A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Management
2.3. Statistical Analysis
3. Results
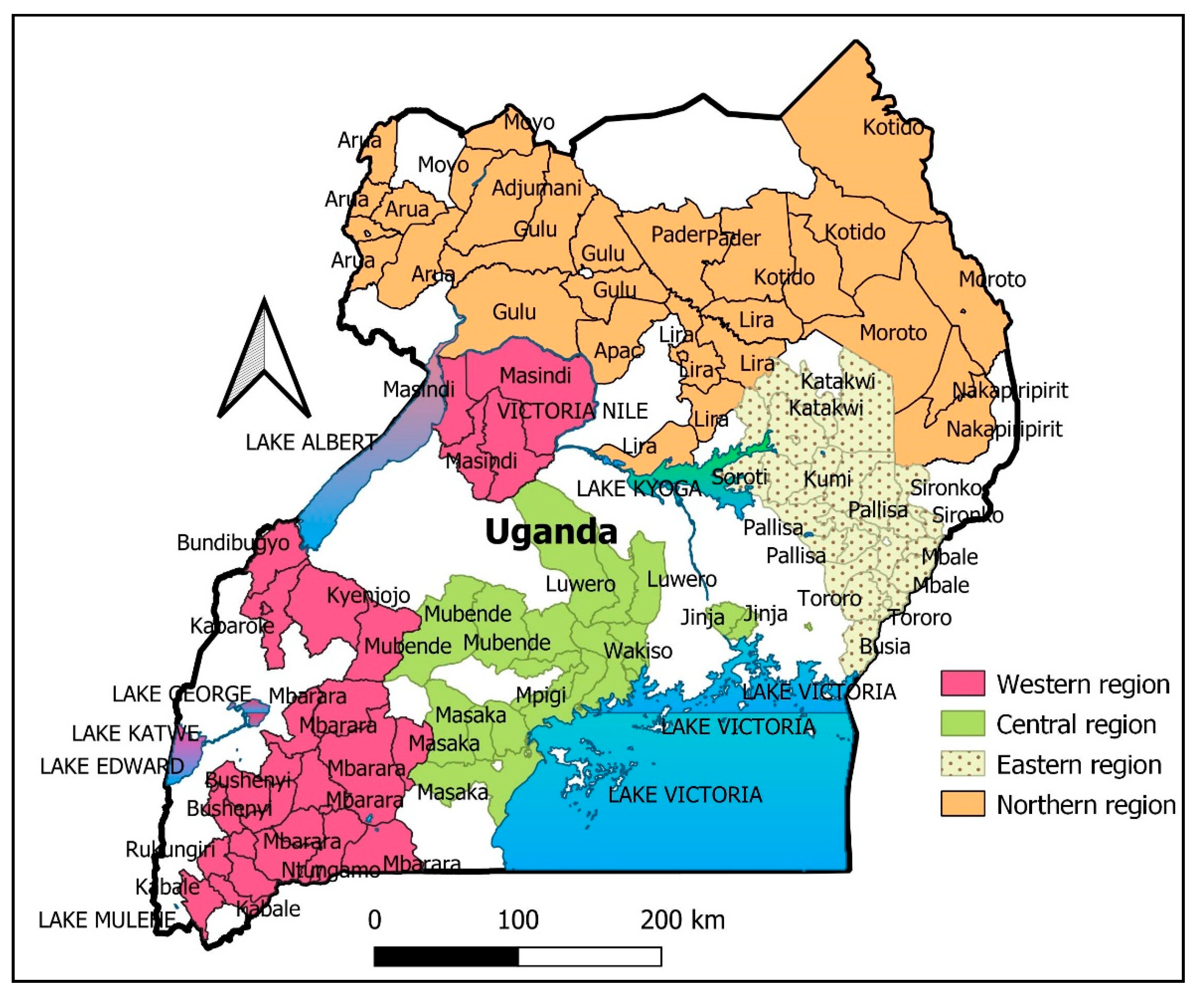
3.1. Population Social Demographic Variables in Ugandan Healthcare Centers
3.2. Influence of Sociodemographic Characteristics on the Knowledge Score, Confidence, and Trust for COVID-19 Vaccine Clinical Trials among the Healthcare Workers
3.3. Descriptive Narrative on Knowledge, Trust and Confidence among Study Participants
3.4. Multivariate Analysis on COVID-19 Clinical Trials amongst Ugandans
3.5. Relationship between Knowledge, Confidence, and Trust
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Conradie, A.; Duys, R.; Forget, P.; Biccard, B. Barriers to clinical research in Africa: A quantitative and qualitative survey of clinical researchers in 27 African countries. Br. J. Anaesth. 2018, 121, 813–821. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, S.B.; Neaton, J.D.; Lane, H.C.; Kieh, M.W.S.; Massaquoi, M.B.F.; Touchette, N.A.; Nason, M.C.; Follmann, D.A.; Boley, F.K.; Johnson, M.P.; et al. Implementation of an Ebola virus disease vaccine clinical trial during the Ebola epidemic in Liberia: Design, procedures, and challenges. Clin. Trials 2016, 13, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Enria, L.; Lees, S.; Smout, E.; Mooney, T.; Tengbeh, A.F.; Leigh, B.; Greenwood, B.; Watson-Jones, D.; Larson, H. Power, fairness and trust: Understanding and engaging with vaccine trial participants and communities in the setting up the EBOVAC-Salone vaccine trial in Sierra Leone. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ezeome, E.R.; Simon, C. Ethical problems in conducting research in acute epidemics: The pfizer meningitis study in nigeria as an illustration. Dev. World Bioeth. 2010, 10, 1–10. [Google Scholar] [CrossRef]
- Erku, D.A.; Belachew, S.A.; Abrha, S.; Sinnollareddy, M.; Thomas, J.; Steadman, K.J.; Tesfaye, W.H. When fear and misinformation go viral: Pharmacists’ role in deterring medication misinformation during the ’infodemic’ surrounding COVID-19. Res. Soc. Adm. Pharm. 2021, 17, 1954–1963. [Google Scholar] [CrossRef]
- Folayan, M.O.; Allman, D.; Haire, B.; Yakubu, A.; Afolabi, M.O.; Cooper, J. Considerations for community engage-ment when conducting clinical trials during infectious disease emergencies in West Africa. Dev. World Bioeth. 2019, 19, 96–105. [Google Scholar] [CrossRef]
- Pratt, B.; de Vries, J. Community engagement in global health research that advances health equity. Bioethics 2018, 32, 454–463. [Google Scholar] [CrossRef]
- Singh, J.A. The Case for Why Africa Should Host COVID-19 Candidate Vaccine Trials. J. Infect. Dis. 2020, 222, 351–355. [Google Scholar] [CrossRef]
- Seth, B. COVAX Explained. 2020. Available online: https://www.gavi.org/vaccineswork/covax-explained (accessed on 20 January 2021).
- Lederer, K.; Castaño, D.; Atria, D.G.; Oguin, T.H.; Wang, S.; Manzoni, T.B.; Muramatsu, H.; Hogan, M.J.; Amanat, F.; Cherubin, P.; et al. SARS-CoV-2 mRNA Vaccines Foster Potent Antigen-Specific Germinal Center Responses Associated with Neutralizing Antibody Generation. Immunity 2020, 53, 1281–1295.e5. [Google Scholar] [CrossRef]
- Mathpati, M.M.; Payyappallimana, U.; Shankar, D.; Porter, J.D. Population self-reliance in health’ and COVID-19: The need for a 4th tier in the health system. J. Ayurveda Integr. Med. 2020, 8, 3. [Google Scholar] [CrossRef]
- Nugraha, R.V.; Ridwansyah, H.; Ghozali, M.; Khairani, A.F.; Atik, N. Traditional Herbal Medicine Candidates as Complementary Treatments for COVID-19: A Review of Their Mechanisms, Pros and Cons. Evid.-Based Complement. Altern. Med. 2020, 2020, 1–12. [Google Scholar] [CrossRef]
- Kasozi, K.I.; Mujinya, R.; Bogere, P.; Ekou, J.; Zirintunda, G.; Ahimbisibwe, S.; Matama, K.; Ninsiima, H.I.; Echoru, I.; Ayikobua, E.T.; et al. Pandemic panic and anxiety in developing countries. Embracing One Health offers practical strategies in management of COVID-19 for Africa. Pan Afr. Med. J. 2020, 35, 3. [Google Scholar] [CrossRef] [PubMed]
- Kasozi, K.I.; MacLeod, E.; Ssempijja, F.; Mahero, M.W.; Matama, K.; Musoke, G.H.; Bardosh, K.; Ssebuufu, R.; Wakoko-Studstil, F.; Echoru, I.; et al. Misconceptions on COVID-19 Risk Among Ugandan Men: Results From a Rapid Exploratory Survey, April 2020. Front. Public Health 2020, 8, 416. [Google Scholar] [CrossRef]
- Usman, I.M.; Ssempijja, F.; Ssebuufu, R.; Lemuel, A.M.; Archibong, V.B.; Ayikobua, E.T.; Aruwa, J.O.; Kembabazi, S.; Kegoye, E.S.; Ayuba, J.T.; et al. Community Drivers Affecting Adherence to WHO Guidelines Against COVID-19 Amongst Rural Ugandan Market Vendors. Front. Public Health 2020, 8, 340. [Google Scholar] [CrossRef] [PubMed]
- Krejcie, R.V.; Morgan, D.W. Determining Sample Size for Research Activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar] [CrossRef]
- Omaswa, F.; Kadama, P.; Eriki, P.; Odedo, R.; Gidudu, H.E. Brain to Brain Gain: Health Workforce Migration: A Case Study of General Practitioners in Uganda, WHO. 2017. Available online: https://www.who.int/workforcealliance/brain-drain-brain-gain/17-340Uganda-case-study2017-10-18.pdf (accessed on 16 February 2021).
- D’Agostino, R.B.; Belanger, A. A Suggestion for Using Powerful and Informative Tests of Normality. Am. Stat. 1990, 44, 316. [Google Scholar] [CrossRef]
- Ssebuufu, R.; Sikakulya, F.K.; Mambo, S.B.; Wasingya, L.; Nganza, S.K.; Ibrahim, B.; Kyamanywa, P. Knowledge, Attitude, and Self-Reported Practice Toward Measures for Prevention of the Spread of COVID-19 Among Ugandans: A Nationwide Online Cross-Sectional Survey. Front. Public Health 2020, 8, 618731. [Google Scholar] [CrossRef]
- French, J.; Deshpande, S.; Evans, W.; Obregon, R. Key Guidelines in Developing a Pre-Emptive COVID-19 Vaccination Uptake Promotion Strategy. Int. J. Environ. Res. Public Health 2020, 17, 5893. [Google Scholar] [CrossRef] [PubMed]
- WHO. Vaccine Acceptance is the Next Hurdle. 2020. Available online: https://www.who.int/news-room/feature-stories/detail/vaccine-acceptance-is-the-next-hurdle (accessed on 20 January 2021).
- El-Sadr, W. The Challenge of Minority Recruitment in Clinical Trials for AIDS. JAMA J. Am. Med. Assoc. 1992, 267, 954. [Google Scholar] [CrossRef]
- Natural Chemotherapeutics Research Institute. Clinical Evaluation of Efficacy, Safety Immunogenicity and Reliability of UBV-01N- a Noval Natural Product- in Adult Patients Infected with SARS-CoV-2 (COVID-19), in Uganda. Published by the Ministry of Health Uganda. 2020. Available online: https://ncri.go.ug/covid-19/ (accessed on 31 December 2020).
- Atukunda, N. Uganda Turns to Herbs in Search for COVID-19 Cure, Daily Monitor. 2020. Available online: https://www.monitor.co.ug/uganda/news/national/uganda-turns-to-herbs-in-search-for-covid-19-cure-3238216 (accessed on 31 December 2020).
- Antananarivo, R.I. Madagascar President’s Herbal Tonic Fails to Halt Covid-19 Spike. BBC News. 13 August 2020. Available online: https://www.bbc.com/news/world-africa-53756752 (accessed on 25 December 2020).
- Felix, T. Nigeria: Madagascar’s Herbal Drink Cannot Cure COVID-19. 2020. Available online: https://www.aa.com.tr/en/africa/nigeria-madagascars-herbal-drink-cannot-cure-covid-19/1915948 (accessed on 25 December 2020).
- Shannon, G.; Jansen, M.; Williams, K.; Cáceres, C.; Motta, A.; Odhiambo, A.; Eleveld, A.; Mannell, J. Gender equality in science, medicine, and global health: Where are we at and why does it matter? Lancet 2019, 393, 560–569. [Google Scholar] [CrossRef] [Green Version]
- Kiracho, E.E. Increasing access to quality health care for the poor: Community perceptions on quality care in Uganda. Patient Prefer. Adherence 2009, 3, 77–85. [Google Scholar] [CrossRef] [Green Version]
- Witter, S.; Namakula, J.; Wurie, H.; Chirwa, Y.; So, S.; Vong, S.; Ros, B.; Buzuzi, S.; Theobald, S. The gendered health workforce: Mixed methods analysis from four fragile and post-conflict contexts. Health Policy Plan. 2017, 32, v52–v62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKinstry, B. Are there too many female medical graduates? Yes. BMJ 2008, 336, 748. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nzaji, M.K.; Ngombe, L.K.; Mwamba, G.N.; Ndala, D.B.B.; Miema, J.M.; Lungoyo, C.L.; Mwimba, B.L.; Bene, A.C.M.; Musenga, E.M. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic Obs. Res. 2020, 11, 103–109. [Google Scholar] [CrossRef]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Vaccine Safety Forum; Evans, G.; Bostrom, A.; Johnston, R.B. Risk Communication and Vaccination: Summary of a Workshop. Washington (DC); National Academies Press: Washington, DC, USA, 1997; Influences on the Acceptability of Vaccine Risks. Available online: https://www.ncbi.nlm.nih.gov/books/NBK233845/ (accessed on 18 February 2021).
- Mahase, E. Covid-19: Vaccine trials need more transparency to enable scrutiny and earn public trust, say experts. BMJ 2020, 371, 4042. [Google Scholar] [CrossRef]
- Ramasamy, M.N.; Minassian, A.M.; Ewer, K.J.; Flaxman, A.L.; Folegatti, P.M.; Owens, D.R.; Voysey, M.; Aley, P.K.; Angus, B.; Babbage, G.; et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): A single-blind, randomised, controlled, phase 2/3 trial. Lancet 2020, 396, 1979–1993. [Google Scholar] [CrossRef]
- Asiimwe, R. Uganda to Access Covid-19 Vaccine from AstraZeneca-Ministry of Health, Daily Monitor. 2021. Available online: https://www.monitor.co.ug/uganda/news/national/uganda-to-access-covid-19-vaccine-from-astrazeneca-ministry-of-health-3246104 (accessed on 9 January 2021).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]

| Parameter | Variable | Frequency (n = 260) | Percent | 95% CI |
|---|---|---|---|---|
| Age (years) | >45 | 23 | 8.8 | 5.8–12.8 |
| 25–45 | 166 | 63.8 | 57.9–69.5 | |
| <25 | 71 | 27.3 | 22.2–33.0 | |
| Gender | Female | 89 | 34.2 | 28.7–40.2 |
| Male | 171 | 65.8 | 59.8–71.4 | |
| Marital status | Married | 118 | 45.4 | 39.4–51.5 |
| Single | 142 | 54.6 | 48.5–60.6 | |
| Education level | Bachelors | 107 | 41.2 | 35.3–47.2 |
| Certificate | 26 | 10.0 | 6.8–14.1 | |
| Diploma | 47 | 18.1 | 19.8–23.1 | |
| None | 8 | 3.1 | 1.3–6.0 | |
| Postgraduate | 72 | 27.7 | 22.5–33.4 | |
| Occupation | Clinician | 34 | 13.1 | 9.4–17.8 |
| Laboratory personnel | 80 | 30.8 | 25.4–36.6 | |
| Nurse | 29 | 11.2 | 7.7–15.4 | |
| Pharmacist | 23 | 8.8 | 5.8–12.8 | |
| Support staff | 94 | 36.2 | 30.5–42.1 | |
| Location | Central | 101 | 38.8 | 33.1–44.9 |
| Eastern | 72 | 27.7 | 22.5–33.4 | |
| Northern | 25 | 9.6 | 6.5–13.7 | |
| Western | 62 | 23.8 | 19.0–29.3 | |
| Preferred COVID-19 vaccine type | DNA Recombinant vaccines | 41 | 15.8 | 11.7–20.6 |
| Herbal treatments | 38 | 14.6 | 10.7–19.3 | |
| Inactivated vaccines | 89 | 34.2 | 28.7–40.2 | |
| Live attenuated vaccines | 35 | 13.5 | 9.7–18.0 | |
| No vaccine | 57 | 21.9 | 17.2–27.3 | |
| Age (years) | Minimum | 18 | ||
| Maximum | 65 | |||
| Mean ± SEM | 31.8 ± 0.5 | |||
| Parameter | Variable | N | Percentage Knowledge Score | Confidence Score | Trust Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SEM | ANOVA F (p) Value | Median (Min-Max) | Mean ± SEM | ANOVA F(p) Value | Median (Min-Max) | Mean ± SEM | ANOVA F(p) Value | Median (Min-Max) | |||
| Age | >45 | 23 | 44.2 ± 3.4 | 0.603 (0.548) | 50 (16.7–66.7) | 2.5 ± 0.2 | 0.2 (0.814) | 2.4 (0.9–4.3) | 2.4 ± 0.2 | 1.4 (0.246) | 2.6 (0.4–3.8) |
| 25–45 | 166 | 41.4 ± 1.2 | 33.3 (0.0–83.3) | 2.5 ± 0.1 | 2.5 (0.3–4.6) | 2.2 ± 0.1 | 2.0 (0.0–5.0) | ||||
| <25 | 71 | 43.4 ± 2.1 | 33.3 (0.0–83.3) | 2.6 ± 0.1 | 2.7 (0.8–4.4) | 2.4 ± 0.1 | 2.2 (0.4–4.8) | ||||
| Gender | Female | 89 | 39.3 ± 1.5 | 4.3 (0.039) | 33.3 (0.0–66.7) | 2.6 ± 0.1 | 2.1 (0.147) | 2.5 (0.9–4.6) | 2.3 ± 0.1 | 0.1 (0.747) | 2.2 (0.4–5.0) |
| Male | 171 | 43.7 ± 1.3 | 50.0 (0.0–83.3) | 2.5 ± 0.1 | 2.5 (0.3–4.4) | 2.3 ± 0.1 | 2.0 (0.0–4.8) | ||||
| Marital status | Married | 118 | 42.7 ± 1.5 | 0.2 (0.666) | 33.3 (16.7–83.3) | 2.6 ± 0.1 | 0.7 (0.413) | 2.5 (0.3–4.4) | 2.4 ± 0.1 | 4.1 (0.045) | 2.4 (0.4–5.0) |
| Single | 142 | 41.8 ± 1.4 | 33.3 (0.0–83.3) | 2.5 ± 0.1 | 2.5 (0.8–4.6) | 2.2 ± 0.1 | 2.0 (0.0–4.8) | ||||
| Education level | Bachelors | 107 | 41.0 ± 1.4 | 2.3 (0.63) | 33.3 (0.0–83.3) | 2.5 ± 0.1 | 1.4 (0.239) | 2.5 (0.6–4.1) | 2.2 ± 0.1 | 6.6 (0.001) | 2.0 (0.4–4.2) |
| Certificate | 26 | 46.2 ± 3.2 | 50.0 (16.7–66.7) | 2.8 ± 0.2 | 2.8 (1.0–4.6) | 2.9 ± 0.3 | 3.0 (0.4–5.0) | ||||
| Diploma | 47 | 46.1 ± 2.6 | 50.0 (16.7–83.3) | 2.5 ± 0.1 | 2.5 (1.0–4.4) | 2.4 ± 0.1 | 2.0 (0.6–4.8) | ||||
| None | 8 | 31.3 ± 6.6 | 33.3 (0.0–50) | 3.1 ± 0.4 | 3.1 (1.6–3.9) | 3.1 ± 0.4 | 3.0 (2.0–4.8) | ||||
| Postgraduate | 72 | 41.2 ± 1.9 | 33.3 (16.7–83.3) | 2.5 ± 0.1 | 2.5 (0.3–4.6) | 2.0 ± 0.1 | 2.0 (0.0–3.4) | ||||
| Occupation | Clinician | 34 | 39.7 ± 2.4 | 0.4 (0.825) | 33.3 (16.7–83.3) | 2.1 ± 0.1 | 3.5 (0.009) | 2.2 (0.3–3.6) | 2.1 ± 0.1 | 6.6 (0.001) | 2.0 (0.6–3.6) |
| Laboratory personnel | 80 | 42.5 ± 1.8 | 50.0 (0.0–83.3) | 2.5 ± 0.1 | 2.5 (0.8–4.3) | 1.9 ± 0.1 | 2.0 (0.0–4.4) | ||||
| Nurse | 29 | 42.5 ± 3.3 | 50.0 (16.7–83.3) | 2.5 ± 0.1 | 2.5 (1.0–4.1) | 2.5 ± 0.1 | 2.5 (1.2–5.0) | ||||
| Pharmacist | 23 | 44.9 ± 3.2 | 50.0 (16.7–83.3) | 2.4 ± 0.2 | 2.3 (0.9–4.6) | 2.2 ± 0.2 | 2.0 (1.0–4.0) | ||||
| Support staff | 94 | 42.0 ± 1.8 | 33.3 (0.0–83.3 | 2.7 ± 0.1 | 2.7 (0.6–4.6) | 2.6 ± 0.1 | 2.4 (0.4–4.8) | ||||
| Location | Central | 101 | 42.4 ± 1.5 | 1.8 (0.144) | 50 (16.7–83.3) | 2.5 ± 0.1 | 6.4 (0.001) | 2.5 (0.9–4.6) | 2.1 ± 0.1 | 10.8 (0.001) | 2.0 (0.4–4.4) |
| Eastern | 72 | 44.9 ± 1.9 | 50 (0.0–83.3) | 2.8 ± 0.1 | 2.9 (0.8–4.4) | 2.8 ± 0.1 | 2.8 (0.6–5.0) | ||||
| Northern | 25 | 36.7 ± 3.2 | 33.3 (16.7–83.3) | 2.2 ± 0.2 | 2.1 (0.9–3.4) | 2.4 ± 0.2 | 2.2 (1.2–3.8) | ||||
| Western | 62 | 40.9 ± 2.3 | 33.3 (0.0–83.3) | 2.3 ± 0.1 | 2.4 (0.3–4.1) | 2.0 ± 0.1 | 2.0 (0.0–3.8) | ||||
| Preferred COVID-19 vaccine | DRV | 41 | 42.3 ± 2.9 | 1.2 (0.319) | 33.3 (16.7–83.3) | 2.5 ± 0.1 | 1.0 (0.412) | 2.5 (0.6–4.1) | 2.2 ± 0.1 | 3.1 (0.018) | 2.0 (0.8–4.0) |
| HV | 38 | 46.9 ± 2.8 | 50 (16.6–83.3) | 2.7 ± 0.1 | 2.6 (1.3–4.3) | 2.5 ± 0.2 | 2.6 (0.8–4.6) | ||||
| IV | 89 | 41.0 ± 1.5 | 33.3 (0.0–83.3) | 2.5 ± 0.1 | 2.5 (0.8–4.6) | 2.1 ± 0.1 | 2.0 (0.0–4.2) | ||||
| LAV | 35 | 39.5 ± 2.5 | 33.3 (16.7–83.3) | 2.5 ± 0.1 | 2.6 (0.9–4.3) | 2.3 ± 0.2 | 2.2 (0.4–4.4) | ||||
| None | 57 | 42.2 ± 1.0 | 33.3 (0.0–83.3) | 2.4 ± 0.1 | 2.4 (0.3–4.6) | 2.6 ± 0.2 | 2.4 (0.6–5.0) | ||||
| Variables | Variable | Proportions by Gender | p Value | OR (95% CI) | ||
|---|---|---|---|---|---|---|
| Females | Males | Total | ||||
| Beta coronaviruses include the following except | Ebola | 67 (25.8) | 122 (46.9) | 189 (72.7) | 1 | |
| MERS | 9 (3.5) | 17 (6.5) | 26 (10.0) | 0.684 | 1.2 (0.5–2.9) | |
| SARS | 13 (5.0) | 32 (12.3) | 45 (17.3) | 0.316 | 1.5 (0.7–3.0) | |
| Do you know any company involved in COVID-19 vaccine development? | No | 65 (25.0) | 105 (40.4) | 170 (65.4) | 0.047 | 1 |
| Yes | 24 (9.2) | 66 (25.4) | 90 (34.6) | 1.8 (1.0–3.2) | ||
| Do you think breaking the COVID-19 circle involves vaccine development? | No | 12 (4.6) | 21 (8.1) | 33 (12.7) | 0.685 | 1 |
| Yes | 77 (29.6) | 150 (57.7) | 227 (87.3) | 1.2 (0.5–2.6) | ||
| Do you have fear about the COVID-19 vaccine? | No | 28 (10.8) | 48 (18.5) | 76 (29.2) | 0.310 | 1 |
| Yes | 61 (23.5) | 123 (47.3) | 184 (70.8) | 1.3 (0.8–2.4) | ||
| Have you ever participated in any clinical trial previously? | No | 79 (30.4) | 149 (57.3) | 228 (87.7) | 0.949 | 1 |
| Yes | 10 (3.8) | 22 (8.5) | 32 (12.3) | 1.0 (0.5–2.3) | ||
| I have received adequate communication on the COVID-19 vaccine trials in Uganda | No | 73 (28.1) | 133 (51.2) | 206 (79.2) | 0.569 | 1 |
| Yes | 16 (6.2) | 38 (14.6) | 54 (20.8) | 1.2 (0.6–2.4) | ||
| Variables | Frequencies on participants responses on COVID-19 | |||||
| High | Low | Moderate | ||||
| Confidence on COVID-19 vaccinations | ||||||
| I have been enlightened on WHO guidelines and stages for vaccine trials | 47 (18.1) | 120 (46.2) | 93 (35.8) | |||
| Rank the Ugandan government’s commitment to the development of a genuine COVID-19 vaccine and therapy? | 54 (20.8) | 101 (38.8) | 105 (40.4) | |||
| Confidence in the skills of Ugandans and their ability to handle the COVID-19 clinical trial? | 98 (37.7) | 44 (16.9) | 118 (45.4) | |||
| My workmates’ committment to COVID-19 control guidelines | 140 (53.8) | 18 (6.9) | 102 (39.2) | |||
| There are sufficient designated medical personnel handling COVID-19 cases at my workplace? | 93 (35.8) | 57 (21.9) | 110 (42.3) | |||
| My information about the planned COVID-19 vaccinations in Uganda | 41 (15.8) | 136 (52.3) | 83 (31.9) | |||
| Level of challenge posed by access to funding in vaccine development for Ugandan COVID-19 vaccine clinical trials | 145 (55.8) | 21 (8.1) | 94 (36.2) | |||
| My level of confidence in herbal COVID-19 treatments being promoted in Uganda | 51 (19.6) | 140 (53.8) | 69 (26.5) | |||
| Trust on COVID-19 vaccinations | ||||||
| Level of fear | 104 (40.0) | 69 (26.5) | 87 (33.5) | |||
| Level of suspicion | 118 (45.) | 58 (22.3) | 84 (32.3) | |||
| Willingness to participate in COVID-19 clinical trials | 60 (23.1) | 123 (47.3) | 77 (29.6) | |||
| Willingness to participate in a COVID-19 clinical trial | 41 (15.8) | 174 (66.9) | 45 (17.3) | |||
| Level of trust for the Ugandan national regulatory guidelines for clinical trials | 57 (21.9) | 86 (33.1) | 117 (45.0) | |||
| Source | SS | Df | MS | F-Ratio | p-Value | R-sq | R-sq (adj) |
|---|---|---|---|---|---|---|---|
| Knowledge | |||||||
| Model | 5589.81 | 15 | 372.654 | 1.47 | 0.117 | 8.29 | 2.65 |
| Residual | 61845.2 | 244 | 253.464 | ||||
| Total (Corr.) | 67435 | 259 | |||||
| Confidence | |||||||
| Model | 24.8141 | 15 | 1.654 | 2.74 | 0.001 | 14.43 | 9.17 |
| Residual | 147.151 | 244 | 0.603 | ||||
| Total (Corr.) | 171.965 | 259 | |||||
| Trust | |||||||
| Model | 59.5571 | 15 | 3.970 | 5.30 | <0.001 | 24.56 | 19.92 |
| Residual | 182.937 | 244 | 0.750 | ||||
| Total (Corr.) | 242.494 | 259 |
| Source | SS | Df | MS | F-Ratio | p-Value | Variance |
|---|---|---|---|---|---|---|
| Knowledge | ||||||
| Age group | 313.274 | 2 | 156.637 | 0.62 | 0.5399 | −2.105 |
| Gender | 2152.75 | 1 | 2152.750 | 8.49 | 0.0039 | 21.888 |
| Marital Status | 68.2873 | 1 | 68.287 | 0.27 | 0.6042 | −2.205 |
| Education | 1336.58 | 4 | 334.144 | 1.32 | 0.2637 | 1.948 |
| Occupation | 626.993 | 4 | 156.748 | 0.62 | 0.6498 | −2.392 |
| Region | 1054.89 | 3 | 351.630 | 1.39 | 0.2472 | 1.857 |
| Residual | 61845.2 | 244 | 253.464 | 253.464 | ||
| Total (corrected) | 67435 | 259 | ||||
| Confidence | ||||||
| Age group | 0.43659 | 2 | 0.218 | 0.36 | 0.697 | −0.008 |
| Gender | 0.39342 | 1 | 0.393 | 0.65 | 0.420 | −0.002 |
| Marital Status | 1.67448 | 1 | 1.674 | 2.78 | 0.097 | 0.013 |
| Education | 2.91125 | 4 | 0.728 | 1.21 | 0.309 | 0.003 |
| Occupation | 7.28699 | 4 | 1.822 | 3.02 | 0.019 | 0.030 |
| Region | 10.944 | 3 | 3.648 | 6.05 | 0.001 | 0.058 |
| Residual | 147.151 | 244 | 0.603 | 0.058 | ||
| Total (corrected) | 171.965 | 259 | ||||
| Trust | ||||||
| Age group | 2.44901 | 2 | 1.225 | 1.63 | 0.197 | 0.010 |
| Gender | 2.64235 | 1 | 2.642 | 3.52 | 0.062 | 0.022 |
| Marital Status | 4.11783 | 1 | 4.118 | 5.49 | 0.020 | 0.040 |
| Education | 10.252 | 4 | 2.563 | 3.42 | 0.010 | 0.044 |
| Occupation | 11.3622 | 4 | 2.841 | 3.79 | 0.005 | 0.052 |
| Region | 14.7894 | 3 | 4.930 | 6.58 | 0.000 | 0.079 |
| Residual | 182.937 | 244 | 0.750 | 0.750 | ||
| Total (corrected) | 242.494 | 259 |
| Variables | Average ± SD | Factor 1 α | Factor 2 α | Estimated Communality | Specific Variance |
|---|---|---|---|---|---|
| Knowledge | 42.18 ± 16.14 | 0.557 | −0.828 | 0.636 | 0.364 |
| Confidence | 2.52 ± 0.81 | 0.815 | 0.341 | 0.674 | 0.326 |
| Trust | 2.29 ± 0.97 | 0.841 | 0.218 | 0.547 | 0.453 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kasozi, K.I.; Laudisoit, A.; Osuwat, L.O.; Batiha, G.E.-S.; Al Omairi, N.E.; Aigbogun, E.; Ninsiima, H.I.; Usman, I.M.; DeTora, L.M.; MacLeod, E.T.; et al. A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda. Vaccines 2021, 9, 253. https://doi.org/10.3390/vaccines9030253
Kasozi KI, Laudisoit A, Osuwat LO, Batiha GE-S, Al Omairi NE, Aigbogun E, Ninsiima HI, Usman IM, DeTora LM, MacLeod ET, et al. A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda. Vaccines. 2021; 9(3):253. https://doi.org/10.3390/vaccines9030253
Chicago/Turabian StyleKasozi, Keneth Iceland, Anne Laudisoit, Lawrence Obado Osuwat, Gaber El-Saber Batiha, Naif E. Al Omairi, Eric Aigbogun, Herbert Izo Ninsiima, Ibe Michael Usman, Lisa M. DeTora, Ewan Thomas MacLeod, and et al. 2021. "A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda" Vaccines 9, no. 3: 253. https://doi.org/10.3390/vaccines9030253
APA StyleKasozi, K. I., Laudisoit, A., Osuwat, L. O., Batiha, G. E.-S., Al Omairi, N. E., Aigbogun, E., Ninsiima, H. I., Usman, I. M., DeTora, L. M., MacLeod, E. T., Nalugo, H., Crawley, F. P., Bierer, B. E., Mwandah, D. C., Kato, C. D., Kiyimba, K., Ayikobua, E. T., Lillian, L., Matama, K., ... Welburn, S. C. (2021). A Descriptive-Multivariate Analysis of Community Knowledge, Confidence, and Trust in COVID-19 Clinical Trials among Healthcare Workers in Uganda. Vaccines, 9(3), 253. https://doi.org/10.3390/vaccines9030253












