Buccal Administration of a Zika Virus Vaccine Utilizing 3D-Printed Oral Dissolving Films in a Mouse Model
Abstract
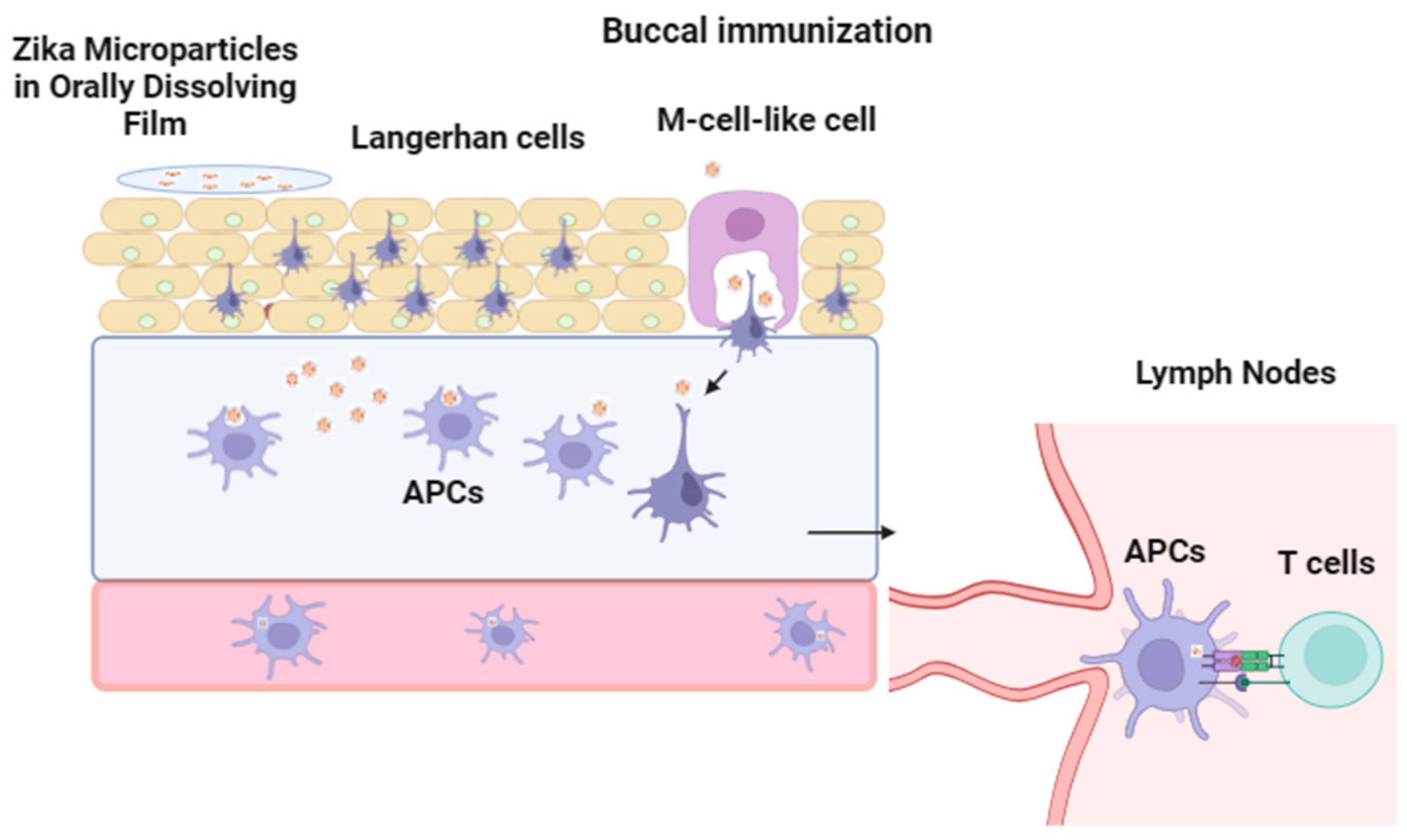
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Formulation of the Microparticulate Vaccine
2.2.2. Preparation of 3D-Printed Orally Dissolving Films (ODFs)
2.2.3. Characterization of Vaccine Particles: Particle Size, Zeta Potential, and Laser Particle Counter
2.2.4. Morphological Characterization of Oral Dissolving Films (ODFs)
2.2.5. Fourier Transform Infrared Microscopy (FTIR)
2.2.6. Physiochemical Assessment of the ODFs
2.2.7. Evaluation of Immunostimulatory Potential of Vaccine MPs Loaded in ODFs
2.2.8. Evaluation of the Ability of the MP Vaccine to Induce Autophagosomes
2.2.9. Evaluation of the Cytotoxicity of Vaccine MPs Loaded in ODFs
2.2.10. In Vivo Study Design for Buccal Immunization with Oral Dissolving Film (ODF)
2.2.11. Measurement of Zika-Specific Antibody Titers Using ELISA
2.2.12. Measurement of Cellular, Memory, and Cytokine Responses
2.2.13. Statistical Analysis
3. Results
3.1. Vaccine Microparticle Characterization: Particle Size, Zeta Potential, and Laser Particle Counter
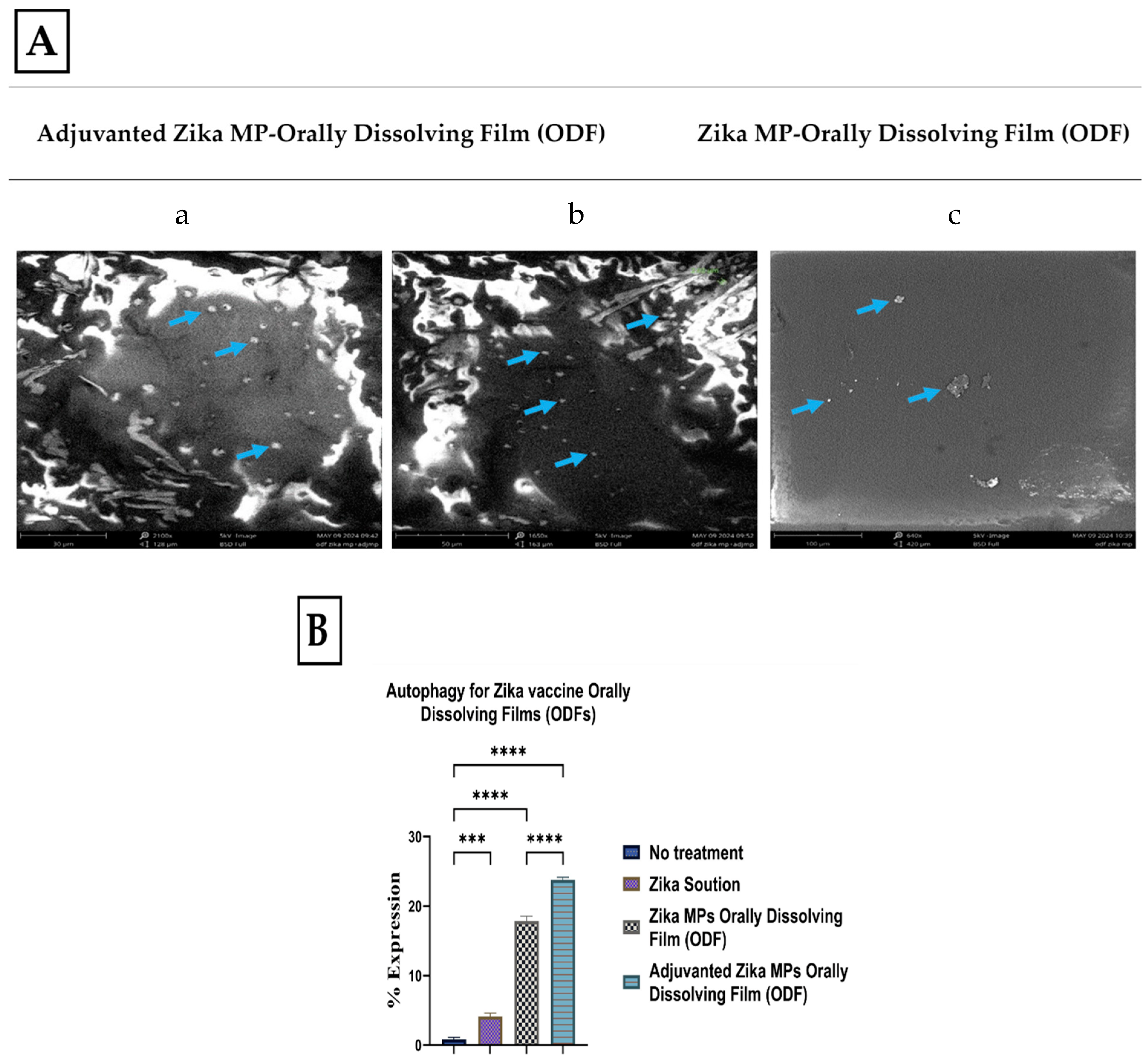
3.2. Morphology of ODFs by Scanning Electron Microscopy (SEM)
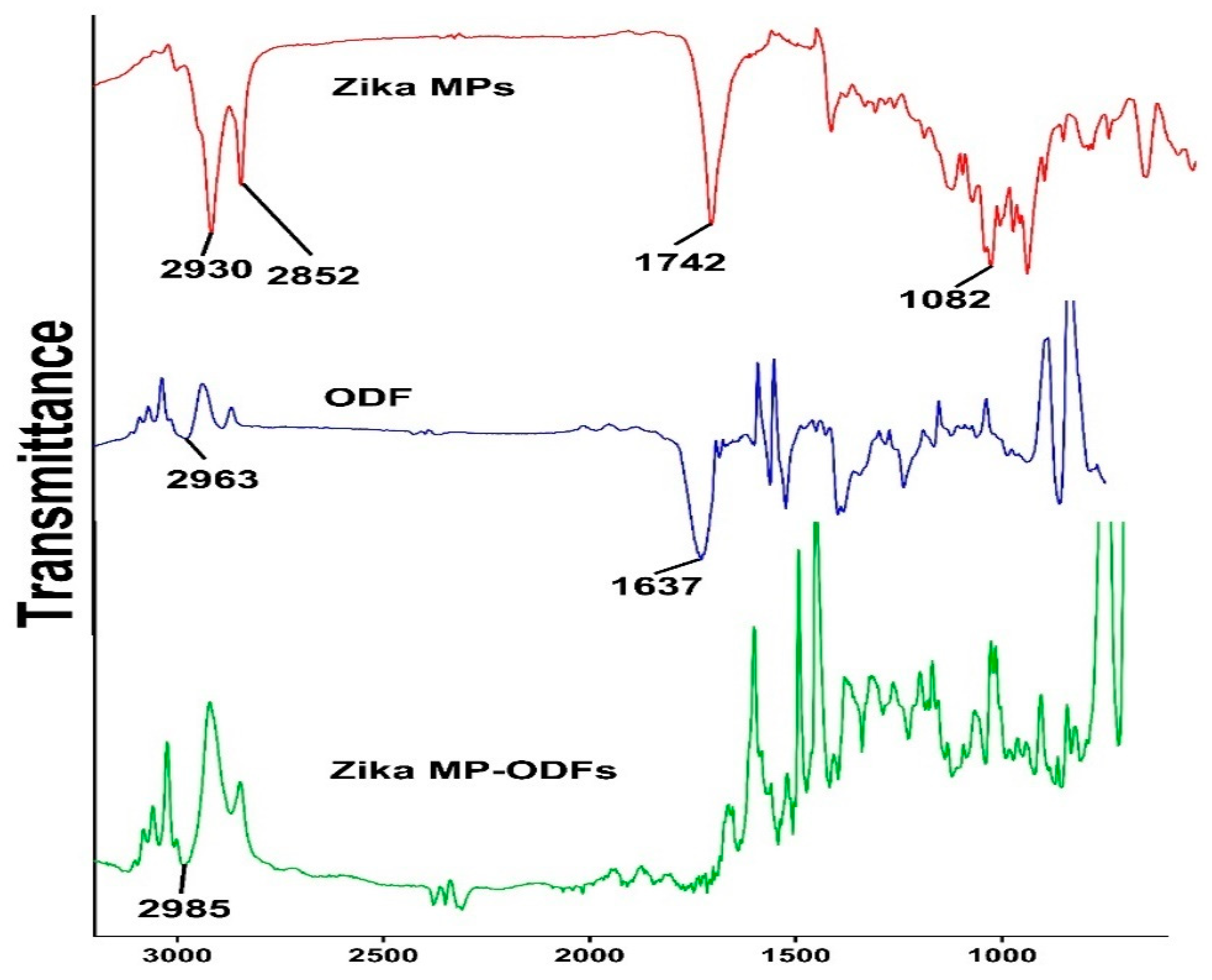
3.3. Fourier Transform Infrared Microscopy (FTIR)
3.4. Physiochemical Assessment of the ODFs
| Without Vaccine | With Zika Vaccine | ||
|---|---|---|---|
| Blank ODF | Zika MP ODF | Adjuvanted Zika MP ODF | |
| Avg. Weight (mg) | 8.83 ± 0.89 | 8.98 ± 0.87 | 10.0 ± 1.37 |
| Thickness (µm) | 0.22 ± 0.11 | 0.25 ± 0.09 | 0.27 ± 0.07 |
| Diameter (mm) | 0.40 ± 0.01 | 0.40 ± 0.01 | 0.40 ± 0.01 |
| Disintegration time (min) | 4.00 ± 0.52 | 3.01 ± 1.18 | 3.39 ±1.26 |
| pH | 7.25 ± 0.07 | 7.05 ± 0.20 | 7.19 ± 0.12 |
| Blank ODF | ||||
|---|---|---|---|---|
| 1 Week | 3 Months | 6 Months | 1 Year | |
| Avg. Weight (mg) | 8.03 ± 01.09 | 8.08 ± 0.87 | 8.25 ± 0.45 | 8.32 ± 02.10 |
| Thickness (µm) | 0.23 ± 0.10 | 0.25 ± 0.09 | 0.28 ± 0.11 | 0.27 ± 0.15 |
| Disintegration time (min) | 3.95 ± 0.43 | 4.01 ± 0.43 | 3.86 ± 0.32 | 3.23 ± 0.17 |
| pH | 7.15 ± 0.03 | 7.18 ± 0.10 | 7.20 ± 0.01 | 7.23 ± 0.16 |
| Zika MP Vaccine ODF | ||||
|---|---|---|---|---|
| 1 Week | 3 Months | 6 Months | 1 Year | |
| Avg. Weight (mg) | 8.76 ± 0.47 | 8.56 ± 0.23 | 8.66 ± 0.43 | 8.23 ± 0.33 |
| Thickness (µm) | 0.26 ± 0.10 | 0.27 ± 0.04 | 0.27 ± 0.12 | 0.26 ± 0.02 |
| Disintegration time (min) | 3.05 ± 0.06 | 3.12 ± 0.23 | 3.23 ±0.11 | 3.15 ±0.15 |
| pH | 7.08 ± 0.10 | 7.00 ± 0.11 | 7.04 ± 0.10 | 7.03 ± 0.05 |
| Adjuvanted Zika MP Vaccine ODF | ||||
|---|---|---|---|---|
| 1 Week | 3 Months | 6 Months | 1 Year | |
| Avg. Weight (mg) | 9.8 ± 0.32 | 9.98 ± 0.82 | 10.1 ± 0.23 | 9.8 ± 0.32 |
| Thickness (µm) | 0.26 ± 0.09 | 0.25 ± 0.11 | 0.28 ± 0.12 | 0.29 ± 0.15 |
| Disintegration time (min) | 3.42 ±0.45 | 3.54 ± 0.32 | 3.16 ±1.16 | 3.40 ± 0.21 |
| pH | 7.23 ± 0.10 | 7.15 ± 0.13 | 7.12 ± 0.09 | 7.22 ± 0.12 |
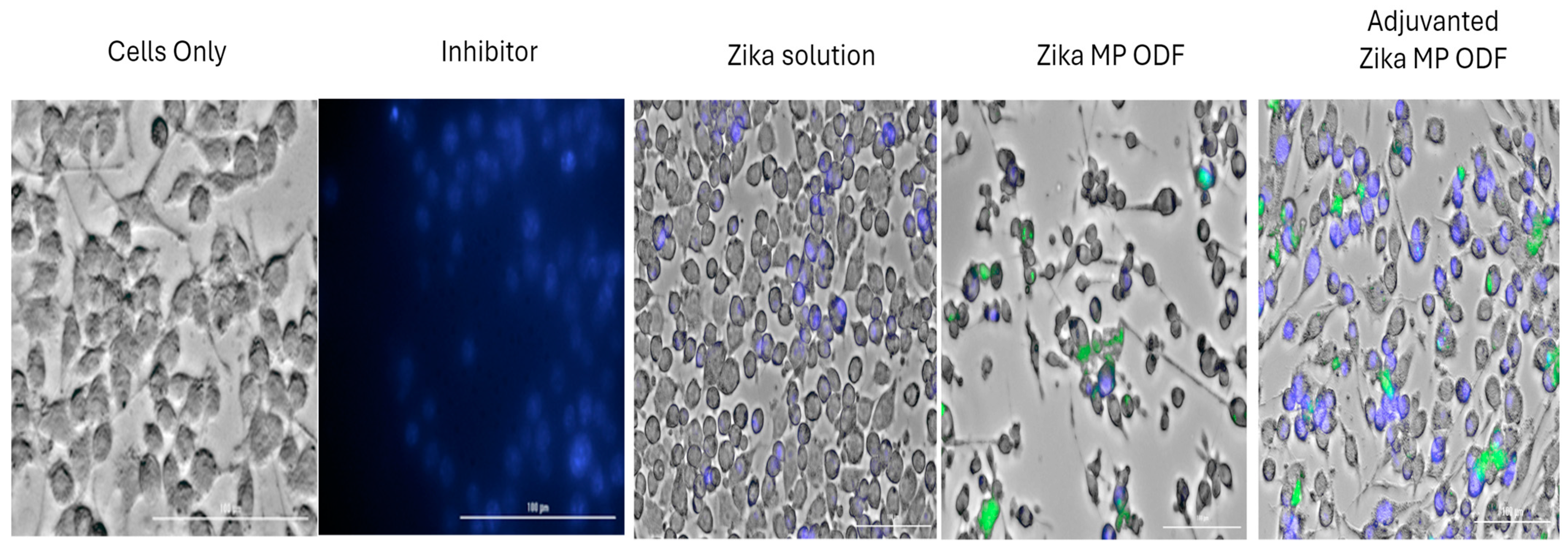
3.5. Immunostimulatory Potential and Cytotoxicity Profile of ODFs
3.6. The Ability of Zika Vaccine MP-ODFs to Induce Autophagosomes
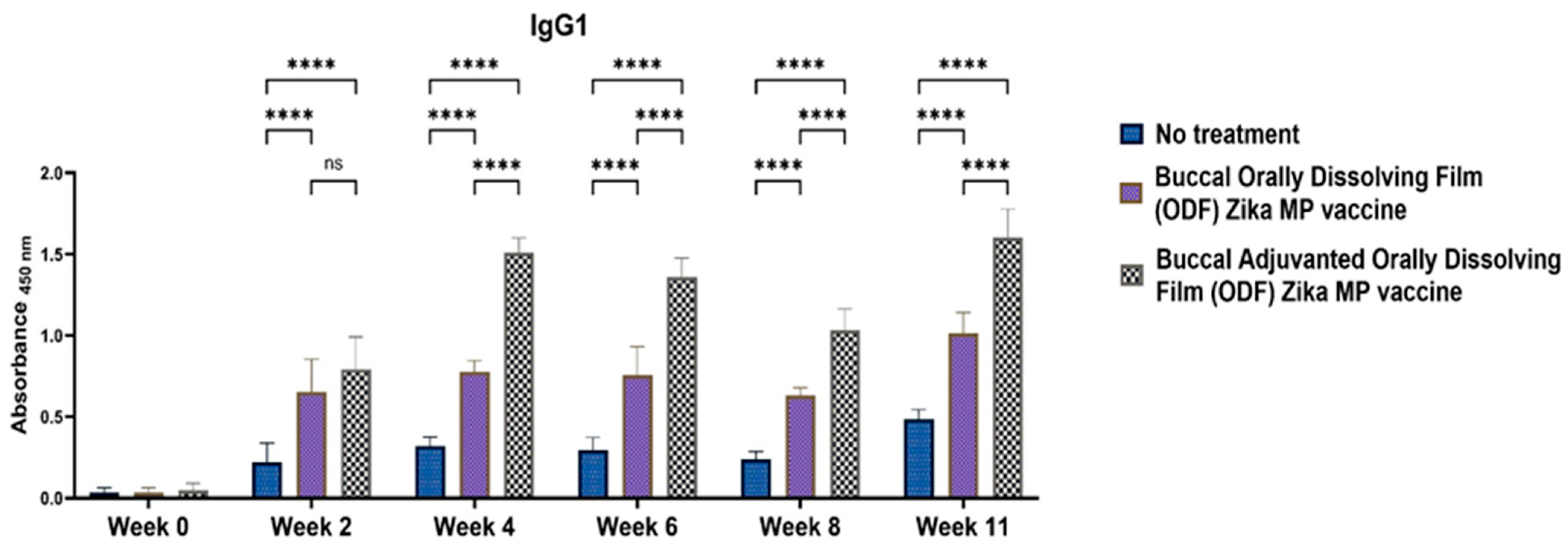
3.7. Zika-Specific Humoral Antibodies
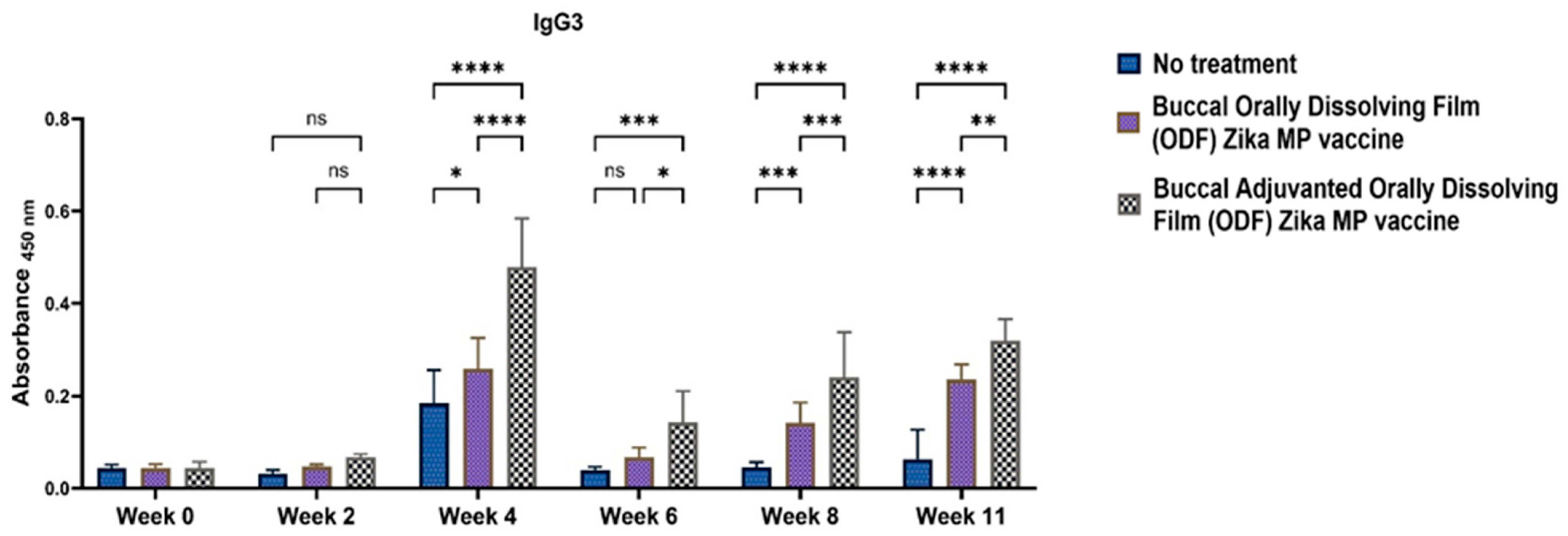
3.8. Zika-Specific Cellular T-Cell Responses Following Buccal Immunization with ODFs
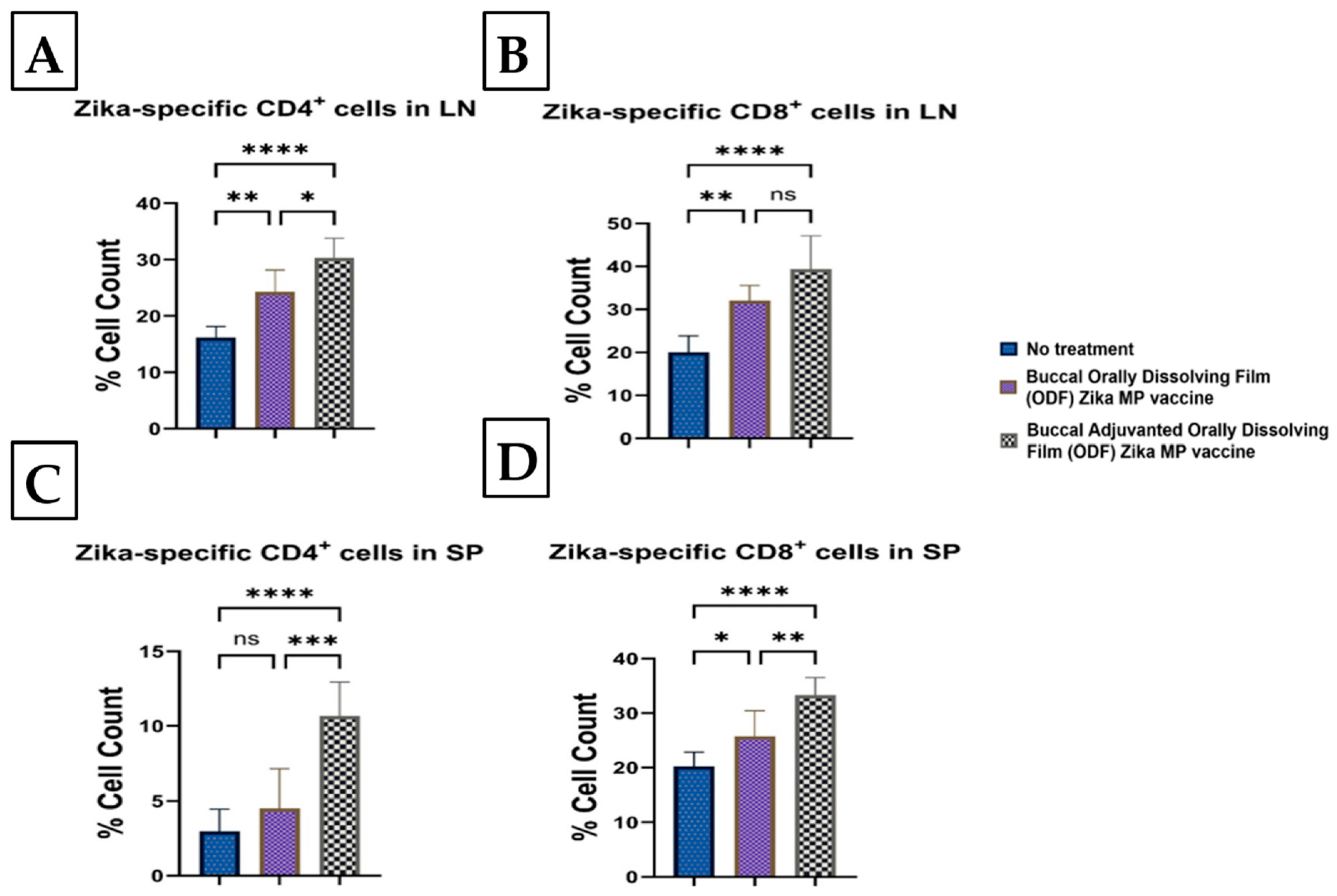
3.9. Memory and Intracellular Cytokine Response after Buccal Vaccination with ODFs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Kale, A. Novel Microparticle-Based Microneedle Vaccine For Zika Virus. Ph.D. Dissertation, Mercer University, Atlanta, GA, USA, 2023. [Google Scholar]
- Kale, A.; Joshi, D.; Menon, I.; Bagwe, P.; Patil, S.; Vijayanand, S.; Gomes, K.B.; D’Souza, M. Novel microparticulate Zika vaccine induces a significant immune response in a preclinical murine model after intramuscular administration. Int. J. Pharm. 2022, 624, 121975. [Google Scholar] [CrossRef] [PubMed]
- Barrett, A.D.T. Current status of Zika vaccine development: Zika vaccines advance into clinical evaluation. NPJ Vaccines 2018, 3, 24. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ling, L.; Zhang, Z.; Marin-Lopez, A. Current Advances in Zika Vaccine Development. Vaccines 2022, 10, 1816. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.Q.; Zhang, N.N.; Li, X.F.; Wang, Y.Q.; Tian, M.; Qiu, Y.F.; Fan, J.W.; Hao, J.N.; Huang, X.Y.; Dong, H.L.; et al. Intranasal infection and contact transmission of Zika virus in guinea pigs. Nat. Commun. 2017, 8, 1648. [Google Scholar] [CrossRef] [PubMed]
- Cauchemez, S.; Besnard, M.; Bompard, P.; Dub, T.; Guillemette-Artur, P.; Eyrolle-Guignot, D.; Salje, H.; Van Kerkhove, M.D.; Abadie, V.; Garel, C.; et al. Association between Zika virus and microcephaly in French Polynesia, 2013–2015: A retrospective study. Lancet 2016, 387, 2125–2132. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, É.S.; Chagas, J.R.L.P.; Cangussu, M.C.T.; Vianna, M.I.P. Chronology and sequence of deciduous teeth eruption in children with microcephaly associated to the Zika virus. Spec. Care Dent. 2020, 40, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Gusmão, T.P.D.L.; Faria, A.B.S.D.; Leão Filho, J.C.; Carvalho, A.D.A.T.; Gueiros, L.A.M.; Leão, J.C. Dental changes in children with congenital Zika syndrome. Oral Dis. 2020, 26, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Gomes, P.N.; do Amaral, B.A.; Azevedo, I.D.; de Medeiros Maia, H.C.; Arrais, N.M.R.; de Lima, K.C. Association of congenital Zika syndrome with dental alterations in children with microcephaly. PLoS ONE 2022, 17, e0276931. [Google Scholar] [CrossRef] [PubMed]
- Kraan, H.; Vrieling, H.; Czerkinsky, C.; Jiskoot, W.; Kersten, G.; Amorij, J.-P. Buccal and sublingual vaccine delivery. J. Control. Release 2014, 190, 580–592. [Google Scholar] [CrossRef]
- Gala, R.P.; Popescu, C.; Knipp, G.T.; McCain, R.R.; Ubale, R.V.; Addo, R.; Bhowmik, T.; Kulczar, C.D.; D’Souza, M.J. Physicochemical and Preclinical Evaluation of a Novel Buccal Measles Vaccine. AAPS PharmSciTech 2017, 18, 283–292. [Google Scholar] [CrossRef]
- Joshi, D.; Shah, S.; Chbib, C.; Uddin, M.N. Potential of DPD ((S)-4,5-dihydroxy-2,3-pentanedione) Analogs in Microparticulate Formulation as Vaccine Adjuvants. Pharmaceuticals 2024, 17, 184. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Park, C.; Song, I.-O.; Lee, B.-J.; Kang, C.-Y.; Park, J.-B. Investigation of Patient-Centric 3D-Printed Orodispersible Films Containing Amorphous Aripiprazole. Pharmaceuticals 2022, 15, 895. [Google Scholar] [CrossRef]
- Cupone, I.E.; Sansone, A.; Marra, F.; Giori, A.M.; Jannini, E.A. Orodispersible Film (ODF) Platform Based on Maltodextrin for Therapeutical Applications. Pharmaceutics 2022, 14, 2011. [Google Scholar] [CrossRef] [PubMed]
- Scarpa, M.; Paudel, A.; Kloprogge, F.; Hsiao, W.K.; Bresciani, M.; Gaisford, S.; Orlu, M. Key acceptability attributes of orodispersible films. Eur. J. Pharm. Biopharm. 2018, 125, 131–140. [Google Scholar] [CrossRef] [PubMed]
- van Meerloo, J.; Kaspers, G.J.L.; Cloos, J. Cell Sensitivity Assays: The MTT Assay; Humana Press: Totowa, NJ, USA, 2011; pp. 237–245. [Google Scholar] [CrossRef]
- Yu, J.; Song, Y.; Tian, W. How to select IgG subclasses in developing anti-tumor therapeutic antibodies. J. Hematol. Oncol. 2020, 13, 45. [Google Scholar] [CrossRef] [PubMed]
- De Taeye, S.W.; Bentlage, A.E.; Mebius, M.M.; Meesters, J.I.; Lissenberg-Thunnissen, S.; Falck, D.; Sénard, T.; Salehi, N.; Wuhrer, M.; Schuurman, J.; et al. FcγR Binding and ADCC Activity of Human IgG Allotypes. Front. Immunol. 2020, 11, 740. [Google Scholar] [CrossRef] [PubMed]
- Ghasemnejad-Berenji, H.; Novin, M.G.; Hajshafiha, M.; Nazarian, H.; Hashemi, S.M.; Ilkhanizadeh, B.; Ghasemnejad, T.; Sadeghpour, S.; Ghasemnejad-Berenji, M. Immunomodulatory effects of hydroxychloroquine on Th1/Th2 balance in women with repeated implantation failure. Biomed. Pharmacother. 2018, 107, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Leung, S.; Liu, X.; Fang, L.; Chen, X.; Guo, T.; Zhang, J. The cytokine milieu in the interplay of pathogenic Th1/Th17 cells and regulatory T cells in autoimmune disease. Cell. Mol. Immunol. 2010, 7, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Damelang, T.; Rogerson, S.J.; Kent, S.J.; Chung, A.W. Role of IgG3 in Infectious Diseases. Trends Immunol. 2019, 40, 197–211. [Google Scholar] [CrossRef]
- Jones, C.W.; Adams, A.C.; Murphy, E.; King, R.P.; Saracco, B.; Stesis, K.R.; Cavanaugh, S.; Roberts, B.W.; Platts-Mills, T.F. Delays in reporting and publishing trial results during pandemics: Cross sectional analysis of 2009 H1N1, 2014 Ebola, and 2016 Zika clinical trials. BMC Med. Res. Methodol. 2021, 21, 120. [Google Scholar] [CrossRef]
- Essink, B.; Chu, L.; Seger, W.; Barranco, E.; Le Cam, N.; Bennett, H.; Faughnan, V.; Pajon, R.; Paila, Y.D.; Bollman, B.; et al. The safety and immunogenicity of two Zika virus mRNA vaccine candidates in healthy flavivirus baseline seropositive and seronegative adults: The results of two randomised, placebo-controlled, dose-ranging, phase 1 clinical trials. Lancet Infect. Dis. 2023, 23, 621–633. [Google Scholar] [CrossRef] [PubMed]
- McLenon, J.; Rogers, M.A.M. The fear of needles: A systematic review and meta-analysis. J. Adv. Nurs. 2019, 75, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.M.; Alsaab, H.O.; Rawas-Qalaji, M.M.; Uddin, M.N. A Review on Current COVID-19 Vaccines and Evaluation of Particulate Vaccine Delivery Systems. Vaccines 2021, 9, 1086. [Google Scholar] [CrossRef] [PubMed]
- Sarthak, S.; Dedeepya, D.; Emmanuel, A.; Amit, B.; Devyani, J.; Smital, P.; Priyal, B.; Mohammad, N.U.; Martin, D. Vaccine adjuvants and carriers. In Advanced Vaccination Technologies for Infectious and Chronic Diseases; Elsevier: Amsterdam, The Netherlands, 2024; pp. 13–36. [Google Scholar] [CrossRef]
- Nakatogawa, H. Mechanisms governing autophagosome biogenesis. Nat. Rev. Mol. Cell Biol. 2020, 21, 439–458. [Google Scholar] [CrossRef] [PubMed]
- Lőrincz, P.; Juhász, G. Autophagosome-Lysosome Fusion. J. Mol. Biol. 2020, 432, 2462–2482. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Chen, C.C.; Wang, W.B.; Lionel, V.; Liu, C.C.; Huang, L.M.; Wu, S.C. Intranasal Immunization with Zika Virus Envelope Domain III-Flagellin Fusion Protein Elicits Systemic and Mucosal Immune Responses and Protection against Subcutaneous and Intravaginal Virus Challenges. Pharmaceutics 2022, 14, 1014. [Google Scholar] [CrossRef] [PubMed]
- Vidarsson, G.; Dekkers, G.; Rispens, T. IgG Subclasses and Allotypes: From Structure to Effector Functions. Front. Immunol. 2014, 5, 117227. [Google Scholar] [CrossRef] [PubMed]
- Crotty, S. T Follicular Helper Cell Differentiation, Function, and Roles in Disease. Immunity 2014, 41, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Li, Q.; Cai, S.; Peng, H.; Huyan, T.; Yang, H. The role of NK cells in fighting the virus infection and sepsis. Int. J. Med. Sci. 2021, 18, 3236–3248. [Google Scholar] [CrossRef]
- Zuo, W.; Zhao, X. Natural killer cells play an important role in virus infection control: Antiviral mechanism, subset expansion and clinical application. Clin. Immunol. 2021, 227, 108727. [Google Scholar] [CrossRef]







Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shah, S.; Patel, P.; Ferguson, A.; Bagwe, P.; Kale, A.; Adediran, E.; Singh, R.; Arte, T.; Pasupuleti, D.; Uddin, M.N.; et al. Buccal Administration of a Zika Virus Vaccine Utilizing 3D-Printed Oral Dissolving Films in a Mouse Model. Vaccines 2024, 12, 720. https://doi.org/10.3390/vaccines12070720
Shah S, Patel P, Ferguson A, Bagwe P, Kale A, Adediran E, Singh R, Arte T, Pasupuleti D, Uddin MN, et al. Buccal Administration of a Zika Virus Vaccine Utilizing 3D-Printed Oral Dissolving Films in a Mouse Model. Vaccines. 2024; 12(7):720. https://doi.org/10.3390/vaccines12070720
Chicago/Turabian StyleShah, Sarthak, Parth Patel, Amarae Ferguson, Priyal Bagwe, Akanksha Kale, Emmanuel Adediran, Revanth Singh, Tanisha Arte, Dedeepya Pasupuleti, Mohammad N. Uddin, and et al. 2024. "Buccal Administration of a Zika Virus Vaccine Utilizing 3D-Printed Oral Dissolving Films in a Mouse Model" Vaccines 12, no. 7: 720. https://doi.org/10.3390/vaccines12070720
APA StyleShah, S., Patel, P., Ferguson, A., Bagwe, P., Kale, A., Adediran, E., Singh, R., Arte, T., Pasupuleti, D., Uddin, M. N., & D’Souza, M. (2024). Buccal Administration of a Zika Virus Vaccine Utilizing 3D-Printed Oral Dissolving Films in a Mouse Model. Vaccines, 12(7), 720. https://doi.org/10.3390/vaccines12070720










