Long-Term Follow-Up of Spinal Stenosis Inpatients Treated with Integrative Korean Medicine Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
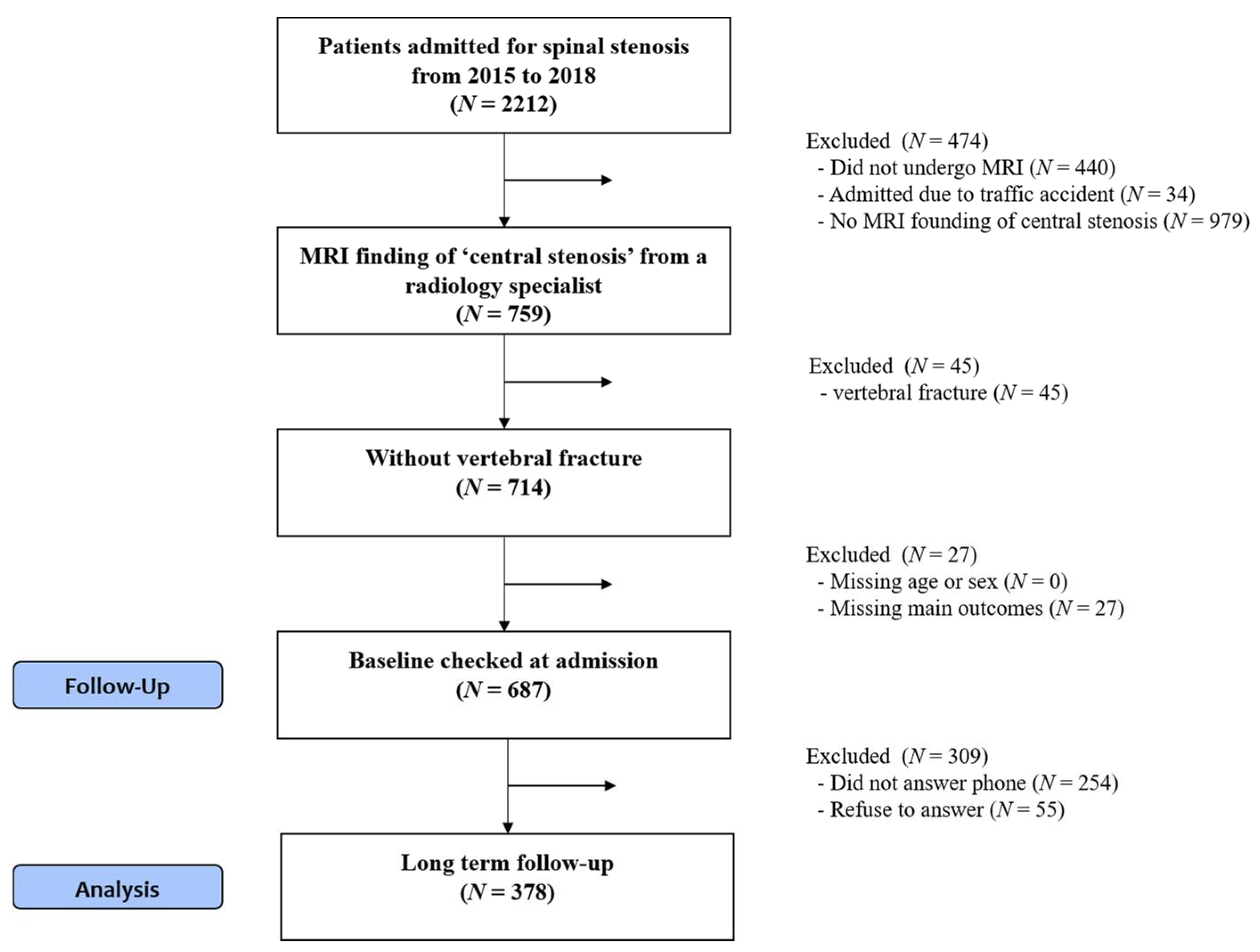
2.2. Participants
2.3. Intervention
2.3.1. Herbal Medicine
2.3.2. Acupuncture
2.3.3. Pharmacopuncture
2.3.4. Bee-Venom Pharmacopuncture
2.3.5. Chuna Manipulation
2.4. Outcome Measures
2.4.1. Primary Outcome
NRS Score for Back Pain
2.4.2. Secondary Outcomes
NRS Score for Leg Pain
ODI
Five-Level EuroQol 5-Dimension (EQ-5D-5L) Questionnaire
Walking Time
Survey at Long-Term Follow-up
2.5. Statistical Analysis
3. Results
3.1. Participants
3.2. Basic Characteristics
3.3. Intervention
3.4. Outcome Changes
3.5. Survival Analysis
3.6. Survey at Long-Term Follow-Up
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weinstein, J.N.; Tosteson, T.D.; Lurie, J.D.; Tosteson, A.N.; Blood, E.; Hanscom, B.; Herkowitz, H.; Cammisa, F.; Albert, T.; Boden, S.D.; et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N. Engl. J. Med. 2008, 358, 794–810. [Google Scholar] [CrossRef] [Green Version]
- Kalichman, L.; Cole, R.; Kim, D.H.; Li, L.; Suri, P.; Guermazi, A.; Hunter, D.J. Spinal stenosis prevalence and association with symptoms: The Framingham Study. Spine J. 2009, 9, 545–550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deyo, R.A.; Mirza, S.K.; Martin, B.I. Error in trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2011, 306, 1088. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Lurie, J.D.; Olson, P.; Bronner, K.K.; Fisher, E.S.; Morgan, M.T.S. United States trends and regional variations in lumbar spine surgery: 1992–2003. Spine 2006, 31, 2707. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Chung, C.K.; Park, C.S.; Choi, B.; Hahn, S.; Kim, M.J.; Lee, K.S.; Park, B.J. Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: A nationwide cohort study. Spine J. 2013, 13, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Martin, B.I.; Kreuter, W.; Jarvik, J.G.; Angier, H.; Mirza, S.K. Revision surgery following operations for lumbar stenosis. J. Bone Jt. Surg. Am. 2011, 93, 1979–1986. [Google Scholar] [CrossRef]
- Patel, J.; Osburn, I.; Wanaselja, A.; Nobles, R. Optimal treatment for lumbar spinal stenosis: An update. Curr. Opin. Anaesthesiol. 2017, 30, 598–603. [Google Scholar] [CrossRef]
- Zaina, F.; Tomkins-Lane, C.; Carragee, E.; Negrini, S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Atlas, S.J.; Keller, R.B.; Wu, Y.A.; Deyo, R.A.; Singer, D.E. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine 2005, 30, 936–943. [Google Scholar] [CrossRef] [Green Version]
- Delitto, A.; Piva, S.R.; Moore, C.G.; Welch, W.C. Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis. Ann. Intern. Med. 2015, 163, 397–398. [Google Scholar] [CrossRef]
- Bodeker, G. Lessons on integration from the developing world’s experience. BMJ 2001, 322, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Jung, B.; Bae, S.; Kim, S. Use of Western Medicine and Traditional Korean Medicine for Joint Disorders: A Retrospective Comparative Analysis Based on Korean Nationwide Insurance Data. Evid. Based Complement. Altern. Med. 2017, 2017, 2038095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, Y.J.; Shin, J.-S.; Lee, J.; Kim, M.-r.; Ahn, Y.-j.; Shin, Y.-s.; Park, K.B.; Shin, B.-C.; Lee, M.S.; Kim, J.-H. Survey of integrative lumbar spinal stenosis treatment in Korean medicine doctors: Preliminary data for clinical practice guidelines. BMC Complementary Altern. Med. 2017, 17, 425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hadianfard, M.J.; Aminlari, A.; Daneshian, A.; Safarpour, A.R. Effect of Acupuncture on Pain and Quality of Life in Patients with Lumbar Spinal Stenosis: A Case Series Study. J. Acupunct. Meridian Stud. 2016, 9, 178–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.; Jeong, Y.; Youn, Y.; Choi, J.; Kim, J.; Chung, W.; Kim, T.H. Nonoperative Korean Medicine Combination Therapy for Lumbar Spinal Stenosis: A Retrospective Case-Series Study. Evid. Based Complement. Altern. Med. 2015, 2015, 263898. [Google Scholar] [CrossRef] [Green Version]
- Oka, H.; Matsudaira, K.; Takano, Y.; Kasuya, D.; Niiya, M.; Tonosu, J.; Fukushima, M.; Oshima, Y.; Fujii, T.; Tanaka, S.; et al. A comparative study of three conservative treatments in patients with lumbar spinal stenosis: Lumbar spinal stenosis with acupuncture and physical therapy study (LAP study). BMC Complementary Altern. Med. 2018, 18, 19. [Google Scholar] [CrossRef] [Green Version]
- Qin, Z.; Ding, Y.; Xu, C.; Kwong, J.S.W.; Ji, Y.; Wu, A.; Wu, J.; Liu, Z. Acupuncture vs Noninsertive Sham Acupuncture in Ageing Patients with Degenerative Lumbar Spinal Stenosis: A Randomized Controlled Trial. Am. J. Med. 2019. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, Y.R.; Baik, S.K.; Noh, S.H.; Kim, D.H.; Lee, S.W.; Yang, G.Y. Acupuncture for patients with lumbar spinal stenosis: A randomised pilot trial. Acupunct. Med. J. Br. Med. Acupunct. Soc. 2016, 34, 267–274. [Google Scholar] [CrossRef]
- Kim, K.H.; Kim, T.H.; Lee, B.R.; Kim, J.K.; Son, D.W.; Lee, S.W.; Yang, G.Y. Acupuncture for lumbar spinal stenosis: A systematic review and meta-analysis. Complement. Ther. Med. 2013, 21, 535–556. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.-J.; Lee, H.-S.; Shin, J.-S.; Lee, S.-H.; Park, B.-M.; Youn, Y.-S.; Lee, S.K. Modulation of acute and chronic inflammatory processes by a traditional medicine preparation GCSB-5 both in vitro and in vivo animal models. J. Ethnopharmacol. 2010, 130, 450–459. [Google Scholar] [CrossRef]
- Kim, T.-H.; Yoon, S.-J.; Lee, W.-C.; Kim, J.-K.; Shin, J.; Lee, S.; Lee, S.-M. Protective effect of GCSB-5, an herbal preparation, against peripheral nerve injury in rats. J. Ethnopharmacol. 2011, 136, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-K.; Park, S.-W.; Kang, J.-W.; Kim, Y.-J.; Lee, S.Y.; Shin, J.; Lee, S.; Lee, S.-M. Effect of GCSB-5, a herbal formulation, on monosodium iodoacetate-induced osteoarthritis in rats. Evid. Based Complement. Altern. Med. 2012, 2012, 730907. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. 2011, 63, S240–S252. [Google Scholar]
- Solodiuk, J.C.; Scott-Sutherland, J.; Meyers, M.; Myette, B.; Shusterman, C.; Karian, V.E.; Harris, S.K.; Curley, M.A. Validation of the Individualized Numeric Rating Scale (INRS): A pain assessment tool for nonverbal children with intellectual disability. Pain 2010, 150, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Jeon, C.-H.; Kim, D.-J.; Kim, S.-K.; Kim, D.-J.; Lee, H.-M.; Park, H.-J. Validation in the cross-cultural adaptation of the Korean version of the Oswestry Disability Index. J. Korean Med. Sci. 2006, 21, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Ahn, J.; Ock, M.; Shin, S.; Park, J.; Luo, N.; Jo, M.-W. The EQ-5D-5L valuation study in Korea. Qual. Life Res. 2016, 25, 1845–1852. [Google Scholar] [CrossRef]
- Conway, J.; Tomkins, C.C.; Haig, A.J. Walking assessment in people with lumbar spinal stenosis: Capacity, performance, and self-report measures. Spine J. 2011, 11, 816–823. [Google Scholar] [CrossRef] [Green Version]
- Ammendolia, C.; Stuber, K.; Tomkins-Lane, C.; Schneider, M.; Rampersaud, Y.R.; Furlan, A.D.; Kennedy, C.A. What interventions improve walking ability in neurogenic claudication with lumbar spinal stenosis? A systematic review. Eur. Spine J. 2014, 23, 1282–1301. [Google Scholar] [CrossRef]
- Jespersen, A.B. Correlation between the Oswestry Disability Index and objective measurements of walking capacity and performance in patients with lumbar spinal stenosis: A systematic literature review. Eur. Spine J. 2018, 27, 1604–1613. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005, 113, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.A.; Whitman, J.M.; Houser, J.L.; Wainner, R.S.; Childs, J.D. Psychometric properties of selected tests in patients with lumbar spinal stenosis. Spine J. 2012, 12, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Copay, A.G.; Glassman, S.D.; Subach, B.R.; Berven, S.; Schuler, T.C.; Carreon, L.Y. Minimum clinically important difference in lumbar spine surgery patients: A choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J. 2008, 8, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, S.; Paquet, J.; Bailey, C.; Nataraj, A.; Stratton, A.; Johnson, M.; Salo, P.; Christie, S.; Fisher, C.; Hall, H. Effect of spinal decompression on back pain in lumbar spinal stenosis: A Canadian Spine Outcomes Research Network (CSORN) study. Spine J. 2019, 19, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; So, Y.; Johnston, G. Analyzing Interval-Censored Data with the ICLIFETEST Procedure; Paper SAS279-2014; SAS Institute: Cary, NC, USA, 2014. [Google Scholar]
- Wellner, J.A.; Zhan, Y. A hybrid algorithm for computation of the nonparametric maximum likelihood estimator from censored data. J. Am. Stat. Assoc. 1997, 92, 945–959. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Yong-Ik, K.; Seung-Taek, K. 2018 National Health Insurance Statistical Yearbook; Health Insurance Review & Assessment Service, National Health Insurance Service: Gangwon-do, Korea, 2018; pp. 638–680. [Google Scholar]
- Mannion, A.F.; Junge, A.; Elfering, A.; Dvorak, J.; Porchet, F.; Grob, D. Great expectations: Really the novel predictor of outcome after spinal surgery? Spine 2009, 34, 1590–1599. [Google Scholar] [CrossRef]
- Lattig, F.; Fekete, T.F.; O’Riordan, D.; Kleinstück, F.S.; Jeszenszky, D.; Porchet, F.; Mutter, U.; Mannion, A.F. A comparison of patient and surgeon preoperative expectations of spinal surgery. Spine 2013, 38, 1040–1048. [Google Scholar] [CrossRef]
- Tuomainen, I.; Pesonen, J.; Rade, M.; Pakarinen, M.; Leinonen, V.; Kröger, H.; Airaksinen, O.; Aalto, T. Preoperative Predictors of Better Long-term Functional Ability and Decreased Pain Following LSS Surgery: A Prospective Observational Study with a 10-year Follow-Up Period. Spine 2020, 45, 776–783. [Google Scholar] [CrossRef]
- Altinel, F.; Yerli, H. Clinical and Radiological Analysis of Dural Sac Diameter in Lumbar Spinal Stenosis. EJMI 2020, 4, 149–154. [Google Scholar] [CrossRef]
- Iwahashi, H.; Yoshimura, N.; Hashizume, H.; Yamada, H.; Oka, H.; Matsudaira, K.; Shinto, K.; Ishimoto, Y.; Nagata, K.; Teraguchi, M. The association between the cross-sectional area of the dural sac and low back pain in a large population: The Wakayama Spine Study. PLoS ONE 2016, 11, e0160002. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, R.T.; Bouknaitir, J.B.; Fruensgaard, S.; Carreon, L.; Andersen, M. Prognostic factors for satisfaction after decompression surgery for lumbar spinal stenosis. Neurosurgery 2018, 82, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Nerland, U.S.; Jakola, A.S.; Giannadakis, C.; Solheim, O.; Weber, C.; Nygaard, Ø.P.; Solberg, T.K.; Gulati, S. The risk of getting worse: Predictors of deterioration after decompressive surgery for lumbar spinal stenosis: A multicenter observational study. World Neurosurg. 2015, 84, 1095–1102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekelund, S. ROC curves—What are they and how are they used? Point Care 2012, 11, 16–21. [Google Scholar] [CrossRef]
- Ogink, P.T.; van Wulfften Palthe, O.; Teunis, T.; Bono, C.M.; Harris, M.B.; Schwab, J.H.; Cha, T.D. Practice variation among surgeons treating lumbar spinal stenosis in a single institution. Spine 2019, 44, 510–516. [Google Scholar] [CrossRef]


| Values | |
|---|---|
| Age (years) | 62.21 ± 12.54 |
| Sex | |
| Male | 127 (33.6) |
| Female | 251 (66.4) |
| Smoking | |
| No | 318 (84.1) |
| Yes | 57 (15.1) |
| Drinking | |
| No | 287 (75.9) |
| Yes | 84 (22.2) |
| Body mass index (kg/m2) | 24.96 ± 7.96 |
| Pain radiating to the leg | |
| None | 69 (18.3) |
| Unilateral (right) | 88 (23.3) |
| Unilateral (left) | 101 (26.7) |
| Bilateral | 120 (31.7) |
| Walking time (min) | 19.14 ± 19.05 |
| Neurogenic claudication | |
| Yes | 65 (17.2) |
| No | 184 (48.7) |
| Muscle weakness | |
| Big toe extension | |
| Normal | 350 (92.6) |
| Weakness | 28 (7.4) |
| Dorsiflexion | |
| Normal | 352 (93.1) |
| Weakness | 25 (6.6) |
| Plantar flexion | |
| Normal | 363 (96.0) |
| Weakness | 15 (4.0) |
| Previous spine surgery | |
| Yes | 50 (13.2) |
| No | 311 (82.3) |
| NRS score for back pain | 5.73 ± 1.45 |
| NRS score for leg pain | 5.85 ± 1.30 |
| ODI | 45.72 ± 17.86 |
| DSCA (mm2) | 58.26 ± 26.37 |
| Accompanying HIVD | 115.0 (30.4) |
| Admission | Discharge | Long-Term Follow-Up | |
|---|---|---|---|
| NRS score for back pain | |||
| Outcome | 5.73 (5.58, 5.87) | 3.66 (3.51, 3.82) | 3.53 (3.35, 3.70) |
| Change from admission | −2.06 (−2.23, −1.9) | −2.20 (−2.41, −1.99) | |
| p-value | <0.001 | <0.001 | |
| NRS score for leg pain | |||
| Outcome | 4.78 (4.53, 5.04) | 3.33 (3.14, 3.51) | 2.51 (2.30, 2.72) |
| Change from admission | −1.46 (−1.69, −1.22) | −2.28 (−2.59, −1.96) | |
| p-value | <0.001 | <0.001 | |
| ODI | |||
| Outcome | 45.72 (43.91, 47.52) | 33.94 (32.15, 35.73) | 28.41 (26.46, 30.36) |
| Change from admission | −11.78 (−13.49, −10.07) | −17.31 (−19.6, −15.02) | |
| p-value | <0.001 | <0.001 | |
| Walking time (min) | |||
| Outcome | 20.72 (17.63, 23.81) | 49.55 (46.12, 52.98) | |
| Change from admission | 28.83 (24.65, 33.01) | ||
| p-value | <0.001 | ||
| EQ-5D-5L | |||
| Outcome | 0.58 (0.55, 0.60) | 0.66 (0.63, 0.68) | 0.80 (0.79, 0.81) |
| Change from admission | 0.08 (0.05, 0.11) | 0.22 (0.19, 0.25) | |
| p-value | <0.001 | <0.001 |
| Outcome | Time (Days, 95% CI) | N (%) of Improvement | |
|---|---|---|---|
| Discharge | Long-Term Follow-Up | ||
| NRS score for back pain | 9 (8, 10) | 216 (57.1) | 232 (61.4) |
| NRS score for leg pain | 12 (10, 12) | 186 (49.2) | 230 (60.8) |
| ODI | 8 (6, 8) | 176 (46.6) | 215 (56.9) |
| Values | |
|---|---|
| Period from discharge to long-term follow-up (days) | |
| Average | 1199.21 ± 392.75 |
| Median | 1193 (839, 1488) |
| Recommendation for surgery prior to admission | 210 (55.6) |
| Experience of surgery after discharge | |
| No | 339 (89.9) |
| Yes | 38 (10.1) |
| Current treatment | |
| None | 198 (52.4) |
| KM | 65 (17.2) |
| WM | 73 (19.3) |
| KM + WM | 42 (11.1) |
| Preference | |
| Preferred treatment | |
| KM | 264 (69.8) |
| WM | 19 (5.0) |
| Similar | 95 (25.1) |
| Degree of preference | |
| KM | 7.78 ± 1.72 |
| WM | 4.90 ± 2.45 |
| PGIC | |
| Very much improved | 92 (24.3) |
| Much improved | 161 (42.6) |
| A little improved | 107 (28.3) |
| No change | 12 (3.2) |
| A little worse | 6 (1.6) |
| Much worse | 0 (0.0) |
| Very much worse | 0 (0.0) |
| Level of satisfaction with the KM treatment received during hospital stay | |
| Very satisfied | 155 (41.0) |
| Satisfied | 183 (48.4) |
| Neutral | 37 (9.8) |
| Dissatisfied | 3 (0.8) |
| Very dissatisfied | 0 (0.0) |
| Degree of helpfulness of inpatient treatment in returning to activities of daily living and work | |
| Very helpful | 137 (36.3) |
| Helpful | 186 (49.3) |
| Average | 49 (13.0) |
| Not helpful | 5 (1.3) |
| Not helpful at all | 0 (0.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.; Shin, J.-S.; Moon, Y.-J.; Ryu, G.; Shin, W.; Lee, J.; Lim, S.; Jeon, H.A.; Seo, J.-Y.; Wang, W.H.; et al. Long-Term Follow-Up of Spinal Stenosis Inpatients Treated with Integrative Korean Medicine Treatment. J. Clin. Med. 2021, 10, 74. https://doi.org/10.3390/jcm10010074
Kim D, Shin J-S, Moon Y-J, Ryu G, Shin W, Lee J, Lim S, Jeon HA, Seo J-Y, Wang WH, et al. Long-Term Follow-Up of Spinal Stenosis Inpatients Treated with Integrative Korean Medicine Treatment. Journal of Clinical Medicine. 2021; 10(1):74. https://doi.org/10.3390/jcm10010074
Chicago/Turabian StyleKim, Doori, Joon-Shik Shin, Young-Joo Moon, Gwanghyun Ryu, Wonbin Shin, Jiyun Lee, Suyeon Lim, Hyun A Jeon, Ji-Yeon Seo, Wu Hao Wang, and et al. 2021. "Long-Term Follow-Up of Spinal Stenosis Inpatients Treated with Integrative Korean Medicine Treatment" Journal of Clinical Medicine 10, no. 1: 74. https://doi.org/10.3390/jcm10010074
APA StyleKim, D., Shin, J.-S., Moon, Y.-J., Ryu, G., Shin, W., Lee, J., Lim, S., Jeon, H. A., Seo, J.-Y., Wang, W. H., Lee, J.-H., Park, K. S., Lee, Y. J., & Ha, I.-H. (2021). Long-Term Follow-Up of Spinal Stenosis Inpatients Treated with Integrative Korean Medicine Treatment. Journal of Clinical Medicine, 10(1), 74. https://doi.org/10.3390/jcm10010074





