Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Instrument
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
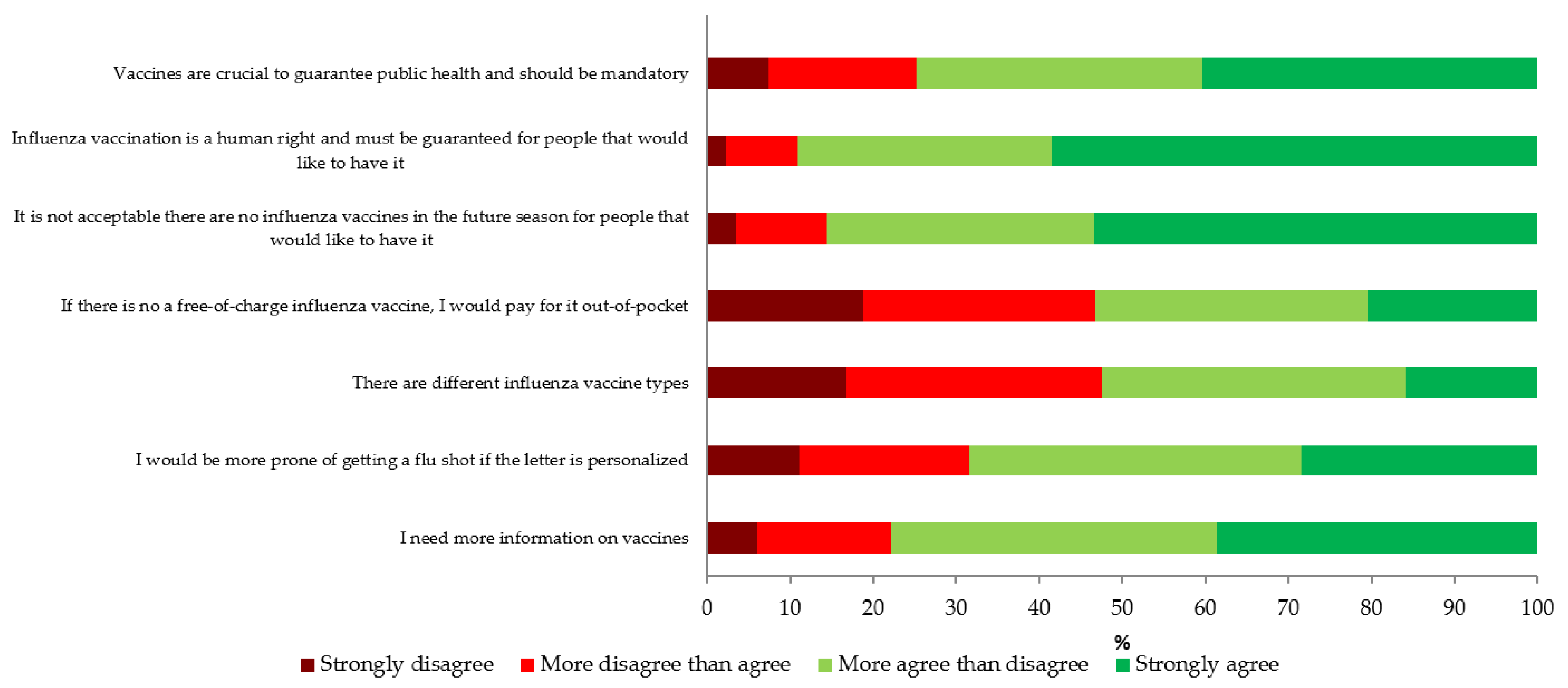
3.2. Attitudes Towards Influenza Vaccination
3.3. Willingness to Receive the 2020/21 Season Influenza Vaccination and Its Relationship to the COVID-19 Pandemic
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization (WHO). Vaccines against influenza WHO position paper—November 2012. Wkly. Epidemiol. Rec. 2012, 87, 461–476. [Google Scholar]
- GBD 2017 Influenza Collaborators. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: An analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2019, 7, 69–89. [Google Scholar] [CrossRef] [Green Version]
- Paget, J.; Spreeuwenberg, P.; Charu, V.; Taylor, R.J.; Iuliano, A.D.; Bresee, J.; Simonsen, L.; Viboud, C. Global Seasonal Influenza-associated Mortality Collaborator Network and GLaMOR Collaborating Teams. Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. J. Glob. Health 2019, 9, 020421. [Google Scholar] [CrossRef] [PubMed]
- Rosano, A.; Bella, A.; Gesualdo, F.; Acampora, A.; Pezzotti, P.; Marchetti, S.; Ricciardi, W.; Rizzo, C. Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14–2016/17 seasons). Int. J. Infect. Dis. 2019, 88, 127–134. [Google Scholar] [CrossRef] [Green Version]
- de Lusignan, S.; Correa, A.; Ellis, J.; Pebody, R. Influenza vaccination: In the UK and across Europe. Br. J. Gen. Pract. 2016, 66, 452–453. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control (ECDC). Seasonal Influenza Vaccination and Antiviral Use in EU/EEA Member States. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/seasonal-influenza-antiviral-use-2018.pdf (accessed on 18 September 2020).
- Organization for Economic Co-Operation and Development (OECD). Influenza Vaccination Rates (Indicator). Available online: https://data.oecd.org/healthcare/influenza-vaccination-rates.htm (accessed on 18 September 2020).
- World Health Organization (WHO). Evaluation of Seasonal Influenza Vaccination Policies and Coverage in the WHO European Region. Available online: https://www.euro.who.int/__data/assets/pdf_file/0003/241644/Evaluation-of-seasonal-influenza-vaccination-policies-and-coverage-in-the-WHO-European-Region.pdf (accessed on 18 September 2020).
- Grohskopf, L.A.; Alyanak, E.; Broder, K.R.; Walter, E.B.; Fry, A.M.; Jernigan, D.B. Prevention and control of seasonal influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices—United States, 2019–2020 influenza season. MMWR Recomm. Rep. 2019, 68, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Italian Ministry of Health. Prevention and Control of Influenza: Recommendations for Season 2020–2021. Available online: http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=74451&parte=1%20&serie=null (accessed on 18 September 2020).
- Nagata, J.M.; Hernández-Ramos, I.; Kurup, A.S.; Albrecht, D.; Vivas-Torrealba, C.; Franco-Paredes, C. Social determinants of health and seasonal influenza vaccination in adults ≥65 years: A systematic review of qualitative and quantitative data. BMC Public Health 2013, 13, 388. [Google Scholar] [CrossRef] [Green Version]
- Kohlhammer, Y.; Schnoor, M.; Schwartz, M.; Raspe, H.; Schäfer, T. Determinants of influenza and pneumococcal vaccination in elderly people: A systematic review. Public Health 2007, 121, 742–751. [Google Scholar] [CrossRef]
- Sarli, L. The pandemic from COVID 19: A lesson that we must not forget. Acta Biomed. 2020, 91, 5–8. [Google Scholar]
- Italian National Institute of Health. FluNews Italia. Available online: https://www.epicentro.iss.it/influenza/flunews (accessed on 18 September 2020).
- Lippi, G.; Mattiuzzi, C.; Cervellin, G. Google search volume predicts the emergence of COVID-19 outbreaks: Google Trends and COVID-19 outbreak. Acta Biomed. 2020, 91, e2020006. [Google Scholar]
- World Health Organization (WHO). Q&A: Influenza and COVID-19—Similarities and Differences. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-similarities-and-differences-covid-19-and-influenza?gclid=CjwKCAjwmMX4BRAAEiwA-zM4JuVJiMhiqtIBrtEvZRgi3Gd7aDMbfSluWM-e-Su_hNuiLUkR-O2-FRoCSykQAvD_BwE (accessed on 18 September 2020).
- Marín-Hernández, D.; Schwartz, R.E.; Nixon, D.F. Epidemiological evidence for association between higher influenza vaccine uptake in the elderly and lower COVID-19 deaths in Italy. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.; Werba, J.P.; Frigerio, B.; Coggi, D.; Sansaro, D.; Ravani, A.; Ferrante, P.; Veglia, F.; Tremoli, E.; Baldassarre, D. Relationship between influenza vaccination coverage rate and COVID-19 outbreak: An Italian ecological study. Vaccines (Basel) 2020, 8, 535. [Google Scholar] [CrossRef] [PubMed]
- Region of Lazio. Mandatory Order for Influenza and Pneumococcal Vaccination. Available online: http://www.regione.lazio.it/rl/coronavirus/ordinanza-per-vaccinazione-antinfluenzale-e-anti-pneumococcica-obbligatoria/ (accessed on 18 September 2020).
- Region of Sicily. Influenza Vaccination Campaign 2020/2021: Involvement of GPs and Pediatricians. Available online: https://www.vaccinarsinsicilia.org/assets/uploads/files/da-n.-743.pdf (accessed on 18 September 2020).
- Region of Calabria. Decree of the President of the Region of Calabria N 47 of 27th May 2020. Available online: https://portale.regione.calabria.it/website/portalmedia/2020-05/ORDINANZA-DEL-PRESIDENTE-DELLA-REGIONE-N.47-DEL-27-MAGGIO-2020.pdf (accessed on 18 September 2020).
- SWG, S.p.A. Activity. Available online: https://www.swg.it/activity (accessed on 18 September 2020).
- Italian National Institute of Statistics (ISTAT). Demography in Numbers. Available online: http://demo.istat.it/ (accessed on 18 September 2020).
- European Union (EU). Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation). Available online: https://eur-lex.europa.eu/eli/reg/2016/679/oj (accessed on 18 September 2020).
- Italian National Institute of Statistics (ISTAT). ISTAT Classification of the Italian Education Qualifications. Available online: https://www.istat.it/it/files/2011/01/Classificazione-titoli-studio-28_ott_2005-nota_metodologica.pdf (accessed on 18 September 2020).
- R Core Team. R: A Language and Environment for Statistical Computing. Available online: http://www.R-project.org/ (accessed on 18 September 2020).
- Italian Ministry of Health. A New Coronavirus. Available online: http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4807 (accessed on 18 September 2020).
- Goldman, R.D.; McGregor, S.; Marneni, S.R.; Katsuta, T.; Griffiths, M.A.; Hall, J.E.; Seiler, M.; Klein, E.J.; Cotanda, C.P.; Gelernter, R.; et al. Willingness to vaccinate children against influenza after the COVID-19 pandemic. J. Pediatr. 2020. [Google Scholar] [CrossRef]
- Italian Ministry of Health. Definition and Update of the Essential Levels of Healthcare. Available online: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=58669&completo=false (accessed on 18 September 2020).
- Bonanni, P.; Gasparini, R.; Greco, D.; Mennini, F.S.; Rossi, A.; Signorelli, C. Lowering the Age of Influenza Vaccine Recommendation to 60 Years: A Choice for the Public Health and Economy. Available online: http://www.societaitalianaigiene.org/site/new/images/docs/gdl/vaccini/201360enni.pdf (accessed on 18 September 2020).
- Kheiraoui, F.; Cadeddu, C.; Quaranta, G.; Poscia, A.; Raponi, M.; de Waure, C.; Boccalini, S.; Pellegrino, E.; Bellini, I.; Pieri, L.; et al. Health technology assessment of the quadrivalent influenza vaccine FLU-QIV (Fluarix Tetra®). Quad. Ital. J. Public Health 2015, 5. Available online: https://www.ijph.it/pdf/2015-v4-n5.pdf (accessed on 18 September 2020).
- Di Pietro, M.L.; Poscia, A.; Specchia, M.L.; de Waure, C.; Zace, D.; Gasparini, R.; Amicizia, D.; Lai, P.L.; Panatto, D.; Arata, L.; et al. Health technology assessment of the adjuvanted influenza vaccine in the Italian elderly population. Quad. Ital. J. Public Health 2017, 6. Available online: https://www.ijph.it/pdf/2017-v6-n9.pdf (accessed on 18 September 2020).
- Boccalini, S.; Bechini, A.; Innocenti, M.; Sartor, G.; Manzi, F.; Bonanni, P.; Panatto, D.; Lai, P.L.; Zangrillo, F.; Rizzitelli, E.; et al. The universal influenza vaccination in children with Vaxigrip Tetra® in Italy: An evaluation of health technology assessment. J. Prev. Med. Hyg. 2018, 59, E1–E86. [Google Scholar]
- Calabrò, G.E.; Boccalini, S.; Del Ricco, M.; Ninci, A.; Manzi, F.; Bechini, A.; Bonanni, P.; Panatto, D.; Lai, P.L.; Amicizia, D.; et al. Health technology assessment of the quadrivalent cell culture-derived influenza vaccine Fluacelvax Tetra. Quad. Ital. J. Public Health 2019, 8. Available online: https://www.ijph.it/pdf/2019-v8-n5.pdf (accessed on 18 September 2020).
- The Italian Lifetime Vaccination Calendar, 4th Edition 2019. Available online: http://www.igienistionline.it/docs/2019/21cvplv.pdf (accessed on 18 September 2020).
- European Centre for Disease Prevention and Control (ECDC). Types of Seasonal Influenza Vaccine. Available online: https://www.ecdc.europa.eu/en/seasonal-influenza/prevention-and-control/vaccines/types-of-seasonal-influenza-vaccine (accessed on 18 September 2020).
- Nicolay, U.; Heijnen, E.; Nacci, P.; Patriarca, P.A.; Leav, B. Immunogenicity of aIIV3, MF59-adjuvanted seasonal trivalent influenza vaccine, in older adults ≥65 years of age: Meta-analysis of cumulative clinical experience. Int. J. Infect. Dis. 2019, 85S, S1–S9. [Google Scholar] [CrossRef] [Green Version]
- Samson, S.I.; Leventhal, P.S.; Salamand, C.; Meng, Y.; Seet, B.T.; Landolfi, V.; Greenberg, D.; Hollingsworth, R. Immunogenicity of high-dose trivalent inactivated influenza vaccine: A systematic review and meta-analysis. Expert Rev. Vaccines 2019, 18, 295–308. [Google Scholar] [CrossRef]
- Boccalini, S.; Tacconi, F.M.; Lai, P.L.; Bechini, A.; Bonanni, P.; Panatto, D. Appropriateness and preferential use of different seasonal influenza vaccines: A pilot study on the opinion of vaccinating physicians in Italy. Vaccine 2019, 37, 915–918. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). The Organization and Delivery of Vaccination Services in the European Union. Available online: https://ec.europa.eu/health/sites/health/files/vaccination/docs/2018_vaccine_services_en.pdf (accessed on 18 September 2020).
- Costantino, C.; Vitale, F. Influenza vaccination in high-risk groups: A revision of existing guidelines and rationale for an evidence-based preventive strategy. J. Prev. Med. Hyg. 2016, 57, E13–E18. [Google Scholar] [PubMed]
- Maurer, J. Who has a clue to preventing the flu? Unravelling supply and demand effects on the take-up of influenza vaccinations. J. Health Econ. 2009, 28, 704–717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levi, M.; Bonanni, P.; Biffino, M.; Conversano, M.; Corongiu, M.; Morato, P.; Maio, T. Influenza vaccination 2014-2015: Results of a survey conducted among general practitioners in Italy. Hum. Vaccin. Immunother. 2018, 14, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Nation Healthcare Service (NHS) of England. The National Flu Immunisation Programme 2020/21. Available online: https://www.england.nhs.uk/wp-content/uploads/2020/05/national-flu-immunisation-programme-2020-2021.pdf (accessed on 18 September 2020).
- Barbieri, M.; Capri, S.; Waure, C.; Boccalini, S.; Panatto, D. Age- and risk-related appropriateness of the use of available influenza vaccines in the Italian elderly population is advantageous: Results from a budget impact analysis. J. Prev. Med. Hyg. 2017, 58, E279–E287. [Google Scholar] [PubMed]
- Ricciardi, W.; Boccia, S. New challenges of public health: Bringing the future of personalised healthcare into focus. Eur. J. Public Health 2017, 27, 36–39. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, G.E.; Specchia, M.L.; Boccalini, S.; Panatto, D.; Rizzo, C.; Merler, S.; Ferriero, A.M.; Di Pietro, M.L.; Bonanni, P.; de Waure, C. Strengthening the evidence-based approach to guiding effective influenza vaccination policies. Vaccines (Basel) 2020, 8, 342. [Google Scholar] [CrossRef]
- de Waure, C.; Veneziano, M.A.; Cadeddu, C.; Capizzi, S.; Specchia, M.L.; Capri, S.; Ricciardi, W. Economic value of influenza vaccination. Hum. Vaccin. Immunother. 2012, 8, 119–129. [Google Scholar] [CrossRef] [Green Version]
- Nowak, G.J.; Sheedy, K.; Bursey, K.; Smith, T.M.; Basket, M. Promoting influenza vaccination: Insights from a qualitative meta-analysis of 14 years of influenza-related communications research by U.S. Centers for Disease Control and Prevention (CDC). Vaccine 2015, 33, 2741–2756. [Google Scholar] [CrossRef]
- Petrova, V.N.; Russell, C.A. The evolution of seasonal influenza viruses. Nat. Rev. Microbiol. 2018, 16, 47–60. [Google Scholar] [CrossRef]
- Domnich, A.; Manini, I.; Calabrò, G.E.; de Waure, C.; Montomoli, E. Mapping host-related correlates of influenza vaccine-induced immune response: An umbrella review of the available systematic reviews and meta-analyses. Vaccines (Basel) 2019, 7, 215. [Google Scholar] [CrossRef] [Green Version]
- Belongia, E.A.; Simpson, M.D.; King, J.P.; Sundaram, M.E.; Kelley, N.S.; Osterholm, M.T.; McLean, H.Q. Variable influenza vaccine effectiveness by subtype: A systematic review and meta-analysis of test-negative design studies. Lancet Infect. Dis. 2016, 16, 942–951. [Google Scholar] [CrossRef]
- Zhao, L.; Stirling, R.; Young, K. Should individuals use influenza vaccine effectiveness studies to inform their decision to get vaccinated? Can. Commun. Dis. Rep. 2019, 45, 156–158. [Google Scholar] [CrossRef] [PubMed]
- Kassianos, G.; Blank, P.; Falup-Pecurariu, O.; Kuchar, E.; Kyncl, J.; De Lejarazu, R.O.; Nitsch-Osuch, A.; van Essen, G.A. Influenza vaccination: Key facts for general practitioners in Europe: A synthesis by European experts based on national guidelines and best practices in the United Kingdom and the Netherlands. Drugs Context 2016, 5, 212293. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. National Minimum Standards and Core Curriculum for Immunisation Training for Registered Healthcare Practitioners. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/679824/Training_standards_and_core_curriculum_immunisation.pdf (accessed on 18 September 2020).
- Santos, A.J.; Kislaya, I.; Machado, A.; Nunes, B. Beliefs and attitudes towards the influenza vaccine in high-risk individuals. Epidemiol. Infect. 2017, 145, 1786–1796. [Google Scholar] [CrossRef] [Green Version]
- Holt, D.; Bouder, F.; Elemuwa, C.; Gaedicke, G.; Khamesipour, A.; Kisler, B.; Kochhar, S.; Kutalek, R.; Maurer, W.; Obermeier, P.; et al. The importance of the patient voice in vaccination and vaccine safety-are we listening? Clin. Microbiol. Infect. 2016, 22, S146–S153. [Google Scholar] [CrossRef] [Green Version]
- Frank, E.; Dresner, Y.; Shani, M.; Vinker, S. The association between physicians’ and patients’ preventive health practices. CMAJ 2013, 185, 649–653. [Google Scholar] [CrossRef] [Green Version]
- Genovese, C.; Picerno, I.A.M.; Trimarchi, G.; Cannavò, G.; Egitto, G.; Cosenza, B.; Merlina, V.; Icardi, G.; Panatto, D.; Amicizia, D.; et al. Vaccination coverage in healthcare workers: A multicenter cross-sectional study in Italy. J. Prev. Med. Hyg. 2019, 60, E12–E17. [Google Scholar]
- Riccò, M.; Cattani, S.; Casagranda, F.; Gualerzi, G.; Signorelli, C. Knowledge, attitudes, beliefs and practices of occupational physicians towards vaccinations of health care workers: A cross sectional pilot study in North-Eastern Italy. Int. J. Occup. Med. Environ. Health 2017, 30, 775–790. [Google Scholar] [CrossRef]
- Panatto, D.; Amicizia, D.; Arata, L.; Lai, P.L.; Gasparini, R. A comprehensive analysis of Italian web pages mentioning squalene-based influenza vaccine adjuvants reveals a high prevalence of misinformation. Hum. Vaccin. Immunother. 2018, 14, 969–977. [Google Scholar] [CrossRef] [Green Version]
- Domnich, A.; Arata, L.; Amicizia, D.; Signori, A.; Gasparini, R.; Panatto, D. Assessing spatial inequalities in accessing community pharmacies: A mixed geographically weighted approach. Geospat. Health 2016, 11, 457. [Google Scholar] [CrossRef] [Green Version]
- Scarpitta, F.; Restivo, V.; Bono, C.M.; Sannasardo, C.E.; Vella, C.; Ventura, G.; Bono, S.; Palmeri, S.; Caracci, F.; Casuccio, A.; et al. The role of the Community Pharmacist in promoting vaccinations among general population according to the National Vaccination Plan 2017–2019: Results from a survey in Sicily, Italy. Ann. Ig. 2019, 31, 25–35. [Google Scholar] [PubMed]
- Poulose, S.; Cheriyan, E.; Cheriyan, R.; Weeratunga, D.; Adham, M. Pharmacist-administered influenza vaccine in a community pharmacy: A patient experience survey. Can. Pharm. J. 2015, 148, 64–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkdale, C.L.; Nebout, G.; Megerlin, F.; Thornley, T. Benefits of pharmacist-led flu vaccination services in community pharmacy. Ann. Pharm. Fr. 2017, 75, 3–8. [Google Scholar] [CrossRef]
- Mondelli Agenda. Available online: http://www.quotidianosanita.it/allegati/allegato177299.pdf (accessed on 18 September 2020).
- Gianfredi, V.; Nucci, D.; Salvatori, T.; Orlacchio, F.; Villarini, M.; Moretti, M.; PErCEIVE IN UMBRIA STUDY GROUP. “PErCEIVE in Umbria”: Evaluation of anti-influenza vaccination’s perception among Umbrian pharmacists. J. Prev. Med. Hyg. 2018, 59, E14–E19. [Google Scholar] [PubMed]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef] [PubMed]
- Amicizia, D.; Domnich, A.; Gasparini, R.; Bragazzi, N.L.; Lai, P.L.; Panatto, D. An overview of current and potential use of information and communication technologies for immunization promotion among adolescents. Hum. Vaccin. Immunother. 2013, 9, 2634–2642. [Google Scholar] [CrossRef] [Green Version]
- Ferro, A.; Odone, A.; Siddu, A.; Colucci, M.; Anello, P.; Longone, M.; Marcon, E.; Castiglia, P.; Bonanni, P.; Signorelli, C. Monitoring the web to support vaccine coverage: Results of two years of the portal VaccinarSì. Epidemiol. Prev. 2015, 39, 88–93. [Google Scholar]
- Costantino, C.; Caracci, F.; Brandi, M.; Bono, S.E.; Ferro, A.; Sannasardo, C.E.; Scarpitta, F.; Siddu, A.; Vella, C.; Ventura, G.; et al. Determinants of vaccine hesitancy and effectiveness of vaccination counseling interventions among a sample of the general population in Palermo, Italy. Hum. Vaccin. Immunother. 2020. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy 2005–2016. Available online: https://apps.who.int/iris/bitstream/handle/10665/251671/WHO-HIS-TTi-GAP-16.2-eng.pdf?sequence=1&isAllowed=y (accessed on 18 September 2020).
- Crocker-Buque, T.; Mindra, G.; Duncan, R.; Mounier-Jack, S. Immunization, urbanization and slums—A systematic review of factors and interventions. BMC Public Health 2017, 17, 556. [Google Scholar] [CrossRef]
- O’Leary, S.T.; Barnard, J.; Lockhart, S.; Kolasa, M.; Shmueli, D.; Dickinson, L.M.; Kile, D.; Dibert, E.; Kempe, A. Urban and rural differences in parental attitudes about influenza vaccination and vaccine delivery models. J. Rural Health 2015, 31, 421–430. [Google Scholar] [CrossRef]
- Restivo, V.; Orsi, A.; Ciampini, S.; Messano, G.A.; Trucchi, C.; Ventura, G.; Casuccio, A.; Vitale, F. How should vaccination services be planned, organized, and managed? Results from a survey on the Italian vaccination services. Ann. Ig 2019, 31, 45–53. [Google Scholar] [PubMed]
- Odone, A.; Lugo, A.; Amerio, A.; Borroni, E.; Bosetti, C.; Carreras, G.; Cavalieri d’Oro, L.; Colombo, P.; Fanucchi, T.; Ghislandi, S.; et al. COVID-19 lockdown impact on lifestyle habits of Italian adults. Acta Biomed. 2020, 91, 87–89. [Google Scholar] [PubMed]
- Vukovic, V.; Lillini, R.; Lupi, S.; Fortunato, F.; Cicconi, M.; Matteo, G.; Arata, L.; Amicizia, D.; Boccalini, S.; Bechini, A.; et al. Identifying people at risk for influenza with low vaccine uptake based on deprivation status: A systematic review. Eur. J. Public Health 2020, 30, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Lucyk, K.; Simmonds, K.A.; Lorenzetti, D.L.; Drews, S.J.; Svenson, L.W.; Russell, M.L. The association between influenza vaccination and socioeconomic status in high income countries varies by the measure used: A systematic review. BMC Med. Res. Methodol. 2019, 19, 153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzo, C.; Rota, M.C.; Bella, A.; Giannitelli, S.; De Santis, S.; Nacca, G.; Pompa, M.G.; Vellucci, L.; Salmaso, S.; Declich, S. Response to the 2009 influenza A(H1N1) pandemic in Italy. Eur. Surveill. 2010, 15, 19744. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Tang, B.; Bragazzi, N.L.; Xiao, Y.; Wu, J. Modeling the impact of mass influenza vaccination and public health interventions on COVID-19 epidemics with limited detection capability. Math. Biosci. 2020, 325, 108378. [Google Scholar] [CrossRef]
- Italian National Institute of Statistics (ISTAT). Internet: Access and Usage Type. Available online: http://dati.istat.it/Index.aspx?DataSetCode=DCCV_ICT (accessed on 18 September 2020).
- Poynton, T.A.; DeFouw, E.R.; Morizio, L.J. A systematic review of online response rates in four counseling journals. J Couns. Dev. 2019, 97, 33–42. [Google Scholar] [CrossRef]
- World Health Organization (WHO). The Guide to Tailoring Immunization Programmes (TIP). Available online: https://www.euro.who.int/__data/assets/pdf_file/0003/187347/The-Guide-to-Tailoring-Immunization-Programmes-TIP.pdf (accessed on 18 September 2020).
- Costantino, C.; Restivo, V.; Tramuto, F.; Casuccio, A.; Vitale, F. Influenza vaccination of healthcare workers in Italy: Could mandatory vaccination be a solution to protect patients? Future Microbiol. 2019, 14, 45–49. [Google Scholar] [CrossRef]

| Variable | Level | % (N) | 95% CI |
|---|---|---|---|
| Sex | Male | 54.5 (1386) | 52.5–56.5 |
| Female | 45.5 (1157) | 43.5–47.5 | |
| Age, years | 18–24 | 9.3 (236) | 8.2–10.5 |
| 25–34 | 16.5 (420) | 15.1–18.2 | |
| 35–44 | 18.7 (476) | 17.2–20.3 | |
| 45–54 | 23.0 (586) | 21.4–24.7 | |
| 55–64 | 17.1 (436) | 15.7–18.7 | |
| 65–74 | 12.4 (315) | 11.1–13.7 | |
| ≥75 | 2.9 (74) | 2.3–3.6 | |
| Geographic area | North-East | 19.6 (499) | 18.1–21.2 |
| North-West | 28.1 (714) | 26.3–29.9 | |
| Center | 20.1 (512) | 18.6–21.7 | |
| South | 21.9 (557) | 20.3–23.6 | |
| Islands | 10.3 (261) | 9.1–11.5 | |
| Urbanization pattern, N of inhabitants | <5000 | 11.4 (291) | 10.2–12.7 |
| 5000–9999 | 11.1 (283) | 9.9–12.4 | |
| 10,000–29,999 | 18.5 (470) | 17.0–20.0 | |
| 30,000–99,999 | 22.1 (561) | 20.5–23.7 | |
| 100,000–249,999 | 11.1 (283) | 9.9–12.4 | |
| ≥250,000 | 25.8 (655) | 24.1–27.5 | |
| Employment status | Unemployed | 8.5 (215) | 7.4–9.6 |
| Student | 9.2 (235) | 8.1–10.4 | |
| Housekeeper | 5.6 (142) | 4.7–6.5 | |
| Occasionally employed | 7.6 (192) | 6.6–8.6 | |
| Permanently employed | 51.6 (1313) | 49.7–53.6 | |
| Retired | 15.8 (402) | 14.4–17.2 | |
| Other | 1.7 (44) | 1.3–2.3 | |
| Household pattern | Living alone | 11.0 (280) | 9.8–12.3 |
| Living with a spouse/partner | 54.6 (1388) | 52.6–56.5 | |
| Living with ≥ 1 child | 39.8 (1013) | 37.9–41.8 | |
| Living with ≥ 1 older adult | 15.8 (114) | 3.7–5.4 | |
| Perceived economic well-being | Low | 3.3 (84) | 2.6–4.1 |
| Lower than average | 10.3 (263) | 9.2–11.6 | |
| Average | 38.9 (989) | 37.0–40.8 | |
| Higher than average | 44.5 (1131) | 42.5–46.4 | |
| High | 3.0 (76) | 2.4–3.7 | |
| ISCED educational level | 1 | 0.7 (19) | 0.5–1.2 |
| 2 | 7.1 (180) | 6.1–8.1 | |
| 3/4 | 41.7 (1061) | 39.8–43.7 | |
| 5 | 48.8 (1240) | 46.8–50.7 | |
| 6 | 1.7 (43) | 1.2–2.3 |
| Variable | Level | % (95% CI) of Subjects that Will Unlikely Receive the 2020/21 Flu Shot | aOR (95% CI) | p |
|---|---|---|---|---|
| Sex | Male | 38.7 (36.2–41.4) | Ref | – |
| Female | 45.7 (42.8–48.6) | 0.94 (0.78–1.14) | 0.55 | |
| Age, years | 1-year increase | – | 0.98 (0.97–0.99) | <0.001 |
| 2019/20 vaccination | Yes | 10.1 (7.9–12.5) | Ref | – |
| No | 53.9 (51.6–56.2) | 0.10 (0.08–0.13) | <0.001 | |
| Geographic area | North-East | 40.1 (35.8–44.5) | Ref | – |
| North-West | 44.8 (41.1–48.6) | 1.13 (0.86–1.49) | 0.36 | |
| Center | 42.2 (37.9–46.6) | 1.02 (0.76–1.38) | 0.87 | |
| South | 38.4 (34.4–42.6) | 0.79 (0.59–1.06) | 0.11 | |
| Islands | 44.4 (38.3–50.7) | 1.08 (0.76–1.52) | 0.67 | |
| Urbanization pattern, N of inhabitants | <5000 | 50.5 (44.6–56.4) | Ref | – |
| 5000–9999 | 48.1 (42.1–54.0) | 0.87 (0.61–1.27) | 0.48 | |
| 10,000–29,999 | 40.0 (35.5–44.6) | 0.61 (0.44–0.85) | 0.004 | |
| 30,000–99,999 | 41.5 (37.4–45.7) | 0.70 (0.51–0.97) | 0.031 | |
| 100,000–249,999 | 41.7 (35.9–47.7) | 0.77 (0.52–1.12) | 0.17 | |
| ≥250,000 | 37.3 (33.5–41.1) | 0.55 (0.40–0.76) | <0.001 | |
| Employment status | Permanently employed | 45.7 (43.0–48.4) | Ref | – |
| Occasionally employed | 45.8 (38.6–53.2) | 0.87 (0.62–1.23) | 0.43 | |
| Student | 43.4 (37.0–50.0) | 0.56 (0.38–0.81) | 0.002 | |
| Housekeeper | 42.3 (34.0–50.8) | 0.90 (0.60–1.37) | 0.65 | |
| Unemployed | 53.5 (46.6–60.3) | 1.34 (0.95–1.88) | 0.091 | |
| Retired | 20.4 (16.6–24.7) | 0.80 (0.55–1.15) | 0.23 | |
| Other | 43.2 (28.3–59.0) | 0.77 (0.40–1.51) | 0.65 | |
| Household pattern | Living alone | 45.4 (39.4–51.4) | 1.41 (1.01–1.99) | 0.046 |
| Living with a spouse/partner | 40.2 (37.6–42.8) | 1.04 (0.83–1.29) | 0.74 | |
| Living with ≥ 1 child | 43.6 (40.6–46.8) | 1.28 (1.05–1.58) | 0.017 | |
| Living with ≥ 1 older adult | 43.0 (33.7–52.6) | 1.11 (0.72–1.73) | 0.63 | |
| Perceived economic well-being | Low | 58.3 (47.1–69.0) | Ref | – |
| Lower than average | 48.3 (42.1–54.5) | 0.64 (0.36–1.13) | 0.12 | |
| Average | 41.8 (38.7–44.9) | 0.51 (0.30–0.86) | 0.011 | |
| Higher than average | 40.1 (37.2–43.0) | 0.48 (0.28–0.82) | 0.007 | |
| High | 31.6 (21.4–43.3) | 0.34 (0.16–0.70) | 0.004 | |
| ISCED educational level | 1 | 26.3 (9.1–51.2) | Ref | – |
| 2 | 37.8 (30.7–45.3) | 0.97 (0.29–3.24) | 0.97 | |
| 3/4 | 43.6 (40.6–46.7) | 1.12 (0.35–3.60) | 0.84 | |
| 5 | 41.5 (38.7–44.3) | 0.93 (0.29–2.98) | 0.90 | |
| 6 | 37.2 (23.0–53.3) | 1.15 (0.29–4.56) | 0.84 |
| Influence of COVID-19 Pandemic on the Intention to Receive the 2020/21 Influenza Vaccination | Vaccination in 2019/20 Season, % (95% CI) | ||
|---|---|---|---|
| % (N) | 95% CI | pOR (95% CI) a | |
| Nothing at all, I would get a 2020/21 flu shot regardless | 83.2 (495) | 79.6–86.4 | 0.08 (0.06–0.10) |
| To some extent | 25.3 (680) | 22.1–28.7 | |
| Enormously, if no COVID-19 pandemic occurred, I would have no intention to get a 2020/21 flu shot | 13.9 (302) | 10.2–18.3 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domnich, A.; Cambiaggi, M.; Vasco, A.; Maraniello, L.; Ansaldi, F.; Baldo, V.; Bonanni, P.; Calabrò, G.E.; Costantino, C.; de Waure, C.; et al. Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey. Vaccines 2020, 8, 711. https://doi.org/10.3390/vaccines8040711
Domnich A, Cambiaggi M, Vasco A, Maraniello L, Ansaldi F, Baldo V, Bonanni P, Calabrò GE, Costantino C, de Waure C, et al. Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey. Vaccines. 2020; 8(4):711. https://doi.org/10.3390/vaccines8040711
Chicago/Turabian StyleDomnich, Alexander, Maura Cambiaggi, Alessandro Vasco, Luca Maraniello, Filippo Ansaldi, Vincenzo Baldo, Paolo Bonanni, Giovanna Elisa Calabrò, Claudio Costantino, Chiara de Waure, and et al. 2020. "Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey" Vaccines 8, no. 4: 711. https://doi.org/10.3390/vaccines8040711
APA StyleDomnich, A., Cambiaggi, M., Vasco, A., Maraniello, L., Ansaldi, F., Baldo, V., Bonanni, P., Calabrò, G. E., Costantino, C., de Waure, C., Gabutti, G., Restivo, V., Rizzo, C., Vitale, F., & Grassi, R. (2020). Attitudes and Beliefs on Influenza Vaccination during the COVID-19 Pandemic: Results from a Representative Italian Survey. Vaccines, 8(4), 711. https://doi.org/10.3390/vaccines8040711











