Host Immune Response to Bovine Viral Diarrhea Virus (BVDV): Insights and Strategies for Effective Vaccine Design
Abstract
1. Introduction
2. Methodology
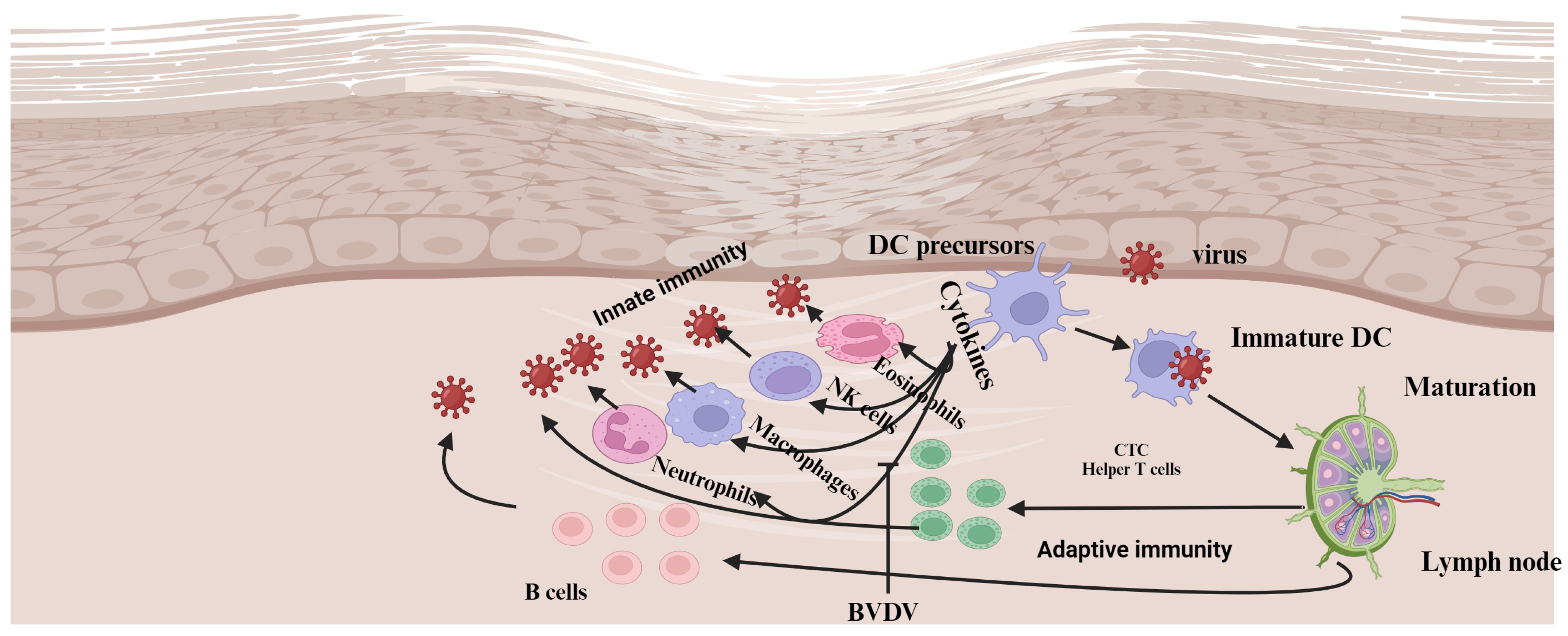
3. BVDV and the Innate Immune System
3.1. Interferon α/β
3.2. BVDV Triggers Apoptosis
3.3. BVDV and Innate Immune Cells
3.3.1. Neutrophils
3.3.2. Macrophages
3.3.3. Antigen Processing and Presenting Cells (APCs)
4. Adaptive Immune System
5. BVDV and Maternal Antibody (MatAb)
6. BVDV Vaccines and Application
6.1. Conventional Vaccines
6.2. Next-Generation Vaccines
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Szabára, Á.; Ózsvári, L. Economic impacts, control and eradication of Bovine Viral Diarrhoea virus. In Challenges for the Agricultural Sector in Central and Eastern Europe; Agroinform Kiadó: Budapest, Hungary, 2014; pp. 247–258. [Google Scholar] [CrossRef]
- Khodakaram-Tafti, A.; Farjanikish, G.H. Persistent bovine viral diarrhea virus (BVDV) infection in cattle herds. Iran. J. Vet. Res. 2017, 18, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.B.; Meyers, G.; Bukh, J.; Gould, E.A.; Monath, T.; Muerhoff, A.S.; Pletnev, A.; Rico-Hesse, R.; Stapleton, J.T.; Simmonds, P.; et al. Proposed revision to the taxonomy of the genus Pestivirus, family Flaviviridae. J. Gen. Virol. 2017, 98, 2106–2112. [Google Scholar] [CrossRef]
- Ammari, M.; McCarthy, F.M.; Nanduri, B.; Pinchuk, L.M. Analysis of Bovine Viral Diarrhea Viruses-infected monocytes: Identification of cytopathic and non-cytopathic biotype differences. BMC Bioinform. 2010, 11, 9. [Google Scholar] [CrossRef]
- Hilleman, M.R. Strategies and mechanisms for host and pathogen survival in acute and persistent viral infections. Proc. Natl. Acad. Sci. USA 2004, 101, 14560–14566. [Google Scholar] [CrossRef] [PubMed]
- Vlasova, A.N.; Saif, L.J. Bovine Immunology: Implications for Dairy Cattle. Front. Immunol. 2021, 12, 643206. [Google Scholar] [CrossRef]
- Chase, C.C.L. The impact of BVDV infection on adaptive immunity. Biologicals 2013, 41, 52–60. [Google Scholar] [CrossRef]
- Givens, M.D.; Marley, M.S. Immunology of chronic BVDV infections. Biologicals 2013, 41, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Fulton, R.W.; Cook, B.J.; Payton, M.E.; Burge, L.J.; Step, D.L. Immune response to bovine viral diarrhea virus (BVDV) vaccines detecting antibodies to BVDV subtypes 1a, 1b, 2a, and 2c. Vaccine 2020, 38, 4032–4037. [Google Scholar] [CrossRef]
- Falkenberg, S.M.; Dassanayake, R.P.; Terhaar, B.; Ridpath, J.F.; Neill, J.D.; Roth, J.A. Evaluation of Antigenic Comparisons Among BVDV Isolates as it Relates to Humoral and Cell Mediated Responses. Front. Vet. Sci. 2021, 8, 685114. [Google Scholar] [CrossRef]
- Sangewar, N.; Hassan, W.; Lokhandwala, S.; Bray, J.; Reith, R.; Markland, M.; Sang, H.; Yao, J.; Fritz, B.; Waghela, S.D.; et al. Mosaic Bovine Viral Diarrhea Virus Antigens Elicit Cross-Protective Immunity in Calves. Front. Immunol. 2020, 11, 589537. [Google Scholar] [CrossRef]
- Lokhandwala, S.; Fang, X.; Waghela, S.D.; Bray, J.; Njongmeta, L.M.; Herring, A.; Abdelsalam, K.W.; Chase, C.; Mwangi, W. Priming cross-protective bovine viral diarrhea virus-specific immunity using live-vectored mosaic antigens. PLoS ONE 2017, 12, e0170425. [Google Scholar] [CrossRef]
- Brackenbury, L.S.; Carr, B.V.; Charleston, B. Aspects of the innate and adaptive immune responses to acute infections with BVDV. Vet. Microbiol. 2003, 96, 337–344. [Google Scholar] [CrossRef]
- Williams, J. A Comprehensive Review of Seven Steps to a Comprehensive Literature Review. Qual. Rep. 2018, 23, 345–349. [Google Scholar] [CrossRef]
- Bencze, D.; Fekete, T.; Pázmándi, K. Type i interferon production of plasmacytoid dendritic cells under control. Int. J. Mol. Sci. 2021, 22, 4190. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, M.; Mätzener, P.; Pfaffen, G.; Stalder, H.; Peterhans, E. “Self” and “Nonself” Manipulation of Interferon Defense during Persistent Infection: Bovine Viral Diarrhea Virus Resists Alpha/Beta Interferon without Blocking Antiviral Activity against Unrelated Viruses Replicating in Its Host Cells. J. Virol. 2006, 80, 6926–6935. [Google Scholar] [CrossRef]
- Daniel Givens, M.; Marley, M.S.D.; Jones, C.A.; Ensley, D.T.; Galik, P.K.; Zhang, Y.; Riddell, K.P.; Joiner, K.S.; Brodersen, B.W.; Rodning, S.P. Protective effects against abortion and fetal infection following exposure to bovine viral diarrhea virus and bovine herpesvirus 1 during pregnancy in beef heifers that received two doses of a multivalent modified-live virus vaccine prior to breeding. J. Am. Vet. Med. Assoc. 2012, 241, 484–495. [Google Scholar] [CrossRef] [PubMed]
- Chase, C.C.L.; Thakur, N.; Darweesh, M.F.; Morarie-Kane, S.E.; Rajput, M.K. Immune response to bovine viral diarrhea virus—Looking at newly defined targets. Anim. Health Res. Rev. 2015, 16, 4–14. [Google Scholar] [CrossRef]
- Schweizer, M.; Peterhans, E. Pestiviruses. Annu. Rev. Anim. Biosci. 2014, 2, 141–163. [Google Scholar] [CrossRef] [PubMed]
- Gil, L.H.V.G.; Ansari, I.H.; Vassilev, V.; Liang, D.; Lai, V.C.H.; Zhong, W.; Hong, Z.; Dubovi, E.J.; Donis, R.O. The Amino-Terminal Domain of Bovine Viral Diarrhea Virus N pro Protein Is Necessary for Alpha/Beta Interferon Antagonism. J. Virol. 2006, 80, 900–911. [Google Scholar] [CrossRef]
- Hong, T.; Yang, Y.; Wang, P.; Zhu, G.; Zhu, C. Pestiviruses infection: Interferon-virus mutual regulation. Front. Cell. Infect. Microbiol. 2023, 13, 1146394. [Google Scholar] [CrossRef]
- Hilton, L.; Moganeradj, K.; Zhang, G.; Chen, Y.-H.; Randall, R.E.; McCauley, J.W.; Goodbourn, S. The NPro Product of Bovine Viral Diarrhea Virus Inhibits DNA Binding by Interferon Regulatory Factor 3 and Targets It for Proteasomal Degradation. J. Virol. 2006, 80, 11723–11732. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Rijnbrand, R.; Jangra, R.K.; Devaraj, S.G.; Qu, L.; Ma, Y.; Lemon, S.M.; Li, K. Ubiquitination and proteasomal degradation of interferon regulatory factor-3 induced by Npro from a cytopathic bovine viral diarrhea virus. Virology 2007, 366, 277–292. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, Y.; Zhao, B.; Xue, Q.; Wang, C.; Wan, S.; Wang, J.; Chen, X.; Qi, X. Non-cytopathic bovine viral diarrhea virus (BVDV) inhibits innate immune responses via induction of mitophagy. Vet. Res. 2024, 55, 27. [Google Scholar] [CrossRef] [PubMed]
- Peterhans, E.; Schweizer, M. BVDV: A pestivirus inducing tolerance of the innate immune response. Biologicals 2013, 41, 39–51. [Google Scholar] [CrossRef]
- Ruggli, N.; Bird, B.H.; Liu, L.; Bauhofer, O.; Tratschin, J.D.; Hofmann, M.A. Npro of classical swine fever virus is an antagonist of double-stranded RNA-mediated apoptosis and IFN-α/β induction. Virology 2005, 340, 265–276. [Google Scholar] [CrossRef]
- Smirnova, N.P.; Bielefeldt-Ohmann, H.; Van Campen, H.; Austin, K.J.; Han, H.; Montgomery, D.L.; Shoemaker, M.L.; van Olphen, A.L.; Hansen, T.R. Acute non-cytopathic bovine viral diarrhea virus infection induces pronounced type I interferon response in pregnant cows and fetuses. Virus Res. 2008, 132, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Peterhans, E.; Jungi, T.W.; Schweizer, M. BVDV and innate immunity. Biologicals 2003, 31, 107–112. [Google Scholar] [CrossRef]
- Schweizer, M.; Peterhans, E. Noncytopathic Bovine Viral Diarrhea Virus Inhibits Double-Stranded RNA-Induced Apoptosis and Interferon Synthesis. J. Virol. 2001, 75, 4692–4698. [Google Scholar] [CrossRef]
- Pang, F.; Long, Q.; Wei, M. Immune evasion strategies of bovine viral diarrhea virus. Front. Cell. Infect. Microbiol. 2023, 13, 1282526. [Google Scholar] [CrossRef]
- Grummer, B.; Bendfeldt, S.; Wagner, B.; Greiser-Wilke, I. Induction of the intrinsic apoptotic pathway in cells infected with cytopathic bovine virus diarrhoea virus. Virus Res. 2002, 90, 143–153. [Google Scholar] [CrossRef]
- Hilbe, M.; Girao, V.; Bachofen, C.; Schweizer, M.; Zlinszky, K.; Ehrensperger, F. Apoptosis in Bovine Viral Diarrhea Virus (BVDV)-Induced Mucosal Disease Lesions: A Histological, Immunohistological, and Virological Investigation. Vet. Pathol. 2013, 50, 46–55. [Google Scholar] [CrossRef]
- Darweesh, M.F.; Rajput, M.K.S.; Braun, L.J.; Rohila, J.S.; Chase, C.C.L. BVDV Npro protein mediates the BVDV induced immunosuppression through interaction with cellular S100A9 protein. Microb. Pathog. 2018, 121, 341–349. [Google Scholar] [CrossRef]
- Kobayashi, S.D.; DeLeo, F.R. Role of neutrophils in innate immunity: A systems biology-level approach. Wiley Interdiscip. Rev. Syst. Biol. Med. 2009, 1, 309–333. [Google Scholar] [CrossRef] [PubMed]
- Thakur, N.; Evans, H.; Abdelsalam, K.; Farr, A.; Rajput, M.K.S.; Young, A.J.; Chase, C.C.L. Bovine viral diarrhea virus compromises Neutrophil’s functions in strain dependent manner. Microb. Pathog. 2020, 149, 104515. [Google Scholar] [CrossRef]
- Abdelsalam, K.; Kaushik, R.S.; Chase, C. The Involvement of Neutrophil in the Immune Dysfunction Associated with BVDV Infection. Pathogens 2023, 12, 737. [Google Scholar] [CrossRef]
- Abdelsalam, K.; Rajput, M.; Elmowalid, G.; Sobraske, J.; Thakur, N.; Abdallah, H.; Ali, A.A.; Chase, C.C. The effect of bovine viral diarrhea virus (BVDV) Strains and the Corresponding Infected-Macrophages’ supernatant on macrophage inflammatory function and lymphocyte apoptosis. Viruses 2020, 12, 701. [Google Scholar] [CrossRef] [PubMed]
- Barone, L.J.; Cardoso, N.P.; Mansilla, F.C.; Castillo, M.; Capozzo, A.V. Enhanced infectivity of bovine viral diarrhoea virus (BVDV) in arginase-producing bovine monocyte-derived macrophages. Virulence 2023, 15, 2283899. [Google Scholar] [CrossRef]
- Schaut, R.G.; Ridpath, J.F.; Sacco, R.E. Bovine viral diarrhea virus type 2 impairs macrophage responsiveness to toll-like receptor ligation with the exception of toll-like receptor 7. PLoS ONE 2016, 11, e0159491. [Google Scholar] [CrossRef] [PubMed]
- Schaut, R.G.; Mcgill, J.L.; Neill, J.D.; Ridpath, J.F.; Sacco, R.E. Bovine viral diarrhea virus type 2 in vivo infection modulates TLR4 responsiveness in differentiated myeloid cells which is associated with decreased MyD88 expression. Virus Res. 2018, 208, 44–55. [Google Scholar] [CrossRef]
- Lee, S.R.; Nanduri, B.; Pharr, G.T.; Stokes, J.V.; Pinchuk, L.M. Bovine Viral Diarrhea Virus infection affects the expression of proteins related to professional antigen presentation in bovine monocytes. Biochim. Biophys. Acta—Proteins Proteom. 2009, 1794, 14–22. [Google Scholar] [CrossRef]
- Rajput, M.K.; Darweesh, M.F.; Park, K.; Braun, L.J.; Mwangi, W.; Young, A.J.; Chase, C.C. The effect of bovine viral diarrhea virus (BVDV) strains on bovine monocyte-derived dendritic cells (Mo-DC) phenotype and capacity to produce BVDV. Virol. J. 2014, 11, 44. [Google Scholar] [CrossRef]
- Glew, E.J.; Carr, B.V.; Brackenbury, L.S.; Hope, J.C.; Charleston, B.; Howard, C.J. Differential effects of bovine viral diarrhoea virus on monocytes and dendritic cells. J. Gen. Virol. 2003, 84, 1771–1780. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, N.; Franco-Mahecha, O.L.; Czepluch, W.; Quintana, M.E.; Malacari, D.A.; Trotta, M.V.; Mansilla, F.C.; Capozzo, A.V. Bovine Viral Diarrhea Virus Infects Monocyte-Derived Bovine Dendritic Cells by an E2-Glycoprotein-Mediated Mechanism and Transiently Impairs Antigen Presentation. Viral Immunol. 2016, 29, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Rajput, M.K.S.; Darweesh, M.F.; Braun, L.J.; Mansour, S.M.G.; Chase, C.C.L. Comparative humoral immune response against cytopathic or non-cytopathic bovine viral diarrhea virus infection. Res. Vet. Sci. 2020, 129, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Downey-Slinker, E.D.; Ridpath, J.F.; Sawyer, J.E.; Skow, L.C.; Herring, A.D. Antibody titers to vaccination are not predictive of level of protection against a BVDV type 1b challenge in Bos indicus—Bos taurus steers. Vaccine 2016, 34, 5053–5059. [Google Scholar] [CrossRef]
- Downey, E.D.; Tait, R.G.; Mayes, M.S.; Park, C.A.; Ridpath, J.F.; Garrick, D.J.; Reecy, J.M. An evaluation of circulating bovine viral diarrhea virus type 2 maternal antibody level and response to vaccination in Angus calves. J. Anim. Sci. 2013, 91, 4440–4450. [Google Scholar] [CrossRef]
- Cavirani, S.; Gambetti, C.; Schiano, E.; Casaletti, E.; Spadini, C.; Mezzasalma, N.; Cabassi, C.S.; Taddei, S. Comparison of immunoglobulin G concentrations in colostrum and newborn calf serum from animals of different breeds, parity and gender. Large Anim. Rev. 2024, 30, 105–111. [Google Scholar]
- Chamorro, M.F.; Walz, P.H.; Passler, T.; Santen, E.; Gard, J.; Rodning, S.P.; Riddell, K.P.; Galik, P.K.; Zhang, Y. Efficacy of multivalent, modified- live virus (MLV) vaccines administered to early weaned beef calves subsequently challenged with virulent Bovine viral diarrhea virus type 2. BMC Vet. Res. 2015, 11, 29. [Google Scholar] [CrossRef]
- Newcomer, B.W.; Chamorro, M.F.; Walz, P.H. Vaccination of cattle against bovine viral diarrhea virus. Vet. Microbiol. 2017, 206, 78–83. [Google Scholar] [CrossRef]
- Xue, W.; Mattick, D.; Smith, L. Protection from persistent infection with a bovine viral diarrhea virus (BVDV) type 1b strain by a modified-live vaccine containing BVDV types 1a and 2, infectious bovine rhinotracheitis virus, parainfluenza 3 virus and bovine respiratory syncytial virus. Vaccine 2011, 29, 4657–4662. [Google Scholar] [CrossRef]
- Ficken, M.D.; Ellsworth, M.A.; Tucker, C.M.; Cortese, V.S. Effects of modified-live bovine viral diarrhea virus vaccines containing either type 1 or types 1 and 2 BVDV on heifers and their offspring after challenge with noncytopathic type 2 BVDV during gestation. J. Am. Vet. Med. Assoc. 2006, 228, 1559–1564. [Google Scholar] [CrossRef] [PubMed]
- Fulton, R.W.; Johnson, B.J.; Briggs, R.E.; Ridpath, J.F.; Saliki, J.T.; Confer, A.W.; Burge, L.J.; Step, D.L.; Walker, D.A.; Payton, M.E. Challege with Bovine viral diarrhea virus by exposure to persistently infected calves: Protection by vaccination and negative results of antigen testing in nonvaccinated acutely infected calves. Can. J. Vet. Res. 2006, 70, 121–127. [Google Scholar]
- Grooms, D.L.; Bolin, S.R.; Coe, P.H.; Borges, R.J.; Coutu, C.E. To Bovine Viral Diarrhea Virus Following to Cattle. Am. J. Vet. Res. 2007, 68, 1417–1422. [Google Scholar] [CrossRef]
- Rodning, S.P.; Marley, M.S.D.; Zhang, Y.; Eason, A.B.; Nunley, C.L.; Walz, P.H.; Riddell, K.P.; Galik, P.K.; Brodersen, B.W.; Givens, M.D. Comparison of three commercial vaccines for preventing persistent infection with bovine viral diarrhea virus. Theriogenology 2010, 73, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Newcomer, B.W.; Walz, P.H.; Givens, M.D.; Wilson, A.E. Efficacy of bovine viral diarrhea virus vaccination to prevent reproductive disease: A meta-analysis. Theriogenology 2015, 83, 360–365.e1. [Google Scholar] [CrossRef]
- Newcomer, B.W.; Givens, D. Diagnosis and Control of Viral Diseases of Reproductive Importance: Infectious Bovine Rhinotracheitis and Bovine Viral Diarrhea. Vet. Clin. N. Am.—Food Anim. Pract. 2016, 32, 425–441. [Google Scholar] [CrossRef] [PubMed]
- Al-Kubati, A.A.G.; Hussen, J.; Kandeel, M.; Al-Mubarak, A.I.A.; Hemida, M.G. Recent Advances on the Bovine Viral Diarrhea Virus Molecular Pathogenesis, Immune Response, and Vaccines Development. Front. Vet. Sci. 2021, 8, 665128. [Google Scholar] [CrossRef]
- Antos, A.; Miroslaw, P.; Rola, J.; Polak, M.P. Vaccination Failure in Eradication and Control Programs for Bovine Viral Diarrhea Infection. Front. Vet. Sci. 2021, 8, 688911. [Google Scholar] [CrossRef]
- Platt, R.; Widel, P.W.; Kesl, L.D.; Roth, J.A. Comparison of humoral and cellular immune responses to a pentavalent modified live virus vaccine in three age groups of calves with maternal antibodies, before and after BVDV type 2 challenge. Vaccine 2009, 27, 4508–4519. [Google Scholar] [CrossRef]
- Platt, R.; Coutu, C.; Meinert, T.; Roth, J.A. Humoral and T cell-mediated immune responses to bivalent killed bovine viral diarrhea virus vaccine in beef cattle. Vet. Immunol. Immunopathol. 2008, 122, 8–15. [Google Scholar] [CrossRef]
- Kalaycioglu, A.T. Bovine viral diarrhoea virus (bvdv) diversity and vaccination. A review. Vet. Q. 2007, 29, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Sozzi, E.; Righi, C.; Boldini, M.; Bazzucchi, M.; Pezzoni, G.; Gradassi, M.; Petrini, S.; Lelli, D.; Ventura, G.; Pierini, I.; et al. Cross-reactivity antibody response after vaccination with modified live and killed bovine viral diarrhoea virus (BVD) vaccines. Vaccines 2020, 8, 374. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Yu, J.; Wang, Y.; Li, X.; Li, Y.; An, M.; Ni, W.; Liu, K. Efficacy of H2O2 inactivated bovine virus diarrhoea virus (BVDV) type 1 vaccine in mice. BMC Vet. Res. 2024, 20, 43. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Romero, N.; Arias, C.F.; Verdugo-Rodríguez, A.; López, S.; Valenzuela-Moreno, L.F.; Cedillo-Peláez, C.; Basurto-Alcántara, F.J. Immune protection induced by E2 recombinant glycoprotein of bovine viral diarrhea virus in a murine model. Front. Vet. Sci. 2023, 10, 1168846. [Google Scholar] [CrossRef]
- Chung, Y.C.; Cheng, L.T.; Zhang, J.Y.; Wu, Y.J.; Liu, S.S.; Chu, C.Y. Recombinant E2 protein enhances protective efficacy of inactivated bovine viral diarrhea virus 2 vaccine in a goat model. BMC Vet. Res. 2018, 14, 194. [Google Scholar] [CrossRef]
- Wang, S.; Yang, G.; Nie, J.; Yang, R.; Du, M.; Su, J.; Wang, J.; Wang, J.; Zhu, Y. Recombinant Erns-E2 protein vaccine formulated with MF59 and CPG-ODN promotes T cell immunity against bovine viral diarrhea virus infection. Vaccine 2020, 38, 3881–3891. [Google Scholar] [CrossRef]
- Jia, S.; Huang, X.; Li, H.; Zheng, D.; Wang, L.; Qiao, X.; Jiang, Y.; Cui, W.; Tang, L.; Li, Y.; et al. Immunogenicity evaluation of recombinant Lactobacillus casei W56 expressing bovine viral diarrhea virus E2 protein in conjunction with cholera toxin B subunit as an adjuvant. Microb. Cell Fact. 2020, 19, 186. [Google Scholar] [CrossRef]
- Koethe, S.; König, P.; Wernike, K.; Pfaff, F.; Schulz, J.; Reimann, I.; Makoschey, B.; Beer, M. A synthetic modified live chimeric marker vaccine against bvdv-1 and bvdv-2. Vaccines 2020, 8, 577. [Google Scholar] [CrossRef]
- El-Attar, L.M.R.; Thomas, C.; Luke, J.; Williams, J.A.; Brownlie, J. Enhanced neutralising antibody response to bovine viral diarrhoea virus (BVDV) induced by DNA vaccination in calves. Vaccine 2015, 33, 4004–4012. [Google Scholar] [CrossRef]
- Chowdhury, S.I.; Pannhorst, K.; Sangewar, N.; Pavulraj, S.; Wen, X.; Stout, R.W.; Mwangi, W.; Paulsen, D.B. Bohv-1-vectored bvdv-2 subunit vaccine induces bvdv cross-reactive cellular immune responses and protects against bvdv-2 challenge. Vaccines 2021, 9, 46. [Google Scholar] [CrossRef]
- Nelson, G.; Marconi, P.; Periolo, O.; La Torre, J.; Alvarez, M.A. Immunocompetent truncated E2 glycoprotein of bovine viral diarrhea virus (BVDV) expressed in Nicotiana tabacum plants: A candidate antigen for new generation of veterinary vaccines. Vaccine 2012, 30, 4499–4504. [Google Scholar] [CrossRef]
- Snider, M.; Garg, R.; Brownlie, R.; van den Hurk, J.V.; Hurk, S. van D.L. van den The bovine viral diarrhea virus E2 protein formulated with a novel adjuvant induces strong, balanced immune responses and provides protection from viral challenge in cattle. Vaccine 2014, 32, 6758–6764. [Google Scholar] [CrossRef] [PubMed]
- Pecora, A.; Malacari, D.A.; Pérez Aguirreburualde, M.S.; Bellido, D.; Escribano, J.M.; Dus Santos, M.J.; Wigdorovitz, A. Development of an enhanced bovine viral diarrhea virus subunit vaccine based on E2 glycoprotein fused to a single chain antibody which targets to antigen-presenting cells. Rev. Argent. Microbiol. 2015, 47, 4–8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bellido, D.; Baztarrica, J.; Rocha, L.; Pecora, A.; Acosta, M.; Escribano, J.M.; Parreño, V.; Wigdorovitz, A. A novel MHC-II targeted BVDV subunit vaccine induces a neutralizing immunological response in guinea pigs and cattle. Transbound. Emerg. Dis. 2021, 68, 3474–3481. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Young, N.J.; Heaney, J.; Collins, M.E.; Brownlie, J. Evaluation of efficacy of mammalian and baculovirus expressed E2 subunit vaccine candidates to bovine viral diarrhoea virus. Vaccine 2009, 27, 2387–2393. [Google Scholar] [CrossRef]
- Sadat, S.M.A.; Snider, M.; Garg, R.; Brownlie, R.; van Drunen Littel-van den Hurk, S. Local innate responses and protective immunity after intradermal immunization with bovine viral diarrhea virus E2 protein formulated with a combination adjuvant in cattle. Vaccine 2017, 35, 3466–3473. [Google Scholar] [CrossRef]
- Avello, V.; Salazar, S.; González, E.E.; Campos, P.; Manríque, V.; Mathieu, C.; Hugues, F.; Cabezas, I.; Gädicke, P.; Parra, N.C.; et al. Recombinant Subunit Vaccine Candidate against the Bovine Viral Diarrhea Virus. Int. J. Mol. Sci. 2024, 25, 8734. [Google Scholar] [CrossRef]
- Luo, Y.; Yuan, Y.; Ankenbauer, R.G.; Nelson, L.D.; Witte, S.B.; Jackson, J.A.; Welch, S.K.W. Construction of chimeric bovine viral diarrhea viruses containing glycoprotein E rns of heterologous pestiviruses and evaluation of the chimeras as potential marker vaccines against BVDV. Vaccine 2012, 30, 3843–3848. [Google Scholar] [CrossRef]
- Wang, L.; Sunyer, J.O.; Bello, L.J. Fusion to C3d Enhances the Immunogenicity of the E2 Glycoprotein of Type 2 Bovine Viral Diarrhea Virus. J. Virol. 2004, 78, 1616–1622. [Google Scholar] [CrossRef]
- Mahony, D.; Cavallaro, A.S.; Mody, K.T.; Xiong, L.; Mahony, T.J.; Qiao, S.Z.; Mitter, N. In vivo delivery of bovine viral diahorrea virus, E2 protein using hollow mesoporous silica nanoparticles. Nanoscale 2014, 6, 6617–6626. [Google Scholar] [CrossRef]
- Huang, J.; Hu, Y.; Niu, Z.; Hao, W.; Ketema, H.; Wang, Z.; Xu, J.; Sheng, L.; Cai, Y.; Yu, Z.; et al. Preclinical Efficacy of Cap-Dependent and Independent mRNA Vaccines against Bovine Viral Diarrhea Virus-1. Vet. Sci. 2024, 11, 373. [Google Scholar] [CrossRef] [PubMed]
- Mody, K.T.; Mahony, D.; Cavallaro, A.S.; Zhang, J.; Zhang, B.; Mahony, T.J.; Yu, C.; Mitter, N. Silica vesicle nanovaccine formulations stimulate long-term immune responses to the Bovine Viral Diarrhoea Virus E2 protein. PLoS ONE 2015, 10, e0143507. [Google Scholar] [CrossRef] [PubMed]


| Vaccines Name | Types | Dose (mL) | RA | Booster | Used During Pregnancy | Genotypes | Strains | Subtypes | Biotypes | Manufacturers | Website (Assessed on 10 February 2025) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bovi-Shield GOLD® IBR-BVD | MLV | 2 mL | SC/IM | 1 year | No | BVDV1 and 2 | NADL | 1a | ncp | Zoetis, NJ, USA | https://www.zoetisus.com/products/cattle/bovi-shield-gold-ibr-bvd |
| Bovela | MLV | 2 mL | IM | 1 year | Yes | BVDV1 and 2 | KE-9 and NY_93 | 1a/2a | ncp | Boehringer | https://www.boehringer-ingelheim.com/animal-health/products/bovela |
| Bovidec | IV | 4 mL | SC | 1 year | No | BVDV 1 | KY1203 | NA | ncp | Zoetis, NJ, USA | https://vmd.defra.gov.uk/ProductInformationDatabase/files/QRD_Documents/QRD-Auth_1189212.PDF |
| Bovilis® BVD | IV | 2 ml | IM | 1 year | Yes | BVDV1 | C-86 | 1a | cp | Zoetis, NJ, USA | https://www.bovilis.com/bovilis-bvd/ |
| ONE SHOT® BVD | IV | 2 mL | SC | 1 year | No | BVDV1 and 2 | NA | NA | NA | Zoetis, NJ, USA | https://www.zoetisus.com/products/cattle/one-shot-bvd |
| PESTIGARD® | IV | 2 mL | SC | Yes | BVDV | NA | NA | NA | Zoetis, NJ, USA | https://www.zoetis.com.au/all-products/portal-site/beef-dairy-sheep/beef-pestigard.aspx | |
| BOVI-SHIELD GOLD FP 5 | IV | 2 mL | IM | 1 year | No | BVDV1 and 2 | NADAL/53637 | 1a/2a | cp | Zoetis, NJ, USA | https://www.zoetisus.com/products/cattle/bovi-shield-gold-fp-5-l5 |
| Cattle Master GOLD FP 5 | IV | 2 mL | SC | 1 year | Yes | BVDV1 and 2 | 5960/53637 | 1a/2a | cp | Zoetis, NJ, USA | https://www.zoetisus.com/products/cattle/cattlemaster-gold-fp-5 |
| CATTLEMASTER 4 | IV | 2 mL | IM | 1 year | Yes | BVDV1 | 5960/6309 | 1a/1 | ncp/cp | Zoetis, NJ, USA | https://www.zoetis.co.za/products/beef-and-feedlot/cattlemaster-4.aspx |
| Elite® 4-HS | IV | 5 mL | IM | 1 year | Yes | BVDV1 | Singer | 1a | cp | Boehringer, Ingelheim, Germany | https://store.animalhealthusa.com/elite4hs.html |
| Master Guard 10 HB | MLV/IV | 3 mL | IM/SC | 1 year | Yes | BVD1 and 2 | C24V | 1a | cp | Elanco, Indiana, USA | https://farmanimal.elanco.com/us/brand/master-guard |
| Triangle 5 | IV | 2 mL | IM/SC | 1 year | Yes | BVDV1 and 2 | Singer/5912 | 1a/2a | cp/cp | Boehringer, Ingelheim, Germany | https://bi-animalhealth.com/cattle/products/triangle |
| Vira Shield 6 + VL5 HB | IV | 5 mL | SC | 1 year | Yes | BVDV1 and 2 | K12/GL 760/TN131 | 1a/1a | cp/ncp/cp | Novarties | https://farmanimal.elanco.com/us/dairy/products/vira-shield |
| Express FP 5 | MLV | 2 mL | 1 year | Yes | BVDV 1 and 2 | Singer | 1a/2c | cp/ncp/cp | Boehringer, Ingelheim, Germany | https://www.drugs.com/vet/express-fp-5.html | |
| Pyramid 4 cattle vaccine | MLV | 2 mL | SC/IM | 1 year | No | BVDV1 and 2 | Singer | 1a | cp | Boehringer, Ingelheim, Germany | https://www.valleyvet.com/ct_detail.html?pgguid=30e076d9-7b6a-11d5-a192-00b0d0204ae5 |
| Titanium 5 | MLV | 2 mL | SC | 1 year | Yes | BVDV1 and 2 | C24V/296 | 1a/2c | cp | Elanco, Indiana, USA | https://farmanimal.elanco.com/us/beef/products/titanium |
| TRIANGLE® 4 + PH-K | IV | 5 mL | SC | 1 year | Not Tested | BVD1 | Singer | 1a | cp | Boehringer, Ingelheim, Germany | https://www.drugs.com/vet/triangle-4-ph-k.html |
| Antigen | Adjuvants | Vaccine Types | References |
|---|---|---|---|
| tE2 | Montanide ISA 70 SEPPIC® and (Al(OH)3Hydrogel®) | Subunit | [67] |
| rE2 | ISA 61 VG | Recombinant | [65] |
| E2 | Cholera toxin B subunit (ctxB) | Recombinant | [68] |
| E2,NS2-3 | MONTANIDETM ISA 201 VG adjuvant | Subunit | [11] |
| Erns-E2 | MF59 and CPG-ODN | Subunit | [67] |
| Erns | NA | Marker vaccine | [69] |
| E2 (E2t) and NS3 | NA | DNA | [70] |
| E2 and flag-tagged Erns | NA | [71] | |
| Npro,E2 and NS2-3 | BenchMark-Vaxliant | Mosaic vaccines | [11] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tesfaye Melkamsew, A.; Sisay Tessema, T.; Paeshuyse, J. Host Immune Response to Bovine Viral Diarrhea Virus (BVDV): Insights and Strategies for Effective Vaccine Design. Vaccines 2025, 13, 456. https://doi.org/10.3390/vaccines13050456
Tesfaye Melkamsew A, Sisay Tessema T, Paeshuyse J. Host Immune Response to Bovine Viral Diarrhea Virus (BVDV): Insights and Strategies for Effective Vaccine Design. Vaccines. 2025; 13(5):456. https://doi.org/10.3390/vaccines13050456
Chicago/Turabian StyleTesfaye Melkamsew, Asamenew, Tesfaye Sisay Tessema, and Jan Paeshuyse. 2025. "Host Immune Response to Bovine Viral Diarrhea Virus (BVDV): Insights and Strategies for Effective Vaccine Design" Vaccines 13, no. 5: 456. https://doi.org/10.3390/vaccines13050456
APA StyleTesfaye Melkamsew, A., Sisay Tessema, T., & Paeshuyse, J. (2025). Host Immune Response to Bovine Viral Diarrhea Virus (BVDV): Insights and Strategies for Effective Vaccine Design. Vaccines, 13(5), 456. https://doi.org/10.3390/vaccines13050456






