Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring
Abstract
1. Introduction
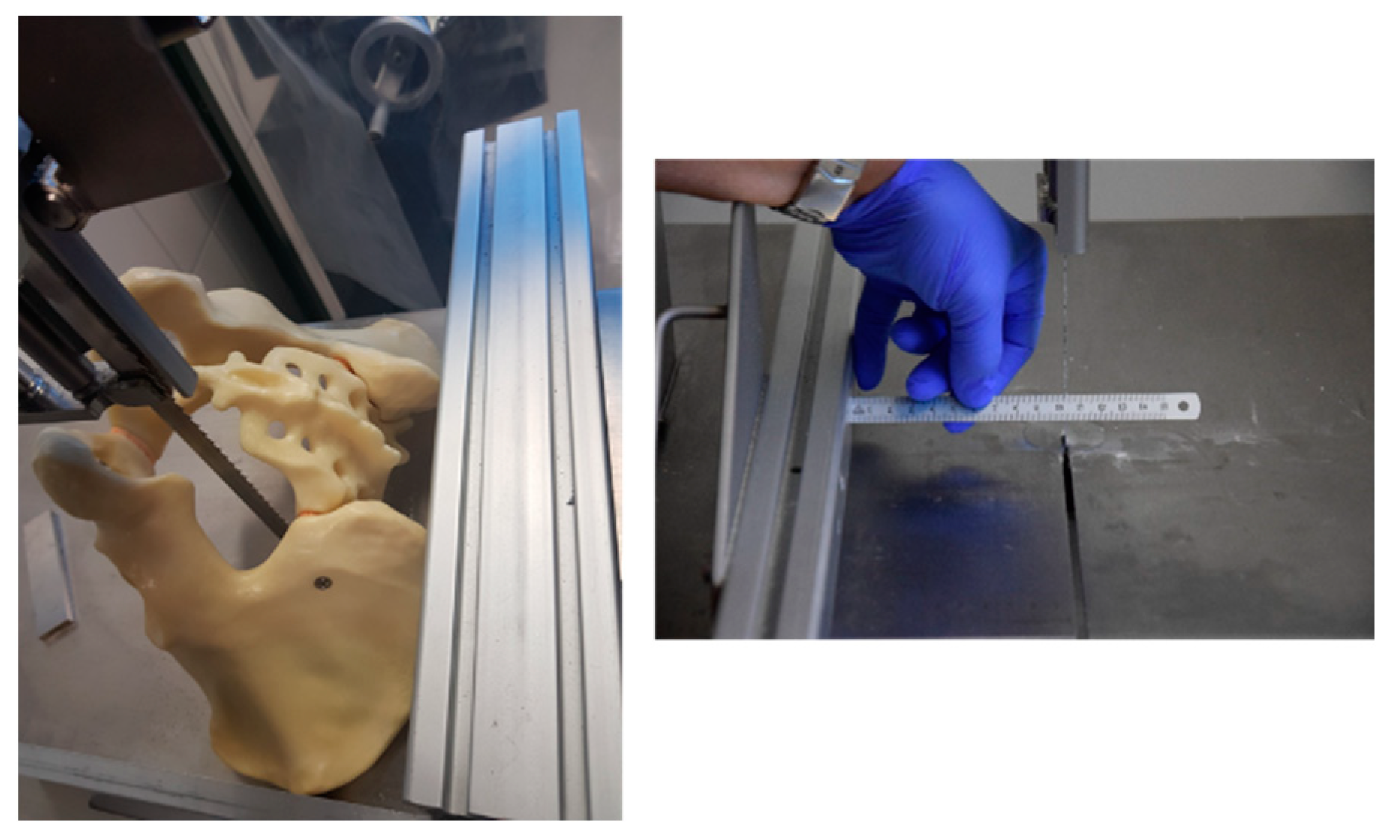
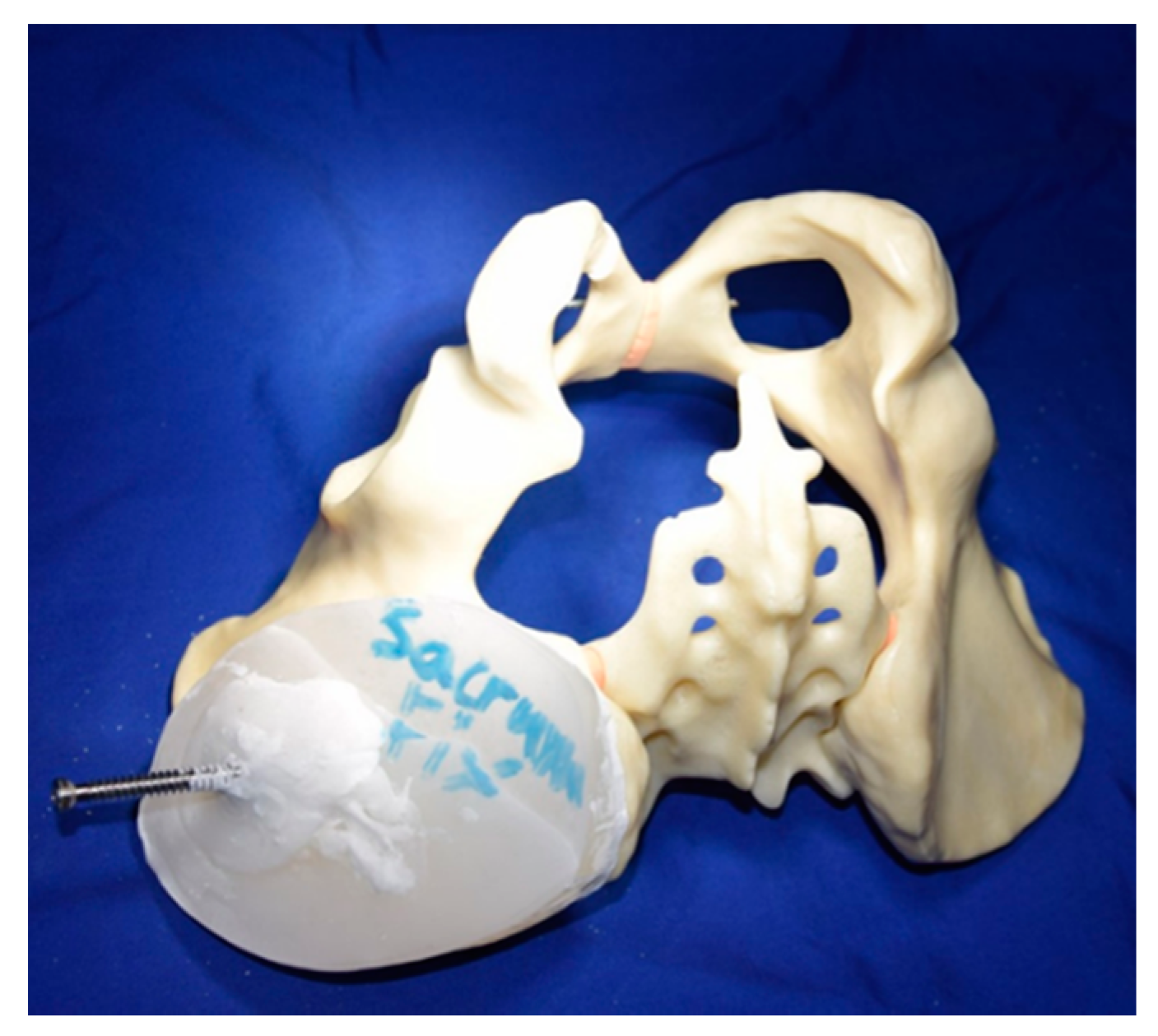
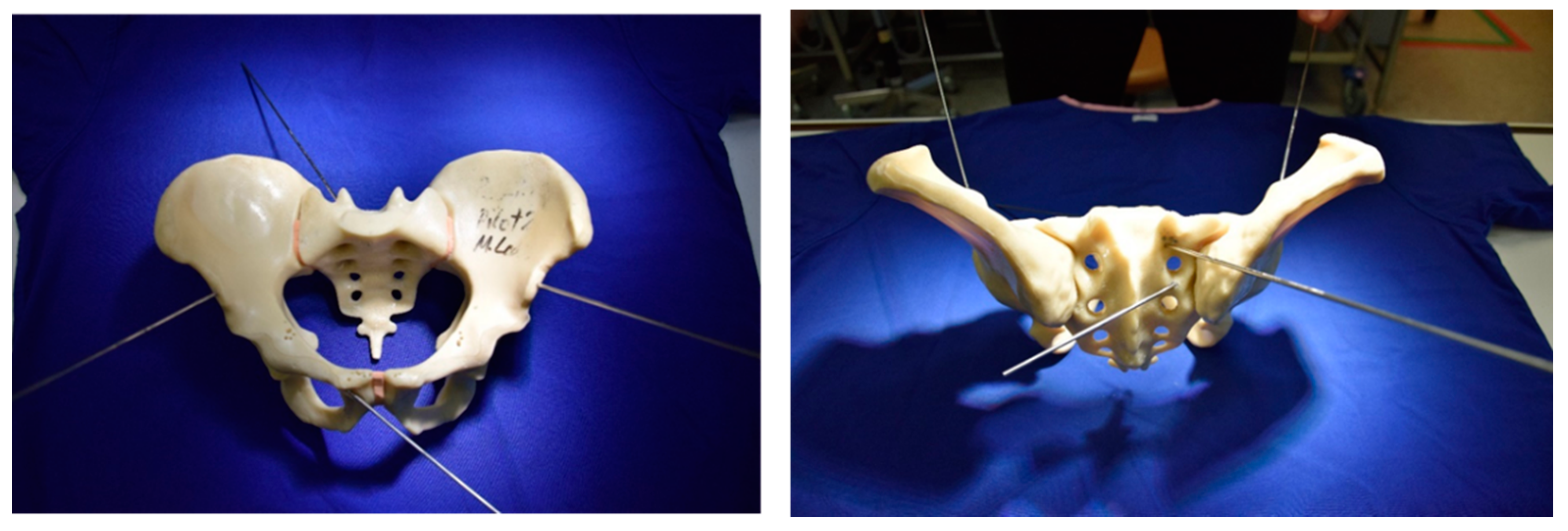
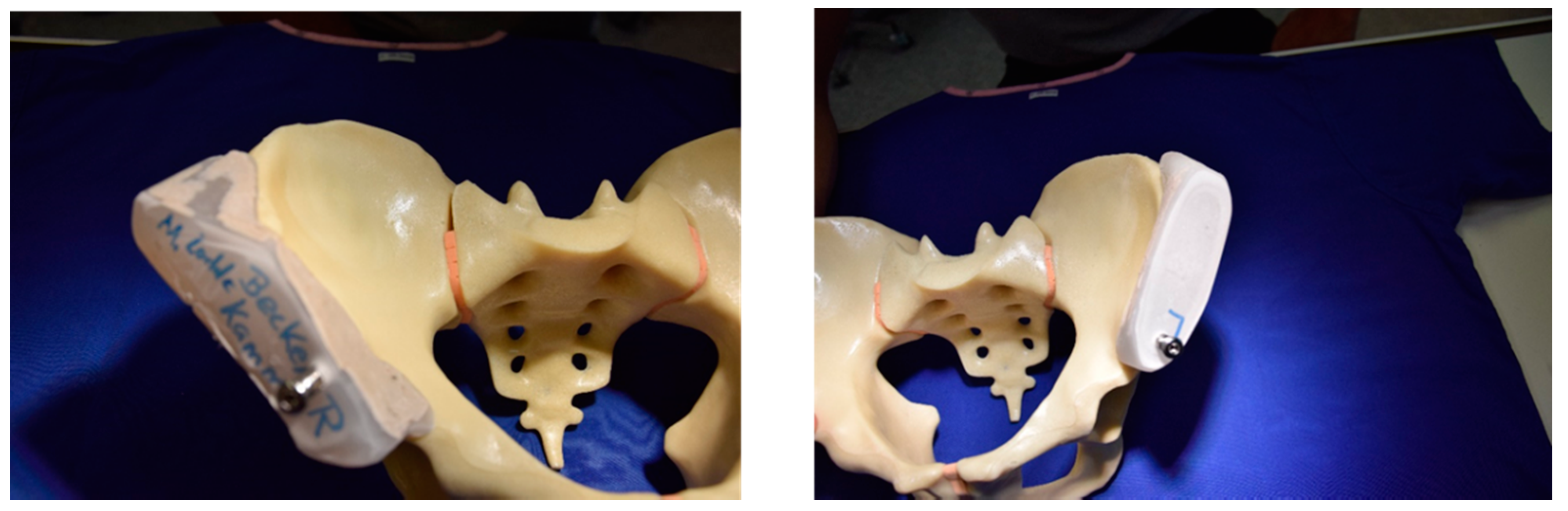
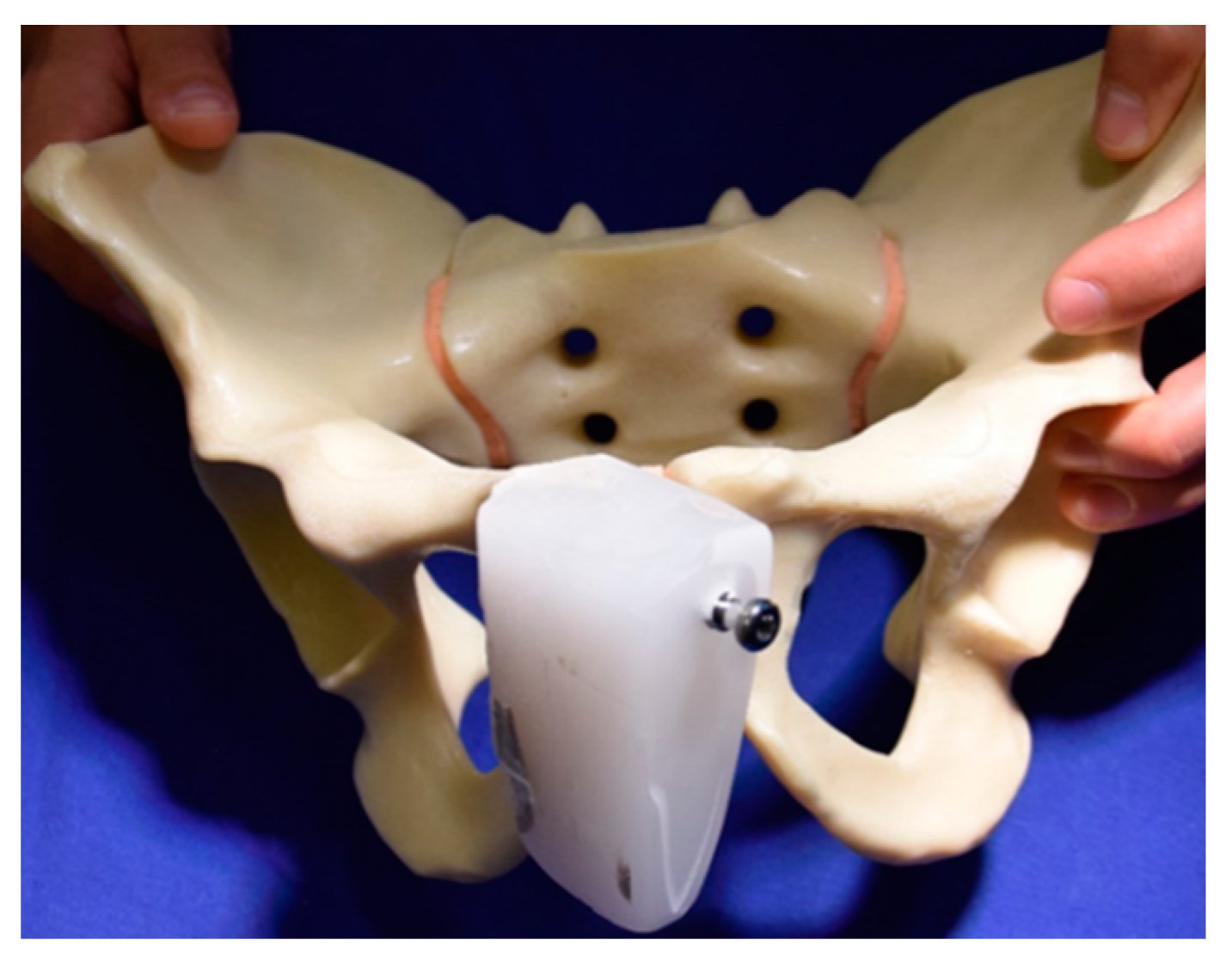
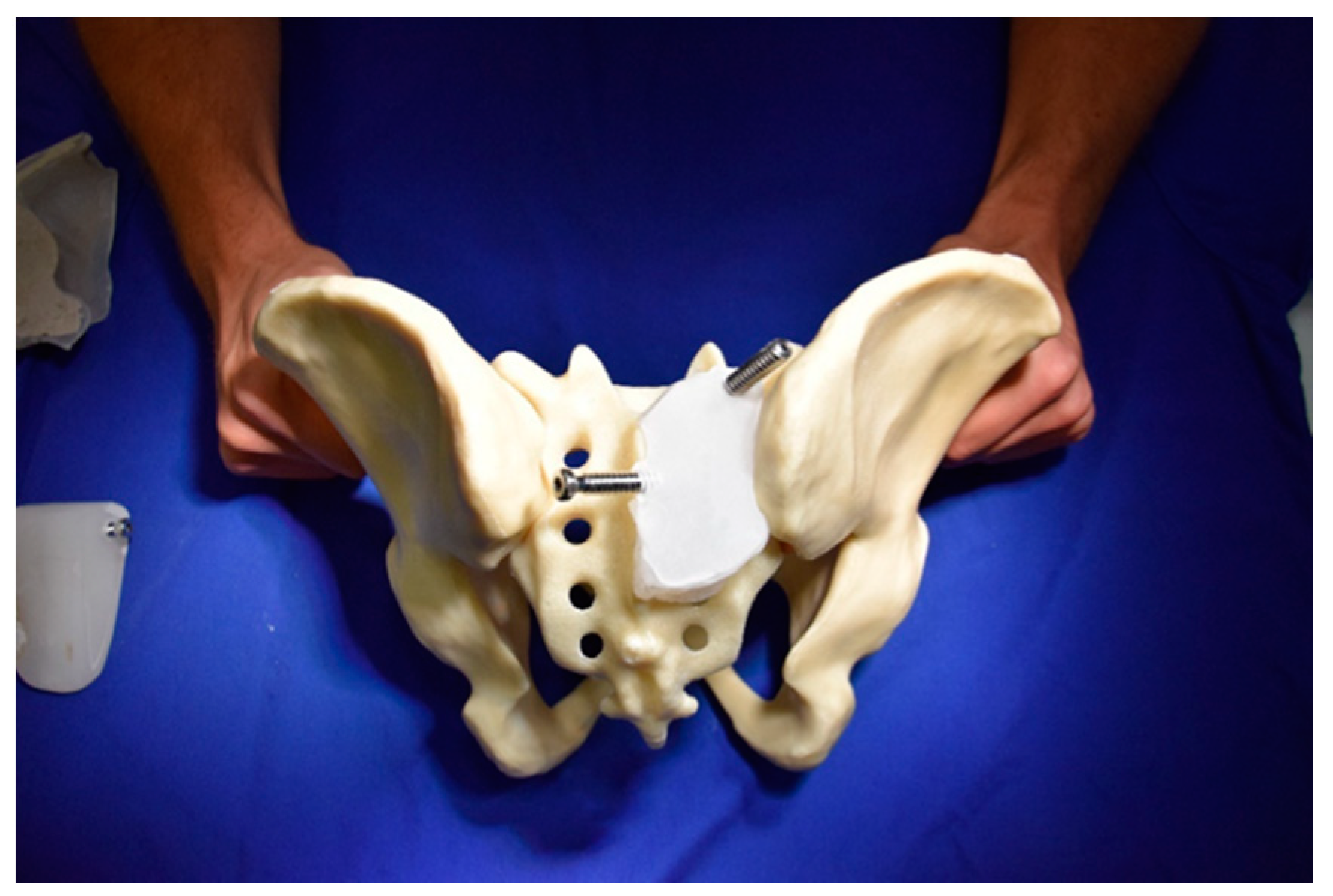
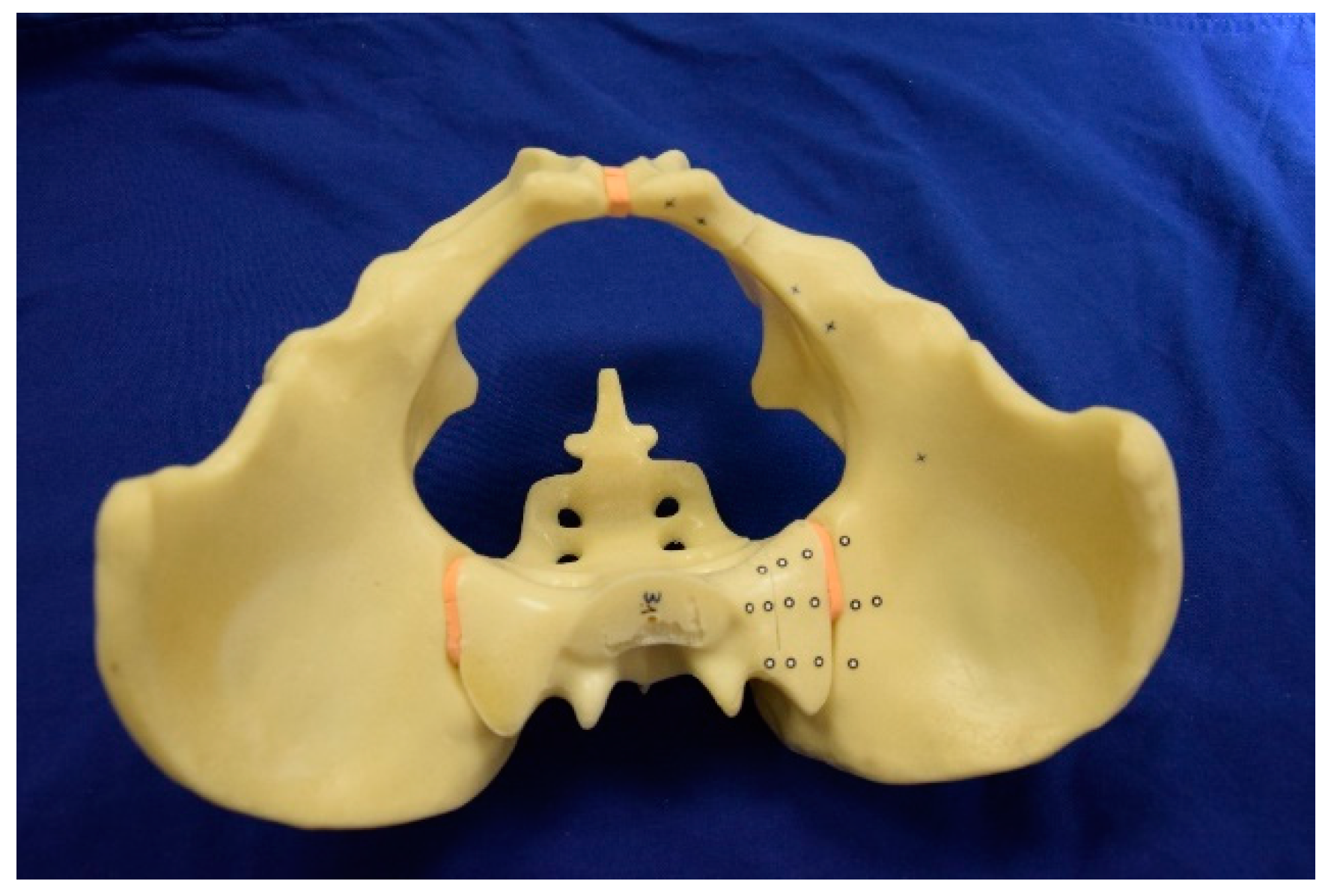
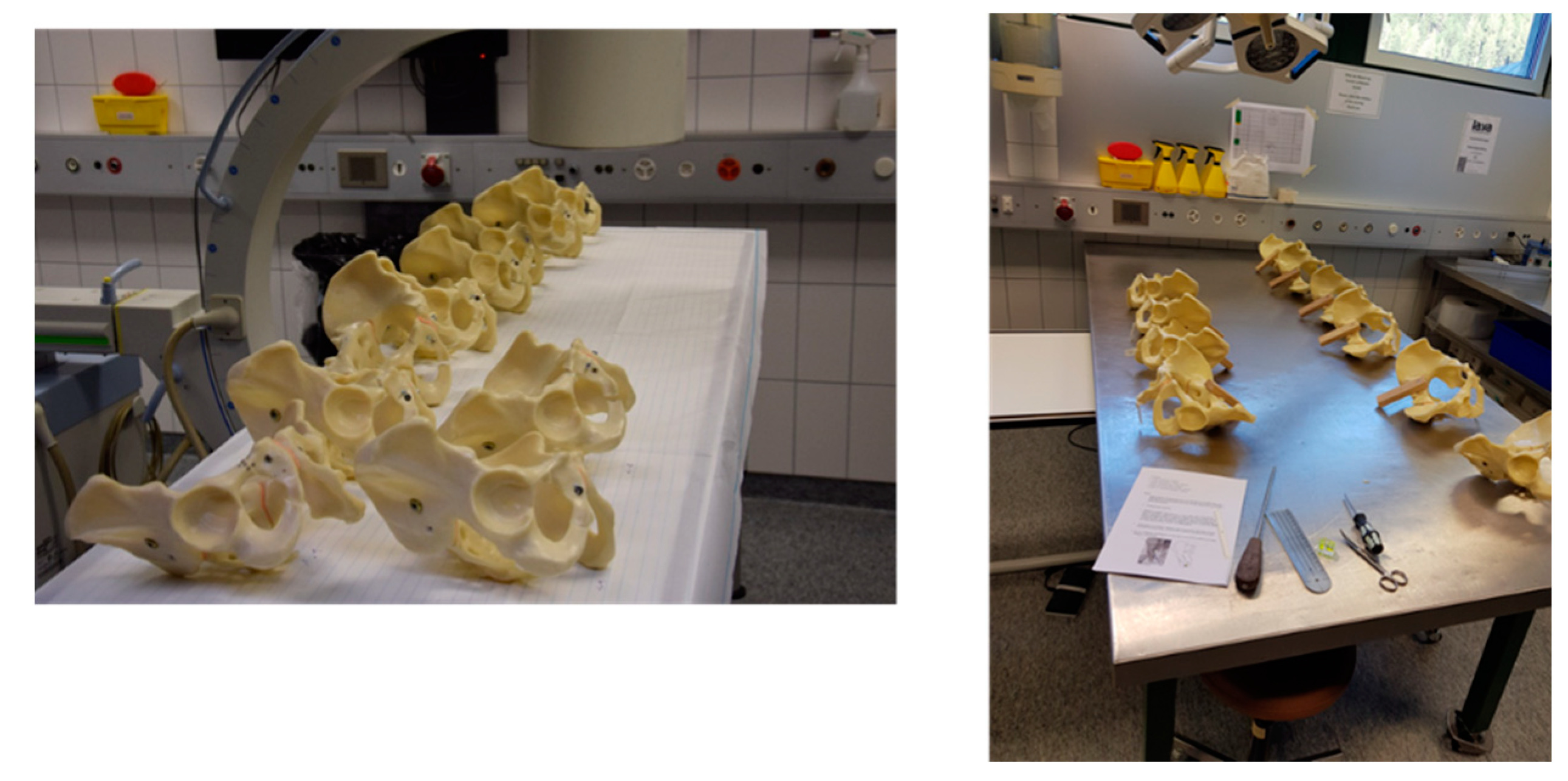
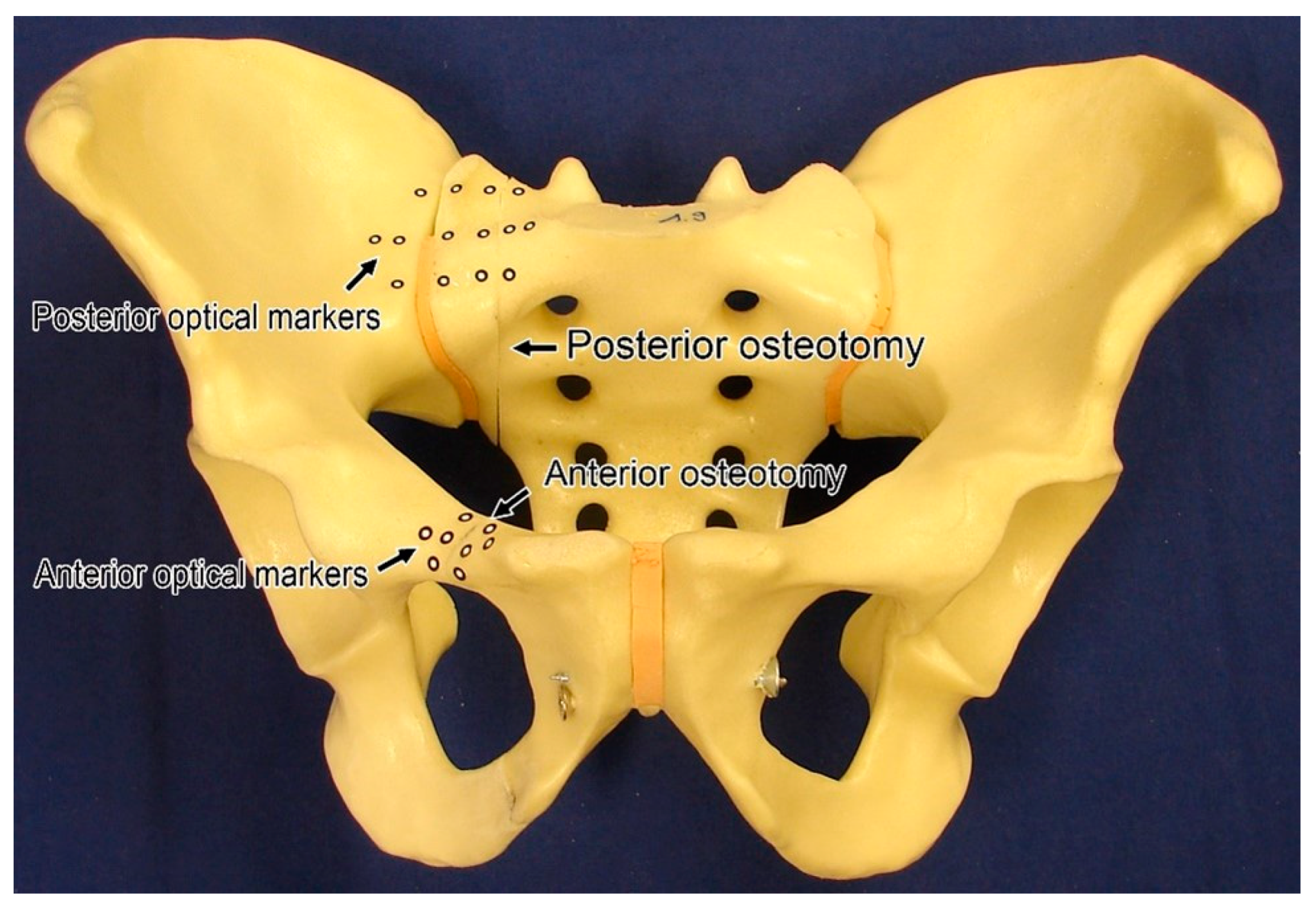
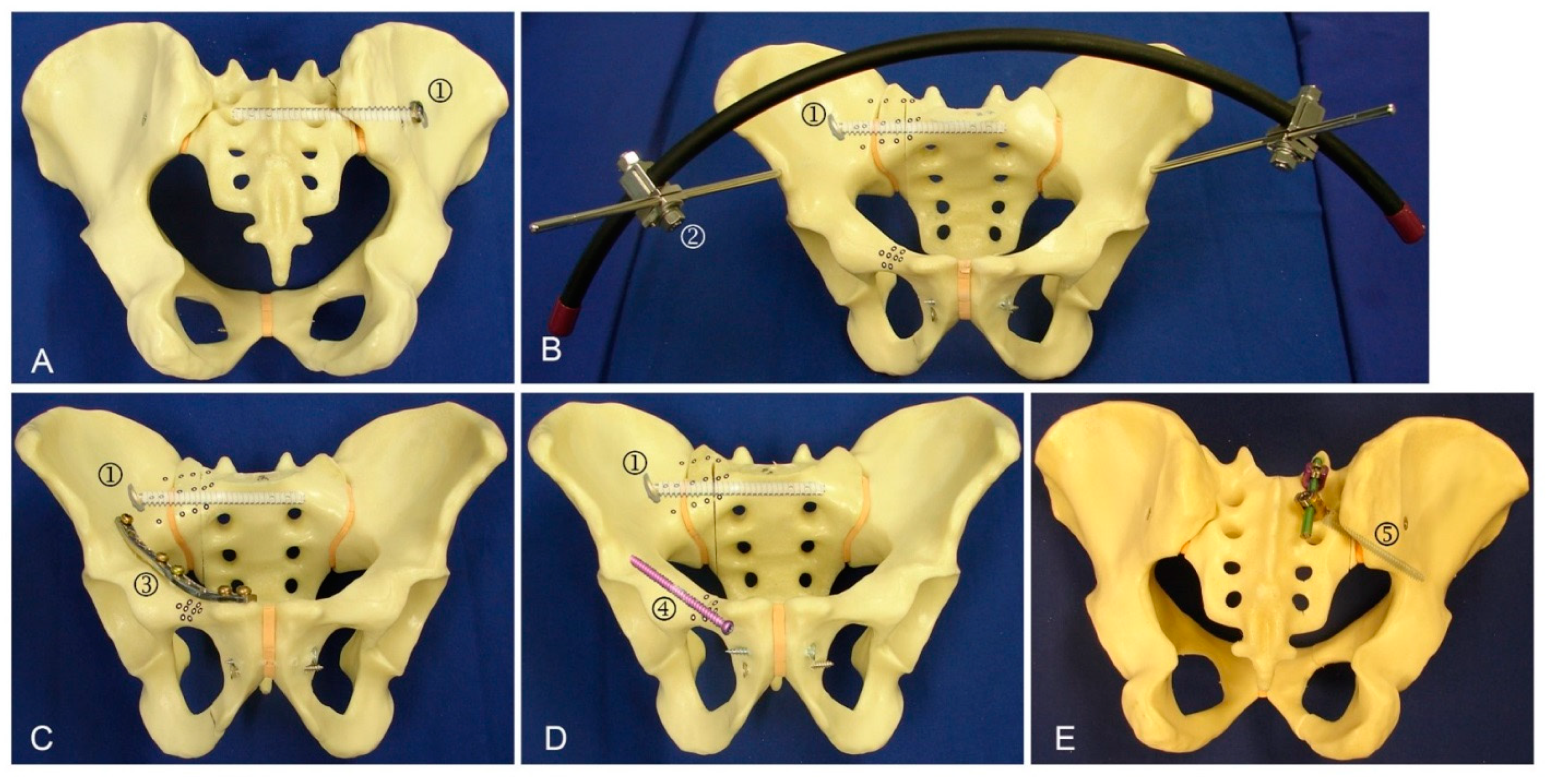
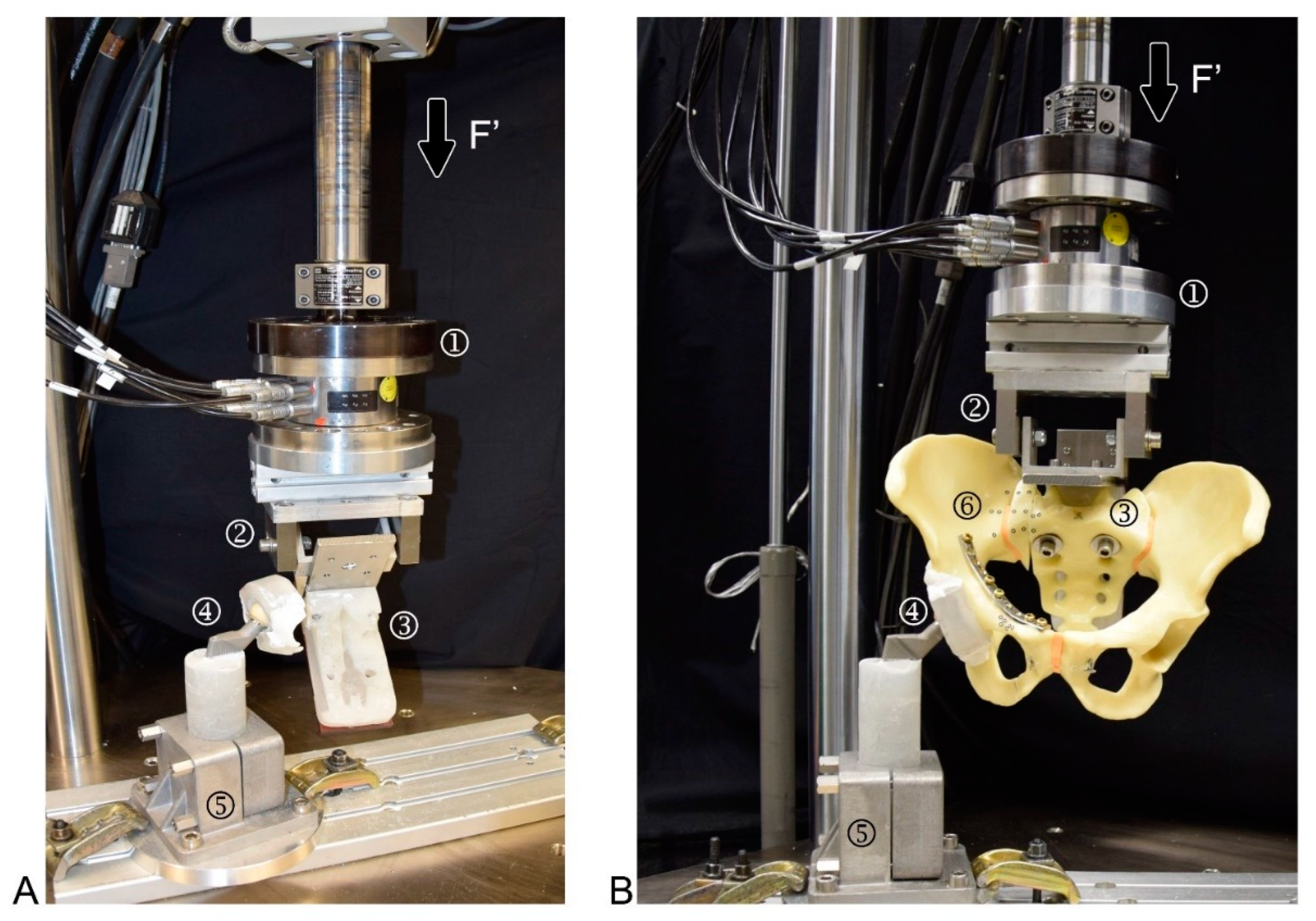
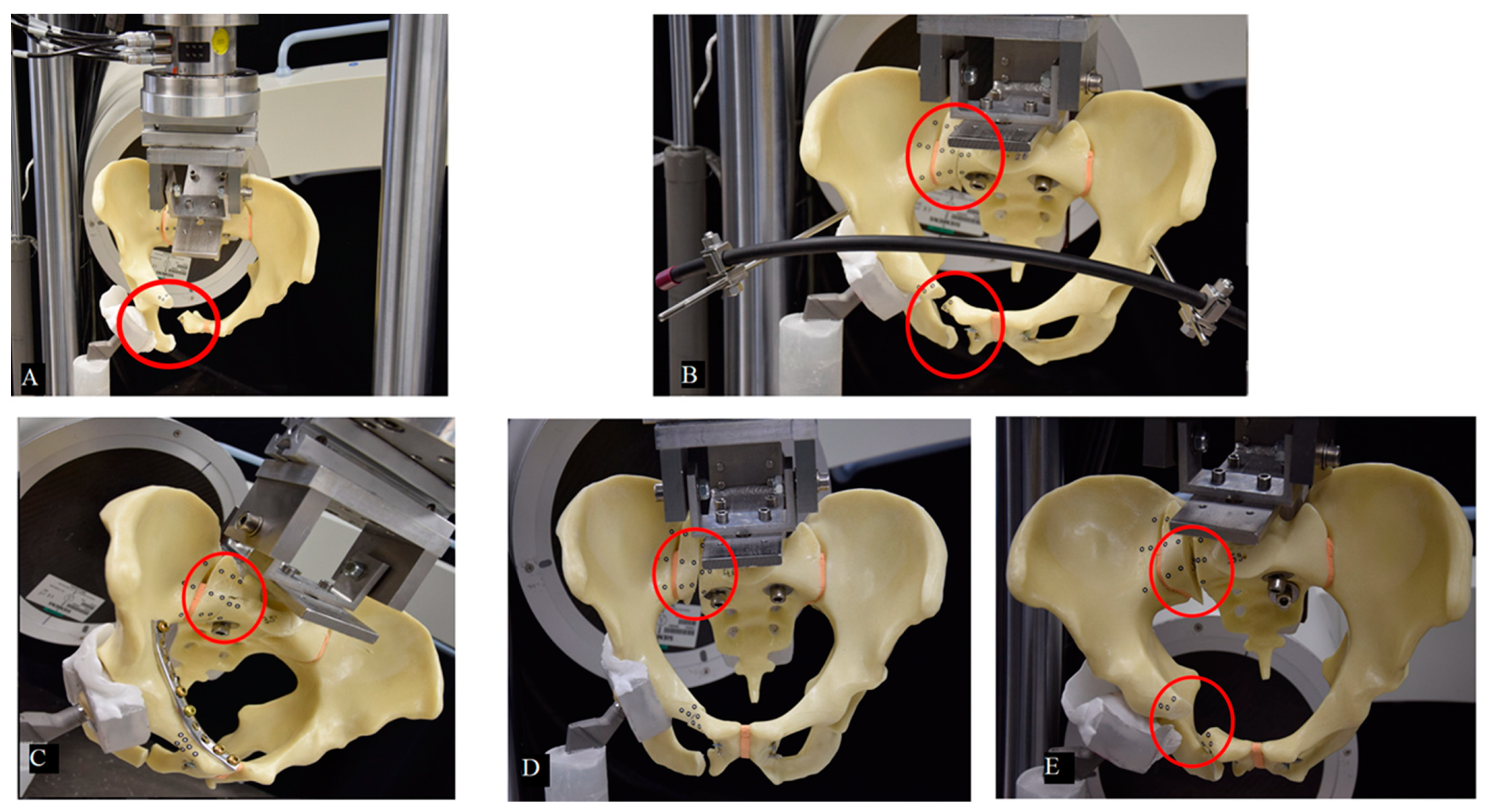
2. Materials and Methods
2.1. Biomechanical Testing
2.2. Data Acquisition and Analysis
3. Results
3.1. Axial Stiffness
3.2. Cycles to Failure
3.3. Fracture Displacement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

| Multiple Comparisons Cycles to Failure | ||||
|---|---|---|---|---|
| Group | Group | Mean | SD | p |
| 1 | 2 | −1023 | 636 | 1.00 |
| 3 | −6792 | 654 | 0.00 | |
| 4 | 7381 | 636 | 0.00 | |
| 5 | −3007 | 636 | 0.00 | |
| 2 | 1 | 102 | 636 | 1.00 |
| 3 | −5768 | 654 | 0.00 | |
| 4 | −6358 | 636 | 0.00 | |
| 5 | −1984 | 636 | 0.03 | |
| 3 | 1 | 6792 | 654 | 0.00 |
| 2 | 5768 | 654 | 0.00 | |
| 4 | −590 | 654 | 0.00 | |
| 5 | 3785 | 654 | 0.00 | |
| 4 | 1 | 7381 | 636 | 0.00 |
| 2 | 6358 | 636 | 0.00 | |
| 3 | 590 | 654 | 1.00 | |
| 5 | 4374 | 636 | 0.00 | |
| 5 | 1 | 3007 | 636 | 0.00 |
| 2 | 1984 | 636 | 0.03 | |
| 3 | −3785 | 654 | 0.00 | |
| 4 | −4374 | 636 | 0.00 | |
| Multiple Comparisons Axial Stiffness [N/mm] | ||||
|---|---|---|---|---|
| Group | Group | Mean | SD | p |
| 1 | 2 | −2.73 | 1.48 | 0.71 |
| 3 | −4.40 | 1.52 | 0.06 | |
| 4 | −5.33 | 1.48 | 0.01 | |
| 5 | −14.97 | 1.48 | 0.00 | |
| 2 | 1 | 2.73 | 1.48 | 0.71 |
| 3 | −1.66 | 1.52 | 1.00 | |
| 4 | −2.60 | 1.48 | 0.86 | |
| 5 | −12.24 | 1.48 | 0.00 | |
| 3 | 1 | 4.39 | 1.52 | 0.06 |
| 2 | 1.66 | 1.52 | 1.00 | |
| 4 | −0.94 | 1.52 | 1.00 | |
| 5 | −10.58 | 1.52 | 0.00 | |
| 4 | 1 | 5.33 | 1.48 | 0.01 |
| 2 | 2.60 | 1.48 | 0.86 | |
| 3 | 0.94 | 1.52 | 1.00 | |
| 5 | −9.65 | 1.48 | 0.00 | |
| 5 | 1 | 14.97 | 1.48 | 0.00 |
| 2 | 12.24 | 1.48 | 0.00 | |
| 3 | 10.58 | 1.52 | 0.00 | |
| 4 | 9.65 | 1.48 | 0.00 | |
| Multiple Comparisons Anterior Displacement | ||
|---|---|---|
| Groups | Displacement [cm] | p |
| 4-3 | 0.08 | 1.00 |
| 4-5 | −0.40 | 1.00 |
| 4-1 | 18.70 | 0.03 |
| 4-2 | 21.50 | 0.01 |
| 3-5 | −0.32 | 1.00 |
| 3-1 | 18.62 | 0.05 |
| 3-2 | 21.42 | 0.01 |
| 5-1 | 18.30 | 0.04 |
| 5-2 | 21.10 | 0.01 |
| 1-2 | −2.80 | 1.00 |
| Multiple Comparisons Posterior Displacement | ||
|---|---|---|
| Groups | Displacement [cm] | p |
| 5-3 | 4.67 | 1.00 |
| 5-4 | 5.00 | 1.00 |
| 5-2 | 21.10 | 0.01 |
| 5-1 | 23.60 | 0.00 |
| 3-4 | −0.33 | 1.00 |
| 3-2 | 16.43 | 0.12 |
| 3-1 | 18.93 | 0.04 |
| 4-2 | 16.10 | 0.12 |
| 4-1 | 18.60 | 0.04 |
| 2-1 | 2.50 | 1.00 |
References
- Tosounidis, G.; Holstein, J.H.; Culemann, U.; Holmenschlager, F.; Stuby, F.; Pohlemann, T. Changes in epidemiology and treatment of pelvic ring fractures in Germany: An analysis on data of German Pelvic Multicenter Study Groups I and III (DGU/AO). Acta Chir. Orthop. Traumatol. Cechoslov. 2010, 77, 450–456. [Google Scholar]
- Buller, L.T.; Best, M.J.; Quinnan, S.M. A nationwide analysis of pelvic ring fractures: Incidence and trends in treatment, length of stay, and mortality. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 9–17. [Google Scholar] [CrossRef]
- Kannus, P.; Palvanen, M.; Niemi, S.; Parkkari, J.; Järvinen, M. Epidemiology of osteoporotic pelvic fractures in elderly people in finland: Sharp increase in 1970–1997 and alarming projections for the new millennium. Osteoporos. Int. 2000, 11, 443–448. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Riesenbeck, O.; Raschke, M.J.; Hartensuer, R. Trends in der operativen Therapie von Frakturen des Beckenrings: Eine bundesweite Analyse von OPS-Daten zwischen 2005 und 2017. Unfallchirurg 2020, 124, 373–381. (In Germany) [Google Scholar] [CrossRef] [PubMed]
- Andrich, S.; Haastert, B.; Neuhaus, E.; Neidert, K.; Arend, W.; Ohmann, C.; Grebe, J.; Vogt, A.; Jungbluth, P.; Thelen, S.; et al. Excess mortality after pelvic fractures among older people. J. Bone Miner. Res. 2017, 32, 1789–1801. [Google Scholar] [CrossRef]
- Rommens, P.M.; Wagner, D.; Hofmann, A. Do we need a separate classification for fragility fractures of the pelvis? J. Orthop. Trauma 2019, 33, S55–S60. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013, 44, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Wagner, D.; Hofmann, A. Minimal invasive surgical treatment of fragility fractures of the pelvis. Chirurgia 2017, 112, 524–537. [Google Scholar] [CrossRef]
- Marecek, G.S.; Scolaro, J.A. Anterior pelvic ring: Introduction to evaluation and management. J. Orthop. Trauma 2018, 32, S1–S3. [Google Scholar] [CrossRef]
- Küper, M.A.; Trulson, A.; Stuby, F.M.; Stöckle, U. Pelvic ring fractures in the elderly. EFORT Open Rev. 2019, 4, 313–320. [Google Scholar] [CrossRef]
- Denis, F.; Davis, S.; Comfort, T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar]
- Hartensuer, R.; Grüneweller, N.; Lodde, M.F.; Evers, J.; Riesenbeck, O.; Raschke, M. Die S2-Ala-Ilium-Schraube in der Beckentraumatologie. Z. Orthop. Unfall. 2020. (In Germany) [Google Scholar] [CrossRef]
- Futamura, K.; Baba, T.; Mogami, A.; Kanda, A.; Obayashi, O.; Iwase, H.; Kaneko, K. “Within ring”-based sacroiliac rod fixation may overcome the weakness of spinopelvic fixation for unstable pelvic ring injuries: Technical notes and clinical outcomes. Int. Orthop. 2018, 42, 1405–1411. [Google Scholar] [CrossRef] [PubMed]
- McLachlin, S.; Lesieur, M.; Stephen, D.; Kreder, H.; Whyne, C. Biomechanical analysis of anterior ring fixation of the ramus in type C pelvis fractures. Eur. J. Trauma Emerg. Surg. 2017, 44, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Grüneweller, N.; Raschke, M.J.; Zderic, I.; Widmer, D.; Wähnert, D.; Gueorguiev, B.; Richards, R.G.; Fuchs, T.; Windolf, M. Biomechanical comparison of augmented versus non-augmented sacroiliac screws in a novel hemi-pelvis test model. J. Orthop. Res. 2016, 35, 1485–1493. [Google Scholar] [CrossRef] [PubMed]
- Shaw, J.A.; Mino, D.E.; Werner, F.W.; Murray, D.G. Posterior stabilization of pelvic fractures by use of threaded compression rods. Case reports and mechanical testing. Clin. Orthop. Relat. Res. 1985, 192, 240–254. [Google Scholar]
- Zderic, I.; Wagner, D.; Schopper, C.; Lodde, M.; Richards, G.; Gueorguiev, B.; Rommens, P.; Acklin, Y.P. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening—Biomechanical evaluation of a new concept. J. Orthop. Res. 2021, 39, 761–770. [Google Scholar] [CrossRef] [PubMed]
- Keating, J.F.; Werier, J.; Blachut, P.; Broekhuyse, H.; Meek, R.N.; O’Brien, P.J. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J. Orthop. Trauma 1999, 13, 107–113. [Google Scholar] [CrossRef]
- Höch, A.; Özkurtul, O.; Pieroh, P.; Josten, C.; Böhme, J. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr. Orthop. Surg. Rehabil. 2017, 8, 3–9. [Google Scholar] [CrossRef]
- Hartensuer, R.; Lodde, M.F.; Keller, J.; Eveslage, M.; Stolberg-Stolberg, J.; Riesenbeck, O.; Raschke, M.J. Safety, effect and feasibility of percutaneous SI-screw with and without augmentation—A 15-year retrospective analysis on over 640 screws. J. Clin. Med. 2020, 9, 2660. [Google Scholar] [CrossRef]
- Rieger, H.; Winckler, S.; Wetterkamp, D.; Overbeck, J. Clinical and biomechanical aspects of external fixation of the pelvis. Clin. Biomech. 1996, 11, 322–327. [Google Scholar] [CrossRef]
- Stocks, G.W.; Gabel, G.T.; Noble, P.C.; Hanson, G.W.; Tullós, H.S. Anterior and posterior internal fixation of vertical shear fractures of the pelvis. J. Orthop. Res. 1991, 9, 237–245. [Google Scholar] [CrossRef]
- Jazini, E.; Klocke, N.; Tannous, O.; Johal, H.S.; Hao, J.; Salloum, K.; Gelb, D.E.; Nascone, J.W.; Belin, E.; Hoshino, C.M.; et al. Does lumbopelvic fixation add stability? A cadaveric biomechanical analysis of an unstable pelvic fracture model. J. Orthop. Trauma 2017, 31, 37–46. [Google Scholar] [CrossRef]
- Simonian, P.T.; Routt, M.L.; Harrington, R.M.; Tencer, A.F. Internal fixation of the unstable anterior pelvic ring: A biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J. Orthop. Trauma 1994, 8, 476–482. [Google Scholar] [CrossRef]
- Cunningham, B.W.; Lewis, S.J.; Long, J.; Dmitriev, A.E.; Linville, D.A.; Bridwell, K.H. Biomechanical evaluation of lumbosacral reconstruction techniques for Spondylolisthesis: An in vitro porcine model. Spine 2002, 27, 2321–2327. [Google Scholar] [CrossRef] [PubMed]
- Gänsslen, A.; Giannoudis, P.; Pape, H.-C. Hemorrhage in pelvic fracture: Who needs angiography? Curr. Opin. Crit. Care 2003, 9, 515–523. [Google Scholar] [CrossRef]
- Grimm, M.R.; Vrahas, M.S.; Thomas, K.A. Pressure-volume characteristics of the intact and disrupted pelvic retroperitoneum. J. Trauma 1998, 44, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Kendoff, D.; Ostermeier, S.; Citak, M.; Hüfner, T.; Krettek, C.; Nork, S.E. Sacroiliac joint compression using an anterior pelvic compressor: A mechanical study in synthetic bone. J. Orthop. Trauma 2007, 21, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Wähnert, D.; Raschke, M.J.; Fuchs, T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum. A new method using modified implants. Int. Orthop. 2013, 37, 1147–1150. [Google Scholar] [CrossRef] [PubMed]
- Weatherby, D.J.; Routt, M.L.C.; Eastman, J.G. The retrograde-antegrade-retrograde technique for successful placement of a retrograde superior ramus screw. J. Orthop. Trauma 2017, 31, e224–e229. [Google Scholar] [CrossRef]
- Mosheiff, R.; Liebergall, M. Maneuvering the retrograde medullary screw in pubic ramus fractures. J. Orthop. Trauma 2002, 16, 594–596. [Google Scholar] [CrossRef]
- Rommens, P.M.; Graafen, M.; Arand, C.; Mehling, I.; Hofmann, A.; Wagner, D. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury 2020, 51, 340–346. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, F.; Condon, F.; McGloughlin, T.; Lenehan, B.; Coffey, C.; Walsh, M. Validity of synthetic bone as a substitute for osteoporotic cadaveric femoral heads in mechanical testing: A biomechanical study. Bone Jt. Res. 2012, 1, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Elfar, J.; Menorca, R.M.G.; Reed, J.D.; Stanbury, S. Composite bone models in orthopaedic surgery research and education. J. Am. Acad. Orthop. Surg. 2014, 22, 111–120. [Google Scholar] [CrossRef]
- Wähnert, D.; Hoffmeier, K.L.; Klos, K.; Stolarczyk, Y.; Fröber, R.; Hofmann, G.O.; Mückley, T. Biomechanical characterization of an osteoporotic artificial bone model for the distal femur. J. Biomater. Appl. 2010, 26, 565–579. [Google Scholar] [CrossRef]
- Gänsslen, A.; Pohlemann, T.; Krettek, C. Der einfache supraazetabuläre Fixateur externe für die Behandlung von Beckenfrakturen. Oper. Orthop. Traumatol. 2005, 17, 296–312. (In Germany) [Google Scholar] [CrossRef] [PubMed]

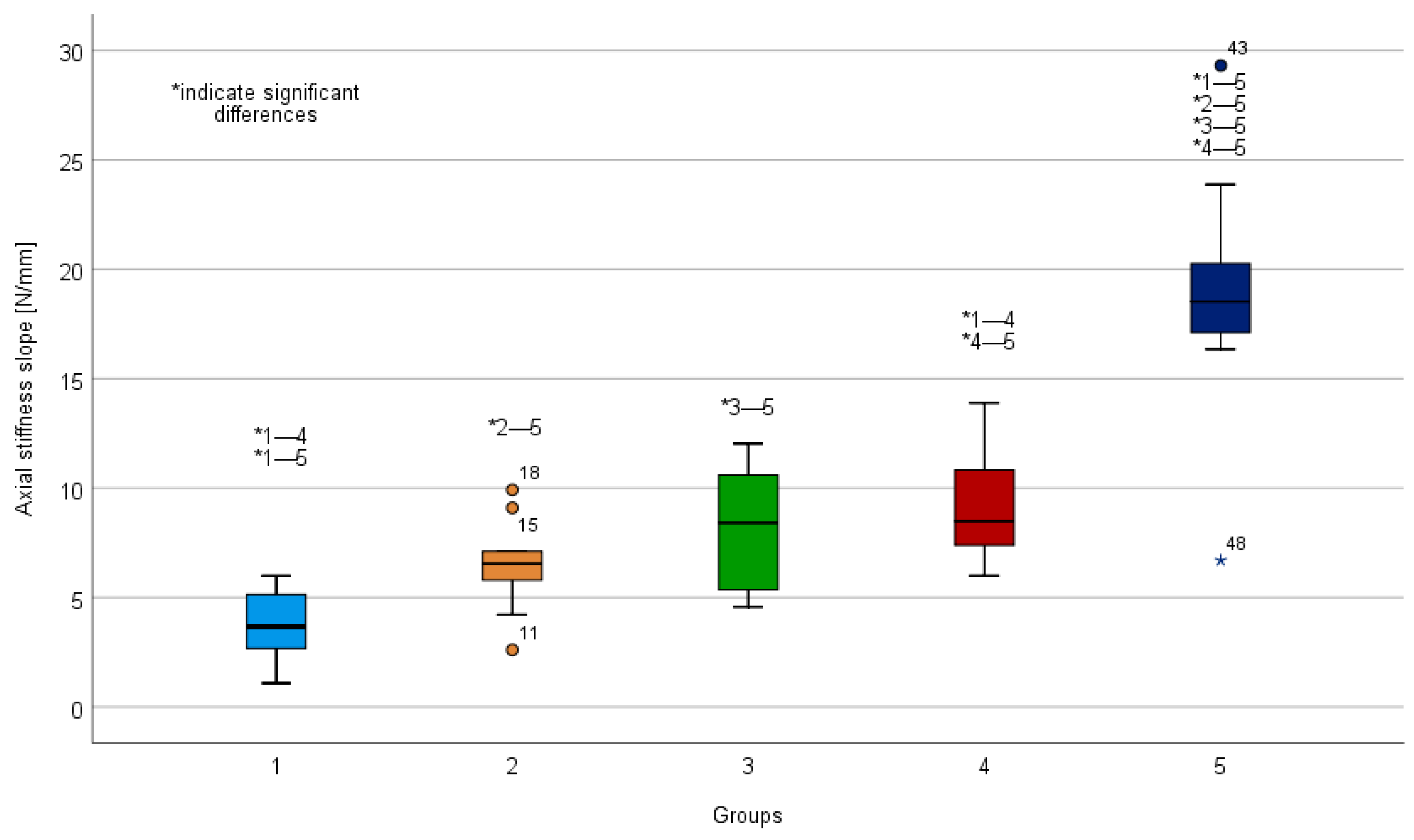
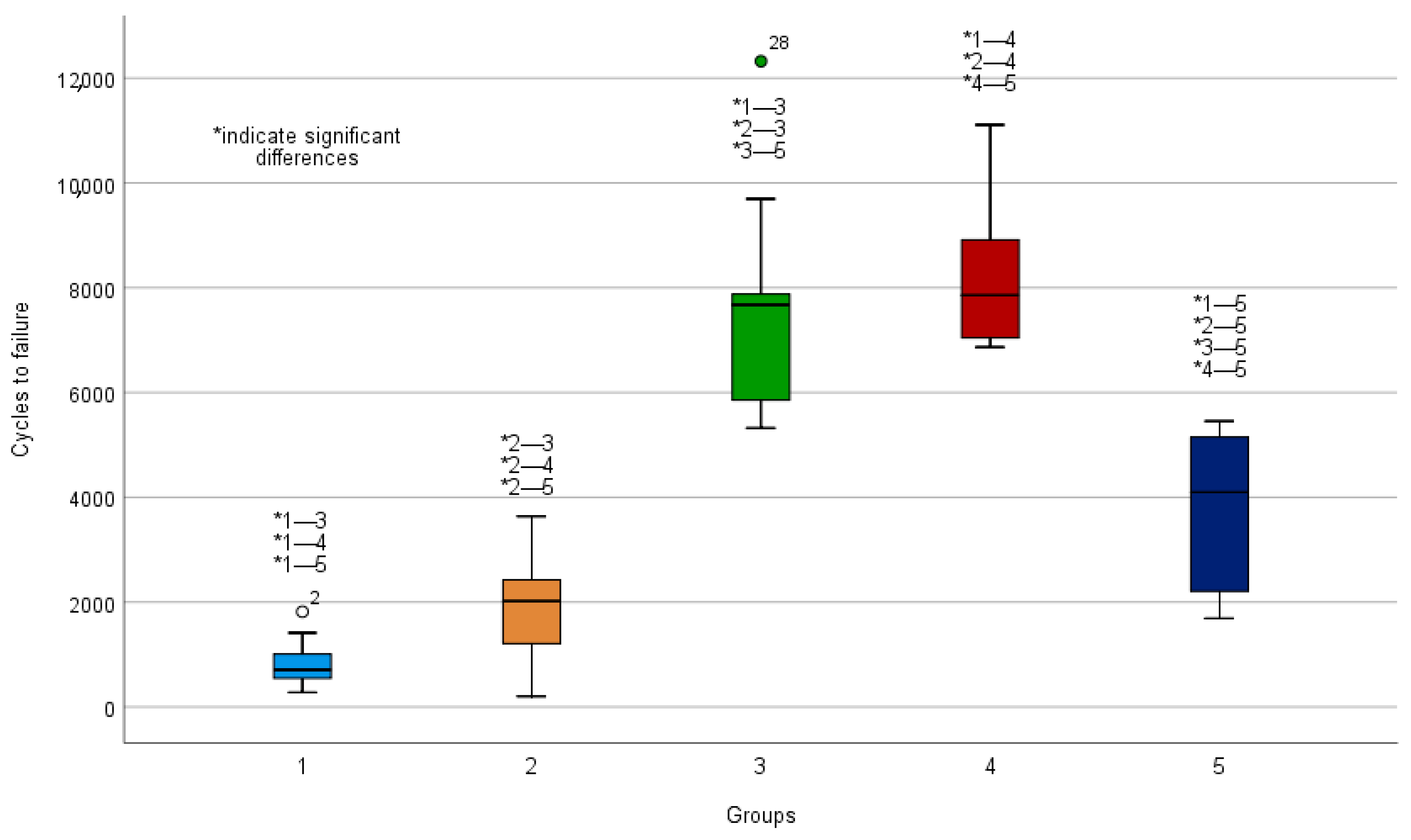
| Groups 1–5 | Initial Axial Stiffness [N/mm] | Cycles to Failure |
|---|---|---|
| SI screw (1); mean (SD) | 3.79 (1.60) | 856 (470) |
| SI screw plus supra-acetabular external fixator (2); mean (SD) | 6.52 (2.11) | 1879 (1027) |
| SI screw plus plate fixation (3); mean (SD) | 8.18 (2.81) | 7647 (2248) |
| SI screw plus a retrograde transpubic screw (4); mean (SD) | 9.10 (2.44) | 8237 (1399) |
| S1/S2 ala–ilium screw fixation (5); mean (SD) | 18.76 (5.77) | 3863 (1476) |
| Groups 1–5 | Anterior Displacement at 500 Cycles [cm] | Posterior Displacement at 500 Cycles [cm] |
|---|---|---|
| SI screw (1); median (IQR) | 5.74 (1.43–8.14) | 0.41 (0.16–0.67) |
| SI screw plus supra-acetabular external fixator (2); median (IQR) | 4.33 (2.42–6.27) | 0.30 (0.16–0.43) |
| SI screw plus plate fixation (3); median (IQR) | 0.01 (0.00–0.02) | 0.00 (0.00–0.11) |
| SI screw plus a retrograde transpubic screw (4); median (IQR) | 0.01 (0.00–0.01) | 0.00 (0.00–0.04) |
| S1/S2 ala–ilium screw fixation (5); median (IQR) | 0.00 (0.00–0.15) | 0.00 (0.00–0.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. J. Clin. Med. 2021, 10, 2326. https://doi.org/10.3390/jcm10112326
Lodde MF, Katthagen JC, Schopper CO, Zderic I, Richards G, Gueorguiev B, Raschke MJ, Hartensuer R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. Journal of Clinical Medicine. 2021; 10(11):2326. https://doi.org/10.3390/jcm10112326
Chicago/Turabian StyleLodde, Moritz F., J. Christoph Katthagen, Clemens O. Schopper, Ivan Zderic, Geoff Richards, Boyko Gueorguiev, Michael J. Raschke, and René Hartensuer. 2021. "Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring" Journal of Clinical Medicine 10, no. 11: 2326. https://doi.org/10.3390/jcm10112326
APA StyleLodde, M. F., Katthagen, J. C., Schopper, C. O., Zderic, I., Richards, G., Gueorguiev, B., Raschke, M. J., & Hartensuer, R. (2021). Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. Journal of Clinical Medicine, 10(11), 2326. https://doi.org/10.3390/jcm10112326









