Epidemiologic, Postmortem Computed Tomography-Morphologic and Biomechanical Analysis of the Effects of Non-Invasive External Pelvic Stabilizers in Genuine Unstable Pelvic Injuries
Abstract
1. Introduction
2. Materials and Methods
- −
- The pneumatic pelvic sling Standard® (100 and 200 mmHg; VBM Medizintechnik GmbH, Sulz, Germany)
- −
- T-POD® (Pyng Medical, Richmond, ON, Canada)
- −
- Conventional cloth sling (bed sheet)
- −
- SAM Pelvic Sling II® (SAM Medical Products, Wilsonville, OR, USA)
- −
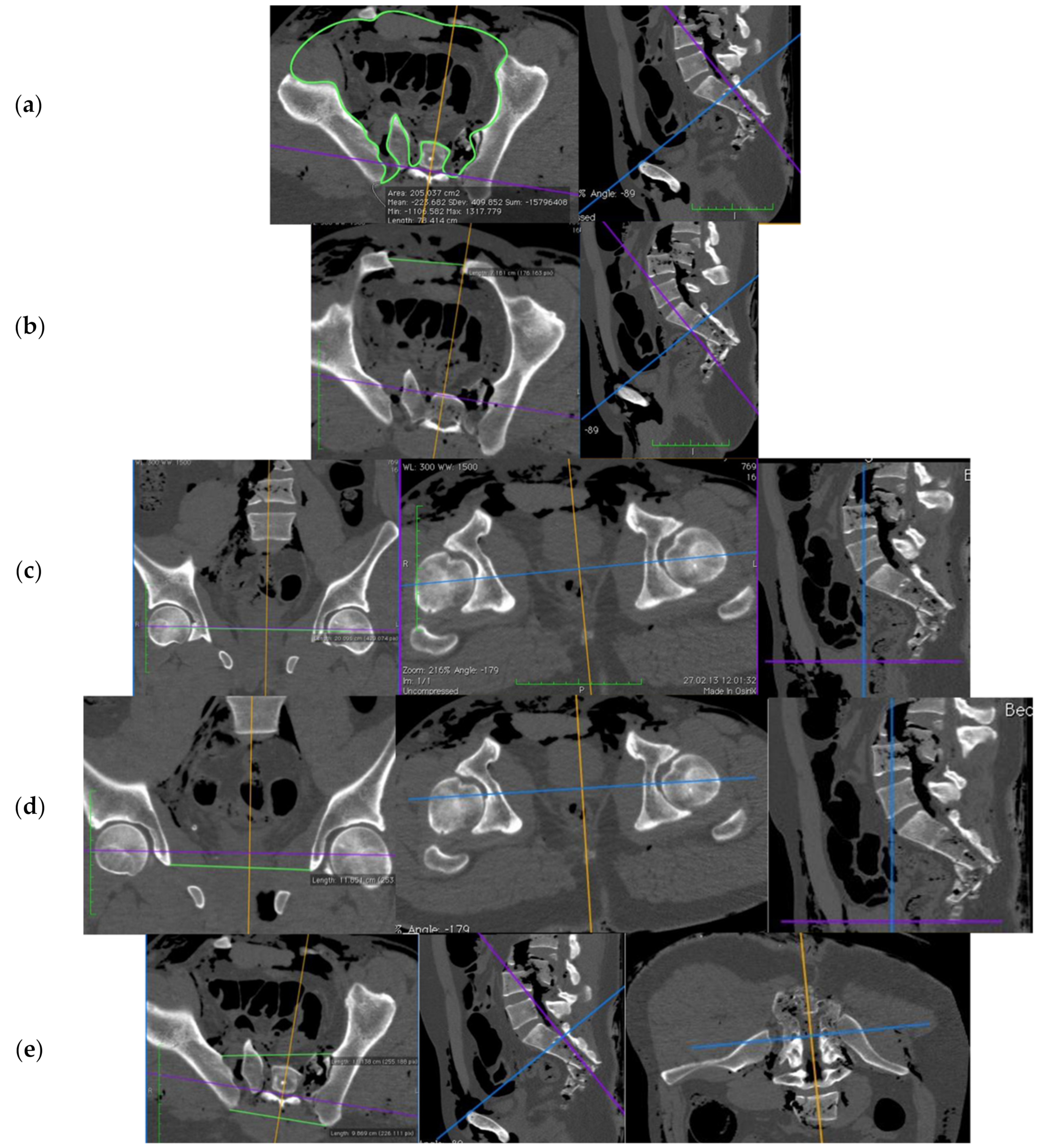
- cranial to caudal: the junction between lumbar vertebrae 4 and 5 to the caudal end of the ischiatic tuber
- −
- the area of pelvic entrance plane: the transverse plane between the lower edge of sacral vertebra 1 and the upper edge of the symphysis
- −
- the symphysis width: the point of greatest distance between the pubic bones
- −
- the femoral head distance: the distance between the centers of the femoral heads (in frontal plane)
- −
- the distance between the Köhler’s tear figures: the shortest distance between the most caudal poles (in frontal plane)
- −
- the distance between the sacroiliac joints (SIJ): the ventral portions of the SIJ space, and for the dorsal distance, the most dorsal bony border of the Os ileum.
3. Results
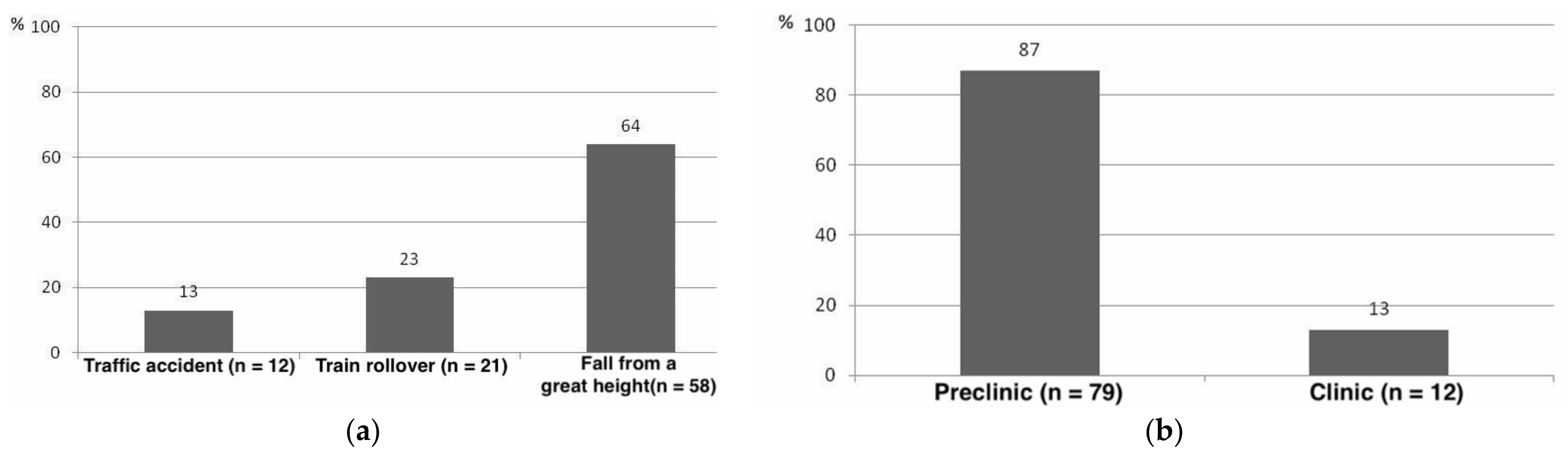
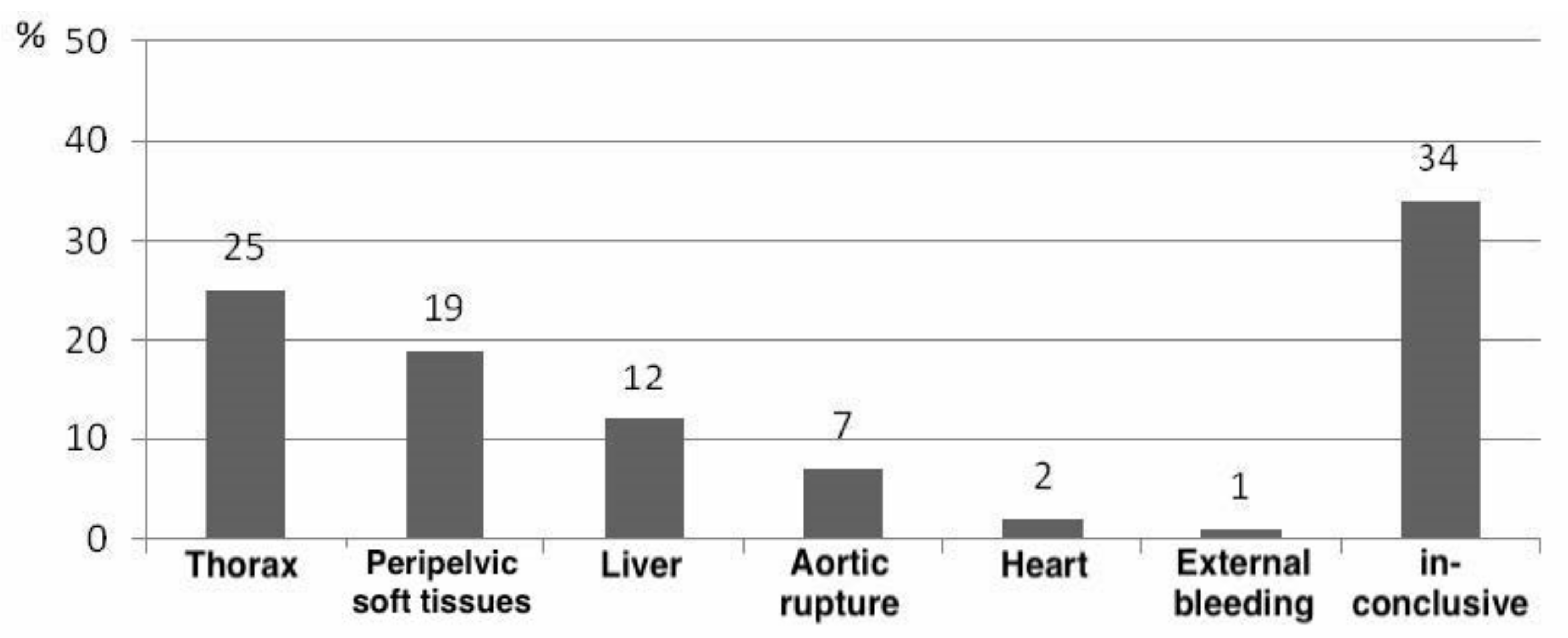
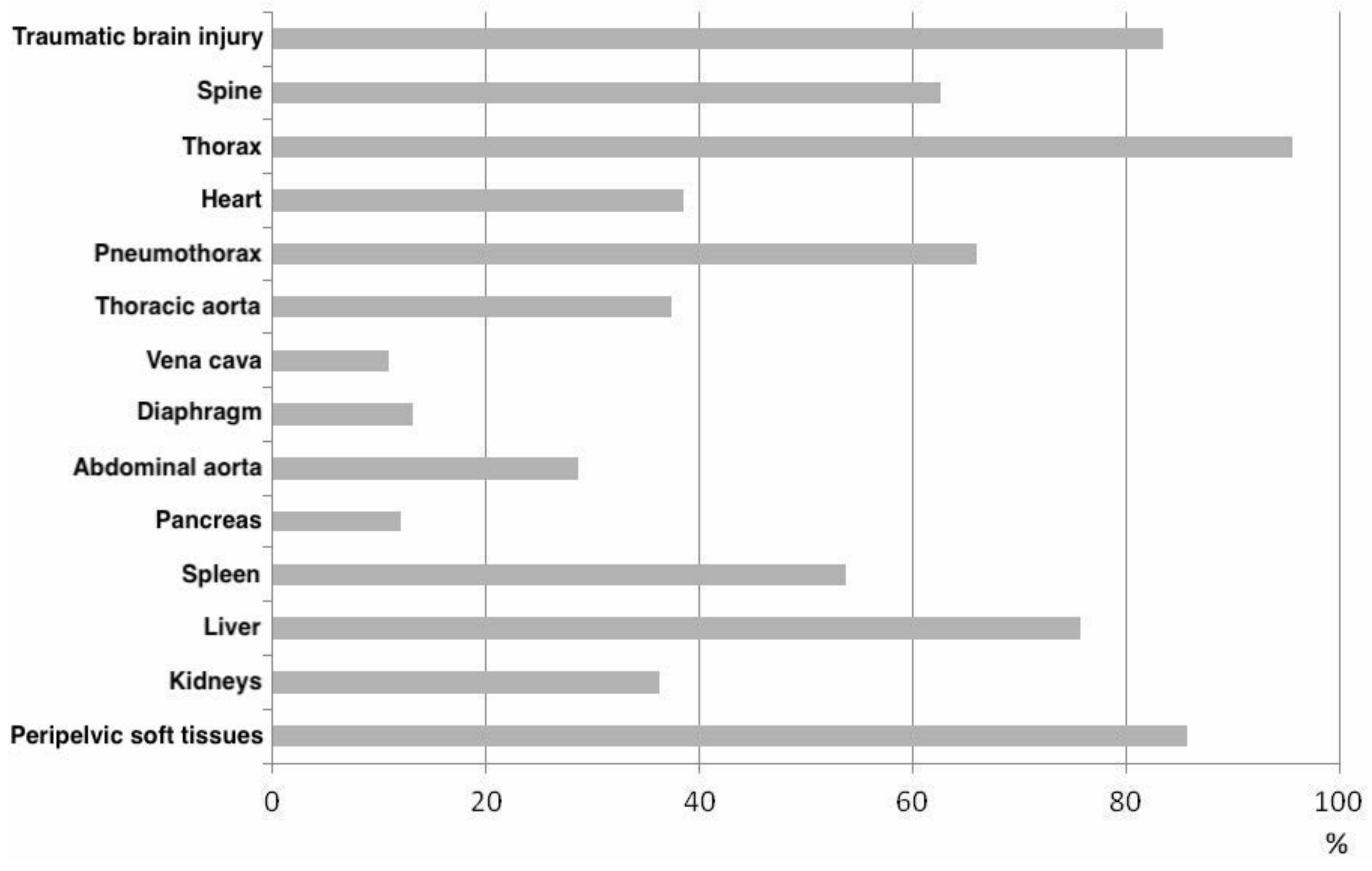
3.1. Epidemiological Data
3.2. Effects on Pelvic Bioarchitecture of External, Non-Invasive Pelvic Stabilizers
3.3. Biomechanical Force Measurement of the Acting Tensile Forces after Pelvic Stabilizer Device
4. Discussion
4.1. Epidemiology of Pelvic Trauma
4.2. “Treat First What Kills First” in Pelvic Trauma
4.3. Reproducibility of Genuine Pelvic Trauma with Artificial Pelvic Trauma Models
4.4. Effect of External Pelvic Stabilization in Real Pelvic Trauma
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Limitations
References
- Esmer, E.; Derst, P.; Schulz, M.; Siekmann, H.; Delank, K.S.; das TraumaRegister DGU®. Einfluss der externen Beckenstabilisierung bei hämodynamisch instabilen Beckenfrakturen. Unfallchirurg 2017, 120, 312–319. [Google Scholar] [CrossRef]
- Gänsslen, A.; Giannoudis, P.; Pape, H.-C. Hemorrhage in Pelvic Fracture: Who Needs Angiography? Curr. Opin. Crit. Care 2003, 9, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, M.; Parchi, P.; Digrandi, G.; Latessa, M.; Guido, G. External Fixation in Pelvic Fractures. Musculoskelet. Surg. 2010, 94, 63–70. [Google Scholar] [CrossRef]
- Bottlang, M.; Simpson, T.; Sigg, J.; Krieg, J.C.; Madey, S.M.; Long, W.B. Noninvasive Reduction of Open-Book Pelvic Fractures by Circumferential Compression. J. Orthop. Trauma 2002, 16, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.-Y.; Wu, Y.-T.; Liao, C.-H.; Kang, S.-C.; Wang, S.-Y.; Hsu, Y.-P.; Lin, B.-C.; Yuan, K.-C.; Kuo, I.-M.; Ouyang, C.-H. Pelvic Circumferential Compression Devices Benefit Patients with Pelvic Fractures Who Need Transfers. Am. J. Emerg. Med. 2013, 31, 1432–1436. [Google Scholar] [CrossRef]
- Schmal, H.; Markmiller, M.; Mehlhorn, A.T.; Sudkamp, N.P. Epidemiology and Outcome of Complex Pelvic Injury. Acta Orthop. Belg 2005, 71, 7. [Google Scholar]
- Bakhshayesh, P.; Boutefnouchet, T.; Tötterman, A. Effectiveness of Non Invasive External Pelvic Compression: A Systematic Review of the Literature. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 73. [Google Scholar] [CrossRef]
- Heetveld, M.J.; Harris, I.; Schlaphoff, G.; Sugrue, M. Guidelines for the Management of Haemodynamically Unstable Pelvic Fracture Patients. ANZ J. Surg. 2004, 74, 520–529. [Google Scholar] [CrossRef]
- Caillot, M.; Hammad, E.; Le Baron, M.; Villes, V.; Leone, M.; Flecher, X. Pelvic Fracture in Multiple Trauma: A 67-Case Series. Orthop. Traumatol. Surg. Res. 2016, 102, 1013–1016. [Google Scholar] [CrossRef]
- Geeraerts, T.; Chhor, V.; Cheisson, G.; Martin, L.; Bessoud, B.; Ozanne, A.; Duranteau, J. Clinical Review: Initial Management of Blunt Pelvic Trauma Patients with Haemodynamic Instability. Crit. Care 2007, 11, 204. [Google Scholar] [CrossRef][Green Version]
- Hak, D.J.; Smith, W.R.; Suzuki, T. Management of Hemorrhage in Life-Threatening Pelvic Fracture. J. Am. Acad. Orthop. Surg. 2009, 17, 447–457. [Google Scholar] [CrossRef]
- Jang, J.Y.; Shim, H.; Jung, P.Y.; Kim, S.; Bae, K.S. Preperitoneal Pelvic Packing in Patients with Hemodynamic Instability Due to Severe Pelvic Fracture: Early Experience in a Korean Trauma Center. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 3. [Google Scholar] [CrossRef]
- Riepl, C.; Beck, A.; Kraus, M. Präklinisches Management von Beckenverletzungen. Der Notarzt 2012, 28, 125–136. [Google Scholar] [CrossRef]
- Lee, C.; Porter, K. The Prehospital Management of Pelvic Fractures. Emerg. Med. J. 2007, 24, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Schweigkofler, U. Is There Any Benefit in the Pre-Hospital Application of Pelvic Binders in Patients with Suspected Pelvic Injuries? Eur. J. Trauma Emerg. Surg. 2021, 47, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Scott, I.; Porter, K.; Laird, C.; Greaves, I.; Bloch, M. The Prehospital Management of Pelvic Fractures: Initial Consensus Statement. Emerg. Med. J. 2013, 30, 1070–1072. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.C.T.H.; van Stigt, S.F.L.; van Vugt, A.B. Effect of a New Pelvic Stabilizer (T-POD®) on Reduction of Pelvic Volume and Haemodynamic Stability in Unstable Pelvic Fractures. Injury 2010, 41, 1239–1243. [Google Scholar] [CrossRef]
- Grimm, M.R.; Vrahas, M.S.; Thomas, K.A. Pressure-Volume Characteristics of the Intact and Disrupted Pelvic Retroperitoneum. J. Trauma Acute Care Surg. 1998, 44, 454–459. [Google Scholar] [CrossRef]
- DeAngelis, N.A.; Wixted, J.J.; Drew, J.; Eskander, M.S.; Eskander, J.P.; French, B.G. Use of the Trauma Pelvic Orthotic Device (T-POD) for Provisional Stabilisation of Anterior–Posterior Compression Type Pelvic Fractures: A Cadaveric Study. Injury 2008, 39, 903–906. [Google Scholar] [CrossRef] [PubMed]
- Knops, S.P.; Schep, N.W.L.; Spoor, C.W.; van Riel, M.P.J.M.; Spanjersberg, W.R.; Kleinrensink, G.J.; van Lieshout, E.M.M.; Patka, P.; Schipper, I.B. Comparison of Three Different Pelvic Circumferential Compression Devices: A Biomechanical Cadaver Study. JBJS 2011, 93, 230–240. [Google Scholar] [CrossRef]
- Krieg, J.; Mohr, M.; Ellis, T.; Simpson, T.; Madey, S.; Bottlang, M. Emergent Stabilization of Pelvic Ring Injuries by Controlled Circumferential Compression: A Clinical Trial. J. Trauma Inj. Infect. Crit. Care 2005, 59, 659–664. [Google Scholar] [CrossRef]
- Haussmann, M.M. Epidemiologische, Postmortale Computertomographie—Morphologische Und Biomechanische Analyse Der Effekte Nicht-Invasiver Externer Beckenstabilisatoren Bei Reellen Instabilen Beckenverletzungen. Ph.D. Thesis, Universitätsmedizin Berlin, Berlin, Germany, 2018. [Google Scholar] [CrossRef]
- Bardenheuer, M.; Obertacke, U.; Waydhas, C.; Nast-Kolb, D. Epidemiology of the severe multiple trauma-a prospective registration of preclinical and clinical supply. J. Orthop. Trauma 2000, 14, 453. [Google Scholar] [CrossRef]
- Cothren, C.C.; Moore, E.E.; Hedegaard, H.B.; Meng, K. Epidemiology of Urban Trauma Deaths: A Comprehensive Reassessment 10 Years Later. World J. Surg. 2007, 31, 1507–1511. [Google Scholar] [CrossRef] [PubMed]
- Siegmeth, A.; Müllner, T.; Kukla, C.; Vécsei, V. Begleitverletzungen beim schweren Beckentrauma. Der Unfallchirurg 2000, 103, 572–581. [Google Scholar] [CrossRef]
- Søreide, K.; Krüger, A.J.; Vårdal, A.L.; Ellingsen, C.L.; Søreide, E.; Lossius, H.M. Epidemiology and Contemporary Patterns of Trauma Deaths: Changing Place, Similar Pace, Older Face. World J. Surg. 2007, 31, 2092–2103. [Google Scholar] [CrossRef]
- Pang, J.-M.; Civil, I.; Ng, A.; Adams, D.; Koelmeyer, T. Is the Trimodal Pattern of Death after Trauma a Dated Concept in the 21st Century? Trauma Deaths in Auckland 2004. Injury 2008, 39, 102–106. [Google Scholar] [CrossRef]
- Evans, J.A.; van Wessem, K.J.P.; McDougall, D.; Lee, K.A.; Lyons, T.; Balogh, Z.J. Epidemiology of Traumatic Deaths: Comprehensive Population-Based Assessment. World J. Surg. 2010, 34, 158–163. [Google Scholar] [CrossRef]
- Gustavo Parreira, J.; Coimbra, R.; Rasslan, S.; Oliveira, A.; Fregoneze, M.; Mercadante, M. The Role of Associated Injuries on Outcome of Blunt Trauma Patients Sustaining Pelvic Fractures. Injury 2000, 31, 677–682. [Google Scholar] [CrossRef]
- Dong, J.; Zhou, D. Management and Outcome of Open Pelvic Fractures: A Retrospective Study of 41 Cases. Injury 2011, 42, 1003–1007. [Google Scholar] [CrossRef]
- Esser, M.; Gabbe, B.; de Steiger, R.; Bucknill, A.; Russ, M.; Cameron, P. Predictors of Mortality Following Severe Pelvic Ring Fracture: Results of a Population-Based Study. Orthop. Proc. 2012, 94, 133. [Google Scholar] [CrossRef]
- Kleber, C.; Giesecke, M.T.; Tsokos, M.; Haas, N.P.; Schaser, K.D.; Stefan, P.; Buschmann, C.T. Overall Distribution of Trauma-Related Deaths in Berlin 2010: Advancement or Stagnation of German Trauma Management? World J. Surg. 2012, 36, 2125–2130. [Google Scholar] [CrossRef]
- Sobrino, J.; Shafi, S. Timing and Causes of Death After Injuries. Bayl. Univ. Med. Cent. Proc. 2013, 26, 120–123. [Google Scholar] [CrossRef]
- Wisborg, T.; Høylo, T.; Siem, G. Death after Injury in Rural Norway: High Rate of Mortality and Prehospital Death. Acta Anaesthesiol. Scand. 2003, 47, 153–156. [Google Scholar] [CrossRef] [PubMed]
- Rogers, F.B.; Shackford, S.R.; Hoyt, D.B.; Camp, L.; Osler, T.M.; Mackersie, R.C.; Davis, J.W. Trauma Deaths in a Mature Urban vs. Rural Trauma System: A Comparison. Arch. Surg. 1997, 132, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Poole, G.V.; Ward, E.F.; Muakkassa, F.F.; Hsu, H.S.; Griswold, J.A.; Rhodes, R.S. Pelvic Fracture from Major Blunt Trauma. Outcome Is Determined by Associated Injuries. Ann. Surg. 1991, 213, 532–539. [Google Scholar] [CrossRef]
- Ballard, R.B.; Rozycki, G.S.; Newman, P.G.; Cubillos, J.E.; Salomone, J.P.; Ingram, W.L.; Feliciano, D.V. An Algorithm to Reduce the Incidence of False-Negative FAST***Focused Assessment for the Sonographic Examination of the Trauma Patient. Examinations in Patients at High Risk for Occult Injury11No Competing Interests Declared. J. Am. Coll. Surg. 1999, 189, 145–150. [Google Scholar] [CrossRef]
- Culemann, U.; Oestern, H.J.; Pohlemann, T. Aktuelle Behandlung der Beckenringfraktur. Unfallchirurg 2014, 117, 145–161. [Google Scholar] [CrossRef]
- Sauerland, S.; Bouillon, B.; Rixen, D.; Raum, M.R.; Koy, T.; Neugebauer, E.A.M. The Reliability of Clinical Examination in Detecting Pelvic Fractures in Blunt Trauma Patients: A Meta-Analysis. Arch. Orthop. Trauma Surg. 2004, 124, 123–128. [Google Scholar] [CrossRef]
- Arbeitsgruppe Trauma des Deutschen Rats für, Wiederbelebung; Roessler, M.S.; Buschmann, C.; Gliwitzky, B.; Hoedtke, J.; Kulla, M.; Wurmb, T.; Kleber, C. Externe, nichtinvasive Beckenstabilisatoren—Wann ist die Anlage indiziert?: Eine Empfehlung der Arbeitsgruppe Trauma des Deutschen Rats für Wiederbelebung. Notf. Rett. 2021. [Google Scholar] [CrossRef]
- Szalay, G.; Meyer, C.; Schaumberg, A.; Mann, V.; Weigand, M.A.; Schnettler, R. Stabilisierung instabiler Beckenfrakturen mittels pneumatischer Beckenschlinge im Schockraum. Notf. Rett. 2010, 13, 47–51. [Google Scholar] [CrossRef]
- Simpson, T.; Krieg, J.C.; Heuer, F.; Bottlang, M. Stabilization of Pelvic Ring Disruptions with a Circumferential Sheet. J. Trauma Acute Care Surg. 2002, 52, 158–161. [Google Scholar] [CrossRef]
- Warme, W.J.; Todd, M.S. The Circumferential Antishock Sheet. Mil. Med. 2002, 167, 438–441. [Google Scholar] [CrossRef]
- Rudol, G.; Ramdass, S.; Mestha, P.; Doughan, S.; Skyrme, A. Major Pelvic Injury Complicated by Abdominal Compartment Syndrome. Inj. Extra 2006, 8, 299–301. [Google Scholar] [CrossRef]
- Routt, C.M.L.J.; Falicov, A.; Woodhouse, E.; Schildhauer, T.A. Circumferential Pelvic Antishock Sheeting: A Temporary Resuscitation Aid. J. Orthop. Trauma 2002, 16, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Prasarn, M.L.; Conrad, B.; Small, J.; Horodyski, M.; Rechtine, G.R. Comparison of Circumferential Pelvic Sheeting versus the T-POD on Unstable Pelvic Injuries: A Cadaveric Study of Stability. Injury 2013, 44, 1756–1759. [Google Scholar] [CrossRef] [PubMed]
- Bonner, T.J.; Eardley, W.G.P.; Newell, N.; Masouros, S.; Matthews, J.J.; Gibb, I.; Clasper, J.C. Accurate Placement of a Pelvic Binder Improves Reduction of Unstable Fractures of the Pelvic Ring. J. Bone Jt. Surg. Br. 2011, 93, 1524–1528. [Google Scholar] [CrossRef] [PubMed]


| Reduction of Intrapelvic Volume (cm3 ± SD) | Reduction Area Pelvic Entrance Level (cm ± SD) | Reduction Symphysis Width (cm ± SD) | Reduction Femoral Head Distance (cm ± SD) | Reduction Distance Köhler’s Tear Figure (cm ± SD) | Reduction SIJ Distance Ventral (cm ± SD) | Reduction SIJ Distance Dorsal (cm ± SD) | |
|---|---|---|---|---|---|---|---|
| PS1 | 268 * ± 185 | 34 * ± 29 | 1.1 ± 1.9 | 2.5 ± 1.3 | 2 ± 1.2 | 1.2 ± 0.9 | 0.8 ± 2 |
| PS2 | 306 * ± 176 | 35 * ± 29 | 1.2 ± 2 | 2.9 ± 1.4 | 2.3 ± 1.2 | 1.4 ± 1 | 0.5 ± 1.3 |
| TP | 333 * ± 234 | 28 * ± 24 | 1.1 ± 1.8 | 2.1 ± 1.4 | 1.6 ± 1.1 | 1.1 ± 0.9 | 0.36 ± 1 |
| TS | 186 * ± 222 | 18 * ± 18 | 0.6 ± 1 | 1.1 ± 1 | 0.9 ± 0.8 | 0.7 ± 0.6 | 0.4 ± 1 |
| SAM | 184 ± 114 | 14 ± 8 | 0.06 ± 0.1 | 1.1 ± 0.5 | 0.9 ± 0.6 | 0.5 ± 0.4 | - |
| PS1 | PS2 | TP | TS | |
|---|---|---|---|---|
| P1 | x | |||
| P2 | PV (p = 0.002) PA (p < 0.001) FH (p < 0.001) KT (p < 0.001) SIJv (p < 0.001) | x | ||
| TP | KT (p < 0.05) | PA (p = 0.004) FH (p = 0.001) KT (p = 0.001) SIJv (p < 0.05) | x | |
| TS | PV (p = 0.01) PA (p < 0.001) SW (p < 0.005) FH (p < 0.001) KT (p < 0.001) SIJv (p < 0.001) | PV (p < 0.001) PA (p < 0.001) FH (p < 0.001) KT (p < 0.001) SIJv (p < 0.001) | PV (p < 0.001) PA (p < 0.001) FH (p < 0.001) KT (p < 0.001) SIJv (p < 0.001) | x |
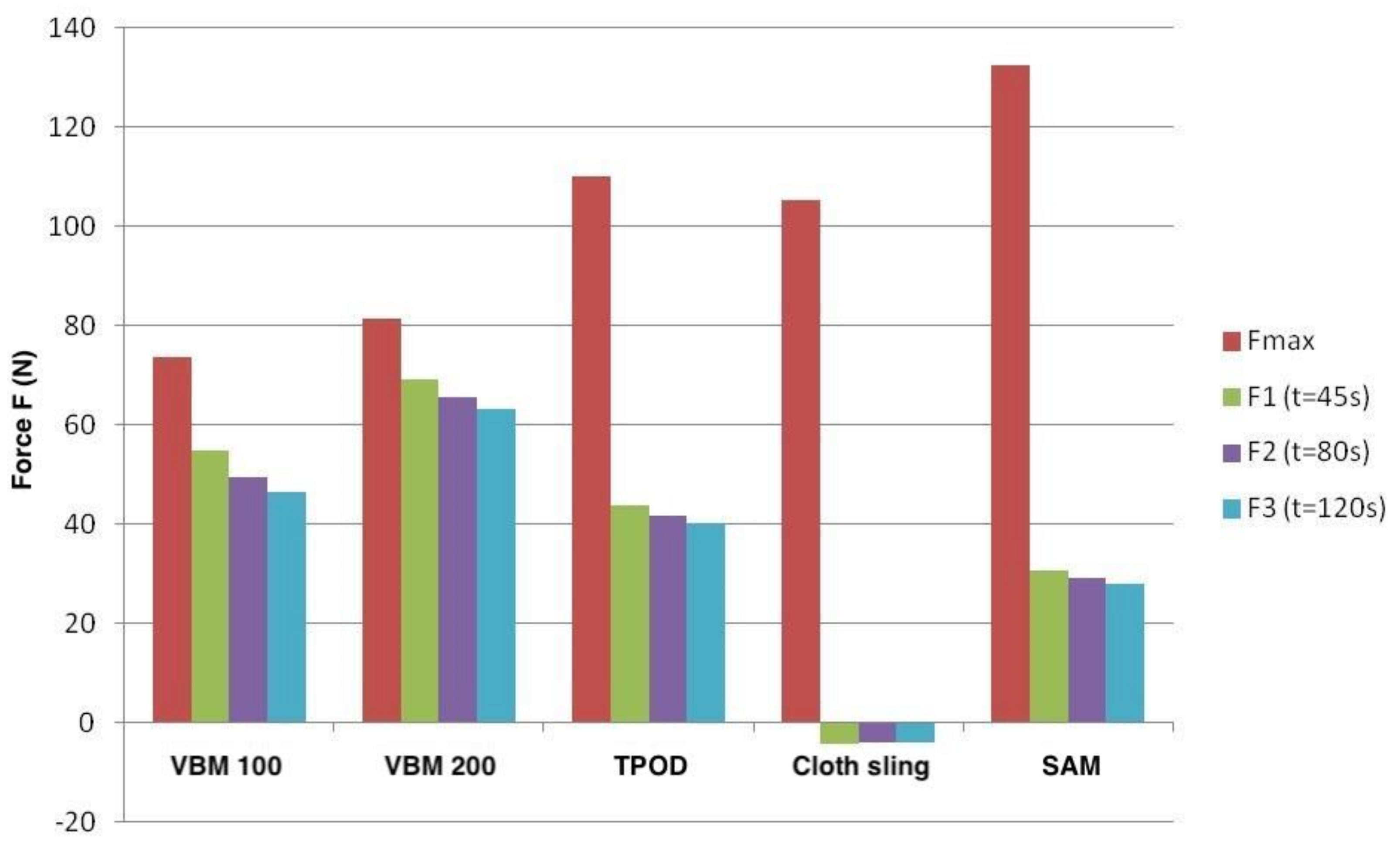
| PS1 | PS2 | TP | CS | SAM | |
|---|---|---|---|---|---|
| Fmax [N] | 73.4 | 81.5 | 109.9 | 105.2 | 132.3 |
| t1 [N] | 54.9 | 69 | 43.8 | −4.4 | 30.6 |
| t2 [N] | 49.4 | 65.5 | 41.6 | −4 | 29 |
| t3 [N] | 46.4 | 63.2 | 40.1 | −4 | 27.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kleber, C.; Haussmann, M.; Hetz, M.; Tsokos, M.; Buschmann, C.T. Epidemiologic, Postmortem Computed Tomography-Morphologic and Biomechanical Analysis of the Effects of Non-Invasive External Pelvic Stabilizers in Genuine Unstable Pelvic Injuries. J. Clin. Med. 2021, 10, 4348. https://doi.org/10.3390/jcm10194348
Kleber C, Haussmann M, Hetz M, Tsokos M, Buschmann CT. Epidemiologic, Postmortem Computed Tomography-Morphologic and Biomechanical Analysis of the Effects of Non-Invasive External Pelvic Stabilizers in Genuine Unstable Pelvic Injuries. Journal of Clinical Medicine. 2021; 10(19):4348. https://doi.org/10.3390/jcm10194348
Chicago/Turabian StyleKleber, Christian, Mirja Haussmann, Michael Hetz, Michael Tsokos, and Claas T. Buschmann. 2021. "Epidemiologic, Postmortem Computed Tomography-Morphologic and Biomechanical Analysis of the Effects of Non-Invasive External Pelvic Stabilizers in Genuine Unstable Pelvic Injuries" Journal of Clinical Medicine 10, no. 19: 4348. https://doi.org/10.3390/jcm10194348
APA StyleKleber, C., Haussmann, M., Hetz, M., Tsokos, M., & Buschmann, C. T. (2021). Epidemiologic, Postmortem Computed Tomography-Morphologic and Biomechanical Analysis of the Effects of Non-Invasive External Pelvic Stabilizers in Genuine Unstable Pelvic Injuries. Journal of Clinical Medicine, 10(19), 4348. https://doi.org/10.3390/jcm10194348







