Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia
Abstract
1. Introduction
2. Methods
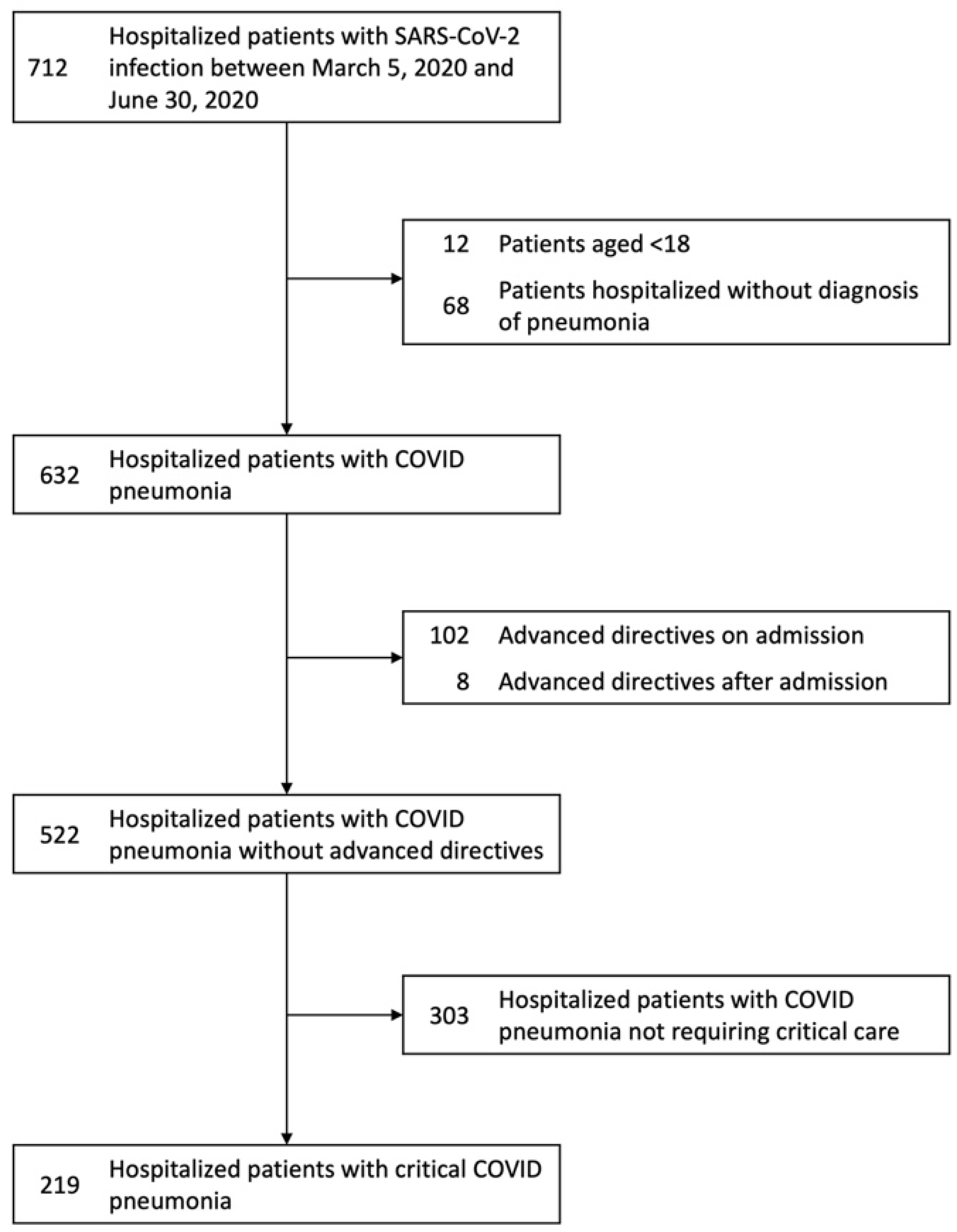
2.1. Study Design, Subjects, and Setting
2.2. Severity of Illness Definitions
2.3. Mortality Prediction
2.4. Exclusion Criteria
2.5. Predictor Variables
2.6. Outcome Variables
2.7. Statistical Analysis
3. Results
3.1. Study Population and Main Characteristics
3.2. Severity of Illness and Outcomes
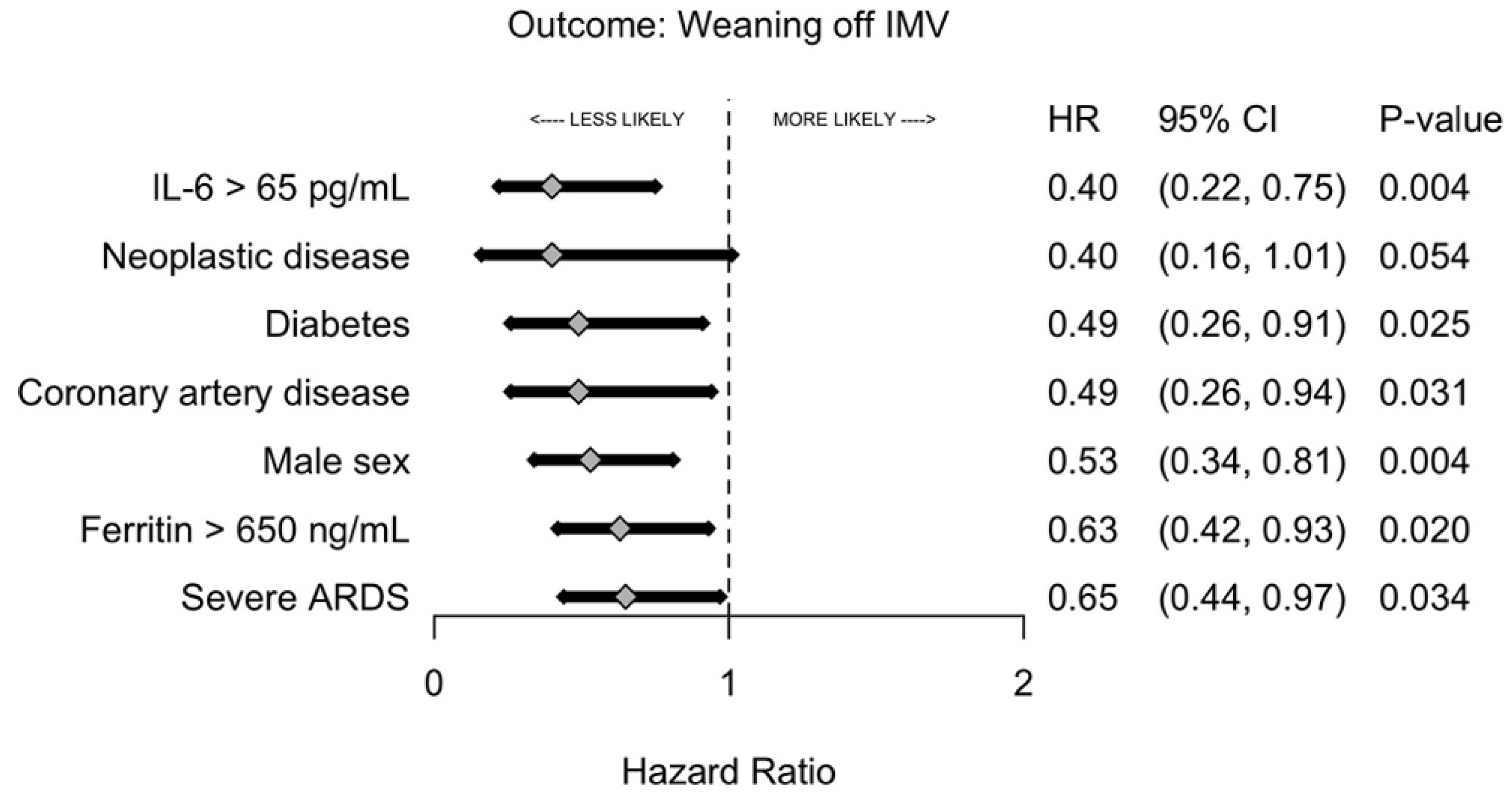
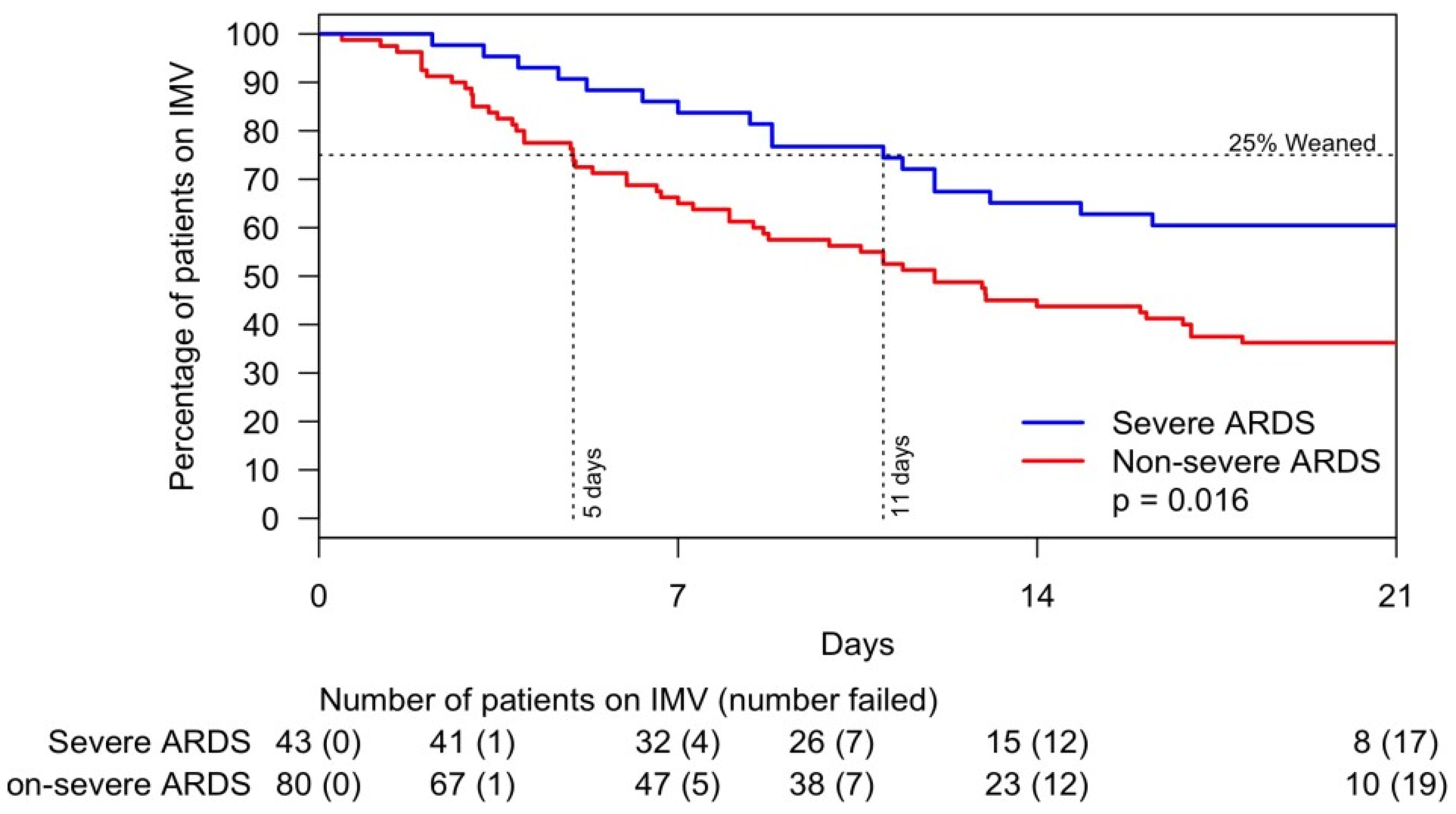
3.3. Weaning Off Invasive Mechanical Ventilation
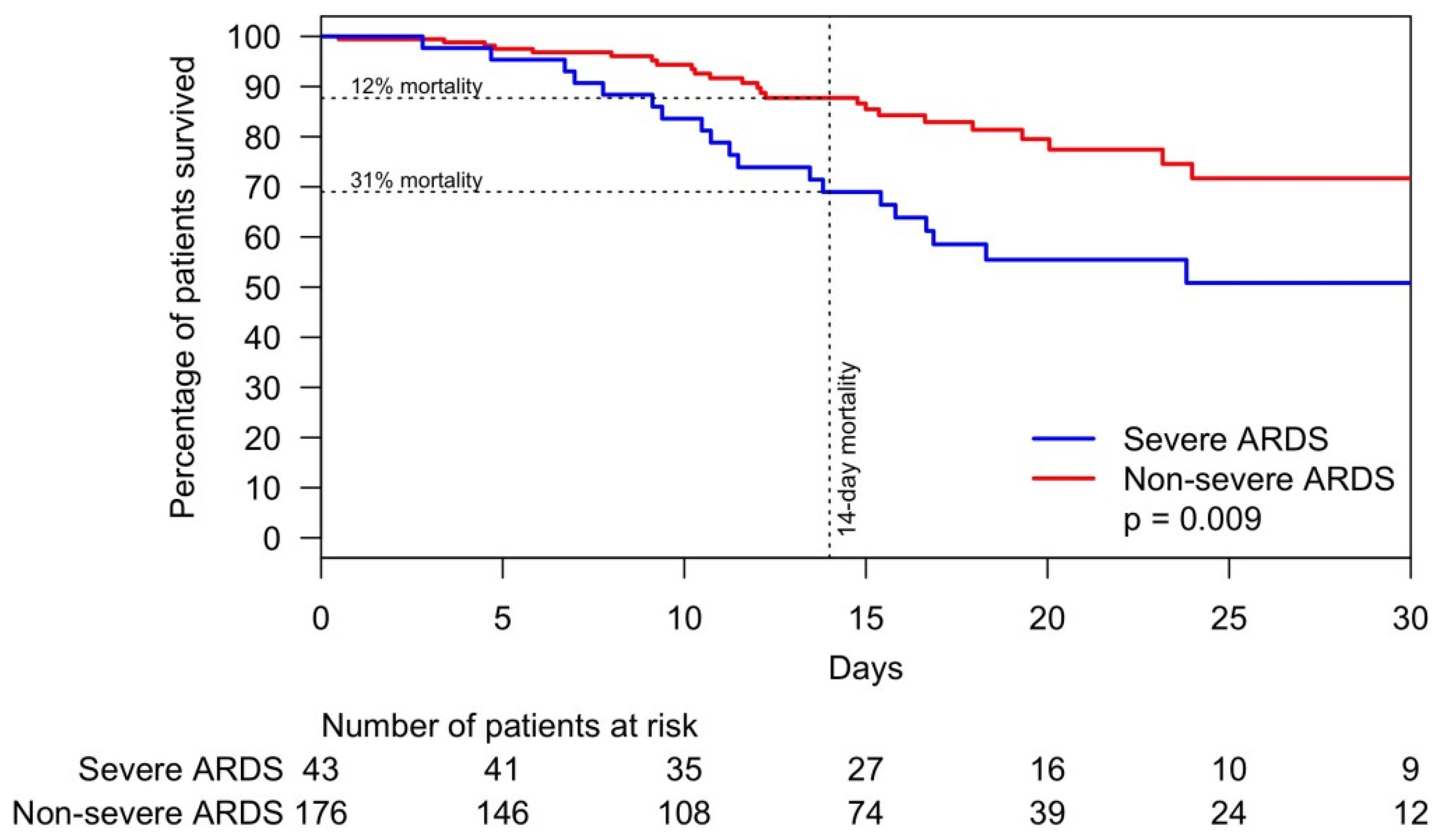
3.4. Mortality
4. Discussion
4.1. Patients Characteristics
4.2. ARDS and the Time to Wean Off IMV of Patients with Critical COVID-19 Pneumonia
4.3. Mortality among COVID-19 Pneumonia
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu (accessed on 22 June 2021).
- Suleyman, G.; Fadel, R.A.; Malette, K.M.; Hammond, C.; Abdulla, H.; Entz, A.; Demertzis, Z.; Hanna, Z.; Failla, A.; Dagher, C.; et al. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit. JAMA Netw. Open 2020, 3, e2012270. [Google Scholar] [CrossRef] [PubMed]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef] [PubMed]
- Furmanek, S.P.; Glick, C.; Chandler, T.; Tella, M.A.; Mattingly, W.A.; Ramirez, J.A.; Wiemken, T.L. The city of Louisville encapsulates the United States demographics. Univ. Louisville J. Respir. Infect. 2020, 4, Article 4. [Google Scholar] [CrossRef]
- United States Census Bureau: QuickFacts. Available online: https://www.census.gov/quickfacts/fact/table/jeffersoncountykentucky%2CUS/PST045219 (accessed on 22 June 2021).
- Bordon, J.; Cavallazzi, R.; Furmanek, S.; Aboelnasr, A.; Tella, M.; Mattingly, W.; Wilde, A.; Sangroula, D.; Antimisiaris, D.; Chung, D.; et al. Characteristics and outcomes of adults hospitalized with SARS-CoV-2 community-acquired pneumonia in Louisville, Kentucky. Univ. Louisville J. Respir. Infect. 2020, 4, 72. [Google Scholar] [CrossRef]
- COVID-19 Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov/overview/clinical-presentation/ (accessed on 1 December 2020).
- Satici, C.; Demirkol, M.A.; Sargin Altunok, E.; Gursoy, B.; Alkan, M.; Kamat, S.; Demirok, B.; Surmeli, C.D.; Calik, M.; Cavus, Z.; et al. Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. Int. J. Infect. Dis. 2020, 98, 84–89. [Google Scholar] [CrossRef]
- Guo, J.; Zhou, B.; Zhu, M.; Yuan, Y.; Wang, Q.; Zhou, H.; Wang, X.; Lv, T.; Li, S.; Liu, P.; et al. CURB-65 may serve as a useful prognostic marker in COVID-19 patients within Wuhan, China: A retrospective cohort study. Epidemiol. Infect. 2020, 148, e241. [Google Scholar] [CrossRef] [PubMed]
- Garibaldi, B.T.; Fiksel, J.; Muschelli, J.; Robinson, M.L.; Rouhizadeh, M.; Perin, J.; Schumock, G.; Nagy, P.; Gray, J.H.; Malapati, H.; et al. Patient Trajectories Among Persons Hospitalized for COVID-19: A Cohort Study. Ann. Intern. Med. 2021, 174, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef]
- Zangrillo, A.; Beretta, L.; Scandroglio, A.M.; Monti, G.; Fominskiy, E.; Colombo, S.; Morselli, F.; Belletti, A.; Silvani, P.; Crivellari, M.; et al. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit. Care. Resusc. 2020, 22, 200–211. [Google Scholar] [PubMed]
- Lazartigues, E.; Qadir, M.M.F.; Mauvais-Jarvis, F. Endocrine Significance of SARS-CoV-2’s Reliance on ACE2. Endocrinology 2020, 161. [Google Scholar] [CrossRef]
- Maleki Dana, P.; Sadoughi, F.; Hallajzadeh, J.; Asemi, Z.; Mansournia, M.A.; Yousefi, B.; Momen-Heravi, M. An Insight into the Sex Differences in COVID-19 Patients: What are the Possible Causes? Prehosp. Disaster. Med. 2020, 35, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Depuydt, P.; Oeyen, S.; De Smet, S.; De Raedt, S.; Benoit, D.; Decruyenaere, J.; Derom, E. Long-term outcome and health-related quality of life in difficult-to-wean patients with and without ventilator dependency at ICU discharge: A retrospective cohort study. BMC. Pulm. Med. 2016, 16, 133. [Google Scholar] [CrossRef][Green Version]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Hernu, R.; Chroboczek, T.; Madelaine, T.; Casalegno, J.S.; Lina, B.; Cour, M.; Argaud, L. Early oseltamivir therapy improves the outcome in critically ill patients with influenza: A propensity analysis. Intensive Care. Med. 2018, 44, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Martínez, A.; Soldevila, N.; Romero-Tamarit, A.; Torner, N.; Godoy, P.; Rius, C.; Jané, M.; Domínguez, À. Risk factors associated with severe outcomes in adult hospitalized patients according to influenza type and subtype. PLoS ONE 2019, 14, e0210353. [Google Scholar] [CrossRef] [PubMed]
- Du, R.H.; Liang, L.R.; Yang, C.Q.; Wang, W.; Cao, T.Z.; Li, M.; Guo, G.Y.; Du, J.; Zheng, C.L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55. [Google Scholar] [CrossRef]
- Gupta, S.; Hayek, S.S.; Wang, W.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J.; et al. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US. JAMA Intern. Med. 2020, 180, 1436–1447. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef]
- Thompson, B.T.; Chambers, R.C.; Liu, K.D. Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2017, 377, 562–572. [Google Scholar] [CrossRef]
- Fajgenbaum, D.C.; June, C.H. Cytokine Storm. N. Engl. J. Med. 2020, 383, 2255–2273. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed]

| Critical Illness | Non-Critical Illness | p Value | |
|---|---|---|---|
| (n = 219) | (n = 303) | ||
| Demographics | |||
| Age (median (IQR)) | 60 (50, 70) | 58 (44, 71) | 0.234 |
| Male sex (%) | 116 (53) | 129 (43) | 0.024 |
| Race (%) | 0.170 | ||
| White | 121 (55) | 144 (48) | |
| Black | 69 (32) | 105 (35) | |
| Other | 29 (13) | 54 (18) | |
| Hispanic ethnicity (%) | 21 (10) | 50 (17) | 0.032 |
| Neoplastic disease (%) | 14 (6) | 14 (5) | 0.490 |
| Renal disease (%) | 34 (16) | 49 (16) | 0.938 |
| Liver disease (%) | 4 (2) | 13 (4) | 0.188 |
| Heart failure (%) | 28 (13) | 29 (10) | 0.308 |
| COPD (%) | 33 (15) | 33 (11) | 0.199 |
| Smoking history, current or former (%) | 82 (37) | 100 (33) | 0.338 |
| Diabetes (%) | 79 (36) | 84 (28) | 0.053 |
| Obese (%) | 121 (55) | 154 (51) | 0.362 |
| Hypertension (%) | 116 (53) | 155 (51) | 0.749 |
| Coronary artery disease (%) | 24 (11) | 40 (13) | 0.525 |
| Hyperlipidemia (%) | 72 (33) | 97 (32) | 0.910 |
| Exam and lab values at time of admission or critical illness, median (IQR) | |||
| Temperature (degrees celsius) | 37.6 (36.9, 38.8) | 37.8 (37.0, 38.5) | 0.880 |
| Respiratory rate (breaths/min) | 27.0 (21.0, 34.0) | 20.0 (18.0, 24.0) | <0.001 |
| Heart rate (beats/min) | 101.0 (87.5, 112.5) | 97.0 (80.0, 110.0) | 0.050 |
| Systolic blood pressure (mmHg) | 110.0 (97.0, 132.0) | 124.0 (109.0, 141.0) | <0.001 |
| Diastolic blood pressure (mmHg) | 61.0 (48.0, 75.0) | 69.0 (61.0, 81.5) | <0.001 |
| Mean arterial pressure (mmHg) | 77.7 (64.7, 92.3) | 88.7 (78.3, 99.0) | <0.001 |
| BUN (mg/dL) | 17.0 (12.0, 29.0) | 15.0 (10.0, 23.0) | 0.021 |
| Glucose (mg/dL) | 132.0 (112.0, 183.0) | 117.0 (102.0, 143.0) | <0.001 |
| Hematocrit (%) | 37.4 (33.0, 40.7) | 39.0 (35.9, 42.6) | <0.001 |
| Sodium (mEq/L) | 136.0 (133.0, 138.0) | 136.0 (134.0, 138.0) | 0.544 |
| White blood cell count (×1000 per uL) | 7.8 (5.8, 11.0) | 5.6 (4.3, 7.3) | <0.001 |
| Neutrophil count (×1000 per uL) | 5.8 (4.5, 8.3) | 3.7 (2.7, 5.6) | <0.001 |
| Lymphocyte count (×1000 per uL) | 0.9 (0.7, 1.1) | 1.1 (0.8, 1.4) | <0.001 |
| Neutrophil/lymphocyte (ratio) | 8.0 (5.2, 10.1) | 3.4 (2.2, 5.9) | <0.001 |
| Interleukin-6 (pg/mL) | 92.2 (51.3, 218.1) | 33.8 (16.6, 58.2) | <0.001 |
| C-reactive protein (CRP) (mg/L) | 162.4 (82.2, 216.4) | 53.0 (24.5, 120.0) | <0.001 |
| D-dimer (ng/mL) | 813.0 (318.2, 2147.5) | 681.0 (370.0, 1080.0) | 0.115 |
| Ferritin (ng/mL) | 554.5 (289.8, 994.8) | 292.0 (115.5, 637.0) | <0.001 |
| Lactate (mmol/L) | 1.5 (1.2, 2.4) | 1.2 (1.0, 1.7) | <0.001 |
| Creatinine (mg/dL) | 1.0 (0.7, 1.4) | 0.9 (0.7, 1.2) | 0.024 |
| Albumin (g/dL) | 3.3 (2.8, 3.6) | 3.8 (3.5, 4.1) | <0.001 |
| Bilirubin (mg/dL) | 0.7 (0.5, 1.0) | 0.6 (0.4, 0.9) | <0.001 |
| PaO2/FiO2 (ratio) | 174.0 (85.4, 253.0) | 355.0 (336.8, 378.5) | <0.001 |
| SpO2/FiO2 (ratio) | 220.0 (95.8, 332.1) | 442.9 (384.5, 457.1) | <0.001 |
| Treatments and therapies, n (%) | |||
| Hydroxychloroquine (%) | 120 (55) | 76 (25) | <0.001 |
| Azithromycin (%) | 158 (72) | 181 (60) | 0.001 |
| Remdesivir (%) | 21 (10) | 7 (2) | <0.001 |
| Steroids (%) | 91 (42) | 28 (9) | <0.001 |
| Low molecular weight heparins (%) | 150 (68) | 180 (59) | 0.092 |
| Heparin (%) | 69 (32) | 17 (6) | <0.001 |
| Plasma (%) | 36 (16) | 7 (2) | <0.001 |
| Critical Illness | Non-Critical Illness | p Value | |
|---|---|---|---|
| (n = 219) | (n = 303) | ||
| Outcomes | |||
| Time to death or discharge from admission | 14.0 (8.0, 20.0) | 4.1 (2.6, 6.9) | <0.001 |
| Time to ICU admission from admission | 1.0 (0.0, 2.5) | ||
| Time to death or ICU discharge from ICU admission | 8.3 (2.7, 15.2) | ||
| Time to IMV from admission | 1.7 (0.3, 3.7) | ||
| Time to death, tracheostomy, or weaning from intubation | 8.8 (4.0, 14.2) | ||
| Time to IMV from ICU admission | 0.1 (0.0, 1.4) | ||
| Septic shock (%) | 60 (27) | 0 (0) | <0.001 |
| DIC (%) | 2 (1) | 0 (0) | 0.343 |
| Development of ARDS (%) | 114 (52) | 0 (0) | <0.001 |
| Cardiovascular or cardiac event (%) | 59 (27) | 24 (8) | <0.001 |
| In-hospital mortality (%) | 43 (20) | 4 (1) | <0.001 |
| Age | 66 (57, 73) | 83 (75, 90) | <0.001 |
| Male sex | 29 (67) | 1 (25) | 0.124 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bordon, J.; Akca, O.; Furmanek, S.; Cavallazzi, R.S.; Suliman, S.; Aboelnasr, A.; Sinanova, B.; Ramirez, J.A. Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia. J. Clin. Med. 2021, 10, 2935. https://doi.org/10.3390/jcm10132935
Bordon J, Akca O, Furmanek S, Cavallazzi RS, Suliman S, Aboelnasr A, Sinanova B, Ramirez JA. Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia. Journal of Clinical Medicine. 2021; 10(13):2935. https://doi.org/10.3390/jcm10132935
Chicago/Turabian StyleBordon, Jose, Ozan Akca, Stephen Furmanek, Rodrigo Silva Cavallazzi, Sally Suliman, Amr Aboelnasr, Bettina Sinanova, and Julio A. Ramirez. 2021. "Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia" Journal of Clinical Medicine 10, no. 13: 2935. https://doi.org/10.3390/jcm10132935
APA StyleBordon, J., Akca, O., Furmanek, S., Cavallazzi, R. S., Suliman, S., Aboelnasr, A., Sinanova, B., & Ramirez, J. A. (2021). Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia. Journal of Clinical Medicine, 10(13), 2935. https://doi.org/10.3390/jcm10132935







