Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review
Abstract
:1. Introduction
2. Methods
3. COVID-19 Vaccine Hesitancy: Addressing Challenges beyond the Pandemic
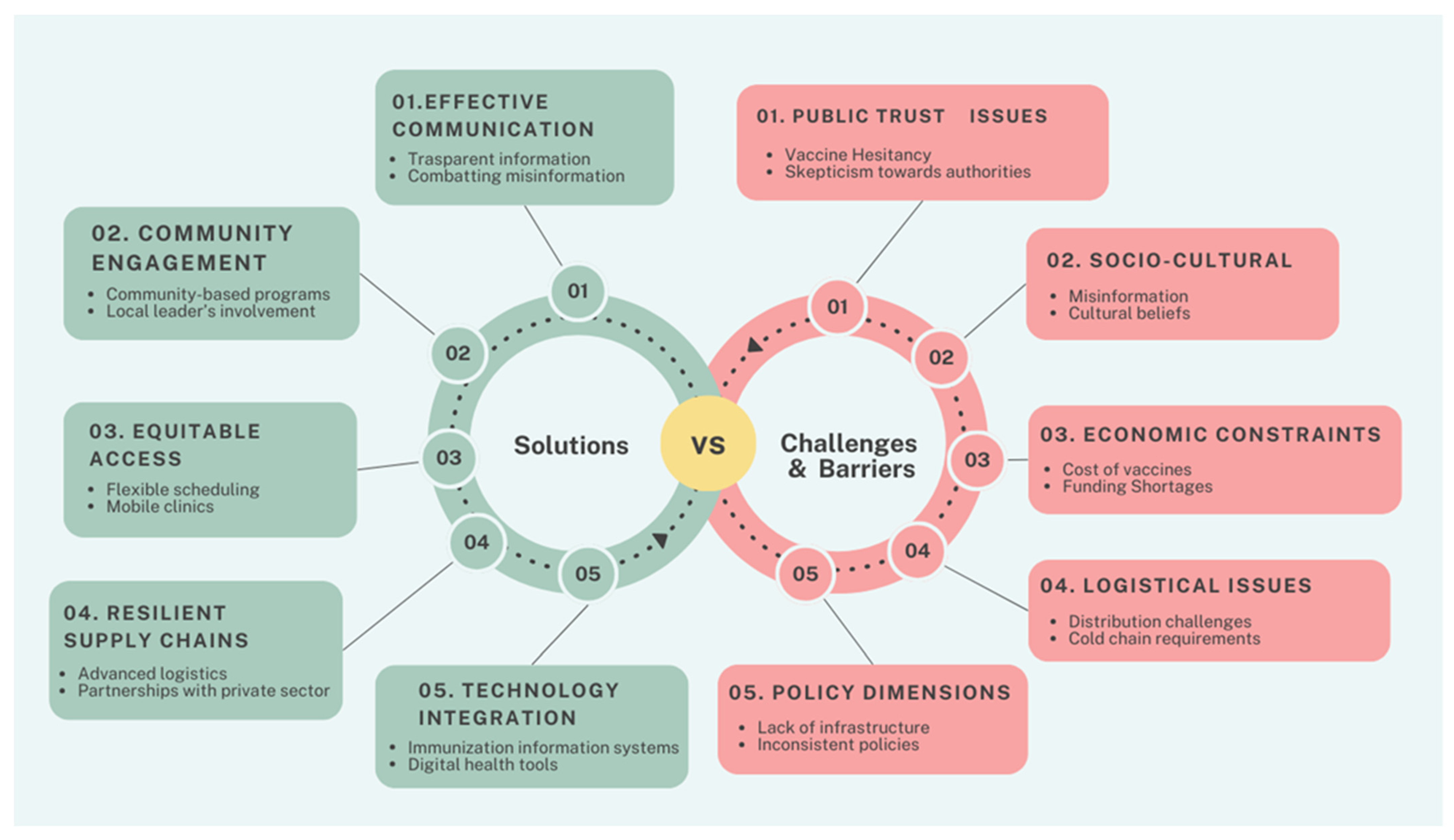
4. Enhancing Vaccine Acceptance: Effective Strategies for Public Health
5. Lessons Learned from Challenges and Barriers of COVID-19 Vaccination Campaigns
6. Overcoming Inequalities in Vaccination Access: Insights from the COVID-19 Campaign
7. Implications for Future Public Health Strategies
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Montero, D.A.; Vidal, R.M.; Velasco, J.; Carreño, L.J.; Torres, J.P.; Benachi, O.M.A.; Tovar-Rosero, Y.Y.; Oñate, A.A.; O’Ryan, M. Two centuries of vaccination: Historical and conceptual approach and future perspectives. Front. Public Health 2024, 11, 1326154. [Google Scholar] [CrossRef] [PubMed]
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Haileamlak, A. The impact of COVID-19 on health and health systems. Ethiop. J. Health Sci. 2021, 31, 1073–1074. [Google Scholar] [CrossRef] [PubMed]
- Sachs, J.D.; Karim, S.S.A.; Aknin, L.; Allen, J.; Brosbol, K.; Colombo, F.; Barron, G.C.; Espinosa, M.F.; Gaspar, V.; Gaviria, A.; et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet 2022, 400, 1224–1280. [Google Scholar] [CrossRef]
- Excler, J.L.; Saville, M.; Privor-Dumm, L.; Gilbert, S.; Hotez, P.J.; Thompson, D.; Abdool-Karim, S.; Kim, J.H. Factors, enablers and challenges for COVID-19 vaccine development. BMJ Glob. Health 2023, 8, e011879. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Chavda, V.P.; Soni, S.; Vora, L.K.; Soni, S.; Khadela, A.; Ajabiya, J. mRNA-Based Vaccines and Therapeutics for COVID-19 and Future Pandemics. Vaccines 2022, 10, 2150. [Google Scholar] [CrossRef] [PubMed]
- Etowa, J.; Beauchamp, S.; Fseifes, M.; Osandatuwa, G.; Brenneman, P.; Salam-Alada, K.; Sulaiman, R.; Okolie, E.; Dinneh, I.; Julmisse, S.; et al. Understanding Low Vaccine Uptake in the Context of Public Health in High-Income Countries: A Scoping Review. Vaccines 2024, 12, 269. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Facilitating COVID-19 Vaccination Acceptance and Uptake in the EU/EEA; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- Nuwarda, R.F.; Ramzan, I.; Weekes, L.; Kayser, V. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines 2022, 10, 1595. [Google Scholar] [CrossRef] [PubMed]
- Cella, P.; Voglino, G.; Barberis, I.; Alagna, E.; Alessandroni, C.; Cuda, A.; D’aloisio, F.; Dallagiacoma, G.; De Nitto, S.; Di Gaspare, F.; et al. Resources for assessing parents’ vaccine hesitancy: A systematic review of the literature. J. Prev. Med. Hyg. 2020, 61, E340–E373. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, S.; Cummings, C.L. Influence of rapid COVID-19 vaccine development on vaccine hesitancy. Vaccine 2021, 39, 7625–7632. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Stefanizzi, P.; Berti, A.; D’Amico, M.; De Lorenzo, V.; Lorenzo, A.D.; Moscara, L.; Castaldi, S. A Systematic Review of Population-Based Studies Assessing Knowledge, Attitudes, Acceptance, and Hesitancy of Pregnant and Breastfeeding Women towards the COVID-19 Vaccine. Vaccines 2023, 11, 1289. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Berti, A.; Stefanizzi, P.; D’Amico, M.; De Lorenzo, V.; Moscara, L.; Di Lorenzo, A.; Venerito, V.; Castaldi, S. COVID-19 Vaccine Knowledge, Attitude, Acceptance and Hesitancy among Pregnancy and Breastfeeding: Systematic Review of Hospital-Based Studies. Vaccines 2023, 11, 1697. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Odone, A.; Fiacchini, D.; Rosselu, R.; Battista, T.; Signorelli, C. Trust and reputation management, branding, social media management nelle organizzazioni sanitarie: Sfide e opportunity per la comunita igienistica italiana. J. Prev. Med. Hyg. 2019, 60, E108–E109. [Google Scholar]
- Fitzpatrick, P.J. Improving health literacy using the power of digital communications to achieve better health outcomes for patients and practitioners. Front. Digit. Health 2023, 5, 1264780. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-A. COVID-19 vaccine communication and advocacy strategy: A social marketing campaign for increasing COVID-19 vaccine uptake in South Korea. Humanit. Soc. Sci. Commun. 2023, 10, 109. [Google Scholar] [CrossRef] [PubMed]
- Lanza, T.E.; Paladini, A.; Marziali, E.; Gianfredi, V.; Blandi, L.; Signorelli, C.; Odone, A.; Ricciardi, W.; Damiani, G.; Cadeddu, C. Training needs assessment of European frontline health care workers on vaccinology and vaccine acceptance: A systematic review. Eur. J. Public Health 2023, 33, 591–595. [Google Scholar] [CrossRef]
- Gianfredi, V.; Oradini-Alacreu, A.; Sá, R.; Blandi, L.; Cadeddu, C.; Ricciardi, W.; Signorelli, C.; Odone, A. Frontline health workers: Training needs assessment on immunisation programme. An EU/EEA-based survey. J. Public Health 2023. [Google Scholar] [CrossRef]
- Odone, A.; Gianfredi, V.; Frascella, B.; Balzarini, F.; Alacreu, A.O.; Signorelli, C. Digitalization of immunization programmes in Europe: Results from the EUVIS project. Eur. J. Public Health 2020, 30, V7. [Google Scholar] [CrossRef]
- Gianfredi, V.; Moretti, M.; Lopalco, P.L. Countering vaccine hesitancy through immunization information systems, a narrative review. Hum. Vaccin. Immunother. 2019, 15, 2508–2526. [Google Scholar] [CrossRef]
- D’Ancona, F.; Gianfredi, V.; Riccardo, F.; Iannazzo, S. Immunisation Registries at regional level in Italy and the roadmap for a future Italian National Registry. Ann. Ig. 2018, 30, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; D’Ancona, F.; Maraglino, F.; Cenci, C.; Iannazzo, S. Polio and measles: Reasons of missed vaccination in Italy, 2015–2017. Ann. Ig. 2019, 31, 191–201. [Google Scholar] [CrossRef]
- Fokoun, C. Strategies implemented to address vaccine hesitancy in France: A review article. Hum. Vaccines Immunother. 2018, 14, 1580–1590. [Google Scholar] [CrossRef] [PubMed]
- Desborough, J.; Wright, M.; Parkinson, A.; Hall Dykgraaf, S.; Ball, L.; Dut, G.M.; Sturgiss, E.; de Toca, L.; Kidd, M. What strategies have been effective in optimising COVID-19 vaccine uptake in Australia and internationally? Aust. J. Gen. Pr. 2022, 51, 725–730. [Google Scholar] [CrossRef]
- Scott, T.; Gutschow, B.; Ragavan, M.I.; Ho, K.; Massart, M.; Ripper, L.; Muthama, V.; Miller, E.; Bey, J.; Abernathy, R.P. A Community Partnered Approach to Promoting COVID-19 Vaccine Equity. Health Promot. Pr. 2021, 22, 758–760. [Google Scholar] [CrossRef]
- Ratzan, S.; Schneider, E.C.; Hatch, H.; Cacchione, J. Missing the Point—How Primary Care Can Overcome COVID-19 Vaccine “Hesitancy”. N. Engl. J. Med. 2021, 384, e100. [Google Scholar] [CrossRef]
- Sinuraya, R.K.; Nuwarda, R.F.; Postma, M.J.; Suwantika, A.A. Vaccine hesitancy and equity: Lessons learned from the past and how they affect the COVID-19 countermeasure in Indonesia. Glob. Health 2024, 20, 11. [Google Scholar] [CrossRef]
- Barry, V.; Dasgupta, S.; Weller, D.L.; Kriss, J.L.; Cadwell, B.L.; Rose, C.; Pingali, C.; Musial, T.; Sharpe, J.D.; Flores, S.A.; et al. Patterns in COVID-19 Vaccination Coverage, by Social Vulnerability and Urbanicity—United States, December 14, 2020–May 1, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 818–824. [Google Scholar] [CrossRef]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.A.; Failla, G.; Puleo, V.; Melnyk, A.; Lontano, A.; Ricciardi, W. Social media and attitudes towards a COVID-19 vaccination: A systematic review of the literature. EClinicalMedicine 2022, 48, 101454. [Google Scholar] [CrossRef]
- Feifer, R.A.; Bethea, L.; White, E.M. Racial Disparities in COVID-19 Vaccine Acceptance: Building Trust to Protect Nursing Home Staff and Residents. J. Am. Med. Dir. Assoc. 2021, 22, 1853–1855.e1851. [Google Scholar] [CrossRef]
- Batteux, E.; Mills, F.; Jones, L.F.; Symons, C.; Weston, D. The Effectiveness of Interventions for Increasing COVID-19 Vaccine Uptake: A Systematic Review. Vaccines 2022, 10, 386. [Google Scholar] [CrossRef]
- Hernandez, R.G.; Hagen, L.; Walker, K.; O’Leary, H.; Lengacher, C. The COVID-19 vaccine social media infodemic: Healthcare providers’ missed dose in addressing misinformation and vaccine hesitancy. Hum. Vaccin. Immunother. 2021, 17, 2962–2964. [Google Scholar] [CrossRef]
- Budhwani, H.; Maragh-Bass, A.C.; Tolley, E.E.; Comello, M.L.G.; Stoner, M.C.D.; Adams Larsen, M.; Brambilla, D.; Muessig, K.E.; Pettifor, A.; Bond, C.L.; et al. Tough Talks COVID-19 Digital Health Intervention for Vaccine Hesitancy Among Black Young Adults: Protocol for a Hybrid Type 1 Effectiveness Implementation Randomized Controlled Trial. JMIR Res. Protoc. 2023, 12, e41240. [Google Scholar] [CrossRef] [PubMed]
- Ngai, C.S.B.; Singh, R.G.; Yao, L. Impact of COVID-19 Vaccine Misinformation on Social Media Virality: Content Analysis of Message Themes and Writing Strategies. J. Med. Internet Res. 2022, 24, e37806. [Google Scholar] [CrossRef]
- Dube, E.; Labbe, F.; Malo, B.; Pelletier, C. Public health communication during the COVID-19 pandemic: Perspectives of communication specialists, healthcare professionals, and community members in Quebec, Canada. Can. J. Public Health 2022, 113 (Suppl. S1), 24–33. [Google Scholar] [CrossRef] [PubMed]
- Lowe, M.; Harmon, S.H.E.; Kholina, K.; Parker, R.; Graham, J.E. Public health communication in Canada during the COVID-19 pandemic. Can. J. Public Health 2022, 113 (Suppl. S1), 34–45. [Google Scholar] [CrossRef] [PubMed]
- Krastev, S.; Krajden, O.; Vang, Z.M.; Perez-Gay Juarez, F.; Solomonova, E.; Goldenberg, M.; Weinstock, D.; Smith, M.J.; Turk, L.; Lin, X.; et al. Navigating the uncertainty: A novel taxonomy of vaccine hesitancy in the context of COVID-19. PLoS ONE 2023, 18, e0295912. [Google Scholar] [CrossRef]
- Pinaka, O.; Spanou, I.; Papadouli, V.; Papanikolaou, E.; Gioulekas, F.; Mouchtouri, V.A. The role of local primary healthcare units in increasing immunization uptake among children in vulnerable social groups through vaccination campaigns. Public Health Pr. 2021, 2, 100185. [Google Scholar] [CrossRef]
- Gianfredi, V.; Pennisi, F.; Lume, A.; Ricciardi, G.E.; Minerva, M.; Ricco, M.; Odone, A.; Signorelli, C. Challenges and Opportunities of Mass Vaccination Centers in COVID-19 Times: A Rapid Review of Literature. Vaccines 2021, 9, 574. [Google Scholar] [CrossRef]
- Pennisi, F.; Mastrangelo, M.; De Ponti, E.; Cuciniello, R.; Mandelli, A.; Vaia, F.; Signorelli, C. The role of pharmacies in the implementation of vaccination cover- age in Italy. Insights from the preliminary data of the Lombardy Region. Ann. Ig. 2024, 36, 363–369. [Google Scholar] [CrossRef]
- Gianfredi, V.; Nucci, D.; Salvatori, T.; Orlacchio, F.; Villarini, M.; Moretti, M. “PErCEIVE in Umbria”: Evaluation of anti-influenza vaccination’s perception among Umbrian pharmacists. J. Prev. Med. Hyg. 2018, 59, E14–E19. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.T.; Althomsons, S.P.; Wu, H.; Budnitz, D.S.; Kalayil, E.J.; Lindley, M.C.; Pingali, C.; Bridges, C.B.; Geller, A.I.; Fiebelkorn, A.P.; et al. Disparities in COVID-19 Vaccination Coverage Among Health Care Personnel Working in Long-Term Care Facilities, by Job Category, National Healthcare Safety Network—United States, March 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1036–1039. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization and the United Nations Children’s Fund. Considerations for Integrating COVID-19 Vaccination into Immunization Programmes and Primary Health Care for 2022 and Beyond; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Albarracin, D.; Jung, H.; Song, W.; Tan, A.; Fishman, J. Rather than inducing psychological reactance, requiring vaccination strengthens intentions to vaccinate in US populations. Sci. Rep. 2021, 11, 20796. [Google Scholar] [CrossRef] [PubMed]
- De Giorgio, A.; Kuvacic, G.; Males, D.; Vecchio, I.; Tornali, C.; Ishac, W.; Ramaci, T.; Barattucci, M.; Milavic, B. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines 2022, 10, 481. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, S.M.; Dehom, S.; Almutairi, D.; Alnasser, B.S.; Alsaif, B.; Alabdrabalnabi, A.A.; Bin Rahmah, A.; Alshahrani, M.S.; El-Metwally, A.; Al-Khateeb, B.F.; et al. Acceptability of COVID-19 vaccination in Saudi Arabia: A cross-sectional study using a web-based survey. Hum. Vaccin. Immunother. 2021, 17, 3338–3347. [Google Scholar] [CrossRef]
- de Figueiredo, A.; Larson, H.J.; Reicher, S.D. The potential impact of vaccine passports on inclination to accept COVID-19 vaccinations in the United Kingdom: Evidence from a large cross-sectional survey and modeling study. EClinicalMedicine 2021, 40, 101109. [Google Scholar] [CrossRef] [PubMed]
- Natalia, Y.A.; Delporte, M.; De Witte, D.; Beutels, P.; Dewatripont, M.; Molenberghs, G. Assessing the impact of COVID-19 passes and mandates on disease transmission, vaccination intention, and uptake: A scoping review. BMC Public Health 2023, 23, 2279. [Google Scholar] [CrossRef]
- Radic, A.; Koo, B.; Kim, J.J.; Han, H. No jab, no international travel? Linking TRA, mass media, motivation, and experience. J. Vacat. Mark. 2023, 29, 365–385. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Cheung, A.W.L.; Huang, J.; Lai, C.K.C.; Yeoh, E.K.; Chan, P.K.S. COVID-19 Vaccine Hesitancy in a City with Free Choice and Sufficient Doses. Vaccines 2021, 9, 1250. [Google Scholar] [CrossRef]
- Oliu-Barton, M.; Pradelski, B.S.R.; Woloszko, N.; Guetta-Jeanrenaud, L.; Aghion, P.; Artus, P.; Fontanet, A.; Martin, P.; Wolff, G.B. The effect of COVID certificates on vaccine uptake, health outcomes, and the economy. Nat. Commun. 2022, 13, 3942. [Google Scholar] [CrossRef]
- Kluver, H.; Hartmann, F.; Humphreys, M.; Geissler, F.; Giesecke, J. Incentives can spur COVID-19 vaccination uptake. Proc. Natl. Acad. Sci. USA 2021, 118, e2109543118. [Google Scholar] [CrossRef]
- Mills, M.C.; Ruttenauer, T. The effect of mandatory COVID-19 certificates on vaccine uptake: Synthetic-control modelling of six countries. Lancet Public Health 2022, 7, e15–e22. [Google Scholar] [CrossRef]
- Walkowiak, M.P.; Walkowiak, J.B.; Walkowiak, D. COVID-19 Passport as a Factor Determining the Success of National Vaccination Campaigns: Does It Work? The Case of Lithuania vs. Poland. Vaccines 2021, 9, 1498. [Google Scholar] [CrossRef]
- Khazanov, G.K.; Stewart, R.; Pieri, M.F.; Huang, C.; Robertson, C.T.; Schaefer, K.A.; Ko, H.; Fishman, J. The effectiveness of financial incentives for COVID-19 vaccination: A systematic review. Prev. Med. 2023, 172, 107538. [Google Scholar] [CrossRef]
- McCosker, L.K.; Ware, R.S.; Seale, H.; Hooshmand, D.; O’Leary, R.; Downes, M.J. The effect of a financial incentive on COVID-19 vaccination uptake, and predictors of uptake, in people experiencing homelessness: A randomized controlled trial. Vaccine 2024, 42, 2578–2584. [Google Scholar] [CrossRef]
- Terrell, R.; Alami, A.; Krewski, D. Interventions for COVID-19 Vaccine Hesitancy: A Systematic Review and Narrative Synthesis. Int. J. Environ. Res. Public Health 2023, 20, 6082. [Google Scholar] [CrossRef] [PubMed]
- Barber, A.; West, J. Conditional cash lotteries increase COVID-19 vaccination rates. J. Health Econ. 2022, 81, 102578. [Google Scholar] [CrossRef]
- Alam, S.T.; Ahmed, S.; Ali, S.M.; Sarker, S.; Kabir, G. Challenges to COVID-19 vaccine supply chain: Implications for sustainable development goals. Int. J. Prod. Econ. 2021, 239, 108193. [Google Scholar] [CrossRef] [PubMed]
- Tagoe, E.T.; Sheikh, N.; Morton, A.; Nonvignon, J.; Sarker, A.R.; Williams, L.; Megiddo, I. COVID-19 Vaccination in Lower-Middle Income Countries: National Stakeholder Views on Challenges, Barriers, and Potential Solutions. Front. Public Health 2021, 9, 709127. [Google Scholar] [CrossRef] [PubMed]
- Fahrni, M.L.; Ismail, I.A.; Refi, D.M.; Almeman, A.; Yaakob, N.C.; Saman, K.M.; Mansor, N.F.; Noordin, N.; Babar, Z.U. Management of COVID-19 vaccines cold chain logistics: A scoping review. J. Pharm. Policy Pr. 2022, 15, 16. [Google Scholar] [CrossRef]
- Chakraborty, C.; Bhattacharya, M.; Dhama, K. SARS-CoV-2 Vaccines, Vaccine Development Technologies, and Significant Efforts in Vaccine Development during the Pandemic: The Lessons Learned Might Help to Fight against the Next Pandemic. Vaccines 2023, 11, 682. [Google Scholar] [CrossRef]
- Khan, W.H.; Hashmi, Z.; Goel, A.; Ahmad, R.; Gupta, K.; Khan, N.; Alam, I.; Ahmed, F.; Ansari, M.A. COVID-19 pandemic and vaccines update on challenges and resolutions. Front. Cell. Infect. Microbiol. 2021, 11, 690621. [Google Scholar] [CrossRef] [PubMed]
- Gong, W.; Parkkila, S.; Wu, X.; Aspatwar, A. SARS-CoV-2 variants and COVID-19 vaccines: Current challenges and future strategies. Int. Rev. Immunol. 2023, 42, 393–414. [Google Scholar] [CrossRef]
- Signorelli, C.; De Ponti, E.; Mastrangelo, M.; Pennisi, F.; Cereda, D.; Corti, F.; Beretta, D.; Pelissero, G. The contribution of the private healthcare sector during the COVID-19 pandemic: The experience of the Lombardy Region in Northern Italy. Ann. Ig. 2024, 36, 250–255. [Google Scholar] [CrossRef]
- McCready, J.L.; Nichol, B.; Steen, M.; Unsworth, J.; Comparcini, D.; Tomietto, M. Understanding the barriers and facilitators of vaccine hesitancy towards the COVID-19 vaccine in healthcare workers and healthcare students worldwide: An Umbrella Review. PLoS ONE 2023, 18, e0280439. [Google Scholar] [CrossRef]
- Nair, L.; Adetayo, O.A. Cultural Competence and Ethnic Diversity in Healthcare. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2219. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.M.; Scrimshaw, S.C.; Fullilove, M.T.; Fielding, J.E.; Normand, J.; Task Force on Community Preventive, S. Culturally competent healthcare systems. A systematic review. Am. J. Prev. Med. 2003, 24, 68–79. [Google Scholar] [CrossRef]
- Ashfield, S.; Donelle, L.; Uppal, G.; Bauer, M.A.; Kothari, A. Community organization perspectives on COVID-19 vaccine hesitancy and how they increased COVID-19 vaccine confidence: A Canadian Immunization Research Network, social sciences and humanities network study. Front. Public Health 2023, 11, 1258742. [Google Scholar] [CrossRef] [PubMed]
- Dube, E.; Gagnon, D.; MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef]
- Opel, D.J.; Mangione-Smith, R.; Robinson, J.D.; Heritage, J.; DeVere, V.; Salas, H.S.; Zhou, C.; Taylor, J.A. The Influence of Provider Communication Behaviors on Parental Vaccine Acceptance and Visit Experience. Am. J. Public Health 2015, 105, 1998–2004. [Google Scholar] [CrossRef]
- Kaholokula, J.K.; Ing, C.T.; Look, M.A.; Delafield, R.; Sinclair, K. Culturally responsive approaches to health promotion for Native Hawaiians and Pacific Islanders. Ann. Hum. Biol. 2018, 45, 249–263. [Google Scholar] [CrossRef] [PubMed]
- AuYoung, M.; Rodriguez Espinosa, P.; Chen, W.T.; Juturu, P.; Young, M.T.; Casillas, A.; Adkins-Jackson, P.; Hopfer, S.; Kissam, E.; Alo, A.K.; et al. Addressing racial/ethnic inequities in vaccine hesitancy and uptake: Lessons learned from the California alliance against COVID-19. J. Behav. Med. 2023, 46, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Sacre, A.; Bambra, C.; Wildman, J.M.; Thomson, K.; Bennett, N.; Sowden, S.; Todd, A. Socioeconomic inequalities in vaccine uptake: A global umbrella review. PLoS ONE 2023, 18, e0294688. [Google Scholar] [CrossRef] [PubMed]
- Flores-Landeros, H.; Pells, C.; Campos-Martinez, M.S.; Fernandez-Bou, A.S.; Ortiz-Partida, J.P.; Medellín-Azuara, J. Community perspectives and environmental justice in California’s San Joaquin Valley. Environ. Justice 2022, 15, 337–345. [Google Scholar] [CrossRef]
- Zhang, X.; Tulloch, J.S.P.; Knott, S.; Allison, R.; Parvulescu, P.; Buchan, I.E.; Garcia-Finana, M.; Piroddi, R.; Green, M.A.; Baird, S.; et al. Evaluating the impact of using mobile vaccination units to increase COVID-19 vaccination uptake in Cheshire and Merseyside, UK: A synthetic control analysis. BMJ Open 2023, 13, e071852. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, E.M.D.; Shadlen, K.C.; Achcar, H.M. Vaccine technology transfer in a global health crisis: Actors, capabilities, and institutions. Res. Policy 2023, 52, 104739. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Kern, A.; Buchanan, A.; Fabre, C.; Halliday, D.; Heath, J.; Herzog, L.; Leland, R.J.; Lemango, E.T.; et al. An ethical framework for global vaccine allocation. Science 2020, 369, 1309–1312. [Google Scholar] [CrossRef]
- Asundi, A.; O’Leary, C.; Bhadelia, N. Global COVID-19 vaccine inequity: The scope, the impact, and the challenges. Cell Host Microbe 2021, 29, 1036–1039. [Google Scholar] [CrossRef] [PubMed]
- The, L. Access to COVID-19 vaccines: Looking beyond COVAX. Lancet 2021, 397, 941. [Google Scholar] [CrossRef]
- Gozzi, N.; Chinazzi, M.; Dean, N.E.; Longini, I.M., Jr.; Halloran, M.E.; Perra, N.; Vespignani, A. Estimating the impact of COVID-19 vaccine inequities: A modeling study. Nat. Commun. 2023, 14, 3272. [Google Scholar] [CrossRef]
- Kaiser, N.; Barstow, C.K. Rural Transportation Infrastructure in Low- and Middle-Income Countries: A Review of Impacts, Implications, and Interventions. Sustainability 2022, 14, 2149. [Google Scholar] [CrossRef]
- Oladimeji, D.; Gupta, K.; Kose, N.A.; Gundogan, K.; Ge, L.; Liang, F. Smart Transportation: An Overview of Technologies and Applications. Sensors 2023, 23, 3880. [Google Scholar] [CrossRef] [PubMed]
- Gianfredi, V.; Filia, A.; Rota, M.C.; Croci, R.; Bellini, L.; Odone, A.; Signorelli, C. Vaccine Procurement: A Conceptual Framework Based on Literature Review. Vaccines 2021, 9, 1434. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Kletter, M.; Dumville, J. Interventions to increase vaccination in vulnerable groups: Rapid overview of reviews. BMC Public Health 2024, 24, 1479. [Google Scholar] [CrossRef]
- Peters, M.D. Addressing vaccine hesitancy and resistance for COVID-19 vaccines. Int. J. Nurs. Stud. 2022, 131, 104241. [Google Scholar] [CrossRef] [PubMed]
- Jabbar, F.; Kadhim, K.A.; Alhilfi, R.A.; Chitheer, A.; Rahi, A.; Hipgrave, D.B. Intensification of integrated immunization services to recover routine vaccination coverage and bring COVID-19 vaccine to the population of Iraq in 2022. Vaccine 2024, 42, 2036–2043. [Google Scholar] [CrossRef] [PubMed]
- Krzysztofowicz, S.; Osinska-Skotak, K. The Use of GIS Technology to Optimize COVID-19 Vaccine Distribution: A Case Study of the City of Warsaw, Poland. Int. J. Env. Res. Public Health 2021, 18, 5636. [Google Scholar] [CrossRef] [PubMed]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef] [PubMed]
- Ghaemmaghamian, Z.; Zarghami, R.; Walker, G.; O’Reilly, E.; Ziaee, A. Stabilizing vaccines via drying: Quality by design considerations. Adv. Drug Deliv. Rev. 2022, 187, 114313. [Google Scholar] [CrossRef]
- Gianfredi, V.; Monarca, S.; Moretti, M.; Villarini, M. Health education, what is the role for pharmacist? Results from a cross sectional study in Umbria, Italy. Recent. Prog. Med. 2017, 108, 433–441. [Google Scholar] [CrossRef]
- Lieneck, C.; Heinemann, K.; Patel, J.; Huynh, H.; Leafblad, A.; Moreno, E.; Wingfield, C. Facilitators and Barriers of COVID-19 Vaccine Promotion on Social Media in the United States: A Systematic Review. Healthcare 2022, 10, 321. [Google Scholar] [CrossRef] [PubMed]
- Khoury, G.; Ward, J.K.; Mancini, J.; Gagneux-Brunon, A.; Luong Nguyen, L.B. Health Literacy and Health Care System Confidence as Determinants of Attitudes to Vaccines in France: Representative Cross-Sectional Study. JMIR Public Health Surveill. 2024, 10, e45837. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pennisi, F.; Genovese, C.; Gianfredi, V. Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review. Vaccines 2024, 12, 891. https://doi.org/10.3390/vaccines12080891
Pennisi F, Genovese C, Gianfredi V. Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review. Vaccines. 2024; 12(8):891. https://doi.org/10.3390/vaccines12080891
Chicago/Turabian StylePennisi, Flavia, Cristina Genovese, and Vincenza Gianfredi. 2024. "Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review" Vaccines 12, no. 8: 891. https://doi.org/10.3390/vaccines12080891






