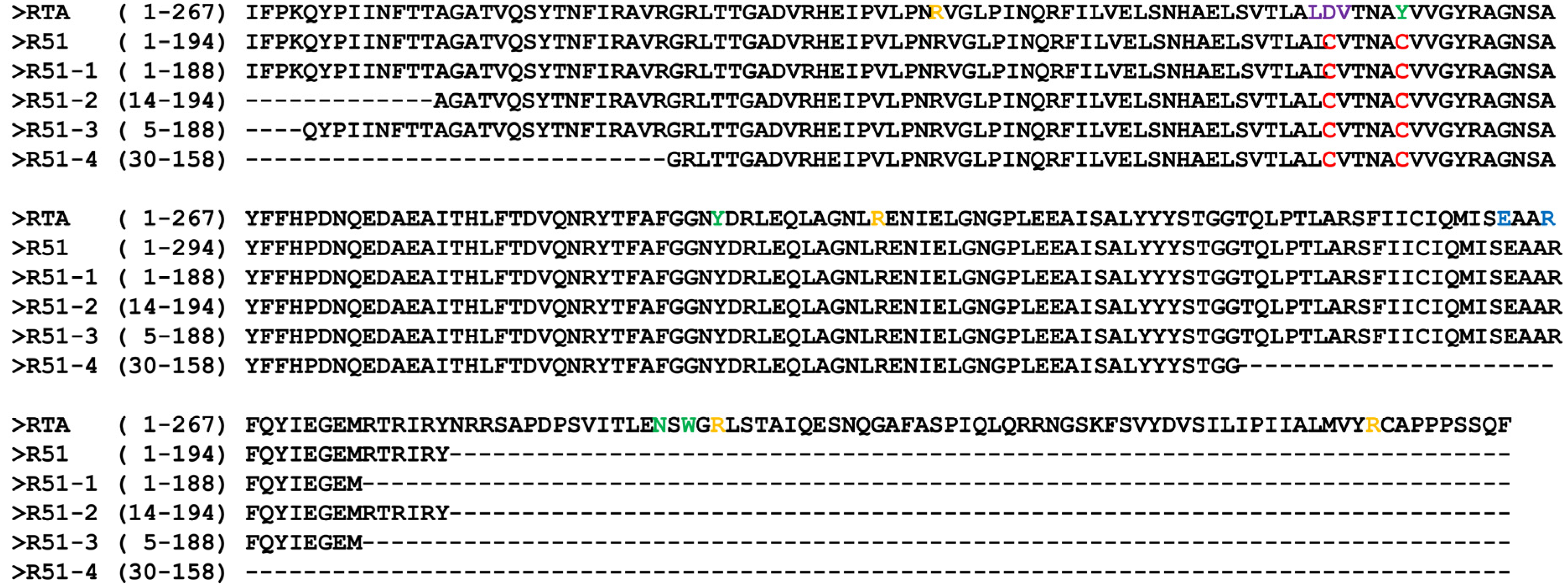
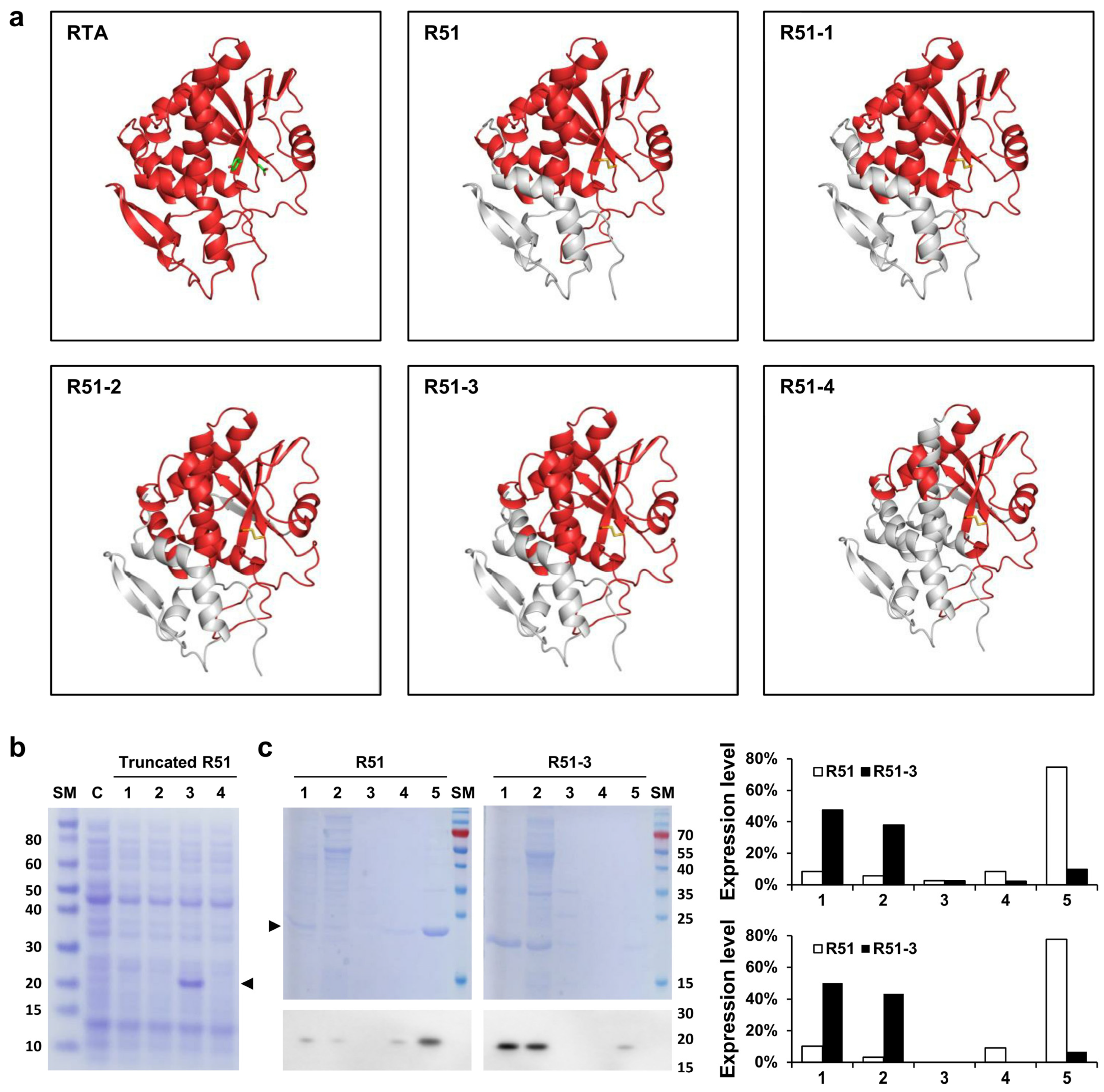
3.1. Structure and Expression of the Truncated R51
3.2. Weight Changes in Mice after Single and Repeated Doses of R51-3
3.3. Pilot Toxicity Assessment
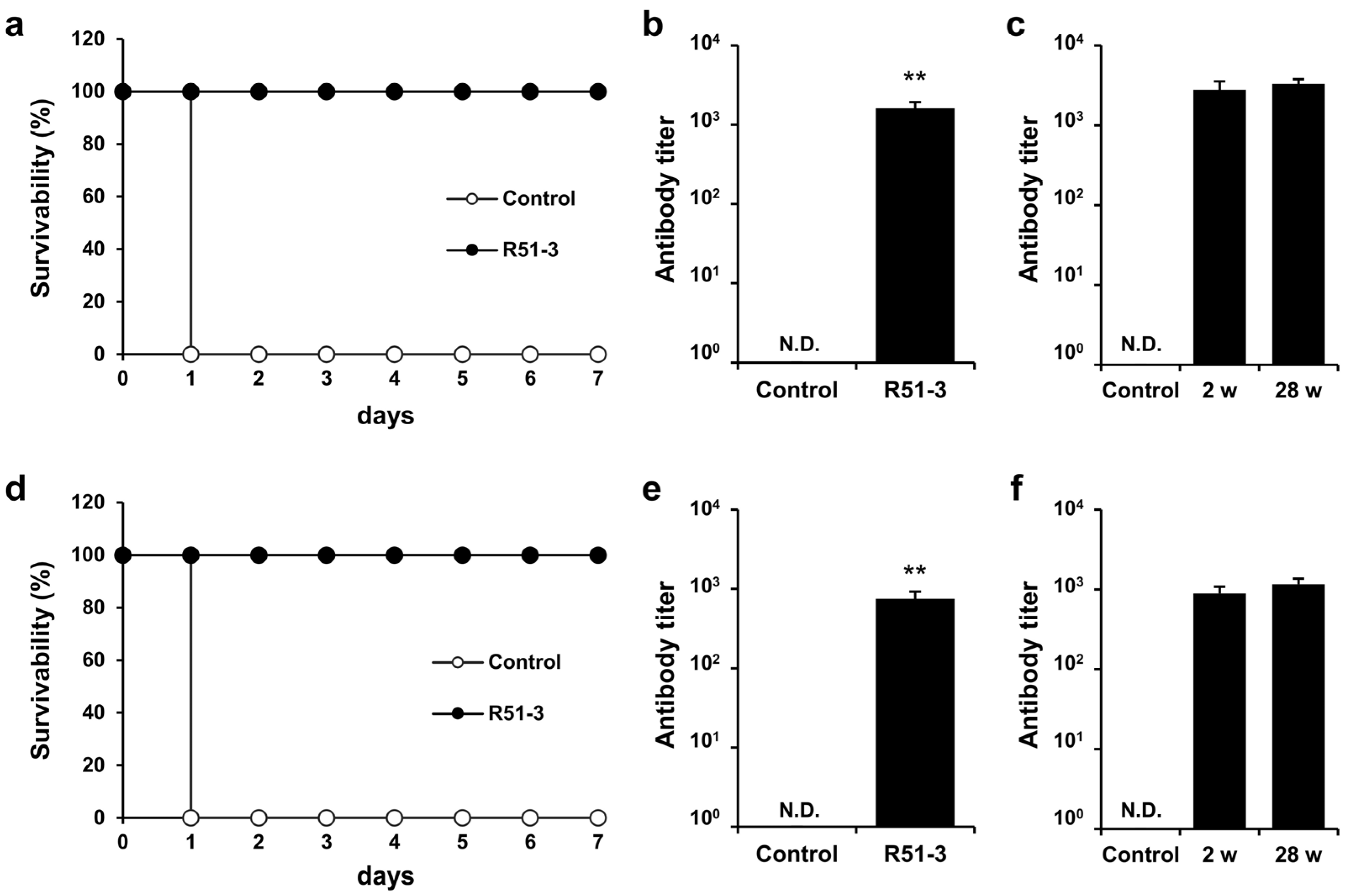
3.4. Ricin Defense Capability, Antibody Titer, and Generation of Neutralizing Antibodies after Ricin Immunization in Mice
3.5. Vaccine Efficacy in Rabbits and Monkeys
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Polito, L.; Bortolotti, M.; Battelli, M.G.; Calafato, G.; Bolognesi, A. Ricin: An ancient story for a timeless plant toxin. Toxins 2019, 11, 324. [Google Scholar] [CrossRef]
- Bolognesi, A.; Bortolotti, M.; Maiello, S.; Battelli, M.G.; Polito, L. Ribosome-inactivating proteins from plants: A historical overview. Molecules 2016, 21, 1627. [Google Scholar] [CrossRef]
- Lord, J.M.; Roberts, L.M.; Robertus, J.D. Ricin: Structure, mode of action, and some current applications. FASEB J. 1994, 8, 201–208. [Google Scholar] [CrossRef]
- Endo, Y.; Tsurugi, K. RNA N-glycosidase activity of ricin A-chain. Mechanism of action of the toxic lectin ricin on eukaryotic ribosomes. J. Biol. Chem. 1987, 262, 8128–8130. [Google Scholar] [CrossRef]
- Lord, M.J.; Jolliffe, N.A.; Marsden, C.J.; Pateman, C.S.; Smith, D.C.; Spooner, R.A.; Watson, P.D.; Roberts, L.M. Ricin: Mechanisms of cytotoxicity. Toxicol. Rev. 2003, 22, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Bradberry, S.M.; Dickers, K.J.; Rice, P.; Griffiths, G.D.; Vale, J.A. Ricin poisoning. Toxicol. Rev. 2003, 22, 65–70. [Google Scholar] [CrossRef]
- Sapoznikov, A.; Rosner, A.; Falach, R.; Gal, Y.; Aftalion, M.; Evgy, Y.; Israeli, O.; Sabo, T.; Kronman, C. Intramuscular ricin poisoning of mice leads to widespread damage in the heart, spleen, and bone marrow. Toxins 2019, 11, 344. [Google Scholar] [CrossRef]
- Franz, D.R.; Jaax, N.K. Chapter 32: Ricin toxin. In Textbook of Military Medicine; Office of the Surgeon General, Department of the Army: Washington, DC, USA, 1997; pp. 631–642. [Google Scholar]
- Grela, P.; Szajwaj, M.; Horbowicz-Drożdżal, P.; Tchórzewski, M. How Ricin Damages the Ribosome. Toxins 2019, 11, 241. [Google Scholar] [CrossRef]
- Maracci, C.; Rodnina, M.V. Review: Translational GTPases. Biopolymers 2016, 105, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Olson, M.A.; Cuff, L. Free energy determinants of binding the rRNA substrate and small ligands to ricin A-chain. Biophys J. 1999, 76, 28–39. [Google Scholar] [CrossRef]
- Monzingo, A.F.; Robertus, J.D. X-ray analysis of substrate analogs in the ricin A-chain active site. J. Mol. Biol. 1992, 227, 1136–1145. [Google Scholar] [CrossRef] [PubMed]
- Ready, M.P.; Kim, Y.; Robertus, J.D. Site-directed mutagenesis of ricin A-chain and implications for the mechanism of action. Proteins 1991, 10, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Robertus, J.D. Analysis of several key active site residues of ricin A chain by mutagenesis and X-ray crystallography. Protein Eng. 1992, 5, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Frankel, A.; Welsh, P.; Richardson, J.; Robertus, J.D. Role of arginine 180 and glutamic acid 177 of ricin toxin A chain in enzymatic inactivation of ribosomes. Mol. Cell. Biol. 1990, 10, 6257–6263. [Google Scholar] [PubMed]
- Vitetta, E.S.; Thorpe, P.E.; Uhr, J.W. Immunotoxins: Magic bullets or misguided missiles. Trends Pharmacol. Sci. 1993, 14, 148–154. [Google Scholar] [CrossRef]
- Lindstrom, A.L.; Erlandsen, S.L.; Kersey, J.H.; Pennell, C.A. An in vitro model for toxin-mediated vascular leak syndrome: Ricin toxin A chain increases the permeability of human endothelial cell monolayers. Blood 1997, 90, 2323–2334. [Google Scholar] [CrossRef]
- Baluna, R.; Coleman, E.; Jones, C.; Ghetie, V.; Vitetta, E.S. The effect of a monoclonal antibody coupled to ricin A chain-derived peptides on endothelial cells in vitro: Insights into toxin-mediated vascular damage. Exp. Cell Res. 2000, 258, 417–424. [Google Scholar] [CrossRef]
- Griffiths, G.D.; Phillips, G.J.; Holley, J. Inhalation toxicology of ricin preparations: Animal models, prophylactic and therapeutic approaches to protection. Inhal. Toxicol. 2007, 19, 873–887. [Google Scholar] [CrossRef]
- Baluna, R.; Rizo, J.; Gordon, B.E.; Ghetie, V.; Vitetta, E.S. Evidence for a structural motif in toxins and interleukin-2 that may be responsible for binding to endothelial cells and initiating vascular leak syndrome. Proc. Natl. Acad. Sci. USA 1999, 96, 3957–3962. [Google Scholar] [CrossRef]
- Griffiths, G.D.; Phillips, G.J.; Bailey, S.C. Comparison of the quality of protection elicited by toxoid and peptide liposomal vaccine formulations against ricin as assessed by markers of inflammation. Vaccine 1999, 17, 2562–2568. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Firan, A.; Fulmer, J.R.; Ruback, S.L.; Ghetie, V.; Vitetta, E.S. A novel recombinant vaccine which protects mice against ricin intoxication. Vaccine 2002, 20, 3422–3427. [Google Scholar] [CrossRef] [PubMed]
- Olson, M.A.; Carra, J.H.; Roxas-Duncan, V.; Wannemacher, R.W.; Smith, L.A.; Millard, C.B. Finding a new vaccine in the ricin protein fold. Protein Eng. Des. Sel. 2004, 17, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Carra, J.H.; Wannemacher, R.W.; Tammariello, R.F.; Lindsey, C.Y.; Dinterman, R.E.; Schokman, R.D.; Smith, L.A. Improved formulation of a recombinant ricin A-chain vaccine increases its stability and effective antigenicity. Vaccine 2007, 25, 4149–4158. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Yang, H.; Kang, L.; Gao, S.; Xin, W.; Yao, W.; Zhuang, X.; Ji, B.; Wang, J. Strong protection against ricin challenge induced by a novel modified ricin A-chain protein in mouse model. Hum. Vaccin. Immunother. 2015, 11, 1779–1787. [Google Scholar] [CrossRef] [PubMed]
- McLain, D.E.; Horn, T.L.; Detrisac, C.J.; Lindsey, C.Y.; Smith, L.A. Progress in biological threat agent vaccine development: A repeat-dose toxicity study of a recombinant ricin toxin A-chain (rRTA) 1-33/44-198 vaccine (RVEc) in male and female New Zealand white rabbits. Int. J. Toxicol. 2011, 30, 143–152. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Richardson, J.A.; Pincus, S.; Schindler, J.; Vitetta, E.S. Preclinical toxicity and efficacy testing of RiVax, a recombinant protein vaccine against ricin. Vaccine 2005, 23, 4775–4784. [Google Scholar] [CrossRef] [PubMed]
- Pittman, P.R.; Reisler, R.B.; Lindsey, C.Y.; Güereña, F.; Rivard, R.; Clizbe, D.P.; Chambers, M.; Norris, S.; Smith, L.A. Safety and immunogenicity of ricin vaccine, RVEc™, in a Phase 1 clinical trial. Vaccine 2015, 33, 7299–7306. [Google Scholar] [CrossRef]
- Vitetta, E.S.; Smallshaw, J.E.; Coleman, E.; Jafri, H.; Foster, C.; Munford, R.; Schindler, J. A pilot clinical trial of a recombinant ricin vaccine in normal humans. Proc. Natl. Acad. Sci. USA 2006, 103, 2268–2673. [Google Scholar] [CrossRef]
- Vitetta, E.S.; Smallshaw, J.E.; Schindler, J. Pilot phase IB clinical trial of an alhydrogel-adsorbed recombinant ricin vaccine. Clin. Vaccine Immunol. 2012, 19, 1697–1699. [Google Scholar] [CrossRef] [PubMed]
- Rasetti-Escargueil, C.; Avril, A. Medical Countermeasures against Ricin Intoxication. Toxins 2023, 15, 100. [Google Scholar] [CrossRef]
- Yun, H.; Joe, H.; Song, D.; Yu, C.; Song, Y.; Hur, G. Development of non-toxic recombinant ricin vaccine and evaluation of vaccine efficacy. J. Korea Inst. Mil. Sci. Technol. 2024, 27, 304–310. [Google Scholar] [CrossRef]
- Upadhyay, V.; Singh, A.; Jha, D.; Singh, A.; Panda, A.K. Recovery of bioactive protein from bacterial inclusion bodies using trifluoroethanol as solubilization agent. Microb. Cell Fact. 2016, 15, 100. [Google Scholar] [CrossRef]
- Schneider, C.A.; Rasband, W.S.; Eliceiri, K.W. NIH Image to ImageJ: 25 years of image analysis. Nat. Methods 2012, 9, 671–675. [Google Scholar] [CrossRef]
- Woo, B.H.; Lee, J.T.; Lee, K.C. Purification of Sepharose-unbinding ricin from castor beans (Ricinus communis) by hydroxyapatite chromatography. Protein Expr. Purif. 1998, 13, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Rungsiwongse, J.; Ratanabanangkoon, K. Development of an ELISA to assess the potency of horse therapeutic antivenom against Thai cobra venom. J. Immunol. Methods 1991, 136, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, C.Y.; Pace-Templeton, J.G.; Millard, C.B.; Wannemacher, R.W.; Hewetson, J.F. Validation of ELISA for the determination of anti-ricin immunoglobulin G concentration in mouse sera. Biologicals 2006, 34, 33–41. [Google Scholar] [CrossRef]
- Simon, S.; Worbs, S.; Avondet, M.A.; Tracz, D.M.; Dano, J.; Schmidt, L.; Volland, H.; Dorner, B.G.; Corbett, C.R. Recommended Immunological Assays to Screen for Ricin-Containing Samples. Toxins 2015, 7, 4967–4986. [Google Scholar] [CrossRef]
- Prigent, J.; Panigai, L.; Lamourette, P.; Sauvaire, D.; Devilliers, K.; Plaisance, M.; Volland, H.; Créminon, C.; Simon, S. Neutralising antibodies against ricin toxin. PLoS ONE 2011, 6, e20166. [Google Scholar] [CrossRef] [PubMed]
- Solanki, A.K.; Bhatia, B.; Kaushik, H.; Deshmukh, S.K.; Dixit, A.; Garg, L.C. Clostridium perfringens beta toxin DNA prime-protein boost elicits enhanced protective immune response in mice. Appl. Microbiol. Biotechnol. 2017, 101, 5699–5708. [Google Scholar] [CrossRef]
- Hebditch, M.; Carballo-Amador, M.A.; Charonis, S.; Curtis, R.; Warwicker, J. Protein-Sol: A web tool for predicting protein solubility from sequence. Bioinformatics 2017, 33, 3098–3100. [Google Scholar] [CrossRef]
- McHugh, C.A.; Tammariello, R.F.; Millard, C.B.; Carra, J.H. Improved stability of a protein vaccine through elimination of a partially unfolded state. Protein Sci. 2004, 13, 2736–2743. [Google Scholar] [CrossRef]
- O’Hara, J.M.; Neal, L.M.; McCarthy, E.A.; Kasten-Jolly, J.A.; Brey, R.N.; Mantis, N.J. Folding domains within the ricin toxin A subunit as targets of protective antibodies. Vaccine 2010, 28, 7035–7046. [Google Scholar] [CrossRef]
- Castelletti, D.; Fracasso, G.; Righetti, S.; Tridente, G.; Schnell, R.; Engert, A.; Colombatti, M. A dominant linear B-cell epitope of ricin A-chain is the target of a neutralizing antibody response in Hodgkin’s lymphoma patients treated with an anti-CD25 immunotoxin. Clin. Exp. Immunol. 2004, 136, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Tommasi, M.; Castelletti, D.; Pasti, M.; Fracasso, G.; Lorenzetti, I.; Sartoris, S.; Pera, C.; Ferrara, G.B.; Tridente, G.; Colombatti, M. Identification of ricin A-chain HLA class II-restricted epitopes by human T-cell clones. Clin. Exp. Immunol. 2001, 125, 391–400. [Google Scholar] [CrossRef]
- Yang, H.; Pan, W.; Chen, G.; Huang, E.; Lu, Q.; Chen, Y.; Chen, Y.; Yang, Z.; Wen, L.; Zhang, S.; et al. Preclinical toxicity and immunogenicity of a COVID-19 vaccine (ZF2001) in cynomolgus monkeys. Vaccines 2022, 10, 2080. [Google Scholar] [CrossRef]
- Zhao, Y.; He, Z.; Wang, Z.; He, Y.; Zhao, X.; Liang, H.; Guo, Y.; Wang, Y.; Zhang, X.; Zhu, H.; et al. Repeat-dose toxicity of candidate Omicron COVID-19 vaccine in Sprague-Dawley rats. COVID 2023, 3, 51–64. [Google Scholar] [CrossRef]
- Song, Y.E.; Tan, H.; Liu, K.J.; Zhang, Y.Z.; Liu, Y.; Lu, C.R.; Yu, D.L.; Tu, J.; Cui, C.Y. Effect of fluoride exposure on bone metabolism indicators ALP, BALP, and BGP. Environ. Health Prev. Med. 2011, 16, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Hata, A.; Fujitani, N.; Takeshita, M.; Tanaka, C.; Matsuda, N.; Takaishi, M.; Shimokawa Miyama, T.; Hoshi, F. Comparison of regression for blood ALP levels using methods of the Japan Society of Clinical Chemistry and the International Federation of Clinical Chemistry and Laboratory Medicine in bovine, canine, feline, and human testing. PLoS ONE 2021, 16, e0253396. [Google Scholar] [CrossRef]
- Bhaskaran, M.; Didier, P.J.; Sivasubramani, S.K.; Doyle, L.A.; Holley, J.; Roy, C.J. Pathology of lethal and sublethal doses of aerosolized ricin in rhesus macaques. Toxicol. Pathol. 2014, 42, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Roy, C.J.; Brey, R.N.; Mantis, N.J.; Mapes, K.; Pop, I.V.; Pop, L.M.; Ruback, S.; Killeen, S.Z.; Doyle-Meyers, L.; Vinet-Oliphant, H.S.; et al. Thermostable ricin vaccine protects rhesus macaques against aerosolized ricin: Epitope-specific neutralizing antibodies correlate with protection. Proc. Natl. Acad. Sci. USA 2015, 112, 3782–3787. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Li, C.; Shi, B.; Han, H.; Liu, Y.; Tan, L.; Wang, K.; Yan, F.; He, W.; Li, B.; et al. Purified immunoglobulin F(ab’)2 could protect mice and rhesus monkeys from lethal ricin intoxication. Zoonoses 2023, 3, 19. [Google Scholar] [CrossRef]
- Brown, P.C.; Wange, R.L. Considerations regarding the use of nonhuman primates in assessing safety endpoints for pharmaceuticals. Regul. Toxicol. Pharmacol. 2023, 143, 105449. [Google Scholar] [CrossRef] [PubMed]
- Smallshaw, J.E.; Richardson, J.A.; Vitetta, E.S. RiVax, a recombinant ricin subunit vaccine, protects mice against ricin delivered by gavage or aerosol. Vaccine 2007, 25, 7459–7469. [Google Scholar] [CrossRef] [PubMed]



| Protein | Predicted Scaled Solubility | pI |
|---|---|---|
| RTA | 0.367 | 6.040 |
| R51 | 0.380 | 6.380 |
| R51-1 | 0.417 | 5.410 |
| R51-2 | 0.423 | 6.010 |
| R51-3 | 0.476 | 5.190 |
| R51-4 | 0.510 | 4.890 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yun, H.; Joe, H.E.; Song, D.H.; Song, Y.-J.; Hong, S.; Kim, C.-H.; Kim, N.Y.; Hur, G.H.; Yu, C.H. Toxicity and Efficacy Evaluation of Soluble Recombinant Ricin Vaccine. Vaccines 2024, 12, 1116. https://doi.org/10.3390/vaccines12101116
Yun H, Joe HE, Song DH, Song Y-J, Hong S, Kim C-H, Kim NY, Hur GH, Yu CH. Toxicity and Efficacy Evaluation of Soluble Recombinant Ricin Vaccine. Vaccines. 2024; 12(10):1116. https://doi.org/10.3390/vaccines12101116
Chicago/Turabian StyleYun, Hyeongseok, Hae Eun Joe, Dong Hyun Song, Young-Jo Song, Sunghyun Hong, Chang-Hwan Kim, Na Young Kim, Gyeung Haeng Hur, and Chi Ho Yu. 2024. "Toxicity and Efficacy Evaluation of Soluble Recombinant Ricin Vaccine" Vaccines 12, no. 10: 1116. https://doi.org/10.3390/vaccines12101116






