Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives
Abstract
:1. Introduction
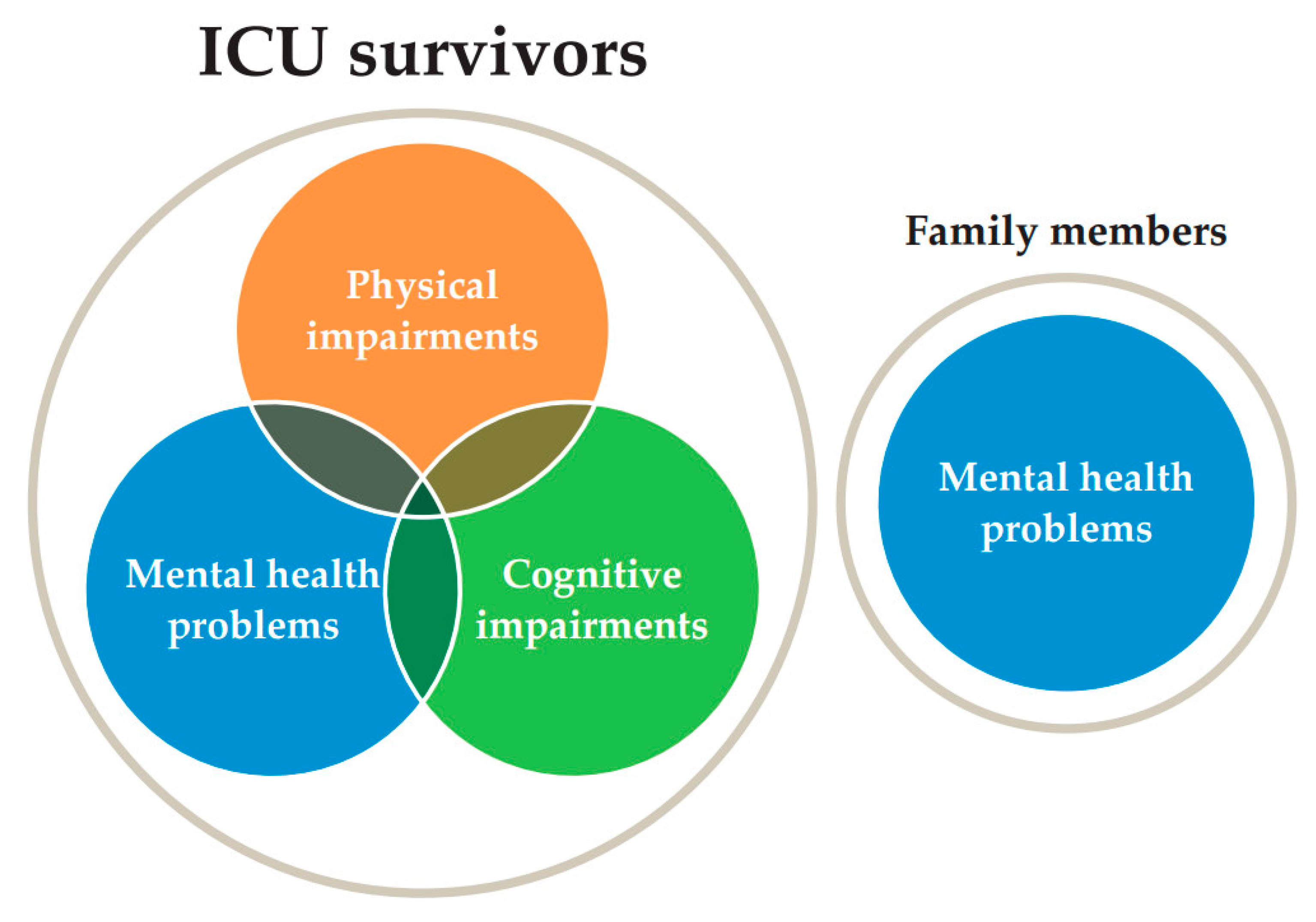
1.1. Recent Advances in PICS
1.1.1. Definition and Epidemiology
1.1.2. Physical Impairments
1.1.3. Cognitive Impairments
1.1.4. Mental Health Problems
1.1.5. PICS-F
1.1.6. Assessment of PICS
2. COVID-19 Infection
2.1. Epidemiology and Incidence
2.2. Pathophysiology of COVID-19
2.3. Treatment for COVID-19
2.4. PICS Features and Epidemiology in COVID-19
2.5. Mental Health for Healthcare Professional during the COVID-19 Pandemic
3. Prevention of PICS in COVID-19
3.1. Implementation of the ABCDEF Bundle
3.2. Team Building
3.3. Analgesia, Sedation, and Delirium Care
3.4. Nursing Care and ICU Diary
3.5. Early Rehabilitation
3.6. Nutrition
3.7. Family Engagement and Online Visitation
3.8. Follow-Up System
4. Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the global burden of disease study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Spieth, P.M.; Chiumello, D.; Goyal, H.; Torres, A.; Laffey, J.G.; Hong, Y. Declining mortality in patients with acute respiratory distress syndrome: An analysis of the acute respiratory distress syndrome network trials. Crit. Care Med. 2019, 47, 315–323. [Google Scholar] [CrossRef]
- Kamdar, B.B.; Suri, R.; Suchyta, M.R.; Digrande, K.F.; Sherwood, K.D.; Colantuoni, E.; Dinglas, V.D.; Needham, D.M.; Hopkins, R.O. Return to work after critical illness: A systematic review and meta-analysis. Thorax 2020, 75, 17–27. [Google Scholar] [CrossRef]
- Needham, D.M.; Davidson, J.; Cohen, H.; Hopkins, R.O.; Weinert, C.; Wunsch, H.; Zawistowski, C.; Bemis-Dougherty, A.; Berney, S.C.; Bienvenu, O.J.; et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders’ conference. Crit. Care Med. 2012, 40, 502–509. [Google Scholar] [CrossRef]
- Kawakami, D.; Fujitani, S.; Morimoto, T.; Dote, H.; Takita, M.; Takaba, A.; Hino, M.; Nakamura, M.; Irie, H.; Adachi, T.; et al. Prevalence of post-intensive care syndrome among Japanese intensive care unit patients: A prospective, multicenter, observational J-PICS study. Crit. Care 2021, 25, 69. [Google Scholar] [CrossRef]
- Marra, A.; Pandharipande, P.P.; Girard, T.D.; Patel, M.B.; Hughes, C.G.; Jackson, J.C.; Thompson, J.L.; Chandrasekhar, R.; Ely, E.W.; Brummel, N.E. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit. Care Med. 2018, 46, 1393–1401. [Google Scholar] [CrossRef]
- Riegel, B.; Huang, L.; Mikkelsen, M.E.; Kutney-Lee, A.; Hanlon, A.L.; Murtaugh, C.M.; Bowles, K.H. Early post-intensive care syndrome among older adult sepsis survivors receiving home care. J. Am. Geriatr Soc. 2019, 67, 520–526. [Google Scholar] [CrossRef]
- Bortz, W.M., II. A conceptual famework of frailty: A review. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M283–M288. [Google Scholar] [CrossRef] [Green Version]
- Parry, S.M.; Nalamalapu, S.R.; Nunna, K.; Rabiee, A.; Friedman, L.A.; Colantuoni, E.; Needham, D.M.; Dinglas, V.D. Six-minute walk distance after critical illness: A systematic review and meta-analysis. J. Intensive Care Med. 2021, 36, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Brummel, N.E.; Jackson, J.C.; Pandharipande, P.P.; Thompson, J.L.; Shintani, A.K.; Dittus, R.S.; Gill, T.M.; Bernard, G.R.; Ely, E.W.; Girard, T.D. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit. Care Med. 2014, 42, 369–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appleton, R.T.; Kinsella, J.; Quasim, T. The incidence of intensive care unit-acquired weakness syndromes: A systematic review. J. Intensive Care Soc. 2015, 16, 126–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Aerde, N.; Meersseman, P.; Debaveye, Y.; Wilmer, A.; Gunst, J.; Casaer, M.P.; Bruyninckx, F.; Wouters, P.J.; Gosselink, R.; Van den Berghe, G.; et al. Five-year impact of ICU-acquired neuromuscular complications: A prospective, observational study. Intensive Care Med. 2020. [Google Scholar] [CrossRef]
- Pandharipande, P.P.; Girard, T.D.; Jackson, J.C.; Morandi, A.; Thompson, J.L.; Pun, B.T.; Brummel, N.E.; Hughes, C.G.; Vasilevskis, E.E.; Shintani, A.K.; et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 2013, 369, 1306–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sukantarat, K.T.; Burgess, P.W.; Williamson, R.C.; Brett, S.J. Prolonged cognitive dysfunction in survivors of critical illness. Anaesthesia 2005, 60, 847–853. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Iwashyna, T.J.; Ely, E.W.; Smith, D.M.; Langa, K.M. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA 2010, 304, 1787–1794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mikkelsen, M.E.; Christie, J.D.; Lanken, P.N.; Biester, R.C.; Thompson, B.T.; Bellamy, S.L.; Localio, A.R.; Demissie, E.; Hopkins, R.O.; Angus, D.C. The adult respiratory distress syndrome cognitive outcomes study: Long-term neuropsychological function in survivors of acute lung injury. Am. J. Respir. Crit. Care Med. 2012, 185, 1307–1315. [Google Scholar] [CrossRef] [Green Version]
- Jackson, J.C.; Pandharipande, P.P.; Girard, T.D.; Brummel, N.E.; Thompson, J.L.; Hughes, C.G.; Pun, B.T.; Vasilevskis, E.E.; Morandi, A.; Shintani, A.K.; et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: A longitudinal cohort study. Lancet Respir. Med. 2014, 2, 369–379. [Google Scholar] [CrossRef] [Green Version]
- Nikayin, S.; Rabiee, A.; Hashem, M.D.; Huang, M.; Bienvenu, O.J.; Turnbull, A.E.; Needham, D.M. Anxiety symptoms in survivors of critical illness: A systematic review and meta-analysis. Gen. Hosp. Psychiatry 2016, 43, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Rabiee, A.; Nikayin, S.; Hashem, M.D.; Huang, M.; Dinglas, V.D.; Bienvenu, O.J.; Turnbull, A.E.; Needham, D.M. Depressive symptoms after critical illness: A systematic review and meta-analysis. Crit. Care Med. 2016, 44, 1744–1753. [Google Scholar] [CrossRef]
- Righy, C.; Rosa, R.G.; da Silva, R.T.A.; Kochhann, R.; Migliavaca, C.B.; Robinson, C.C.; Teche, S.P.; Teixeira, C.; Bozza, F.A.; Falavigna, M. Prevalence of post-traumatic stress disorder symptoms in adult critical care survivors: A systematic review and meta-analysis. Crit. Care 2019, 23, 213. [Google Scholar] [CrossRef] [Green Version]
- Hatch, R.; Young, D.; Barber, V.; Griffiths, J.; Harrison, D.A.; Watkinson, P. Anxiety, Depression and Post Traumatic Stress Disorder after critical illness: A UK-wide prospective cohort study. Crit. Care 2018, 22, 310. [Google Scholar] [CrossRef] [Green Version]
- Tripathy, S.; Acharya, S.P.; Singh, S.; Patra, S.; Mishra, B.R.; Kar, N. Post traumatic stress symptoms, anxiety, and depression in patients after intensive care unit discharge—A longitudinal cohort study from a LMIC tertiary care centre. BMC Psychiatry 2020, 20, 220. [Google Scholar] [CrossRef]
- Harlan, E.A.; Miller, J.; Costa, D.K.; Fagerlin, A.; Iwashyna, T.J.; Chen, E.P.; Lipman, K.; Valley, T.S. Emotional experiences and coping strategies of family members of critically ill patients. Chest 2020, 158, 1464–1472. [Google Scholar] [CrossRef]
- Pochard, F.; Azoulay, E.; Chevret, S.; Lemaire, F.; Hubert, P.; Canoui, P.; Grassin, M.; Zittoun, R.; le Gall, J.-R.; Dhainaut, J.F.; et al. Symptoms of anxiety and depression in family members of intensive care unit patients: Ethical hypothesis regarding decision-making capacity. Crit. Care Med. 2001, 29, 1893–1897. [Google Scholar] [CrossRef]
- Azoulay, E.; Pochard, F.; Kentish-Barnes, N.; Chevret, S.; Aboab, J.; Adrie, C.; Annane, D.; Bleichner, G.; Bollaert, P.E.; Darmon, M.; et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am. J. Respir. Crit. Care Med. 2005, 171, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Khandelwal, N.; Hough, C.L.; Downey, L.; Engelberg, R.A.; Carson, S.S.; White, D.B.; Kahn, J.M.; Jones, D.M.; Key, M.D.; Reagan, W.; et al. Prevalence, risk factors, and outcomes of financial stress in survivors of critical illness. Crit. Care Med. 2018, 46, e530–e539. [Google Scholar] [CrossRef]
- Mikkelsen, M.E.; Still, M.; Anderson, B.J.; Bienvenu, O.J.; Brodsky, M.B.; Brummel, N.; Butcher, B.; Clay, A.S.; Felt, H.; Ferrante, L.E.; et al. Society of critical care medicine’s international consensus conference on prediction and identification of long-term impairments after critical illness. Crit. Care Med. 2020, 48, 1670–1679. [Google Scholar] [CrossRef]
- Turan, Z.; Topaloglu, M.; Ozyemisci Taskiran, O. Medical Research Council-sumscore: A tool for evaluating muscle weakness in patients with post-intensive care syndrome. Crit. Care 2020, 24, 562. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Kawasaki, A.; Suzuki, N.; Hosoi, S.; Fujita, T.; Hachisu, S.; Nakano, H.; Naraba, H.; Mochizuki, M.; Takahashi, Y. Grip strength correlates with mental health and quality of life after critical care: A retrospective study in a post-intensive care syndrome clinic. J. Clin. Med. 2021, 10, 3044. [Google Scholar] [CrossRef] [PubMed]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Scanlan, J.; Borson, S. The Mini-Cog: Receiver operating characteristics with expert and naive raters. Int. J. Geriatr. Psychiatry 2001, 16, 216–222. [Google Scholar] [CrossRef]
- Koss, E.; Patterson, M.B.; Ownby, R.; Stuckey, J.C.; Whitehouse, P.J. Memory evaluation in Alzheimer’s disease. Caregivers’ appraisals and objective testing. Arch. Neurol. 1993, 50, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F. The informant questionnaire on cognitive decline in the elderly (IQCODE): A review. Int. Psychogeriatr. 2004, 16, 275–293. [Google Scholar] [CrossRef]
- Dunstan, D.A.; Scott, N.; Todd, A.K. Screening for anxiety and depression: Reassessing the utility of the Zung scales. BMC Psychiatry 2017, 17, 329. [Google Scholar] [CrossRef] [PubMed]
- Levis, B.; Sun, Y.; He, C.; Wu, Y.; Krishnan, A.; Bhandari, P.M.; Neupane, D.; Imran, M.; Brehaut, E.; Negeri, Z.; et al. Accuracy of the PHQ-2 Alone and in Combination With the PHQ-9 for Screening to Detect Major Depression: Systematic Review and Meta-analysis. JAMA 2020, 323, 2290–2300. [Google Scholar] [CrossRef]
- Bovin, M.J.; Marx, B.P.; Weathers, F.W.; Gallagher, M.W.; Rodriguez, P.; Schnurr, P.P.; Keane, T.M. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol. Assess. 2016, 28, 1379–1391. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Resource Center, Johns Hopkins University & Medicine. COVID-19 Dashboard. 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 28 August 2021).
- Meyerowitz-Katz, G.; Merone, L. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. Int. J. Infect. Dis. 2020, 101, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Anesi, G.L.; Jablonski, J.; Harhay, M.O.; Atkins, J.H.; Bajaj, J.; Baston, C.; Brennan, P.J.; Candeloro, C.L.; Catalano, L.M.; Cereda, M.F.; et al. Characteristics, outcomes, and trends of patients with COVID-19-related critical illness at a learning health system in the United States. Ann. Intern. Med. 2021, 174, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. USA 2020, 117, 11875–11877. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Caricchio, R.; Gallucci, M.; Dass, C.; Zhang, X.; Gallucci, S.; Fleece, D.; Bromberg, M.; Criner, G.J. Preliminary predictive criteria for COVID-19 cytokine storm. Ann. Rheum. Dis. 2021, 80, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Al-Ramadan, A.; Rabab’h, O.; Shah, J.; Gharaibeh, A. Acute and post-acute neurological complications of COVID-19. Neurol. Int. 2021, 13, 10. [Google Scholar] [CrossRef]
- Puelles, V.G.; Lütgehetmann, M.; Lindenmeyer, M.T.; Sperhake, J.P.; Wong, M.N.; Allweiss, L.; Chilla, S.; Heinemann, A.; Wanner, N.; Liu, S.; et al. Multiorgan and renal tropism of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Tampe, D.; Hakroush, S.; Bösherz, M.-S.; Franz, J.; Hofmann-Winkler, H.; Pöhlmann, S.; Kluge, S.; Moerer, O.; Stadelmann, C.; Ströbel, P.; et al. Urinary levels of SARS-CoV-2 nucleocapsid protein associate with risk of AKI and COVID-19 severity: A single-center observational study. Front. Med. 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Ellul, M.A.; Benjamin, L.; Singh, B.; Lant, S.; Michael, B.D.; Easton, A.; Kneen, R.; Defres, S.; Sejvar, J.; Solomon, T. Neurological associations of COVID-19. Lancet Neurol. 2020, 19, 767–783. [Google Scholar] [CrossRef]
- Saito, M.; Fujinami, Y.; Ono, Y.; Ohyama, S.; Fujioka, K.; Yamashita, K.; Inoue, S.; Kotani, J. Infiltrated regulatory T cells and Th2 cells in the brain contribute to attenuation of sepsis-associated encephalopathy and alleviation of mental impairments in mice with polymicrobial sepsis. Brain Behav. Immun. 2021, 92, 25–38. [Google Scholar] [CrossRef]
- Ono, Y.; Maejima, Y.; Saito, M.; Sakamoto, K.; Horita, S.; Shimomura, K.; Inoue, S.; Kotani, J. TAK-242, a specific inhibitor of Toll-like receptor 4 signalling, prevents endotoxemia-induced skeletal muscle wasting in mice. Sci. Rep. 2020, 10, 694. [Google Scholar] [CrossRef] [Green Version]
- Papoutsi, E.; Giannakoulis, V.G.; Xourgia, E.; Routsi, C.; Kotanidou, A.; Siempos, I.I. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: A systematic review and meta-analysis of non-randomized cohort studies. Crit. Care 2021, 25, 121. [Google Scholar] [CrossRef] [PubMed]
- Wendel Garcia, P.D.; Aguirre-Bermeo, H.; Buehler, P.K.; Alfaro-Farias, M.; Yuen, B.; David, S.; Tschoellitsch, T.; Wengenmayer, T.; Korsos, A.; Fogagnolo, A.; et al. Implications of early respiratory support strategies on disease progression in critical COVID-19: A matched subanalysis of the prospective RISC-19-ICU cohort. Crit. Care 2021, 25, 175. [Google Scholar] [CrossRef] [PubMed]
- Pappert, D.; Rossaint, R.; Slama, K.; Grüning, T.; Falke, K.J. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest 1994, 106, 1511–1516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langer, T.; Brioni, M.; Guzzardella, A.; Carlesso, E.; Cabrini, L.; Castelli, G.; Dalla Corte, F.; De Robertis, E.; Favarato, M.; Forastieri, A.; et al. Prone position in intubated, mechanically ventilated patients with COVID-19: A multi-centric study of more than 1000 patients. Crit. Care 2021, 25, 128. [Google Scholar] [CrossRef]
- Elharrar, X.; Trigui, Y.; Dols, A.-M.; Touchon, F.; Martinez, S.; Prud’homme, E.; Papazian, L. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA 2020, 323, 2336–2338. [Google Scholar] [CrossRef]
- Saeed, O.; Tatooles, A.J.; Farooq, M.; Schwartz, G.; Pham, D.T.; Mustafa, A.K.; D’Alessandro, D.; Arbol, S.; Jorde, U.P.; Gregoric, I.D.; et al. Characteristics and outcomes of patients with COVID-19 supported by extracorporeal membrane oxygenation: A retrospective multicenter study. J. Thorac. Cardiovasc. Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health anc Care Exellence. COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19. NICE Guideline [NG188]. 2020. Available online: https://www.nice.org.uk/guidance/ng188 (accessed on 28 August 2021).
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Blomberg, B.; Mohn, K.G.-I.; Brokstad, K.A.; Zhou, F.; Linchausen, D.W.; Hansen, B.-A.; Lartey, S.; Onyango, T.B.; Kuwelker, K.; Sævik, M.; et al. Long COVID in a prospective cohort of home-isolated patients. Nat. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Liu, X.; Zhou, Y.; Yu, H.; Li, R.; Zhan, Q.; Ni, F.; Fang, S.; Lu, Y.; Ding, X.; et al. 3-month, 6-month, 9-month, and 12-month respiratory outcomes in patients following COVID-19-related hospitalisation: A prospective study. Lancet Respir. Med. 2021, 9, 747–754. [Google Scholar] [CrossRef]
- Morin, L.; Savale, L.; Pham, T.; Colle, R.; Figueiredo, S.; Harrois, A.; Gasnier, M.; Lecoq, A.L.; Meyrignac, O.; Noel, N.; et al. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA 2021, 325, 1525–1534. [Google Scholar] [CrossRef]
- Martillo, M.; Dangayach, N.; Tabacof, L.; Spielman, L.A.; Dams-O’Connor, K.; Chan, C.C.; Kohli-Seth, R.; Cortes, M.; Escalon, M.X. Postintensive care syndrome in survivors of critical illness related to coronavirus disease 2019: Cohort study from a New York city critical care recovery clinic. Crit. Care Med. 2021. [Google Scholar] [CrossRef]
- van Gassel, R.J.J.; Bels, J.; Remij, L.; van Bussel, B.C.T.; Posthuma, R.; Gietema, H.A.; Verbunt, J.; van der Horst, I.C.C.; Olde Damink, S.W.M.; van Santen, S.; et al. Functional outcomes and their association with physical performance in mechanically ventilated coronavirus disease 2019 survivors at 3 months following hospital discharge: A cohort study. Crit. Care Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Mongodi, S.; Salve, G.; Tavazzi, G.; Politi, P.; Mojoli, F. High prevalence of acute stress disorder and persisting symptoms in ICU survivors after COVID-19. Intensive Care Med. 2021, 47, 616–618. [Google Scholar] [CrossRef]
- Ramani, C.; Davis, E.M.; Kim, J.S.; Provencio, J.J.; Enfield, K.B.; Kadl, A. Post-ICU COVID-19 outcomes: A case series. Chest 2021, 159, 215–218. [Google Scholar] [CrossRef] [PubMed]
- Prével, R.; Coelho, J.; Orieux, A.; Philip, P.; Gruson, D.; Bioulac, S. Psychological evaluation and support in COVID-19 critically ill patients: A feasibility study. Crit. Care 2021, 25, 218. [Google Scholar] [CrossRef]
- Sahashi, Y.; Endo, H.; Sugimoto, T.; Nabeta, T.; Nishizaki, K.; Kikuchi, A.; Matsumoto, S.; Sato, H.; Goto, T.; Hasegawa, K.; et al. Worries and concerns among healthcare workers during the coronavirus 2019 pandemic: A web-based cross-sectional survey. Humanit. Soc. Sci. Commun. 2021, 8, 41. [Google Scholar] [CrossRef]
- Li, Y.; Scherer, N.; Felix, L.; Kuper, H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246454. [Google Scholar] [CrossRef]
- Hennein, R.; Mew, E.J.; Lowe, S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS ONE 2021, 16, e0246602. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Di Lorenzo, G.; Di Marco, A.; Siracusano, A.; Rossi, A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open 2020, 3, e2010185. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Pun, B.T.; Balas, M.C.; Barnes-Daly, M.A.; Thompson, J.L.; Aldrich, J.M.; Barr, J.; Byrum, D.; Carson, S.S.; Devlin, J.W.; Engel, H.J.; et al. Caring for critically ill patients with the ABCDEF bundle: Results of the ICU liberation collaborative in over 15,000 adults. Crit. Care Med. 2019, 47, 3–14. [Google Scholar] [CrossRef]
- Liu, K.; Nakamura, K.; Katsukawa, H.; Elhadi, M.; Nydahl, P.; Ely, E.W.; Kudchadkar, S.R.; Takahashi, K.; Inoue, S.; Lefor, A.K.; et al. ABCDEF bundle and supportive ICU practices for patients with coronavirus disease 2019 infection: An international point prevalence study. Crit. Care Explor. 2021, 3, e0353. [Google Scholar] [CrossRef] [PubMed]
- Vranas, K.C.; Golden, S.E.; Mathews, K.S.; Schutz, A.; Valley, T.S.; Duggal, A.; Seitz, K.P.; Chang, S.Y.; Nugent, S.; Slatore, C.G.; et al. The Influence of the COVID-19 pandemic on ICU organization, care processes, and frontline clinician experiences: A qualitative study. Chest 2021. [Google Scholar] [CrossRef] [PubMed]
- Parry, S.M.; Nydahl, P.; Needham, D.M. Implementing early physical rehabilitation and mobilisation in the ICU: Institutional, clinician, and patient considerations. Intensive Care Med. 2018, 44, 470–473. [Google Scholar] [CrossRef]
- Tyson, S.F.; Greenhalgh, J.; Long, A.F.; Flynn, R. The influence of objective measurement tools on communication and clinical decision making in neurological rehabilitation. J. Eval. Clin. Pract. 2012, 18, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Schaller, S.J.; Anstey, M.; Blobner, M.; Edrich, T.; Grabitz, S.D.; Gradwohl-Matis, I.; Heim, M.; Houle, T.; Kurth, T.; Latronico, N.; et al. Early, goal-directed mobilisation in the surgical intensive care unit: A randomised controlled trial. Lancet 2016, 388, 1377–1388. [Google Scholar] [CrossRef]
- Simonelli, C.; Paneroni, M.; Fokom, A.G.; Saleri, M.; Speltoni, I.; Favero, I.; Garofali, F.; Scalvini, S.; Vitacca, M. How the COVID-19 infection tsunami revolutionized the work of respiratory physiotherapists: An experience from Northern Italy. Monaldi Arch. Chest Dis. 2020, 90. [Google Scholar] [CrossRef] [PubMed]
- Chhina, A.K.; Loyd, G.E.; Szymanski, T.J.; Nowak, K.A.; Peruzzi, W.T.; Yeldo, N.S.; Han, X.; Kerzabi, L.S.; Galusca, D.M.; Cazacu, S.; et al. Frequency and analysis of unplanned extubation in coronavirus disease 2019 patients. Crit. Care Explor. 2020, 2, e0291. [Google Scholar] [CrossRef] [PubMed]
- Balakrishna, A.; Walsh, E.C.; Hamidi, A.; Berg, S.; Austin, D.; Pino, R.M.; Hanidziar, D.; Chang, M.G.; Bittner, E.A. An examination of sedation requirements and practices for mechanically ventilated critically ill patients with COVID-19. Am. J. Health Syst. Pharm. 2021. [Google Scholar] [CrossRef]
- Hanidziar, D.; Bittner, E.A. Sedation of mechanically ventilated COVID-19 patients: Challenges and special considerations. Anesth. Analg. 2020, 131, e40–e41. [Google Scholar] [CrossRef]
- Pun, B.T.; Badenes, R.; Heras La Calle, G.; Orun, O.M.; Chen, W.; Raman, R.; Simpson, B.K.; Wilson-Linville, S.; Hinojal Olmedillo, B.; Vallejo de la Cueva, A.; et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): A multicentre cohort study. Lancet Respir. Med. 2021, 9, 239–250. [Google Scholar] [CrossRef]
- Helms, J.; Kremer, S.; Merdji, H.; Schenck, M.; Severac, F.; Clere-Jehl, R.; Studer, A.; Radosavljevic, M.; Kummerlen, C.; Monnier, A.; et al. Delirium and encephalopathy in severe COVID-19: A cohort analysis of ICU patients. Crit. Care 2020, 24, 491. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Williams Roberson, S.; Wilson, J.E.; Dabrowski, W.; Pun, B.T.; Ely, E.W. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care 2020, 24, 176. [Google Scholar] [CrossRef] [PubMed]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, Immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef] [Green Version]
- Donovan, A.L.; Aldrich, J.M.; Gross, A.K.; Barchas, D.M.; Thornton, K.C.; Schell-Chaple, H.M.; Gropper, M.A.; Lipshutz, A.K.M. Interprofessional care and teamwork in the ICU. Crit. Care Med. 2018, 46, 980–990. [Google Scholar] [CrossRef] [PubMed]
- Bruyneel, A.; Gallani, M.C.; Tack, J.; d’Hondt, A.; Canipel, S.; Franck, S.; Reper, P.; Pirson, M. Impact of COVID-19 on nursing time in intensive care units in Belgium. Intensive Crit. Care Nurs. 2021, 62, 102967. [Google Scholar] [CrossRef]
- Floris, L.; Madeddu, A.; Deiana, V.; Pasero, D.; Terragni, P. The use of the ICU diary during the COVID-19 pandemic as a tool to enhance critically ill patient recovery. Minerva Anestesiol. 2021, 87, 490–491. [Google Scholar] [CrossRef]
- Van Aerde, N.; Van den Berghe, G.; Wilmer, A.; Gosselink, R.; Hermans, G.; Meersseman, P.; Gunst, J.; Aerts, V.; Balthazar, T.; Barbé, A.; et al. Intensive care unit acquired muscle weakness in COVID-19 patients. Intensive Care Med. 2020, 46, 2083–2085. [Google Scholar] [CrossRef]
- Curci, C.; Pisano, F.; Bonacci, E.; Camozzi, D.M.; Ceravolo, C.; Bergonzi, R.; De Franceschi, S.; Moro, P.; Guarnieri, R.; Ferrillo, M.; et al. Early rehabilitation in post-acute COVID-19 patients: Data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur. J. Phys. Rehabil. Med. 2020, 56, 633–641. [Google Scholar] [CrossRef]
- Belli, S.; Balbi, B.; Prince, I.; Cattaneo, D.; Masocco, F.; Zaccaria, S.; Bertalli, L.; Cattini, F.; Lomazzo, A.; Dal Negro, F.; et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived hospitalisation. Eur. Respir. J. 2020, 56, 2002096. [Google Scholar] [CrossRef] [PubMed]
- Li, J. Rehabilitation management of patients with COVID-19: Lessons learned from the first experience in China. Eur. J. Phys. Rehabil. Med. 2020, 56, 335–338. [Google Scholar] [CrossRef]
- McWilliams, D.; Weblin, J.; Hodson, J.; Veenith, T.; Whitehouse, T.; Snelson, C. Rehabilitation levels in patients with COVID-19 admitted to intensive care requiring invasive ventilation. An observational study. Ann. Am. Thorac. Soc. 2021, 18, 122–129. [Google Scholar] [CrossRef]
- Lazzeri, M.; Lanza, A.; Bellini, R.; Bellofiore, A.; Cecchetto, S.; Colombo, A.; D’Abrosca, F.; Del Monaco, C.; Gaudiello, G.; Paneroni, M.; et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: A position paper of the Italian association of respiratory physiotherapists (ARIR). Monaldi Arch. Chest Dis. 2020, 90. [Google Scholar] [CrossRef] [PubMed]
- Chanques, G.; Constantin, J.M.; Devlin, J.W.; Ely, E.W.; Fraser, G.L.; Gélinas, C.; Girard, T.D.; Guérin, C.; Jabaudon, M.; Jaber, S.; et al. Analgesia and sedation in patients with ARDS. Intensive Care Med. 2020, 46, 2342–2356. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Nakano, H.; Naraba, H.; Mochizuki, M.; Hashimoto, H. Early rehabilitation with dedicated use of belt-type electrical muscle stimulation for severe COVID-19 patients. Crit. Care 2020, 24, 342. [Google Scholar] [CrossRef]
- de Andrade-Junior, M.C.; de Salles, I.C.D.; de Brito, C.M.M.; Pastore-Junior, L.; Righetti, R.F.; Yamaguti, W.P. Skeletal muscle wasting and function impairment in intensive care patients with severe COVID-19. Front. Physiol. 2021, 12, 640973. [Google Scholar] [CrossRef]
- Rives-Lange, C.; Zimmer, A.; Merazka, A.; Carette, C.; Martins-Bexinga, A.; Hauw-Berlemont, C.; Guerot, E.; Jannot, A.S.; Diehl, J.L.; Czernichow, S.; et al. Evolution of the nutritional status of COVID-19 critically-ill patients: A prospective observational study from ICU admission to three months after ICU discharge. Clin. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- El Moheb, M.; Naar, L.; Christensen, M.A.; Kapoen, C.; Maurer, L.R.; Farhat, M.; Kaafarani, H.M.A. Gastrointestinal complications in critically ill patients with and without COVID-19. JAMA 2020, 324, 1899–1901. [Google Scholar] [CrossRef] [PubMed]
- Martindale, R.; Patel, J.J.; Taylor, B.; Arabi, Y.M.; Warren, M.; McClave, S.A. Nutrition therapy in critically ill patients with coronavirus disease 2019. J. Parenter. Enteral. Nutr. 2020, 44, 1174–1184. [Google Scholar] [CrossRef] [PubMed]
- Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Krznaric, Z.; Nitzan, D.; Pirlich, M.; Singer, P. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020, 39, 1631–1638. [Google Scholar] [CrossRef]
- Chapple, L.S.; Fetterplace, K.; Asrani, V.; Burrell, A.; Cheng, A.C.; Collins, P.; Doola, R.; Ferrie, S.; Marshall, A.P.; Ridley, E.J. Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID-19) in Australia and New Zealand. Nutr. Diet. 2020, 77, 426–436. [Google Scholar] [CrossRef]
- Gobbi, M.; Brunani, A.; Arreghini, M.; Baccalaro, G.; Dellepiane, D.; La Vela, V.; Lucchetti, E.; Barbaglia, M.; Cova, A.; Fornara, E.; et al. Nutritional status in post SARS-Cov2 rehabilitation patients. Clin. Nutr. 2021. [Google Scholar] [CrossRef]
- Kandori, K.; Okada, Y.; Ishii, W.; Narumiya, H.; Maebayashi, Y.; Iizuka, R. Association between visitation restriction during the COVID-19 pandemic and delirium incidence among emergency admission patients: A single-center retrospective observational cohort study in Japan. J. Intensive Care 2020, 8, 90. [Google Scholar] [CrossRef]
- Cattelan, J.; Castellano, S.; Merdji, H.; Audusseau, J.; Claude, B.; Feuillassier, L.; Cunat, S.; Astrié, M.; Aquin, C.; Buis, G.; et al. Psychological effects of remote-only communication among reference persons of ICU patients during COVID-19 pandemic. J. Intensive Care 2021, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Beck, K.; Vincent, A.; Becker, C.; Keller, A.; Cam, H.; Schaefert, R.; Reinhardt, T.; Sutter, R.; Tisljar, K.; Bassetti, S.; et al. Prevalence and factors associated with psychological burden in COVID-19 patients and their relatives: A prospective observational cohort study. PLoS ONE 2021, 16, e0250590. [Google Scholar] [CrossRef]
- Cortez, C.; Mansour, O.; Qato, D.M.; Stafford, R.S.; Alexander, G.C. Changes in short-term, long-term, and preventive care delivery in US office-based and telemedicine visits during the COVID-19 pandemic. JAMA Health Forum 2021, 2, e211529. [Google Scholar] [CrossRef]
- Rose, L.; Yu, L.; Casey, J.; Cook, A.; Metaxa, V.; Pattison, N.; Rafferty, A.M.; Ramsay, P.; Saha, S.; Xyrichis, A.; et al. Communication and virtual visiting for families of patients in intensive care during COVID-19: A UK national survey. Ann. Am. Thorac Soc. 2021. [Google Scholar] [CrossRef] [PubMed]
- Sasangohar, F.; Dhala, A.; Zheng, F.; Ahmadi, N.; Kash, B.; Masud, F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: An interview study and sentiment analysis. BMJ Qual. Saf. 2020, 30, 715–721. [Google Scholar] [CrossRef]
- Mercadante, S.; Adile, C.; Ferrera, P.; Giuliana, F.; Terruso, L.; Piccione, T. Palliative care in the time of COVID-19. J. Pain Symptom Manag. 2020, 60, e79–e80. [Google Scholar] [CrossRef]
- Rovere Querini, P.; De Lorenzo, R.; Conte, C.; Brioni, E.; Lanzani, C.; Yacoub, M.R.; Chionna, R.; Martinenghi, S.; Vitali, G.; Tresoldi, M.; et al. Post-COVID-19 follow-up clinic: Depicting chronicity of a new disease. Acta Biomed. 2020, 91, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Walter, K. An inside look at a post–COVID-19 clinic. JAMA 2021, 325, 2036–2037. [Google Scholar] [CrossRef] [PubMed]
- Scheunemann, L.P.; Girard, T.D. Advancing telehealth-based screening for postintensive care syndrome: A coronavirus disease 2019 paradigm shift. Crit. Care Med. 2021. [Google Scholar] [CrossRef]
- Haines, K.J.; McPeake, J.; Hibbert, E.; Boehm, L.M.; Aparanji, K.; Bakhru, R.N.; Bastin, A.J.; Beesley, S.J.; Beveridge, L.; Butcher, B.W.; et al. Enablers and barriers to implementing ICU follow-up clinics and peer support groups following critical illness: The thrive collaboratives. Crit. Care Med. 2019, 47, 1194–1200. [Google Scholar] [CrossRef]
- Fernando, S.M.; Qureshi, D.; Sood, M.M.; Pugliese, M.; Talarico, R.; Myran, D.T.; Herridge, M.S.; Needham, D.M.; Rochwerg, B.; Cook, D.J.; et al. Suicide and self-harm in adult survivors of critical illness: Population based cohort study. BMJ 2021, 373, n973. [Google Scholar] [CrossRef] [PubMed]
- Hirshberg, E.L.; Wilson, E.L.; Stanfield, V.; Kuttler, K.G.; Majercik, S.; Beesley, S.J.; Orme, J.; Hopkins, R.O.; Brown, S.M. Impact of critical illness on resource utilization: A comparison of use in the year before and after ICU admission. Crit. Care Med. 2019, 47, 1497–1504. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.J.; Otusanya, O.; Gershengorn, H.B.; Hope, A.A.; Dayton, C.; Levi, D.; Garcia, M.; Prince, D.; Mills, M.; Fein, D.; et al. Staged implementation of awakening and breathing, coordination, delirium monitoring and management, and early mobilization bundle improves patient outcomes and reduces hospital costs. Crit. Care Med. 2019, 47, 885–893. [Google Scholar] [CrossRef]
- Snell, K.P.; Beiter, C.L.; Hall, E.L.; Junod, A.S.; Wilson, B.J.; Lepone, D.K.; McIntyre, J.R.; Swartz, D.P.; Berger, A.L.; Kirchner, H.L.; et al. A novel approach to ICU survivor care: A population health quality improvement project. Crit. Care Med. 2020, 48, e1164–e1170. [Google Scholar] [CrossRef]


| Category | Methods | Contents | Score Range | Cut-Off Value | Ref. | |
|---|---|---|---|---|---|---|
| Physical | Muscle strength | MRC score | MMT in 12 points | 12–60 | ICU-AW (<48) | [29] |
| Grip strength | - | - | - | [30] | ||
| Physical function | 6-min walk test | Walking distance for 6 min | - | Relative score to standard value | [9,28] | |
| EQ-5D-5L | 5 levels of severity for 5 items | 0–1 | Different values in countries | [28] | ||
| SF-36 | 36 items | 0–100 | Score change (≥10) | [5] | ||
| Barthel index | ADL scale in 10 items | 0–100 | ADL independence (<85) | |||
| FIM | 13 items | 13–91 | - | |||
| Cognitive | Dementia | MoCA test | 8 items | 0–30 | Mild (18–25), moderate (10–17), severe (<10) | [15,28] |
| MMSE | 11 items | 0–30 | Mild (<24), moderate (<20), severe (<10) | [31] | ||
| Mini-Cog | 3 item recall and clock drawing | 0–5 | Cognitive dysfunction (≤2) | [32] | ||
| SMQ | 14 items | 4–46 | <40 | [33] | ||
| IQCODE | 26 items | 0–3 | ≥1 | [34] | ||
| Mental health | Anxiety & depression | HADS | 14 items | 0–14 | ≥8 | [28] |
| SAS and SDS | 20 items | 20–80 | Anxiety (>45), depression: mild (45–59), Moderate (60–69), severe (70–80) | [35] | ||
| Depression | PHQ-9 | 9 items | 0–27 | ≥10 | [36] | |
| PHQ-2 | 2 items | 0–6 | ≥2 | [36] | ||
| PTSD | IES-R | 22 items | 0–4 (average) | >1.6 at average | [28] | |
| IES-6 | 6 items | 0–4 (average) | >1.75 at average | [28] | ||
| PCL-5 | 20 items | 0–80 | ≥31–33 | [37] |
| Author Location Journal | Population Assessment after Hospital Discharge | Physical Impairments | Cognitive Impairments | Mental Health Problems | Ref. |
|---|---|---|---|---|---|
| COMEBAC France JAMA. 2021 | 94 patients 4 months | ICU-related neuromyopathy: 28% (14/51) | Anxiety (HADS): 23.4% (22/94) Depression (BDI test): 18.1% (17/94) PTSD (PCL-5): 7.4% (7/94) | [62] | |
| Mongodi et al. Italy ICM. 2021 | 47 patients at least 1 month | Acute stress disorder (IES-R): 40.4% (19/47) | [65] | ||
| Martillo et al. US CCM. 2021 | 45 patients (ICU stay ≥ 7 days) 1 month | Various measures †: 86.7% (39/45) | T-MoCA: 20.0% (6/30) | Anxiety/depression (EQ-5D-3L): 43.2% (19/44) Depression (PHQ-9): 40.5% (17/42) PTSD (PCL-5): 19.0% (8/42) | [63] |
| Ramani et al. US CHEST. 2021 | 28 patients 6 weeks | MoCA: 57.1% (16/28) | Depression (PROMIS Depression 8a T Score): 25.0% (7/28) | [66] | |
| Prèvel et al. France CC. 2021 | 37 patients 6 months | Anxiety (HADS): 22.2% (4/18) Depression (HADS): 10.5% (2/19) PTSD (PCL-5): 5.6% (1/18) | [67] | ||
| van Gassel et al. Netherlands CCM. 2021 | 46 patients 3 month | 6-min walking test < 80%: 48% (22/46) | [64] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakanishi, N.; Liu, K.; Kawakami, D.; Kawai, Y.; Morisawa, T.; Nishida, T.; Sumita, H.; Unoki, T.; Hifumi, T.; Iida, Y.; et al. Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives. J. Clin. Med. 2021, 10, 3870. https://doi.org/10.3390/jcm10173870
Nakanishi N, Liu K, Kawakami D, Kawai Y, Morisawa T, Nishida T, Sumita H, Unoki T, Hifumi T, Iida Y, et al. Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives. Journal of Clinical Medicine. 2021; 10(17):3870. https://doi.org/10.3390/jcm10173870
Chicago/Turabian StyleNakanishi, Nobuto, Keibun Liu, Daisuke Kawakami, Yusuke Kawai, Tomoyuki Morisawa, Takeshi Nishida, Hidenori Sumita, Takeshi Unoki, Toru Hifumi, Yuki Iida, and et al. 2021. "Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives" Journal of Clinical Medicine 10, no. 17: 3870. https://doi.org/10.3390/jcm10173870
APA StyleNakanishi, N., Liu, K., Kawakami, D., Kawai, Y., Morisawa, T., Nishida, T., Sumita, H., Unoki, T., Hifumi, T., Iida, Y., Katsukawa, H., Nakamura, K., Ohshimo, S., Hatakeyama, J., Inoue, S., & Nishida, O. (2021). Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives. Journal of Clinical Medicine, 10(17), 3870. https://doi.org/10.3390/jcm10173870








