Variablity of Mechanical or Tissue Valve Implantation in Patients Undergoing Surgical Aortic Valve Replacement in Spain: National Retrospective Analysis from 2007 to 2018
Abstract
1. Introduction
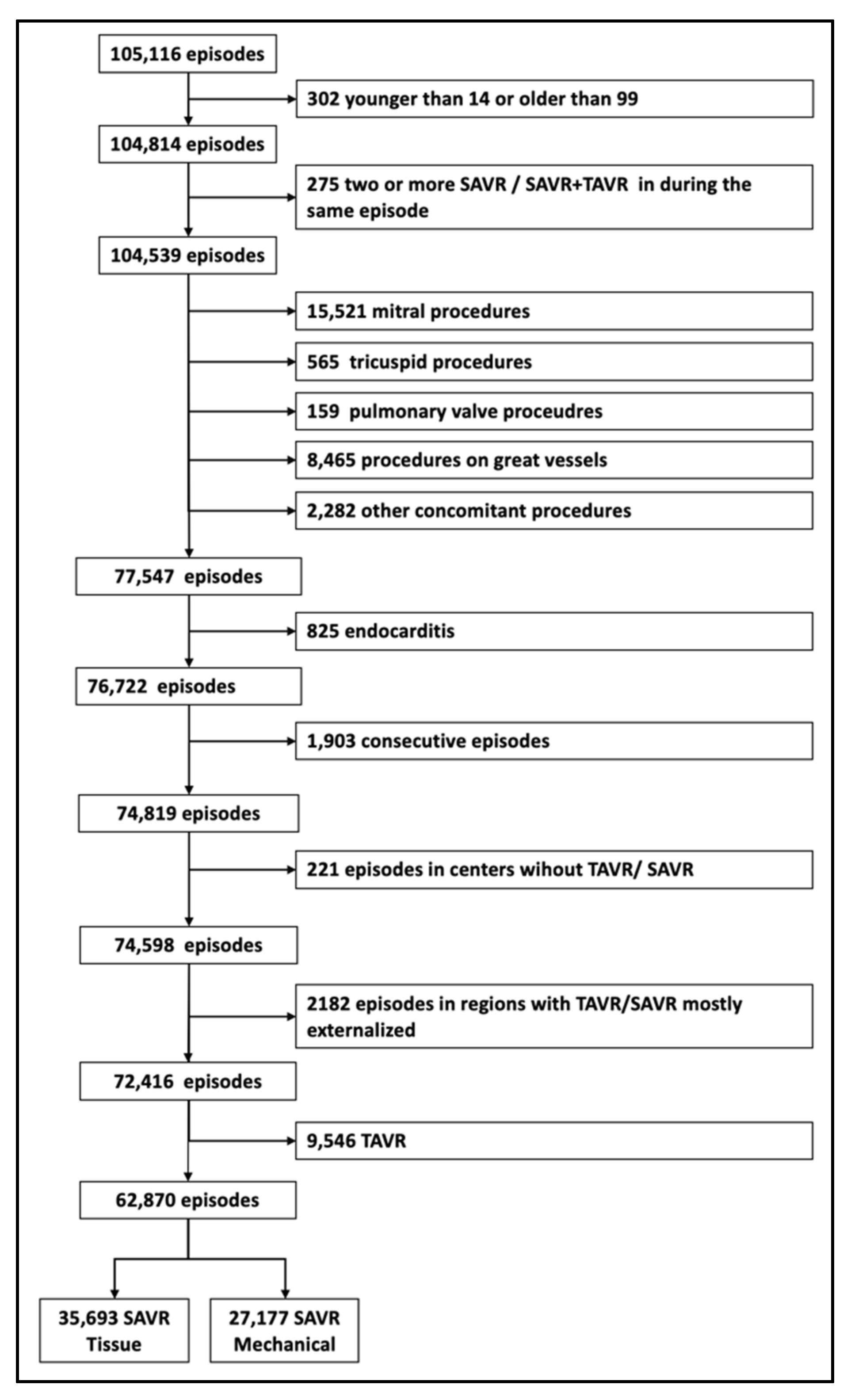
2. Materials and Methods
2.1. Type of Aortic Valve Procedure
2.2. National Volume of SAVR Procedures and Risk Profile of the Patients
2.3. Statistical Analysis
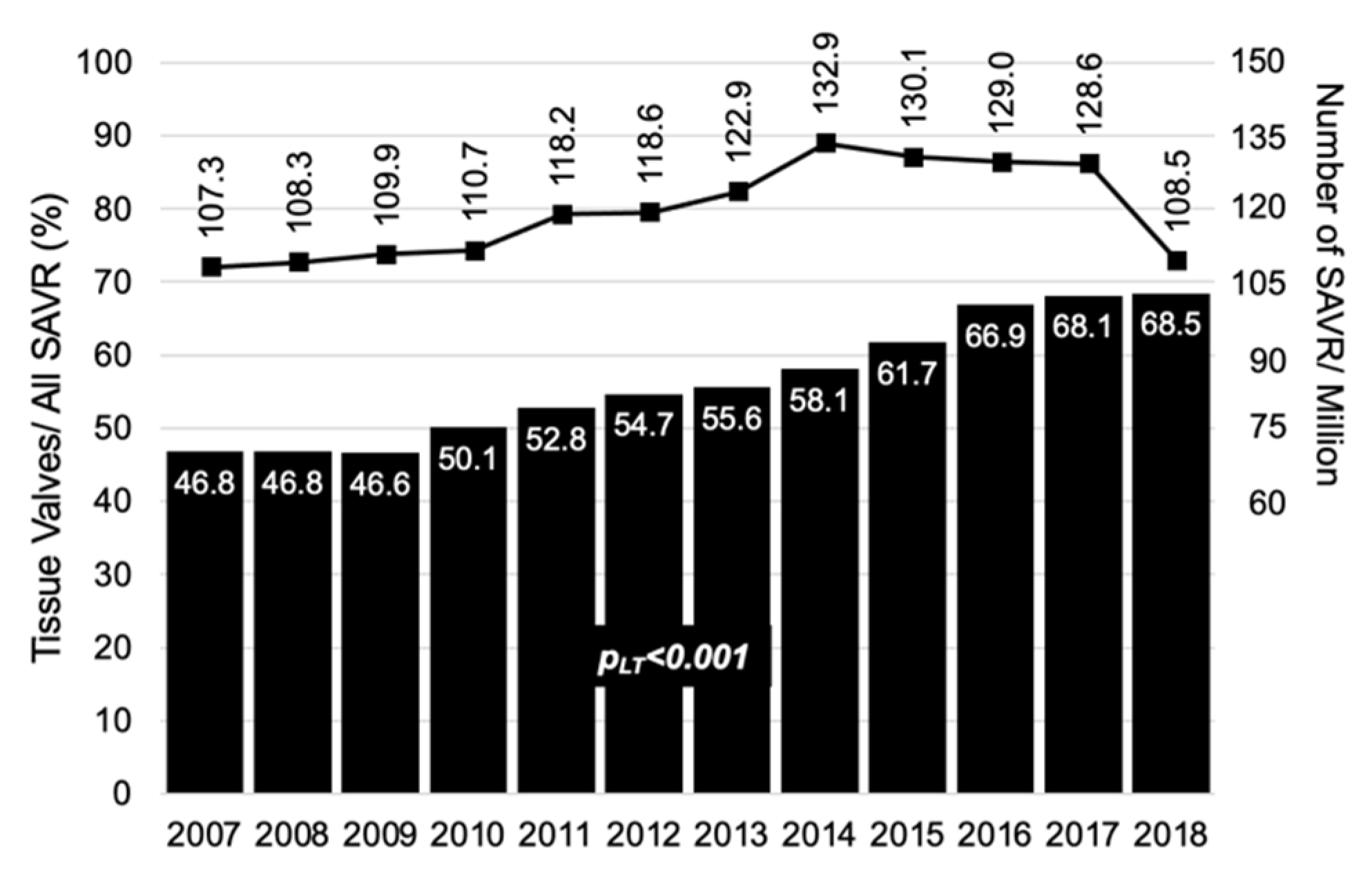
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Coffey, S.; Cairns, B.; Iung, B. The modern epidemiology of heart valve disease. Heart 2016, 102, 75–85. [Google Scholar] [CrossRef]
- Leon, M.B.; Mack, M.J.; Hahn, R.T.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Alu, M.C.; Madhavan, M.V.; Chau, K.H.; Russo, M.; et al. Outcomes 2 Years After Transcathe-ter Aortic Valve Replacement in Patients at Low Surgical Risk. J. Am. Coll. Cardiol. 2021, 77, 1149–1161. [Google Scholar] [CrossRef]
- Leon, M.B.; Smith, C.R.; Mack, M.J.; Makkar, R.R.; Svensson, L.G.; Kodali, S.K.; Thourani, V.H.; Tuzcu, E.M.; Miller, D.C.; Herrmann, H.C.; et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N. Engl. J. Med. 2016, 374, 1609–1620. [Google Scholar] [CrossRef]
- Mentias, A.; Sarrazin, M.V.; Desai, M.; Kapadia, S.; Cram, P.; Girotra, S. Expansion of transcatheter aortic valve replacement in the United States. Am. Hear. J. 2021, 234, 23–30. [Google Scholar] [CrossRef]
- Daeter, E.J.; van Veghel, D.; Houterman, S.; Olsthoorn, J.; Soliman-Hamad, M.A. Recent trends in aortic valve interventions: Data of the Netherlands heart registration. J. Card. Surg. 2021, 36, 573–581. [Google Scholar] [CrossRef]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e35–e71. [Google Scholar] [CrossRef]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Muñoz, D.R.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef]
- Wendt, D.; Thielmann, M.; Plicht, B.; Aßmann, J.; Price, V.; Neuhäuser, M.; Jakob, H. The new St Jude Trifecta versus Carpentier-Edwards Perimount Magna and Magna Ease aortic bioprosthesis: Is there a hemodynamic superiority? J. Thorac. Cardiovasc. Surg. 2014, 147, 1553–1560. [Google Scholar] [CrossRef][Green Version]
- Bourguignon, T.; Bouquiaux-Stablo, A.-L.; Candolfi, P.; Mirza, A.; Loardi, C.; May, M.-A.; El-Khoury, R.; Marchand, M.; Aupart, M. Very long-term out-comes of the Carpentier-Edwards Perimount valve in aortic position. Ann. Thorac. Surg. 2015, 99, 831–837. [Google Scholar] [CrossRef]
- Brown, J.M.; O’Brien, S.M.; Wu, C.; Sikora, J.A.H.; Griffith, B.P.; Gammie, J.S. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: Changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J. Thorac. Cardiovasc. Surg. 2009, 137, 82–90. [Google Scholar] [CrossRef]
- Dunning, J.; Gao, H.; Chambers, J.; Moat, N.; Murphy, G.; Pagano, D.; Ray, S.; Roxburgh, J.; Bridgewater, B. Aortic valve surgery: Marked increases in volume and significant decreases in mechanical valve use—An analysis of 41,227 patients over 5 years from the Society for Cardiothoracic Surgery in Great Britain and Ireland National database. J. Thorac. Cardiovasc. Surg. 2011, 142, 776–782.e3. [Google Scholar] [CrossRef]
- Siregar, S.; De Heer, F.; Groenwold, R.H.; Versteegh, M.I.; Bekkers, J.A.; Brinkman, E.S.; Bots, M.L.; Van Der Graaf, Y.; Van Herwerden, L.A. Trends and outcomes of valve surgery: 16-year results of Netherlands Cardiac Surgery National Database†. Eur. J. Cardio Thorac. Surg. 2014, 46, 386–397. [Google Scholar] [CrossRef]
- World Population Prospects 2019: Demographic Profiles. Available online: https://population.un.org/wpp/ (accessed on 20 July 2021).
- Ramos, J.; Monteagudo, J.M.; González-Alujas, T.; Fuentes, M.E.; Sitges, M.; Peña, M.L.; Carrasco-Chinchilla, F.; Echeverría, T.; Bouzas-Mosquera, A.; Alberti, J.F.F.; et al. Large-scale assessment of aortic stenosis: Facing the next cardiac epidemic? Eur. Hear. J. Cardiovasc. Imaging 2017, 19, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Bernal-Delgado, E.; Garcia-Armesto, S.; Oliva, J.; Sanchez Martinez, F.I.; Repullo, J.R.; Pena-Longobardo, L.M.; Ridao-Lopez, M.; Hernandez-Quevedo, C. Spain: Health System Review. Health Syst. Transit. 2018, 20, 1–179. [Google Scholar] [PubMed]
- Cequier, Á.; Ariza-Solé, A.; Elola, F.J.; Fernández-Pérez, C.; Bernal, J.L.; Segura, J.V.; Iniguez, A.; Bertomeu, V. Impact on Mortality of Different Network Systems in the Treatment of ST-segment Elevation Acute Myocardial Infarction. The Spanish Experience. Rev. Esp. Cardiol. Engl. Ed. 2017, 70, 155–161. [Google Scholar] [CrossRef]
- Mack, M.J.; Herbert, M.; Prince, S.; Dewey, T.M.; Magee, M.J.; Edgerton, J.R. Does reporting of coronary artery bypass grafting from administrative databases accurately reflect actual clinical outcomes? J. Thorac. Cardiovasc. Surg. 2005, 129, 1309–1317. [Google Scholar] [CrossRef] [PubMed]
- Bertomeu, V.; Cequier, Á.; Bernal, J.L.; Alfonso, F.; Anguita, M.P.; Muñiz, J.; Barrabés, J.A.; García-Dorado, D.; Goicolea, J.; Elola, F.J. In-hospital Mortality Due to Acute Myocardial Infarction. Relevance of Type of Hospital and Care Provided. RECALCAR Study. Rev. Española Cardiol. 2013, 66, 935–942. [Google Scholar] [CrossRef]
- Íñiguez Romo, A.; Bertomeu Martínez, V.; Rodríguez Padial, L.; Anguita Sánchez, M.; Ruiz Mateas, F.; Hidalgo Urbano, R.; Bernal Sobrino, J.L.; Fernandez Perez, C.; Macaya de Miguel, C.; Elola Somoza, F.J. The RECALCAR Project. Healthcare in the Cardiology Units of the Spanish National Health System, 2011 to 2014. Rev. Espanola Cardiol. 2017, 70, 567–575. [Google Scholar] [CrossRef]
- Carnero Alcazar, M.; Hernandez-Vaquero, D.; Cubero-Gallego, H.; Lopez Menendez, J.; Piñon, M.; Albors Martin, J.; Cuerpo Caballero, G.; Cobiella Carnicer, J.; Villamor, C.; Forteza, A.; et al. Retrospective cohort analysis of Spanish national trends of coronary artery bypass grafting and per-cutaneous coronary intervention from 1998 to 2017. BMJ Open 2021, 11, e046141. [Google Scholar] [CrossRef]
- Carnero-Alcázar, M.; Maroto-Castellanos, L.C.; Hernández-Vaquero, D.; López-Menéndez, J.; Hornero-Sos, F.; Silva-Guisasola, J.; Cobiella-Carnicer, J.; Pérez-Camargo, D.; Arcaya, M.A.; Álvarez-D Arcaya, M.A.; et al. Isolated aortic valve replacement in Spain: National trends in risks, valve types, and mortality from 1998 to 2017. Rev. Española Cardiol. 2020. [Google Scholar] [CrossRef]
- Goicolea Ruigómez, F.J.; Elola, F.J.; Durante-López, A.; Fernández Pérez, C.; Bernal, J.L.; Macaya, C. Coronary artery bypass grafting in Spain. Influence of procedural volume on outcomes. Rev. Espanola Cardiol. 2020, 73, 488–494. [Google Scholar] [CrossRef]
- Herreros, J.M.; Mastrobuoni, S.; Ubilla, M.; Rábago, G.; Lorente Ruiz, M.; Rifón, J.; Hernandez, M. Cardiac and vascular homograft valves transplant. An. Sist. Sanit. Navar. 2006, 29 (Suppl. 2), 153–161. [Google Scholar] [CrossRef][Green Version]
- INE. Economy; INE (Instituto Nacional de Estadística/Statistical Spanish Office): Madrid, Spain, 2018; Available online: http://www.ine.es (accessed on 22 April 2021).
- Charlson, M.; Szatrowski, T.P.; Peterson, J.; Gold, J. Validation of a combined comorbidity index. J. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2019: Health Expenditure Per Capita; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Goldstone, A.B.; Chiu, P.; Baiocchi, M.; Lingala, B.; Patrick, W.L.; Fischbein, M.P.; Woo, Y.J. Mechanical or Biologic Prostheses for Aortic-Valve and Mitral-Valve Replacement. N. Engl. J. Med. 2017, 377, 1847–1857. [Google Scholar] [CrossRef] [PubMed]
- Glaser, N.; Jackson, V.; Holzmann, M.J.; Franco-Cereceda, A.; Sartipy, U. Aortic valve replacement with mechanical vs. biological prostheses in patients aged 50–69 years. Eur. Heart J. 2016, 37, 2658–2667. [Google Scholar] [CrossRef] [PubMed]
- Schelbert, E.B.; Vaughan-Sarrazin, M.S.; Welke, K.F.; Rosenthal, G.E. Hospital Volume and Selection of Valve Type in Older Patients Undergoing Aortic Valve Replacement Surgery in the United States. Circulation 2005, 111, 2178–2182. [Google Scholar] [CrossRef] [PubMed]
- Ramos Martín-Vegue, A.J. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM): Only shadows in its implementation. Rev. Calid. Asist. 2017, 32, 6–9. [Google Scholar] [PubMed]
| And | Ara | Ast | Bal | Can | Cant | CyL | Cat | Val | Ext | Gal | Mad | Mur | Nav | BC | p | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SAVR | 9212 (14.7) | 1580 (2.5) | 2922 (4.7) | 1646 (2.6) | 2061 (3.3) | 1470 (2.3) | 3783 (6) | 9488 (15.1) | 7442 (11.8) | 1007 (1.6) | 6900 (11) | 9892 (15.7) | 1745 (2.8) | 1097 (1.7) | 2625 (4.2) | <0.001 | 62,870 |
| Mechanical | 5031 (54.6) | 403 (25.5) | 1579 (54) | 390 (23.7) | 1215 (59) | 462 (31.4) | 1469 (38.8) | 3446 (36.3) | 3637 (48.9) | 821 (81.5) | 1572 (22.8) | 4808 (48.6) | 837 48) | 323 (29.4) | 1184 (45.1) | <0.001 | 27,177 (43.2) |
| Bioprosthesis | 4181 (45.4) | 1177 (74.5) | 1343 (46) | 1256 (76.3) | 846 (41) | 1008 (68.6) | 2314 (61.2) | 6042 (63.7) | 3805 (51.1) | 186 (18.5) | 5328 (77.2) | 5084 (51.4) | 908 (52) | 774 (70.6) | 1441 (54.9) | <0.001 | 35,693 (56.8) |
| Bio in >65 | 3731/6466 (57.7) | 1089/1233 (88.3) | 1290/2375 (54.3) | 1173/1322 (88.7) | 800/1592 (50.3) | 965/1134 (85.1) | 2232/3008 (74.2) | 5501/7128 (77.2) | 3583/5844 (61.3) | 184/703 (26.2) | 4962/5913 (83.9) | 4564/7361 (62) | 820/1239 (66.2) | 715/831 (86) | 1350/2018 (66.9) | <0.001 | 32,959/48,167 (68.4) |
| Bio in ≤65 | 450/2746 (16.4) | 88/347 (25.4) | 537,547 (9.7) | 83/324 (25.6) | 46/469 (9.8) | 43/336 (12.8) | 82/775 (10.6) | 541/1819 (22.9) | 222/1598 (13.9) | 2/304 (0.7) | 366/987 (37.1) | 520/2531 (20.6) | 88/506 (17.4) | 59/266 (22.2) | 91/607 (15) | <0.001 | 2734/14,703 (18.6) |
| Age | 68.5 (11) | 71.4 (10.4) | 72.5 (9.8) | 71.8 (10.3) | 70.8 (10.5) | 71.4 (9.7) | 72 (9.9) | 70.3 (11.5) | 71.2 (10.7) | 68.4 (10.4) | 73.7 (9) | 70.3 (12.1) | 68.6 (11.5) | 70.4 (11.4) | 71.3 (10.7) | <0.001 | 70.8 (10.9) |
| Female | 3770 (40.9) | 562 (35.6) | 1177 (40.3) | 648 (39.4) | 845 (40.5) | 567 (38.6) | 1369 (36.2) | 2764 (39.7) | 3025 (40.7) | 347 (34.5) | 2853 (41.4) | 4038 (40.8) | 684 (39.2) | 375 (34.2) | 988 (37.6) | <0.001 | 25,002 (39.8) |
| MI | 524 (5.7) | 51 (3.2) | 152 (5.2) | 133 (8.1) | 82 (4) | 71 (4.8) | 271 (7.2) | 546 (5.8) | 397 (5.3) | 22 (2.2) | 217 (3.1) | 486 (4.9) | 94 (5.4) | 54 (4.9) | 120 (4.6) | <0.001 | 3220 (5.1) |
| CHF | 1588 (17.2) | 113 (7.2) | 280 (9.6) | 400 (24.3) | 373 (18.1) | 214 (14.6) | 551 (14.6) | 2284 (24.1) | 1117 (15) | 47 (4.7) | 494 (7.2) | 1283 (13) | 207 (11.9) | 146 (13.3) | 258 (9.8) | <0.001 | 9355 (14.9) |
| PVD | 756 (8.2) | 63 (4) | 208 (7.1) | 178 (10.8) | 141 (6.8) | 189 (12.9) | 557 (14.7) | 1006 (10.6) | 774 (10.4) | 66 (6.6) | 358 (5.2) | 856 (8.7) | 162 (9.3) | 144 (13.1) | 269 (10.3) | <0.001 | 5727 (9.1) |
| COPD | 1067 (11.6) | 101 (6.4) | 228 (7.8) | 264 (16) | 166 (8.1) | 96 (8.1) | 590 (15.6) | 1309 (13.8) | 986 (13.3) | 67 (6.7) | 470 (6.8) | 1099 (11.1) | 196 (11.2) | 115 (10.5) | 351 (9.6) | <0.001 | 7005 (11.1) |
| CVD | 502 (5.5) | 34 (2.2) | 92 (3.2) | 189 (11.5) | 140 (6.8) | 65 (4.4) | 175 (4.6) | 573 (6) | 394 (5.3) | 23 (2.3) | 181 (2.6) | 435 (4.4) | 134 (7.7) | 33 (3) | 100 (3.8) | <0.001 | 3070 (4.9) |
| Diabetes | 2795 (30.3) | 378 (23.9) | 634 (21.7) | 519 (13.5) | 783 (38) | 268 (18.2) | 931 (24.6) | 2423 (25.5) | 2312 (31.1) | 206 (20.5) | 1687 (24.5) | 2637 (26.7) | 610 (35) | 225 (20.5) | 660 (25.1) | <0.001 | 17,068 (27.2) |
| CKD | 636 (6.9) | 148 (9.4) | 147 (5) | 259 (15.7) | 209 (10.1) | 68 (4.6) | 272 (7.2) | 919 (9.7) | 759 (10.2) | 37 (3.7) | 437 (6.3) | 849 (8.6) | 158 (9.1) | 119 (10.9) | 239 (9.1) | <0.001 | 5256 (8.4) |
| CABG | 1443 (15.7) | 392 (24.8) | 898 (30.7) | 715 (43.4) | 450 (21.8) | 410 (27.9) | 1239 (32.8) | 2137 (22.5) | 2035 (27.3) | 174 (17.3) | 1882 (27.3) | 1814 (18.3) | 256 (14.7) | 195 (17.8) | 696 (26.5) | <0.001 | 14,736 (23.4) |
| OAC | 859 (9.3) | 66 (4.2) | 111 (3.8) | 107 (6.5) | 203 (9.9) | 153 (10.4) | 562 (14.9) | 654 (6.9) | 7869 (10.6) | 80 (7.9) | 700 (10.1) | 870 (8.8) | 221 (12.7) | 128 (11.7) | 199 (7.6) | <0.001 | 5702 (9.1) |
| Prev. CS | 428 (4.7) | 52 (3.3) | 147 (5) | 47 (2.9) | 58 (2.8) | 42 (2.9) | 165 (4.4) | 432 (4.6) | 356 (4.8) | 50 (5) | 258 (3.7) | 543 (5.5) | 77 (4.4) | 45 (4.1) | 102 (3.9) | <0.001 | 2802 (4.5) |
| Prev. PCI | 684 (7.4) | 82 (5.2) | 73 (2.5) | 78 (4.8) | 81 (3.9) | 53 (3.6) | 235 (6.2) | 276 (2.9) | 353 (4.7) | 46 (4.6) | 324 (4.7) | 556 (5.6) | 195 (11.2) | 47 (4.3) | 157 (6) | <0.001 | 3242 (5.2) |
| Charlson | 3.5 (1.7) | 3.4 (1.5) | 3.6 (1.5) | 4.2 (1.9) | 3.8 (1.7) | 3.5 (1.5) | 3.8 (1.6) | 3.8 (1.8) | 3.8 (1.7) | 2.9 (1.4) | 3.6 (1.5) | 3.6 (1.8) | 3.5 (1.7) | 3.5 (1.7) | 3.6 (1.7) | <0.001 | 3.6 (1.7) |
| No. of SAVR Hospitals 1 | 0/3/3/1 | 0/1/0/0 | 1/0/0/0 | 0/1/0/0 | 0/0/1/1 | 0/1/0/0 | 0/1/1/1 | 4/1/0/1 | 0/3/1/3 | 0/0/1/0 | 3/0/0/0 | 2/0/3/4 | 1/0/0/0 | 0/0/1/0 | 0/1/1/0 | 0.018 | 46 |
| Hospital SAVR vol. | <0.001 | ||||||||||||||||
| High | 0 | 0 | 2922 (100) | 0 | 0 | 0 | 0 | 7451 (78.5) | 0 | 0 | 6900 (100) | 4406 (44.5) | 1745 (100) | 0 | 0 | 23,424 (37.3) | |
| I-H | 4573 (49.6) | 1580 (100) | 0 | 1646 (100) | 0 | 1470 (100) | 1620 (42.8) | 1724 (18.2) | 4569 (61.4) | 0 | 0 | 0 | 0 | 0 | 1353 (51.5) | 18,535 (29.5) | |
| L-I | 3730 (40.5) | 0 | 0 | 0 | 1097 (53.2) | 0 | 1215 (32.1) | 0 | 1120 (15.1) | 1007 (100) | 0 | 3789 (38.3) | 0 | 1097 (100) | 1272 (48.5) | 14,327 (22.8) | |
| Low | 909 (9.9) | 0 | 0 | 0 | 964 (46.8) | 0 | 948 (25.1) | 313 (3.3) | 1753 (23.6) | 0 | 0 | 1697 (17.2) | 0 | 0 | 0 | 6584 (10.5) | |
| No. of SAVR Hospitals 2 | 2/3/2/0 | 0/0/1/0 | 1/0/0/0 | 0/0/1/0 | 0/0/1/1 | 1/0/0/0 | 1/1/1/0 | 1/2/1/2 | 0/3/0/4 | 0/1/0/0 | 3/0/0/0 | 3/2/2/2 | 1/0/0/0 | 0/0/1/0 | 0/2/0/0 | 0.2 | 46 |
| Hospital TAVR vol. | <0.001 | ||||||||||||||||
| High | 2386 (25.9) | 0 | 2922 (100) | 0 | 0 | 1470 (100) | 1620 (42.8) | 1821 (19.2) | 0 | 0 | 6900 (100) | 4363 (44.1) | 0 | 0 | 0 | 23,227 (36.9) | |
| I-H | 4210 (45.7) | 0 | 0 | 0 | 0 | 0 | 948 (25.1) | 3850 (40.6) | 3576 (48.1) | 1007 (100) | 0 | 3497 (35.4) | 1745 (100) | 0 | 2625 (100) | 19,713 (31.4) | |
| L-I | 2616 (28.4) | 1580 (100) | 0 | 1646 (100) | 1097 (53.2) | 0 | 1215 (32.1) | 1780 (18.8) | 0 | 0 | 0 | 1710 (17.3) | 0 | 1097 (100) | 0 | 12,741 (20.3) | |
| Low | 0 | 0 | 0 | 0 | 964 (46.8) | 0 | 0 | 2037 (21.5) | 3866 (52) | 0 | 0 | 322 (3.3) | 0 | 0 | 0 | 7189 (11.4) |
| 2007–2009 | 2010–2012 | 2013–2015 | 2016–2018 | pLT | |
|---|---|---|---|---|---|
| SAVR | 14,163 | 15,488 | 17,086 | 16,133 | 62,870 |
| Mechanical | 7543 (53.3) | 7342 (47.4) | 7096 (41.5) | 5196 (32.2) | <0.001 |
| Tissue | 6620 (46.7) | 8146 (52.6) | 9990 (58.5) | 10,937 (67.8) | <0.001 |
| Tissue > 65 | 6150 (58.8) | 7559 (64) | 9326 (69.1) | 9924 (80) | <0.001 |
| Edad | 69.7 (11.2) | 70.7 (11) | 71.5 (10.7) | 71 (10.8) | <0.001 |
| Female | 5635 (39.8) | 6251 (40.4) | 6849 (40.1) | 6267 (38.9) | 0.068 |
| Previous MI | 861 (6.1) | 735 (4.8) | 687 (4) | 937 (5.8) | 0.093 |
| CHF | 2138 (15.1) | 2159 (13.9) | 2814 (16.5) | 2244 (13.9) | 0.46 |
| PVD | 1373 (9.7) | 1536 (9.9) | 1423 (8.3) | 1395 (8.7) | <0.001 |
| CVD | 527 (3.7) | 711 (4.6) | 978 (5.7) | 854 (5.3) | <0.001 |
| COPD | 1605 (11.3) | 1688 (10.9) | 1910 (11.2) | 1802 (11.2) | 0.89 |
| Diabetes | 3364 (23.8) | 4175 (27) | 4806 (28.1) | 4723 (29.3) | <0.001 |
| CKD | 799 (5.6) | 1240 (8) | 1697 (9.9) | 1520 (9.4) | <0.001 |
| CABG | 3477 (24.6) | 3757 (24.3) | 3953 (23.1) | 3549 (22) | <0.001 |
| OAC | 1054 (7.4) | 1206 (7.8) | 1613 (9.4) | 1829 (11.3) | <0.001 |
| Previous CS | 609 (4.3) | 649 (4.2) | 683 (4) | 861 (5.3) | <0.001 |
| Previous PCI | 528 (3.7) | 800 (5.2) | 891 (5.2) | 1023 (6.3) | <0.001 |
| Charlson | 3.4 (1.6) | 3.6 (1.7) | 3.8 (1.7) | 3.7 (1.7) | <0.001 |
| Autonomous Region | <0.001 * | ||||
| Andalusia | 2150 (14.9) | 2420 (15.1) | 2829 (14.7) | 2593 (15.8) | |
| Aragon | 283 (2) | 362 (2.3) | 508 (2.6) | 518 (2.3) | |
| P. Asturias | 705 (4.9) | 678 (4.2) | 887 (4.6) | 1019 (4.5) | |
| Balears Islands | 392 (2.7) | 412 (2.6) | 440 (2.3) | 537 (2.4) | |
| Canary Islands | 430 (3) | 447 (2.8) | 658 (3.4) | 719 (3.2) | |
| Castile & Leon | 985 (6.8) | 1032 (6.5) | 1105 (5.7) | 1372 (6) | |
| Catalonia | 2156 (15) | 2159 (13.5) | 2689 (13.9) | 3456 (15.2) | |
| Valencianan C. | 1367 (9.5) | 1698 (10.6) | 2358 (12.2) | 2619 (11.5) | |
| Extremadura | 206 (1.4) | 250 (1.6) | 317 (1.6) | 401 (1.8) | |
| Galicia | 1551 (10.8) | 1827 (11.4) | 2378 (12.3) | 2387 (10.5) | |
| C. of Madrid | 2496 (17.3) | 2751 (17.2) | 2995 (15.5) | 3693 (16.3) | |
| R. of Murcia | 431 (3) | 405 (2.5) | 547 (2.8) | 657 (2.9) | |
| Foral C. of Navarra | 255 (1.8) | 336 (2.1) | 307 (1.6) | 347 (1.5) | |
| Basque Country | 601 (4.2) | 753 (4.7) | 770 (4) | 897 (4) |
| Univariable | Multivariable | |||
|---|---|---|---|---|
| OR (CI 95%) | p | OR (CI 95%) | p | |
| Age group 1 | ||||
| 60–70 | 3.42 (3.2 to 3.66) | <0.001 | 3.45 (3.19 to 3.74) | <0.001 |
| 70–80 | 14.27 (13.4 to 15.2) | <0.001 | 16.95 (15.59 to 18.44) | <0.001 |
| >80 | 20.85 (19.37 to 22.43) | <0.001 | 21.91 (20.7 to 23.2) | <0.001 |
| Female sex | 1.32 (1.28 to 1.36) | <0.001 | ||
| Previous MI | 1.04 (0.97 to 1.12) | 0.24 | ||
| CHF | 0.94 (0.9 to 0.99) | 0.014 | 0.84 (0.81 to 0.87) | <0.001 |
| PVD | 0.74 (0.7; 0.78) | <0.001 | 0.79 (0.75 to 0.83) | <0.001 |
| CVD | 1.28 (1.18 to 1.37) | <0.001 | ||
| COPD | 1.02 (0.97 to 1.08) | 0.34 | ||
| CKD | 1.45 (1.36 to 1.53) | <0.001 | ||
| CABG | 1.61 (1.56 to 1.68) | <0.001 | 1.29 (1.22 to 1.36) | <0.001 |
| Previous PCI | 1.32 (1.22 to 1.42) | <0.001 | 1.1 (1.03 to 1.16) | 0.004 |
| Previous CS | 0.46 (0.42 to 0.49) | <0.001 | 0.5 (0.45 to 0.55) | <0.001 |
| Charlson | 1.5 (1.48 to 1.51) | <0.001 | 1.02 (1.01 to 1.03) | <0.001 |
| SAVR Volume 2 | ||||
| I-H | 0.85 (0.82 to 0.88) | <0.001 | 0.82 (0.74 to 0.9) | <0.001 |
| L-I | 0.51 (0.49 to 0.53) | <0.001 | 0.56 (0.52 to 0.6) | <0.001 |
| Low | 0.46 (0.43 to 0.49) | <0.001 | 0.49 (0.47 to 0.51) | <0.001 |
| OAC | 0.78 (0.73 to 0.82) | <0.001 | 0.53 (0.49 to 0.56) | <0.001 |
| Diabetes | 1.23 (1.18 to 1.27) | <0.001 | ||
| Period 3 | ||||
| 2010–2012 | 1.26 (1.21 to 1.32) | <0.001 | 1.27 (1.22 to 1.32) | <0.001 |
| 2013–2015 | 1.6 (1.53 to 1.68) | <0.001 | 1.67 (1.6 to 1.74) | <0.001 |
| 2016–2018 | 2.4 (2.29 to 2.51) | <0.001 | 3.28 (3.19 to 3.39) | <0.001 |
| Autonomous Region 4 | ||||
| Andalusia | 0.79 (0.75 to 0.84) | <0.001 | 1.07 (1.1 to 1.14) | 0.034 |
| Aragon | 2.79 (2.47 to 3.15) | <0.001 | 3.08 (2.89 to 3.28) | <0.001 |
| P. Asturias | 0.81 (0.76 to 0.89) | <0.001 | 0.47 (0.4 to 0.55) | <0.001 |
| Balears Islands | 3.08 (2.72 to 3.48) | <0.001 | 3.46 (3.02 to 3.97) | <0.001 |
| Canary Islands | 0.67 (0.6 to 0.73) | <0.001 | 0.8 (0.75 to 0.86) | <0.001 |
| Cantabria | 2.09 (1.85 to 2.35) | <0.001 | 2.6 (2.23 to 3.03) | <0.001 |
| Castile & Leon | 1.51 (1.39 to 1.63) | <0.001 | 1.95 (1.93 to 1.98) | <0.001 |
| Catalonia | 1.67 (1.57 to 1.78) | <0.001 | 1.66 (1.51 to 1.92) | <0.001 |
| Valencianan C. | 0.22 (0.18 to 0.26) | <0.001 | 0.25 (0.2 to 0.31) | <0.001 |
| Galicia | 3.24 (3.01 to 3.48) | <0.001 | 2.57 (2.24 to 2.97) | <0.001 |
| C. of Madrid | 1.01 (0.95 to 1.07) | 0.73 | 1.19 (1.13 to 1.25) | <0.001 |
| R. of Murcia | 1.03 (0.93 to 1.15) | 0.5 | 1 (0.95 to 1.05) | 0.87 |
| Foral C. of Navarra | 2.29 (2 to 2.63) | <0.001 | 4.67 (4.46 to 4.89) | <0.001 |
| Basque Country | 1.16 (1.06 to 1.27) | 0.001 | 1.32 (1.12 to 1.55) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carnero-Alcázar, M.; Rodríguez-Caulo, E.; Hernández-Vaquero, D.; Montero-Cruces, L.; Perez-Camargo, D.; Fernández-De Velasco, D.; Cobiella-Carnicer, J.; Maroto-Castellanos, L. Variablity of Mechanical or Tissue Valve Implantation in Patients Undergoing Surgical Aortic Valve Replacement in Spain: National Retrospective Analysis from 2007 to 2018. J. Clin. Med. 2021, 10, 3209. https://doi.org/10.3390/jcm10153209
Carnero-Alcázar M, Rodríguez-Caulo E, Hernández-Vaquero D, Montero-Cruces L, Perez-Camargo D, Fernández-De Velasco D, Cobiella-Carnicer J, Maroto-Castellanos L. Variablity of Mechanical or Tissue Valve Implantation in Patients Undergoing Surgical Aortic Valve Replacement in Spain: National Retrospective Analysis from 2007 to 2018. Journal of Clinical Medicine. 2021; 10(15):3209. https://doi.org/10.3390/jcm10153209
Chicago/Turabian StyleCarnero-Alcázar, Manuel, Emiliano Rodríguez-Caulo, Daniel Hernández-Vaquero, Lourdes Montero-Cruces, Daniel Perez-Camargo, David Fernández-De Velasco, Javier Cobiella-Carnicer, and Luis Maroto-Castellanos. 2021. "Variablity of Mechanical or Tissue Valve Implantation in Patients Undergoing Surgical Aortic Valve Replacement in Spain: National Retrospective Analysis from 2007 to 2018" Journal of Clinical Medicine 10, no. 15: 3209. https://doi.org/10.3390/jcm10153209
APA StyleCarnero-Alcázar, M., Rodríguez-Caulo, E., Hernández-Vaquero, D., Montero-Cruces, L., Perez-Camargo, D., Fernández-De Velasco, D., Cobiella-Carnicer, J., & Maroto-Castellanos, L. (2021). Variablity of Mechanical or Tissue Valve Implantation in Patients Undergoing Surgical Aortic Valve Replacement in Spain: National Retrospective Analysis from 2007 to 2018. Journal of Clinical Medicine, 10(15), 3209. https://doi.org/10.3390/jcm10153209






