Multi-Institutional Study of Dorsal Onlay Urethroplasty of the Membranous Urethra after Endoscopic Prostate Procedures: Operative Results, Continence, Erectile Function and Patient Reported Outcomes
Abstract
:1. Introduction
2. Materials and Methods
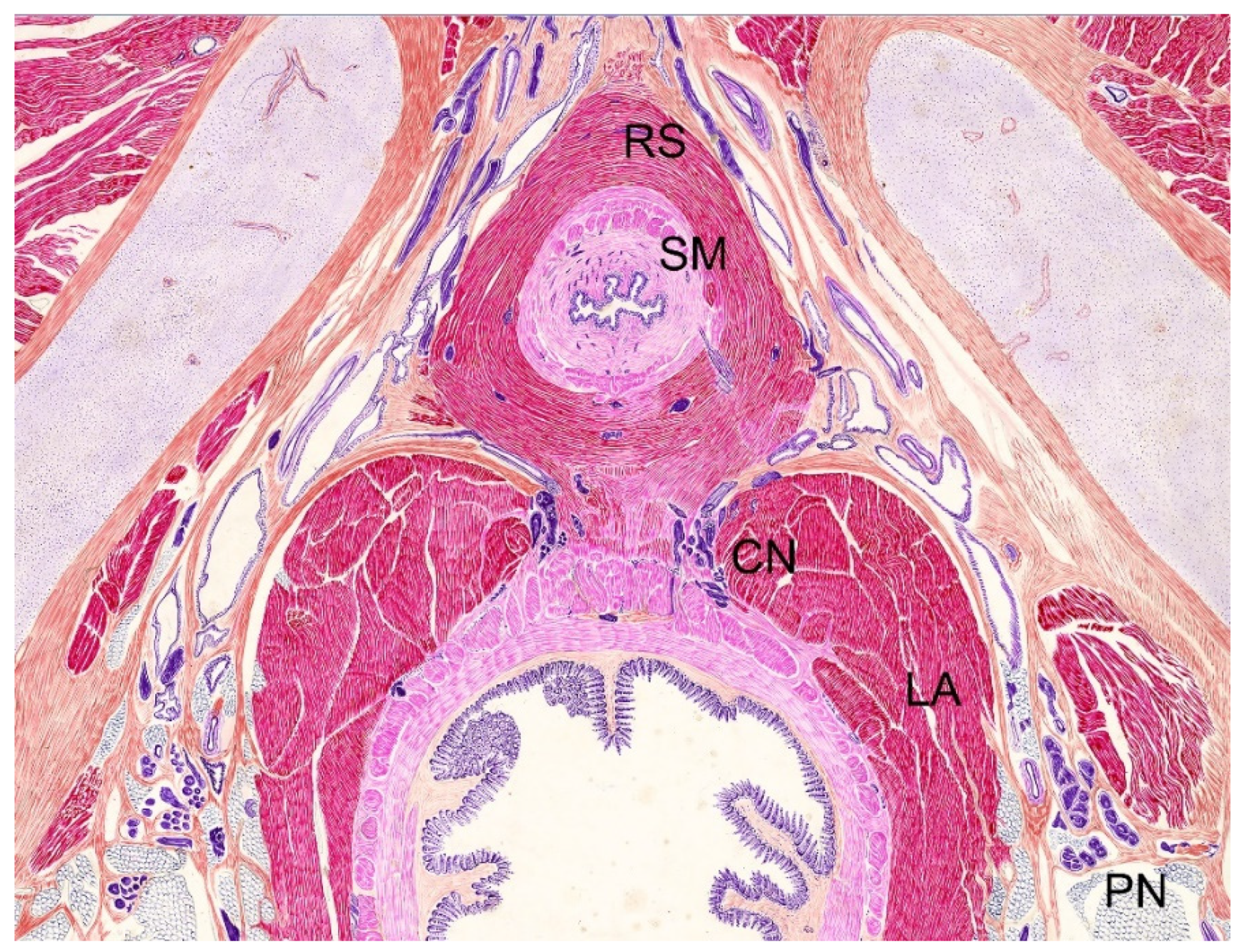
2.1. Surgical Technique
2.2. Follow-Up
2.3. Patient-Reported Outcomes
2.4. Incontinence
2.5. Statistical Analysis
3. Results
3.1. Patency Outcomes
3.2. Clinical Outcomes (Uroflow, PVR, IPSS)
3.3. Continence Outcomes
3.4. Sexual Function Outcomes
3.5. Global Response Assessment Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rassweiler, J.; Teber, D.; Kuntz, R.; Hofmann, R. Complications of Transurethral Resection of the Prostate (TURP)—Incidence, Management, and Prevention. Eur. Urol. 2006, 50, 969–980. [Google Scholar] [CrossRef]
- Mamoulakis, C.; Ubbink, D.T.; de la Rosette, J.J. Bipolar versus Monopolar Transurethral Resection of the Prostate: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Eur. Urol. 2009, 56, 798–809. [Google Scholar] [CrossRef]
- Gravas, S.; Cornu, J.N.; Gacci, M.; Gratzke, C.; Herrmann, T.R.W.; Mamoulakis, C.; Rieken, M.; Speakman, M.J.; Tikkinen, K.A.O.; Karavitakis, M.; et al. EAU Guidelines on Management of Non-Neurogenic Male Lowr Urinary Tract Symptoms (LUTS), Including Benign Prostatic Obstruction (BPO); European Association of Urology, EAU Guidelines Office: Arnhem, The Netherlands, 2019; Available online: https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/ (accessed on 23 August 2021).
- Tascı, A.I.; Ilbey, Y.O.; Tugcu, V.; Cicekler, O.; Cevik, C.; Zoroglu, F. Transurethral resection of the prostate with monopolar resecto-scope: Single-surgeon experience and long-term results of after 3589 procedures. Urology 2011, 78, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Li, J.; Pu, C.; Bai, Y.; Yuan, H.; Wei, Q.; Han, P. Bipolar Transurethral Resection Versus Monopolar Transurethral Resection for Benign Prostatic Hypertrophy: A Systematic Review and Meta-Analysis. J. Endourol. 2014, 28, 1107–1114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komura, K.; Inamoto, T.; Takai, T.; Uchimoto, T.; Saito, K.; Tanda, N.; Minami, K.; Oide, R.; Uehara, H.; Takahara, K.; et al. Incidence of urethral stricture after bipolar transurethral resection of the prostate using TURis: Results from a randomised trial. BJU Int. 2015, 115, 644–652. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.-W.; Man, L.-B. Transurethral resection of the prostate stricture management. Asian J. Androl. 2020, 22, 140–144. [Google Scholar] [CrossRef]
- Angulo, J.C.; Gómez, R.G.; Nikolavsky, D. Reconstruction of Membranous Urethral Strictures. Curr. Urol. Rep. 2018, 19, 37. [Google Scholar] [CrossRef]
- Kulkarni, S.B.; Joglekar, O.; Alkandari, M.; Joshi, P.M. Management of post TURP strictures. World J. Urol. 2018, 37, 589–594. [Google Scholar] [CrossRef]
- Mundy, A.R. The Treatment of Sphincter Strictures. BJU Int. 1989, 64, 626–628. [Google Scholar] [CrossRef]
- Hofer, M.D.; Zhao, L.C.; Morey, A.F.; Scott, J.F.; Chang, A.J.; Brandes, S.B.; Gonzalez, C.M. Outcomes after Urethroplasty for Radiotherapy Induced Bulbomembranous Urethral Stricture Disease. J. Urol. 2014, 191, 1307–1312. [Google Scholar] [CrossRef]
- Rourke, K.; Kinnaird, A.; Zorn, J. Observations and outcomes of urethroplasty for bulbomembranous stenosis after radiation therapy for prostate cancer. World J. Urol. 2016, 34, 377–382. [Google Scholar] [CrossRef]
- Chung, P.H.; Esposito, P.; Wessells, H.; Voelzke, B.B. Incidence of stress urinary incontinence after posterior urethroplasty for ra-diation-induced urethral strictures. Urology 2018, 114, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Gimbernat, H.; Arance, I.; Redondo, C.; Meilan, E.; Andres, G.; Angulo, J.C. Treatment for long bulbar urethral strictures with membranous involvement using urethroplasty with oral mucosa graft. Actas Urol. Esp. 2014, 38, 544–551. [Google Scholar] [CrossRef]
- Barbagli, G.; Kulkarni, S.B.; Joshi, P.M.; Nikolavsky, D.; Montorsi, F.; Sansalone, S.; Loreto, C.; Lazzeri, M. Repair of sphincter urethral strictures pre-serving urinary continence: Surgical technique and outcomes. World J. Urol. 2019, 37, 2473–2479. [Google Scholar] [CrossRef] [PubMed]
- Latini, J.M.; McAninch, J.W.; Brandes, S.B.; Chung, J.Y.; Rosenstein, D. SIU/ICUD Consultation on Urethral Strictures: Epidemiology, Etiology, Anatomy, and Nomenclature of Urethral Stenoses, Strictures, and Pelvic Fracture Urethral Disruption Injuries. Urology 2014, 83, S1–S7. [Google Scholar] [CrossRef]
- Gómez, R.G.; Velarde, L.G.; Campos, R.A.; Saavedra, A.A.; Delgado, E.J.; Santucci, R.A.; Scarberry, K.A. Intrasphincteric anastomotic urethroplasty allows preservation of continence in men with bulbomembranous urethral strictures following benign prostatic hyperplasia surgery. World J. Urol. 2020, 39, 2099–2106. [Google Scholar] [CrossRef]
- Gomez, R.G.; Scarberry, K. Anatomy and techniques in posterior urethroplasty. Transl. Androl. Urol. 2018, 7, 567–579. [Google Scholar] [CrossRef]
- Mundy, A. Urethroplasty for posterior urethral strictures. BJU Int. 1996, 78, 243–247. [Google Scholar] [CrossRef]
- Meeks, J.J.; Brandes, S.B.; Morey, A.F.; Thom, M.; Mehdiratta, N.; Valadez, C.; Granieri, M.A.; Gonzalez, C.M. Urethroplasty for Radiotherapy Induced Bulbomembranous Strictures: A Multi-Institutional Experience. J. Urol. 2011, 185, 1761–1765. [Google Scholar] [CrossRef]
- Policastro, C.G.; Simhan, J.; Martins, F.E.; Lumen, N.; Venkatesan, K.; Angulo, J.C.; Gupta, S.; Rusilko, P.; Pérez, E.A.R.; Redger, K.; et al. A multi-institutional critical assessment of dorsal onlay urethroplasty for post-radiation urethral stenosis. World J. Urol. 2020, 39, 2669–2675. [Google Scholar] [CrossRef]
- Blakely, S.; Caza, T.; Landas, S.; Nikolavsky, D. Dorsal Onlay Urethroplasty for Membranous Urethral Strictures: Urinary and Erectile Functional Outcomes. J. Urol. 2016, 195, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Favre, G.A.; Alfieri, A.G.; Gil, V.S.A.; Tobia, I.; Giudice, C.R. Bulbomembranous Urethral Strictures Repair After Surgical Treatment of Benign Prostatic Hyperplasia. Experience From a Latin American Referral Centre. Urology 2021, 147, 281–286. [Google Scholar] [CrossRef]
- Lumen, N.; Campos-Juanatey, F.; Dimitropoulos, K.; Greenwell, T.; Martins, F.E.; Osman, N.; Riechardt, S.; Waterloos, M.; Barratt, R.; Chan, G.; et al. EAU Guidelines on Urethral Stricture. Available online: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Urethral-Strictures1-2021.pdf (accessed on 23 August 2021).
- Al-Rifaei, M.A.; Zaghloul, S.; Al-Rifaei, A.M. Bulboprostatic anastomotic urethroplasty with preservation of potency: Anatomical study, operative approach and clinical results. Scand. J. Urol. Nephrol. 2005, 39, 163–168. [Google Scholar] [CrossRef]
- Hinata, N.; Murakami, G.; Miyake, H.; Abe, S.; Fujisawa, M. Histological Study of the Cavernous Nerve Mesh Outside the Periprostatic Region: Anatomical Basis for Erectile Function after Nonnerve Sparing Radical Prostatectomy. J. Urol. 2015, 193, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- Dalpiaz, O.; Mitterberger, M.; Kerschbaumer, A.; Pinggera, G.-M.; Bartsch, G.; Strasser, H. Anatomical approach for surgery of the male posterior urethra. BJU Int. 2008, 102, 1448–1451. [Google Scholar] [CrossRef]
- Barbagli, G.; Montorsi, F.; Guazzoni, G.F.; Larcher, A.; Fossati, N.; Sansalone, S.; Romano, G.; Buffi, N.; Lazzeri, M. Ventral Oral Mucosal Onlay Graft Urethroplasty in Nontraumatic Bulbar Urethral Strictures: Surgical Technique and Multivariable Analysis of Results in 214 Patients. Eur. Urol. 2013, 64, 440–447. [Google Scholar] [CrossRef]
- Ahyai, S.A.; Schmid, M.; Kuhl, M.; Kluth, L.A.; Soave, A.; Riechardt, S.; Chun, F.K.H.; Engel, O.; Fisch, M.; Dahlem, R. Outcomes of ventral onlay buccal mucosa graft urethroplasty in patients after radiotherapy. J. Urol. 2015, 194, 441–446. [Google Scholar] [CrossRef] [PubMed]

| Variables | n (%) |
|---|---|
| Age, year * | 69.1 ± 9.5 |
| Body mass index, kg/m2 * | 27.7 ± 5.1 |
| HT/CVD 1 | 44 (41.1) |
| Diabetes mellitus | 32 (29.9) |
| Active smoking 2 | 29 (27.1) |
| Race | |
| Caucasian | 81 (75.7) |
| Black | 8 (7.5) |
| Asian | 5 (4.7) |
| Latin | 13 (12.1) |
| Type of TURP 3 | |
| Monopolar TURP | 47 (44.3) |
| Bipolar TURP | 33 (31.1) |
| Greenlight laser | 16 (15.1) |
| Holmium enucleation | 9 (8.5) |
| Bladder neck incision | 2 (1.9) |
| Time from TURP to urethroplasty, month * | 24.1 ± 25 |
| Prior dilatation | |
| None | 35 (32.7) |
| One | 32 (29.9) |
| Two or more (up to 20) | 40 (37.4) |
| Prior DVIU 4 | |
| None | 66 (61.7) |
| One | 27 (25.2) |
| Two or more (up to 4) | 14 (13.1) |
| Prior urethroplasty | 3 (2.8) |
| Stricture length, cm * | 3.5 ± 1.85 |
| Concomitant involvement of anterior urethra | 27 (25.2) |
| Use of ancillary techniques | 19 (16.8%) |
| Follow-up since urethroplasty, month * | 59.3 ± 45.1 |
| Stenosis recurrence during follow-up | 10 (9.35) |
| Variables | n | Stenosis Recurrence | p Value | |
|---|---|---|---|---|
| % With | % Without | |||
| Patient age | <70 years (n = 55) | - | 66.7 | 0.339 |
| ≥70 years (n = 52) | 50 | 33.3 | ||
| HT/CVD 1 | No (n = 63) | 58.8 | 60 | 0.94 |
| Yes (n = 44) | 41.2 | 40 | ||
| Diabetes Mellitus | No (n = 75) | 73.2 | 40 | 0.029 * |
| Yes (n = 32) | 26.8 | 60 | ||
| Smoking habit | No (n = 78) | 75.3 | 50 | 0.087 * |
| Yes (n = 29) | 24.7 | 50 | ||
| Type of TURP 2 | Monopolar TURP (n = 47) | 25.9 | 63.6 | 0.049 * |
| Bipolar TURP (n = 33) | 14.7 | 27.3 | ||
| Greenlight laser (n = 16) | 0 | 0 | ||
| Holmium laser (n = 9) | 9.4 | 0 | ||
| Bladder neck incision (n = 2) | 1 | 9.1 | ||
| Radiation | No (n = 97) | 93.8 | 60 | 0.006 * |
| Yes (n = 10) | 6.2 | 40 | ||
| Prior dilatation | None or 1 (n = 67) | 66 | 30 | 0.038 * |
| More than 1 (n = 40) | 34 | 70 | ||
| Prior DVIU 3 | No (n = 41) | 36.1 | 60 | 0.069 * |
| Yes (n = 66) | 63.9 | 40 | ||
| Prior urethroplasty | No (n = 104) | 96.9 | 100 | 1 |
| Yes (n = 3) | 3.1 | 0 | ||
| Stricture length | <4 cm (n = 77) | 75.3 | 40 | 0.027 * |
| ≥4 cm (n = 30) | 24.7 | 60 | ||
| Associated anterior stenosis | No (n = 80) | 75.3 | 70 | 0.71 |
| Yes (n = 27) | 24.7 | 30 | ||
| Postoperative complications 4 | No (n = 99) | 89.7 | 60 | 0.025 * |
| Yes (n = 14) | 10.3 | 40 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angulo, J.C.; Dorado, J.F.; Policastro, C.G.; Martins, F.E.; Rourke, K.; Ramírez, E.A.; Simhan, J.; Li, E.S.; Rusilko, P.; Venkatesan, K.; et al. Multi-Institutional Study of Dorsal Onlay Urethroplasty of the Membranous Urethra after Endoscopic Prostate Procedures: Operative Results, Continence, Erectile Function and Patient Reported Outcomes. J. Clin. Med. 2021, 10, 3969. https://doi.org/10.3390/jcm10173969
Angulo JC, Dorado JF, Policastro CG, Martins FE, Rourke K, Ramírez EA, Simhan J, Li ES, Rusilko P, Venkatesan K, et al. Multi-Institutional Study of Dorsal Onlay Urethroplasty of the Membranous Urethra after Endoscopic Prostate Procedures: Operative Results, Continence, Erectile Function and Patient Reported Outcomes. Journal of Clinical Medicine. 2021; 10(17):3969. https://doi.org/10.3390/jcm10173969
Chicago/Turabian StyleAngulo, Javier C., Juan F. Dorado, Connor G. Policastro, Francisco E. Martins, Keith Rourke, Erick A. Ramírez, Jay Simhan, Eric S. Li, Paul Rusilko, Krishnan Venkatesan, and et al. 2021. "Multi-Institutional Study of Dorsal Onlay Urethroplasty of the Membranous Urethra after Endoscopic Prostate Procedures: Operative Results, Continence, Erectile Function and Patient Reported Outcomes" Journal of Clinical Medicine 10, no. 17: 3969. https://doi.org/10.3390/jcm10173969






