The Underestimated Prevalence of Neglected Chronic Pelvic Pain in Women, a Nationwide Cross-Sectional Study in France
Abstract
:1. Introduction
2. Material and Methods
2.1. Design of the CONSTANCES Cohort Project
2.2. Study Design
2.3. Statistical Analysis
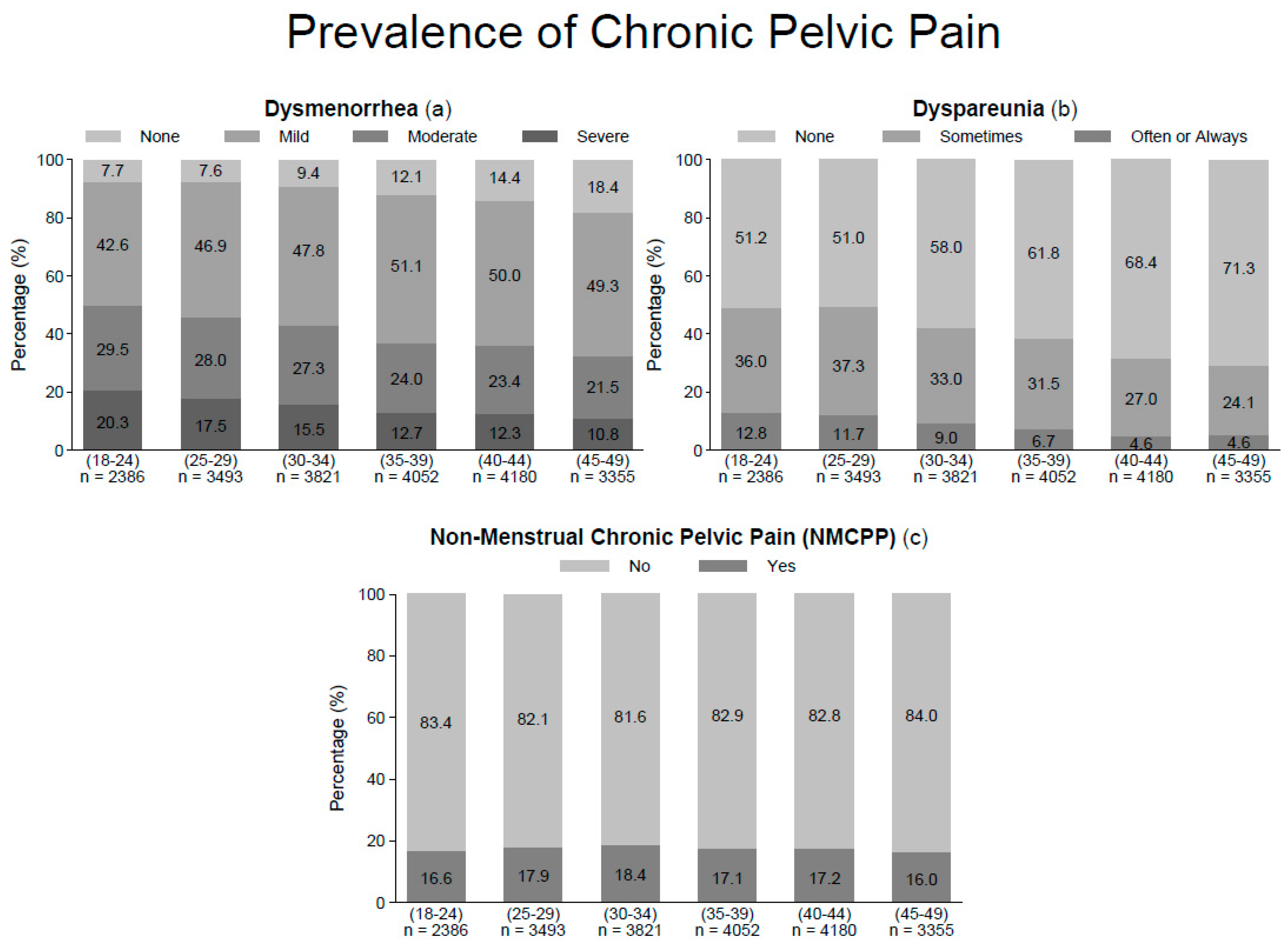
3. Results
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Interpretation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Zondervan, K.T.; Yudkin, P.L.; Vessey, M.P.; Dawes, M.G.; Barlow, D.H.; Kennedy, S.H. Prevalence and Incidence of Chronic Pelvic Pain in Primary Care: Evidence from a National General Practice Database. Br. J. Obstet. Gynaecol. 1999, 106, 1149–1155. [Google Scholar] [CrossRef]
- Mathias, S.D.; Kuppermann, M.; Liberman, R.F.; Lipschutz, R.C.; Steege, J.F. Chronic Pelvic Pain: Prevalence, Health-Related Quality of Life, and Economic Correlates. Obstet. Gynecol. 1996, 87, 321–327. [Google Scholar] [CrossRef]
- Jamieson, D.J.; Steege, J.F. The Prevalence of Dysmenorrhea, Dyspareunia, Pelvic Pain, and Irritable Bowel Syndrome in Primary Care Practices. Obstet. Gynecol. 1996, 87, 55–58. [Google Scholar] [CrossRef]
- Fauconnier, A.; Dubuisson, J.-B.; Foulot, H.; Deyrolles, C.; Sarrot, F.; Laveyssière, M.-N.; Jansé-Marec, J.; Bréart, G. Mobile Uterine Retroversion Is Associated with Dyspareunia and Dysmenorrhea in an Unselected Population of Women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 127, 252–256. [Google Scholar] [CrossRef]
- Wong, L.P. Attitudes towards Dysmenorrhoea, Impact and Treatment Seeking among Adolescent Girls: A Rural School-Based Survey. Aust. J. Rural Health 2011, 19, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Kapadi, R.; Elander, J. Pain Coping, Pain Acceptance and Analgesic Use as Predictors of Health-Related Quality of Life among Women with Primary Dysmenorrhea. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 246, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Sobhgol, S.S.; Alizadeli Charndabee, S.M. Rate and Related Factors of Dyspareunia in Reproductive Age Women: A Cross-Sectional Study. Int. J. Impot. Res. 2007, 19, 88–94. [Google Scholar] [CrossRef] [Green Version]
- Thomtén, J. Living with Genital Pain: Sexual Function, Satisfaction, and Help-Seeking among Women Living in Sweden. Scand. J. Pain 2014, 5, 19–25. [Google Scholar] [CrossRef]
- Righarts, A.; Osborne, L.; Connor, J.; Gillett, W. The Prevalence and Potential Determinants of Dysmenorrhoea and Other Pelvic Pain in Women: A Prospective Study. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 1532–1539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pitts, M.K.; Ferris, J.A.; Smith, A.M.A.; Shelley, J.M.; Richters, J. Prevalence and Correlates of Three Types of Pelvic Pain in a Nationally Representative Sample of Australian Women. Med. J. Aust. 2008, 189, 138–143. [Google Scholar] [CrossRef]
- Zondervan, K.T.; Yudkin, P.L.; Vessey, M.P.; Jenkinson, C.P.; Dawes, M.G.; Barlow, D.H.; Kennedy, S.H. The Community Prevalence of Chronic Pelvic Pain in Women and Associated Illness Behaviour. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2001, 51, 541–547. [Google Scholar]
- Mackenbach, J.P.; Stirbu, I.; Roskam, A.-J.R.; Schaap, M.M.; Menvielle, G.; Leinsalu, M.; Kunst, A.E.; European Union Working Group on Socioeconomic Inequalities in Health. Socioeconomic Inequalities in Health in 22 European Countries. N. Engl. J. Med. 2008, 358, 2468–2481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zins, M.; Goldberg, M.; CONSTANCES Team. The French CONSTANCES Population-Based Cohort: Design, Inclusion and Follow-Up. Eur. J. Epidemiol. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldberg, M.; Carton, M.; Descatha, A.; Leclerc, A.; Roquelaure, Y.; Santin, G.; Zins, M.; CONSTANCES Team. CONSTANCES: A General Prospective Population-Based Cohort for Occupational and Environmental Epidemiology: Cohort Profile. Occup. Environ. Med. 2017, 74, 66–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zins, M.; Bonenfant, S.; Carton, M.; Coeuret-Pellicer, M.; Guéguen, A.; Gourmelen, J.; Nachtigal, M.; Ozguler, A.; Quesnot, A.; Ribet, C.; et al. The CONSTANCES Cohort: An Open Epidemiological Laboratory. BMC Public Health 2010, 10, 479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santin, G.; Geoffroy, B.; Bénézet, L.; Delézire, P.; Chatelot, J.; Sitta, R.; Bouyer, J.; Gueguen, A.; SNIIR-AM Cohorts Group. In an Occupational Health Surveillance Study, Auxiliary Data from Administrative Health and Occupational Databases Effectively Corrected for Nonresponse. J. Clin. Epidemiol. 2014, 67, 722–730. [Google Scholar] [CrossRef]
- Chapron, C.; Fauconnier, A.; Dubuisson, J.-B.; Barakat, H.; Vieira, M.; Bréart, G. Deep Infiltrating Endometriosis: Relation between Severity of Dysmenorrhoea and Extent of Disease. Hum. Reprod. Oxf. Engl. 2003, 18, 760–766. [Google Scholar] [CrossRef] [Green Version]
- Chapron, C.; Barakat, H.; Fritel, X.; Dubuisson, J.-B.; Bréart, G.; Fauconnier, A. Presurgical Diagnosis of Posterior Deep Infiltrating Endometriosis Based on a Standardized Questionnaire. Hum. Reprod. Oxf. Engl. 2005, 20, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Bourdel, N.; Alves, J.; Pickering, G.; Ramilo, I.; Roman, H.; Canis, M. Systematic Review of Endometriosis Pain Assessment: How to Choose a Scale? Hum. Reprod. Update 2015, 21, 136–152. [Google Scholar] [CrossRef]
- Vincent, K.; Kennedy, S.; Stratton, P. Pain Scoring in Endometriosis: Entry Criteria and Outcome Measures for Clinical Trials. Report from the Art and Science of Endometriosis Meeting. Fertil. Steril. 2010, 93, 62–67. [Google Scholar] [CrossRef] [Green Version]
- Dworkin, R.H.; Turk, D.C.; Wyrwich, K.W.; Beaton, D.; Cleeland, C.S.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Kerns, R.D.; Ader, D.N.; et al. Interpreting the Clinical Importance of Treatment Outcomes in Chronic Pain Clinical Trials: IMMPACT Recommendations. J. Pain 2008, 9, 105–121. [Google Scholar] [CrossRef] [PubMed]
- Santin, G.; Bénézet, L.; Geoffroy-Perez, B.; Bouyer, J.; Guéguen, A. A Two-Phase Sampling Survey for Nonresponse and Its Paradata to Correct Nonresponse Bias in a Health Surveillance Survey. Rev. Epidemiol. Sante Publique 2017, 65, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Grace, V.M.; Zondervan, K.T. Chronic Pelvic Pain in New Zealand: Prevalence, Pain Severity, Diagnoses and Use of the Health Services. Aust. N. Z. J. Public Health 2004, 28, 369–375. [Google Scholar] [CrossRef] [Green Version]
- Loving, S.; Thomsen, T.; Jaszczak, P.; Nordling, J. Female Chronic Pelvic Pain Is Highly Prevalent in Denmark. A Cross-Sectional Population-Based Study with Randomly Selected Participants. Scand. J. Pain 2014, 5, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Ayorinde, A.A.; Bhattacharya, S.; Druce, K.L.; Jones, G.T.; Macfarlane, G.J. Chronic Pelvic Pain in Women of Reproductive and Post-Reproductive Age: A Population-Based Study. Eur. J. Pain Lond. Engl. 2017, 21, 445–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ju, H.; Jones, M.; Mishra, G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiol. Rev. 2014, 36, 104–113. [Google Scholar] [CrossRef] [Green Version]
- van Aken, M.; Oosterman, J.; van Rijn, T.; Woudsma, K.; Ferdek, M.; Ruigt, G.; Kozicz, T.; Braat, D.; Peeters, A.; Nap, A. Experimental Pain Tolerance Is Decreased and Independent of Clinical Pain Intensity in Patients with Endometriosis. Fertil. Steril. 2018, 110, 1118–1128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberico, D.; Somigliana, E.; Bracco, B.; Dhouha, D.; Roberto, A.; Mosconi, P.; Facchin, F.; Vercellini, P. Potential Benefits of Pregnancy on Endometriosis Symptoms. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 230, 182–187. [Google Scholar] [CrossRef]
- Collinet, P.; Fritel, X.; Revel-Delhom, C.; Ballester, M.; Bolze, P.A.; Borghese, B.; Bornsztein, N.; Boujenah, J.; Brillac, T.; Chabbert-Buffet, N.; et al. Management of Endometriosis: CNGOF/HAS Clinical Practice Guidelines—Short Version. J. Gynecol. Obstet. Hum. Reprod. 2018, 47, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Dunselman, G.A.J.; Vermeulen, N.; Becker, C.; Calhaz-Jorge, C.; D’Hooghe, T.; De Bie, B.; Heikinheimo, O.; Horne, A.W.; Kiesel, L.; Nap, A.; et al. ESHRE Guideline: Management of Women with Endometriosis. Hum. Reprod. 2014, 29, 400–412. [Google Scholar] [CrossRef]
- Fauconnier, A.; Staraci, S.; Huchon, C.; Roman, H.; Panel, P.; Descamps, P. Comparison of Patient- and Physician-Based Descriptions of Symptoms of Endometriosis: A Qualitative Study. Hum. Reprod. Oxf. Engl. 2013, 28, 2686–2694. [Google Scholar] [CrossRef] [Green Version]
- Vercellini, P.; Fedele, L.; Aimi, G.; Pietropaolo, G.; Consonni, D.; Crosignani, P.G. Association between Endometriosis Stage, Lesion Type, Patient Characteristics and Severity of Pelvic Pain Symptoms: A Multivariate Analysis of over 1000 Patients. Hum. Reprod. Oxf. Engl. 2007, 22, 266–271. [Google Scholar] [CrossRef]
- Sinaii, N.; Plumb, K.; Cotton, L.; Lambert, A.; Kennedy, S.; Zondervan, K.; Stratton, P. Differences in Characteristics among 1,000 Women with Endometriosis Based on Extent of Disease. Fertil. Steril. 2008, 89, 538–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armour, M.; Parry, K.; Manohar, N.; Holmes, K.; Ferfolja, T.; Curry, C.; MacMillan, F.; Smith, C.A. The Prevalence and Academic Impact of Dysmenorrhea in 21,573 Young Women: A Systematic Review and Meta-Analysis. J. Womens Health 2002 2019, 28, 1161–1171. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Parry, K.; Al-Dabbas, M.A.; Curry, C.; Holmes, K.; MacMillan, F.; Ferfolja, T.; Smith, C.A. Self-Care Strategies and Sources of Knowledge on Menstruation in 12,526 Young Women with Dysmenorrhea: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0220103. [Google Scholar] [CrossRef] [PubMed]

| Age of Participants Number of Participants (Range, y) | (18–24) n = 2386 n (%) | (25–29) n = 3493 n (%) | (30–34) n = 3821 n (%) | (35–39) n = 4052 n (%) | (40–44) n = 4180 n (%) | (45–49) n = 3355 n (%) | Total n = 21,287 n (%) |
|---|---|---|---|---|---|---|---|
| Body Mass Index (BMI), (kg/m²) | |||||||
| BMI < 18.5 (n = 1133) | 223 (9.5) | 198 (5.8) | 235 (6.3) | 223 (5.7) | 155 (3.8) | 99 (3.0) | 1133(5.5) |
| 18.5 < BMI < 25 (n = 14,039) | 1686 (72.2) | 2448 (72.0) | 2586 (69.7) | 2622 (66.6) | 2628 (64.6) | 2069 (63.3) | 14,039 (67.8) |
| 25 < BMI < 30 (n = 3778) | 311 (13.3) | 510 (15.0) | 633 (17.1) | 728 (18.5) | 844 (20.8) | 752 (23.0) | 3778 (18.2) |
| 30 < BMI < 35 (n = 1205) | 84 (3.6) | 162 (4.8) | 187 (5.0) | 230 (5.8) | 298 (7.3) | 244 (7.5) | 1205 (5.8) |
| 35 < BMI < 40 (n = 408) | 25 (1.1) | 60 (1.8) | 50 (1.3) | 92 (2.3) | 102 (2.5) | 79 (2.4) | 408 (2.0) |
| BMI > 40 (n = 153) | 7 (0.3) | 21 (0.6) | 21 (0.6) | 41 (1.0) | 38 (0.9) | 25 (0.8) | 153 (0.7) |
| Smoking status | |||||||
| Never smoker (n = 10,312) | 1313 (56.4) | 1846 (54.4) | 1701 (46.0) | 1936 (49.3) | 2020 (50.1) | 1496 (46.3) | 10,312 (50.1) |
| Former smoker (n = 5226) | 262 (11.3) | 573 (16.9) | 952 (25.8) | 1123 (28.6) | 1181 (29.3) | 1135 (35.2) | 5226 (25.4) |
| Smoker (n = 5062) | 752 (32.3) | 976 (28.7) | 1042 (28.2) | 866 (22.1) | 828 (20.6) | 598 (18.5) | 5062 (24.6) |
| Employment status | |||||||
| Not working (n = 3624) | 1280 (54.7) | 618 (18.0) | 488 (13.0) | 480 (12.1) | 435 (10.6) | 323 (9.8) | 3624 (17.3) |
| Working (n = 17,311) | 1060 (45.3) | 2817 (82.0) | 3272 (87.0) | 3499 (87.9) | 3685 (89.4) | 2978 (90.2) | 17311(82.7) |
| Geographic origin | |||||||
| Mainland France (n = 18,915) | 2190 (92.2) | 3151 (90.6) | 3357 (88.2) | 3511 (87.0) | 3709 (89.1) | 2997 (89.7) | 18,915 (89.2) |
| French overseas territories (n = 252) | 49 (2.1) | 52 (1.5) | 51 (1.3) | 44 (1.1) | 32 (0.8) | 24 (0.7) | 252 (1.2) |
| Europe (n = 909) | 58 (2.4) | 112 (3.2) | 173 (4.5) | 200 (5.0) | 197 (4.7) | 169 (5.1) | 909 (4.3) |
| Africa (n = 588) | 43 (1.8) | 96 (2.8) | 109 (2.9) | 141 (3.5) | 126 (3.0) | 73 (2.2) | 588 (2.8) |
| Asia (n = 250) | 18 (0.8) | 30 (0.9) | 53 (1.4) | 69 (1.7) | 49 (1.2) | 31 (0.9) | 250 (1.2) |
| Other (n = 286) | 18 (0.8) | 36 (1.0) | 65 (1.7) | 70 (1.7) | 50 (1.2) | 47 (1.4) | 286 (1.3) |
| Duration of periods (days) | |||||||
| (0–4) (n = 9146) | 2088 (88.7) | 3042 (88.1) | 3290 (87.0) | 3508 (87.8) | 3589 (86.7) | 2552 (77.2) | 9146 (43.2) |
| (5–15) (n = 12,014) | 265 (11.3) | 411 (11.9) | 491 (13.0) | 488 (12.2) | 551 (13.3) | 755 (22.8) | 12,014 (56.8) |
| Parity | |||||||
| P0 (n = 8958) | 2252 (98.0) | 2813 (82.7) | 1788 (47.8) | 936 (23.8) | 695 (17.1) | 474 (14.7) | 8958 (43.3) |
| P1 (n = 3309) | 41 (1.8) | 376 (11.0) | 852 (22.8) | 724 (18.4) | 750 (18.4) | 566 (17.5) | 3309 (16.0) |
| P2 (n = 5816) | 4 (0.2) | 179 (5.3) | 895 (23.9) | 1667 (42.4) | 1743 (42.9) | 1328 (41.1) | 5816 (28.1) |
| P3+ (n = 2594) | 0 (0.0) | 35 (1.0) | 204 (5.5) | 609 (15.5) | 879 (21.6) | 867 (26.8) | 2594 (12.5) |
| Contraception method | |||||||
| None (n = 5395) | 280 (12.2) | 702 (20.7) | 988 (26.5) | 1050 (26.6) | 1274 (31.9) | 1101 (34.6) | 5395 (26.3) |
| Mechanic (condom, cup) (n = 3425) | 324 (14.1) | 532 (15.7) | 703 (18.9) | 736 (18.6) | 638 (16.0) | 492 (15.5) | 3425 (16.7) |
| Sterilization (n = 471) | 0 (0.0) | 1 (0.0) | 5 (0.1) | 48 (1.2) | 193 (4.8) | 224 (7.0) | 471 (2.3) |
| Copper intrauterine device (n = 3246) | 122 (5.3) | 362 (10.7) | 595 (16.0) | 849 (21.5) | 737 (18.5) | 581 (18.3) | 3246 (15.8) |
| Hormonal intrauterine device (n = 1169) | 18 (0.8) | 56 (1.7) | 157 (4.2) | 306 (7.8) | 338 (8.5) | 294 (9.3) | 1169 (5.7) |
| Hormonal (pills, implant...) (n = 6816) | 1550 (67.6) | 1737 (51.2) | 1276 (34.3) | 958 (24.3) | 809 (20.3) | 486 (15.3) | 6816 (33.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Margueritte, F.; Fritel, X.; Zins, M.; Goldberg, M.; Panjo, H.; Fauconnier, A.; Ringa, V. The Underestimated Prevalence of Neglected Chronic Pelvic Pain in Women, a Nationwide Cross-Sectional Study in France. J. Clin. Med. 2021, 10, 2481. https://doi.org/10.3390/jcm10112481
Margueritte F, Fritel X, Zins M, Goldberg M, Panjo H, Fauconnier A, Ringa V. The Underestimated Prevalence of Neglected Chronic Pelvic Pain in Women, a Nationwide Cross-Sectional Study in France. Journal of Clinical Medicine. 2021; 10(11):2481. https://doi.org/10.3390/jcm10112481
Chicago/Turabian StyleMargueritte, François, Xavier Fritel, Marie Zins, Marcel Goldberg, Henri Panjo, Arnaud Fauconnier, and Virginie Ringa. 2021. "The Underestimated Prevalence of Neglected Chronic Pelvic Pain in Women, a Nationwide Cross-Sectional Study in France" Journal of Clinical Medicine 10, no. 11: 2481. https://doi.org/10.3390/jcm10112481
APA StyleMargueritte, F., Fritel, X., Zins, M., Goldberg, M., Panjo, H., Fauconnier, A., & Ringa, V. (2021). The Underestimated Prevalence of Neglected Chronic Pelvic Pain in Women, a Nationwide Cross-Sectional Study in France. Journal of Clinical Medicine, 10(11), 2481. https://doi.org/10.3390/jcm10112481






