Insights into the Pathogenesis and Development of Recombinant Japanese Encephalitis Virus Genotype 3 as a Vaccine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture, Virus Preparation, and Antibodies
2.2. cDNA Synthesis and Cloning
2.3. Transfection and Propagation of Recombinant JEV3
2.4. Analysis of Confocal Fluorescence Microscopy
2.5. Sequence Analysis of the Recombinant Virus
2.6. Cryo-Electron Microscopy (Cryo-EM) Analysis
2.7. Viral Titration
2.8. Mouse Immunization
2.9. Enzyme-Linked Immunosorbent Assay (ELISA) Analysis
2.10. Serum Neutralization (SN) Test
2.11. Statistical Analysis
3. Results
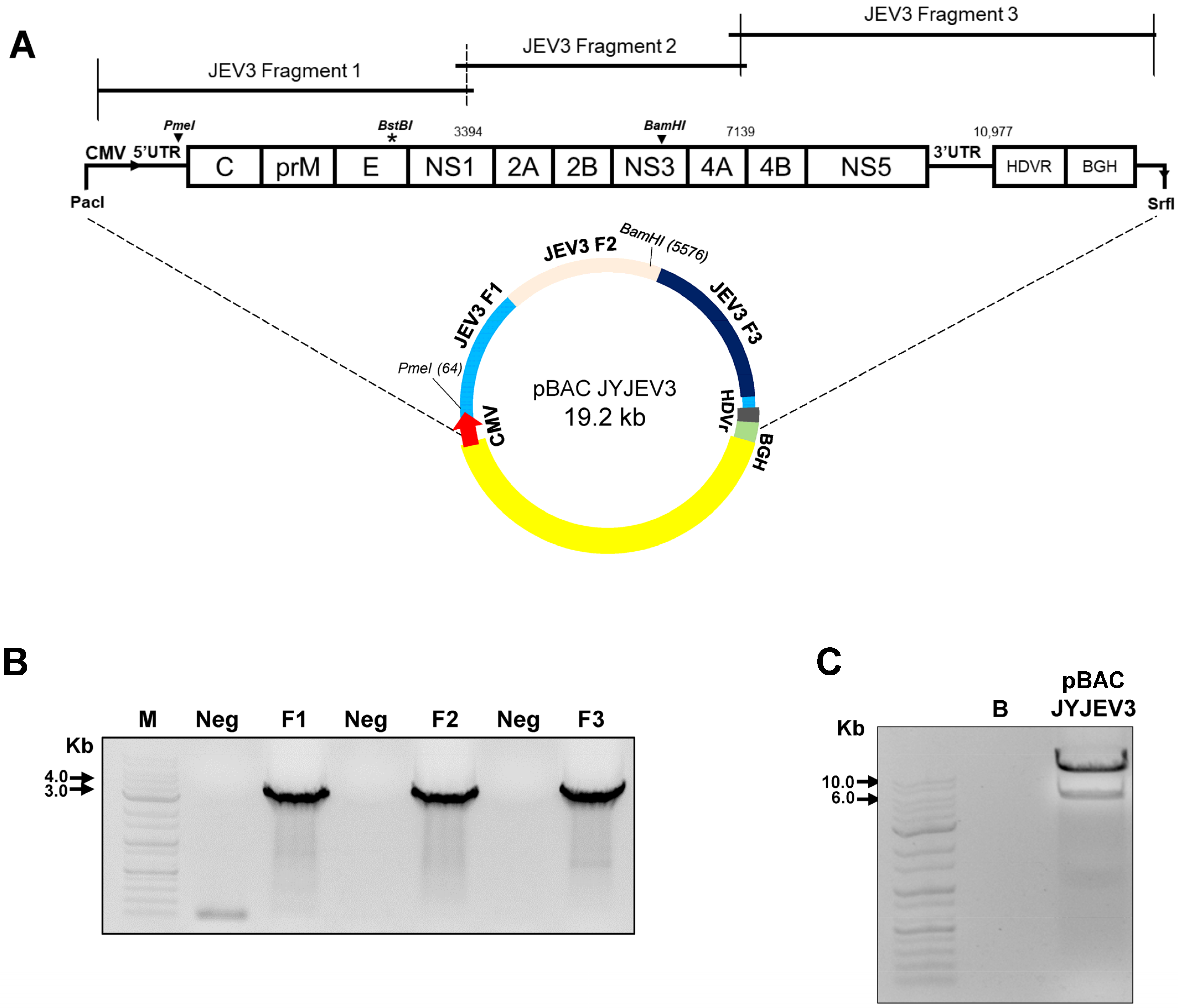
3.1. Construction of the Full-Length cDNA Clone for JEV3
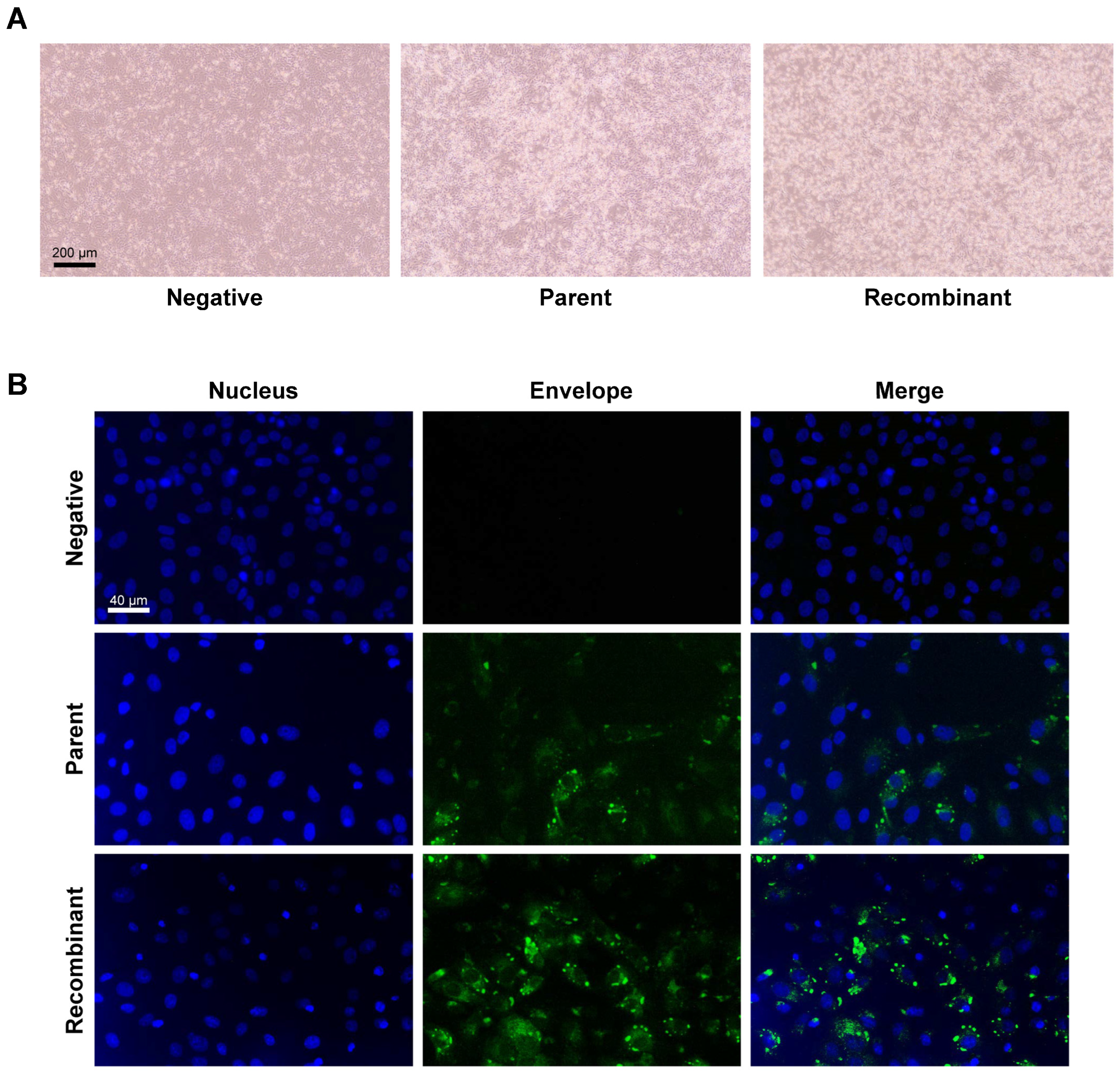
3.2. Transfection of the JEV3 Infectious Clone Plasmid Produced Infectious JEV3 Particles
3.3. Genetic Marker Development and Mutation Analysis of Recombinant JEV3
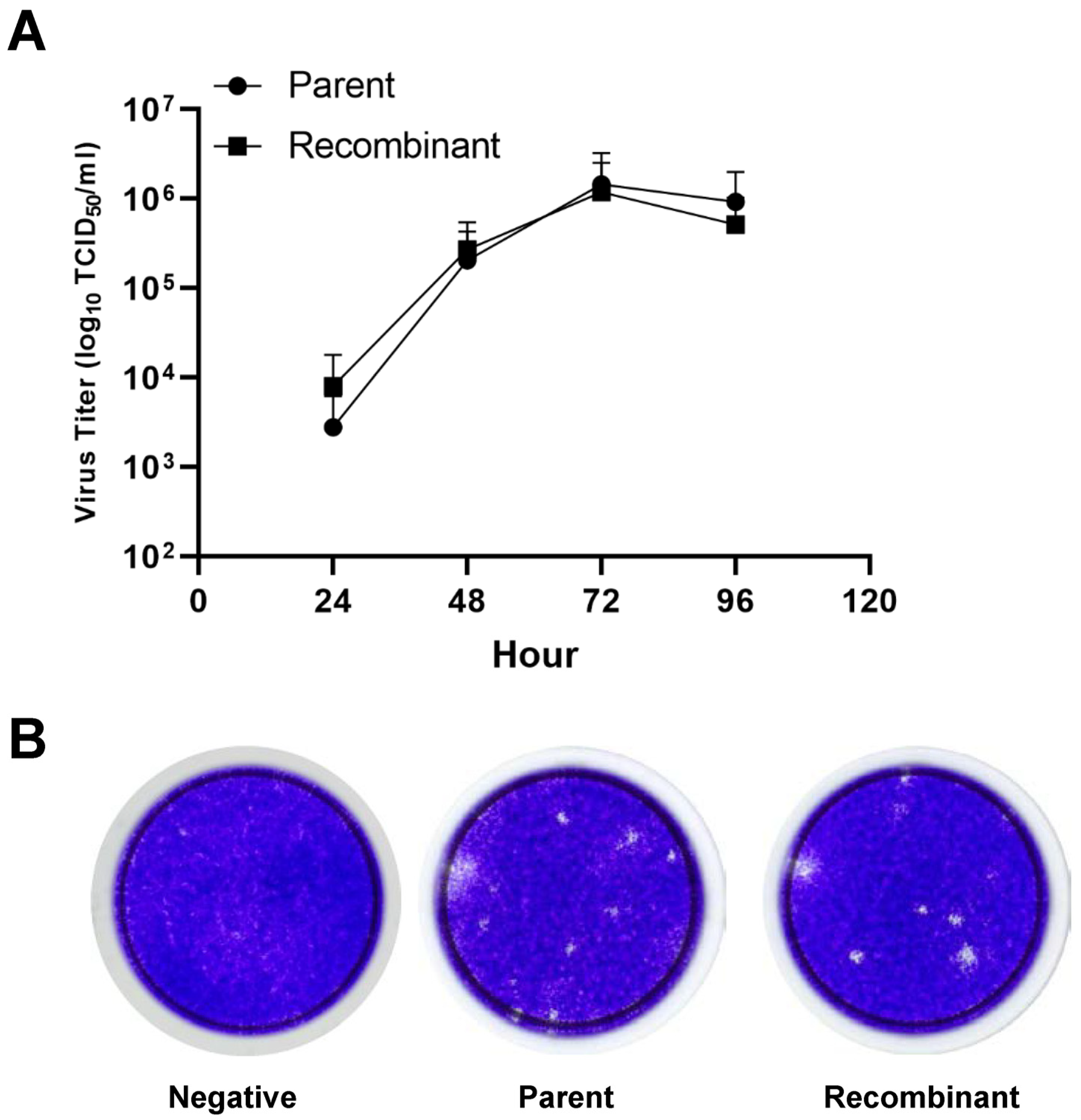
3.4. Comparison of the Growth Kinetics of the Parental and Recombinant Virus in Cell Culture
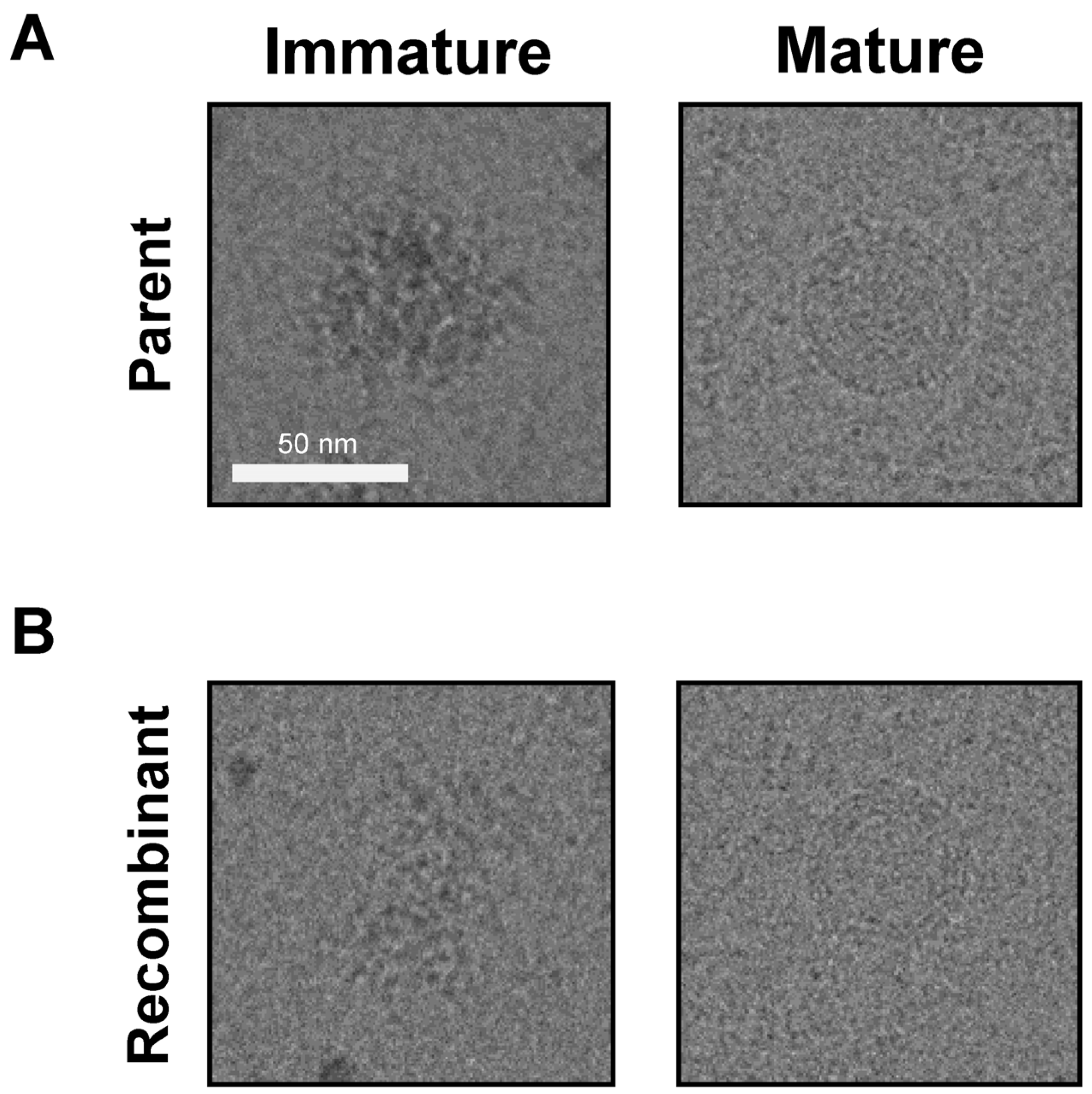
3.5. JEV3 Parent and Recombinant Virus Morphology Was Revealed by Cryo-EM Analysis
3.6. Investigation of the Immune Response in Mice
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Erlanger, T.E.; Weiss, S.; Keiser, J.; Utzinger, J.; Wiedenmayer, K. Past, present, and future of Japanese encephalitis. Emerg. Infect. Dis. 2009, 15, 1–7. [Google Scholar] [CrossRef]
- Le Flohic, G.; Porphyre, V.; Barbazan, P.; Gonzalez, J.P. Review of Climate, Landscape, and Viral Genetics as Drivers of the Japanese Encephalitis Virus Ecology. PLoS Neglected Trop. Dis. 2013, 7, e2208. [Google Scholar] [CrossRef]
- Pan, X.L.; Liu, H.; Wang, H.Y.; Fu, S.H.; Liu, H.Z.; Zhang, H.L.; Li, M.H.; Gao, X.Y.; Wang, J.L.; Sun, X.H.; et al. Emergence of Genotype I of Japanese Encephalitis Virus as the Dominant Genotype in Asia. J. Virol. 2011, 85, 9847–9853. [Google Scholar] [CrossRef]
- Solomon, T.; Ni, H.; Beasley, D.W.C.; Ekkelenkamp, M.; Cardosa, M.J.; Barrett, A.D.T. Origin and evolution of Japanese encephalitis virus in southeast Asia. J. Virol. 2003, 77, 3091–3098. [Google Scholar] [CrossRef]
- Kuwata, R.; Torii, S.; Shimoda, H.; Supriyono; Phichitraslip, T.; Prasertsincharoen, N.; Takemae, H.; Bautista, R.C.J.T.; Ebora, V.D.B.M.; Abella, J.A.C.; et al. Distribution of Japanese Encephalitis Virus, Japan and Southeast Asia, 2016–2018. Emerg. Infect. Dis. 2020, 26, 125–128. [Google Scholar] [CrossRef]
- Campbell, G.L.; Hills, S.L.; Fischer, M.; Jacobson, J.A.; Hoke, C.H.; Hombach, J.M.; Marfin, A.A.; Solomon, T.; Tsai, T.F.; Tsu, V.D.; et al. Estimated global incidence of Japanese encephalitis: A systematic review. B World Health Organ. 2011, 89, 766–774. [Google Scholar] [CrossRef]
- Weaver, S.C.; Barrett, A.D.T. Transmission cycles, host range, evolution and emergence of arboviral disease. Nat. Rev. Microbiol. 2004, 2, 789–801. [Google Scholar] [CrossRef]
- Ellis, P.M.; Daniels, P.W.; Banks, D.J. Japanese encephalitis. Vet. Clin. North. Am. Equine Pract. 2000, 16, 565–578. [Google Scholar] [CrossRef]
- Lee, A.R.; Song, J.M.; Seo, S.U. Emerging Japanese Encephalitis Virus Genotype V in Republic of Korea. J. Microbiol. Biotechnol. 2022, 32, 955–959. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, M.J.; Turtle, L.; Solomon, T. Japanese encephalitis virus infection. Handb. Clin. Neurol. 2014, 123, 561–576. [Google Scholar] [CrossRef] [PubMed]
- Misra, U.K.; Kalita, J. Overview: Japanese encephalitis. Prog. Neurobiol. 2010, 91, 108–120. [Google Scholar] [CrossRef] [PubMed]
- Laureti, M.; Narayanan, D.; Rodriguez-Andres, J.; Fazakerley, J.K.; Kedzierski, L. Flavivirus Receptors: Diversity, Identity, and Cell Entry. Front. Immunol. 2018, 9, 2180. [Google Scholar] [CrossRef] [PubMed]
- Jan, L.R.; Yang, C.S.; Trent, D.W.; Falgout, B.; Lai, C.J. Processing of Japanese encephalitis virus non-structural proteins: NS2B-NS3 complex and heterologous proteases. J. Gen. Virol. 1995, 76 Pt 3, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, S.; Kuhn, R.J.; Rossmann, M.G. A structural perspective of the flavivirus life cycle. Nat. Rev. Microbiol. 2005, 3, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Almazan, F.; Gonzalez, J.M.; Penzes, Z.; Izeta, A.; Calvo, E.; Plana-Duran, J.; Enjuanes, L. Engineering the largest RNA virus genome as an infectious bacterial artificial chromosome. Proc. Natl. Acad. Sci. USA 2000, 97, 5516–5521. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.J.; Magalhaes, T.; Silva Junior, J.V.; Silva, A.N.; Cordeiro, M.T.; Gil, L.H. Full-length infectious clone of a low passage dengue virus serotype 2 from Brazil. Mem. Inst. Oswaldo Cruz 2015, 110, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Almazán, F.; DeDiego, M.L.; Sola, I.; Zuñiga, S.; Nieto-Torres, J.L.; Marquez-Jurado, S.; Andrés, G.; Enjuanes, L. Engineering a Replication-Competent, Propagation-Defective Middle East Respiratory Syndrome Coronavirus as a Vaccine Candidate. Mbio 2013, 4, e00650-13. [Google Scholar] [CrossRef] [PubMed]
- Yamshchikov, V.; Mishin, V.; Cominelli, F. A new strategy in design of (+)RNA virus infectious clones enabling their stable propagation in. Virology 2001, 281, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Bredenbeek, P.J.; Kooi, E.A.; Lindenbach, B.; Huijkman, N.; Rice, C.M.; Spaan, W.J.M. A stable full-length yellow fever virus cDNA clone and the role of conserved RNA elements in flavivirus replication. J. Gen. Virol. 2003, 84, 1261–1268. [Google Scholar] [CrossRef]
- Aubry, F.; Nougairede, A.; de Fabritus, L.; Querat, G.; Gould, E.A.; de Lamballerie, X. Single-stranded positive-sense RNA viruses generated in days using infectious subgenomic amplicons. J. Gen. Virol. 2014, 95, 2462–2467. [Google Scholar] [CrossRef]
- Thiel, V.; Herold, J.; Schelle, B.; Siddell, S.G. Infectious RNA transcribed in vitro from a cDNA copy of the human coronavirus genome cloned in vaccinia virus. J. Gen. Virol. 2001, 82, 1273–1281. [Google Scholar] [CrossRef]
- Donaldson, E.F.; Yount, B.; Sims, A.C.; Burkett, S.; Pickles, R.J.; Baric, R.S. Systematic assembly of a full-length infectious clone of human coronavirus NL63. J. Virol. 2008, 82, 11948–11957. [Google Scholar] [CrossRef]
- Hou, Y.J.; Okuda, K.; Edwards, C.E.; Martinez, D.R.; Asakura, T.; Dinnon, K.H., 3rd; Kato, T.; Lee, R.E.; Yount, B.L.; Mascenik, T.M.; et al. SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell 2020, 182, 429–446 e414. [Google Scholar] [CrossRef]
- Edmonds, J.; van Grinsven, E.; Prow, N.; Bosco-Lauth, A.; Brault, A.C.; Bowen, R.A.; Hall, R.A.; Khromykh, A.A. A novel bacterium-free method for generation of flavivirus infectious DNA by circular polymerase extension reaction allows accurate recapitulation of viral heterogeneity. J. Virol. 2013, 87, 2367–2372. [Google Scholar] [CrossRef]
- Gracheva, A.V.; Korchevaya, E.R.; Ammour, Y.I.; Smirnova, D.I.; Sokolova, O.S.; Glukhov, G.S.; Moiseenko, A.V.; Zubarev, I.V.; Samoilikov, R.V.; Leneva, I.A.; et al. Immunogenic properties of SARS-CoV-2 inactivated by ultraviolet light. Arch. Virol. 2022, 167, 2181–2191. [Google Scholar] [CrossRef]
- Neumann, G.; Kawaoka, Y. Reverse genetics systems for the generation of segmented negative-sense RNA viruses entirely from cloned cDNA. Curr. Top. Microbiol. Immunol. 2004, 283, 43–60. [Google Scholar] [CrossRef]
- Stobart, C.C.; Moore, M.L. RNA virus reverse genetics and vaccine design. Viruses 2014, 6, 2531–2550. [Google Scholar] [CrossRef]
- Pu, S.Y.; Wu, R.H.; Yang, C.C.; Jao, T.M.; Tsai, M.H.; Wang, J.C.; Lin, H.M.; Chao, Y.S.; Yueh, A. Successful propagation of flavivirus infectious cDNAs by a novel method to reduce the cryptic bacterial promoter activity of virus genomes. J. Virol. 2011, 85, 2927–2941. [Google Scholar] [CrossRef]
- Almazan, F.; Sola, I.; Zuniga, S.; Marquez-Jurado, S.; Morales, L.; Becares, M.; Enjuanes, L. Coronavirus reverse genetic systems: Infectious clones and replicons. Virus Res. 2014, 189, 262–270. [Google Scholar] [CrossRef]
- Li, D.; Aaskov, J.; Lott, W.B. Identification of a cryptic prokaryotic promoter within the cDNA encoding the 5’ end of dengue virus RNA genome. PLoS ONE 2011, 6, e18197. [Google Scholar] [CrossRef]
- Shiu, J.S.; Liu, S.T.; Chang, T.J.; Ho, W.C.; Lai, S.S.; Chang, Y.S. The presence of RNA splicing signals in the cDNA construct of the E2 gene of classical swine fever virus affected its expression. J. Virol. Methods 1997, 69, 223–230. [Google Scholar] [CrossRef]
- Satyanarayana, T.; Gowda, S.; Ayllon, M.A.; Dawson, W.O. Frameshift mutations in infectious cDNA clones of Citrus tristeza virus: A strategy to minimize the toxicity of viral sequences to Escherichia coli. Virology 2003, 313, 481–491. [Google Scholar] [CrossRef]
- Yun, S.I.; Kim, S.Y.; Rice, C.M.; Lee, Y.M. Development and application of a reverse genetics system for Japanese encephalitis virus. J. Virol. 2003, 77, 6450–6465. [Google Scholar] [CrossRef]
- Ferro, M.M.M.; Ramos-Sobrinho, R.; Xavier, C.A.D.; Zerbini, F.M.; Lima, G.S.A.; Nagata, T.; Assuncao, I.P. New approach for the construction of infectious clones of a circular DNA plant virus using Gibson Assembly. J. Virol. Methods 2019, 263, 20–23. [Google Scholar] [CrossRef]
- Xu, W.; Klumbys, E.; Ang, E.L.; Zhao, H. Emerging molecular biology tools and strategies for engineering natural product biosynthesis. Metab. Eng. Commun. 2020, 10, e00108. [Google Scholar] [CrossRef]
- Avila-Perez, G.; Nogales, A.; Martin, V.; Almazan, F.; Martinez-Sobrido, L. Reverse Genetic Approaches for the Generation of Recombinant Zika Virus. Viruses 2018, 10, 597. [Google Scholar] [CrossRef]
- Shizuya, H.; Kouros-Mehr, H. The development and applications of the bacterial artificial chromosome cloning system. Keio J. Med. 2001, 50, 26–30. [Google Scholar] [CrossRef]
- Cui, X.; Adler, S.P.; Davison, A.J.; Smith, L.; Habib, E.-S.E.; McVoy, M.A. Bacterial artificial chromosome clones of viruses comprising the towne cytomegalovirus vaccine. J. Biomed. Biotechnol. 2012, 2012, 428498. [Google Scholar] [CrossRef]
- Kim, M.; Cho, H.; Lee, S.H.; Park, W.J.; Kim, J.M.; Moon, J.S.; Kim, G.W.; Lee, W.; Jung, H.G.; Yang, J.S.; et al. An infectious cDNA clone of a growth attenuated Korean isolate of MERS coronavirus KNIH002 in clade B. Emerg. Microbes Infect. 2020, 9, 2714–2726. [Google Scholar] [CrossRef]
- Lee, J.; Bae, S.; Myoung, J. Generation of Full-Length Infectious cDNA Clones of Middle East Respiratory Syndrome Coronavirus. J. Microbiol. Biotechnol. 2019, 29, 999–1007. [Google Scholar] [CrossRef]
- Xie, X.; Muruato, A.; Lokugamage, K.G.; Narayanan, K.; Zhang, X.; Zou, J.; Liu, J.; Schindewolf, C.; Bopp, N.E.; Aguilar, P.V.; et al. An Infectious cDNA Clone of SARS-CoV-2. Cell Host Microbe 2020, 27, 841–848 e843. [Google Scholar] [CrossRef]
- Yount, B.; Curtis, K.M.; Fritz, E.A.; Hensley, L.E.; Jahrling, P.B.; Prentice, E.; Denison, M.R.; Geisbert, T.W.; Baric, R.S. Reverse genetics with a full-length infectious cDNA of severe acute respiratory syndrome coronavirus. Proc. Natl. Acad. Sci. USA 2003, 100, 12995–13000. [Google Scholar] [CrossRef]
- Hoffmann, E.; Neumann, G.; Kawaoka, Y.; Hobom, G.; Webster, R.G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 2000, 97, 6108–6113. [Google Scholar] [CrossRef]
- Wang, J.; Osterrieder, N. Generation of an infectious clone of duck enteritis virus (DEV) and of a vectored DEV expressing hemagglutinin of H5N1 avian influenza virus. Virus Res. 2011, 159, 23–31. [Google Scholar] [CrossRef]
- Shan, C.; Xie, X.; Muruato, A.E.; Rossi, S.L.; Roundy, C.M.; Azar, S.R.; Yang, Y.; Tesh, R.B.; Bourne, N.; Barrett, A.D.; et al. An Infectious cDNA Clone of Zika Virus to Study Viral Virulence, Mosquito Transmission, and Antiviral Inhibitors. Cell Host Microbe 2016, 19, 891–900. [Google Scholar] [CrossRef]
- Choo, J.J.Y.; Vet, L.J.; McMillan, C.L.D.; Harrison, J.J.; Scott, C.A.P.; Depelsenaire, A.C.I.; Fernando, G.J.P.; Watterson, D.; Hall, R.A.; Young, P.R.; et al. A chimeric dengue virus vaccine candidate delivered by high density microarray patches protects against infection in mice. NPJ Vaccines 2021, 6, 66. [Google Scholar] [CrossRef]
- Erra, E.O.; Askling, H.H.; Yoksan, S.; Rombo, L.; Riutta, J.; Vene, S.; Lindquist, L.; Vapalahti, O.; Kantele, A. Cross-protection elicited by primary and booster vaccinations against Japanese encephalitis: A two-year follow-up study. Vaccine 2013, 32, 119–123. [Google Scholar] [CrossRef]
- Hegde, N.R.; Gore, M.M. Japanese encephalitis vaccines: Immunogenicity, protective efficacy, effectiveness, and impact on the burden of disease. Hum. Vaccin. Immunother. 2017, 13, 1320–1337. [Google Scholar] [CrossRef]
- Liu, X.; Yu, Y.; Li, M.; Liang, G.; Wang, H.; Jia, L.; Dong, G. Study on the protective efficacy of SA14-14-2 attenuated Japanese encephalitis against different JE virus isolates circulating in China. Vaccine 2011, 29, 2127–2130. [Google Scholar] [CrossRef]
- Singh, A.; Mitra, M.; Sampath, G.; Venugopal, P.; Rao, J.V.; Krishnamurthy, B.; Gupta, M.K.; Sri Krishna, S.; Sudhakar, B.; Rao, N.B.; et al. A Japanese Encephalitis Vaccine from India Induces Durable and Cross-protective Immunity Against Temporally and Spatially Wide-ranging Global Field Strains. J. Infect. Dis. 2015, 212, 715–725. [Google Scholar] [CrossRef]
- Dolan, P.T.; Whitfield, Z.J.; Andino, R. Mechanisms and Concepts in RNA Virus Population Dynamics and Evolution. Annu. Rev. Virol. 2018, 5, 69–92. [Google Scholar] [CrossRef] [PubMed]
- Shi, M.; Lin, X.D.; Chen, X.; Tian, J.H.; Chen, L.J.; Li, K.; Wang, W.; Eden, J.S.; Shen, J.J.; Liu, L.; et al. The evolutionary history of vertebrate RNA viruses. Nature 2018, 556, 197–202. [Google Scholar] [CrossRef]


| Primer | Sequence (5′–3′) |
|---|---|
| JEV3 Fragment 1 F | CTATATAAGCAGAGCTAGAAGTTTATCTGCGTGAACTTCTTG |
| JEV3 Fragment 1 R | CCAGTCAGTGATCAACTTTCCACTGTCAGTAGTGGTTCTGACC |
| JEV3 Fragment 2 F | CTACTGACAGTGGAAAGTTGATCACTGACTGGTGCTGTCGC |
| JEV3 Fragment 2 R | GGACAAATAATGAGCCAGCTTGTGAGTTAATTGAGGCTAGCG |
| JEV3 Fragment 3 F | AATTAACTCACAAGCTGGCTCATTATTTGTCCTGCCACGAGG |
| JEV3 Fragment 3 R | GCTGGTGGTGAGGAAGAACACAGGATCTGGGTCGGCATGGCATC |
| Silent F (BstBl) | CAAGTGTTTGGTGGTGCCTTTCGAACACTCTTCGGGGGAATG |
| Silent R (BstBl) | CATTCCCCCGAAGAGTGTTCGAAAGGCACCACCAAACACTTG |
| Detection (Envelope) F | TTCAACTGTCTGGGAATGGGCAATC |
| Detection (Envelope) R | AGCATGCACATTGGTCGCTAAGAAC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-Y.; Lee, H.-M.; Jun, S.-H.; Kamitani, W.; Kim, O.; Shin, H.-J. Insights into the Pathogenesis and Development of Recombinant Japanese Encephalitis Virus Genotype 3 as a Vaccine. Vaccines 2024, 12, 597. https://doi.org/10.3390/vaccines12060597
Park J-Y, Lee H-M, Jun S-H, Kamitani W, Kim O, Shin H-J. Insights into the Pathogenesis and Development of Recombinant Japanese Encephalitis Virus Genotype 3 as a Vaccine. Vaccines. 2024; 12(6):597. https://doi.org/10.3390/vaccines12060597
Chicago/Turabian StylePark, Jae-Yeon, Hye-Mi Lee, Sung-Hoon Jun, Wataru Kamitani, Onnuri Kim, and Hyun-Jin Shin. 2024. "Insights into the Pathogenesis and Development of Recombinant Japanese Encephalitis Virus Genotype 3 as a Vaccine" Vaccines 12, no. 6: 597. https://doi.org/10.3390/vaccines12060597
APA StylePark, J.-Y., Lee, H.-M., Jun, S.-H., Kamitani, W., Kim, O., & Shin, H.-J. (2024). Insights into the Pathogenesis and Development of Recombinant Japanese Encephalitis Virus Genotype 3 as a Vaccine. Vaccines, 12(6), 597. https://doi.org/10.3390/vaccines12060597







