Clinical Outcomes of Arthroscopic Notchplasty and Partial Resection for Mucoid Degeneration of the Anterior Cruciate Ligament
Abstract
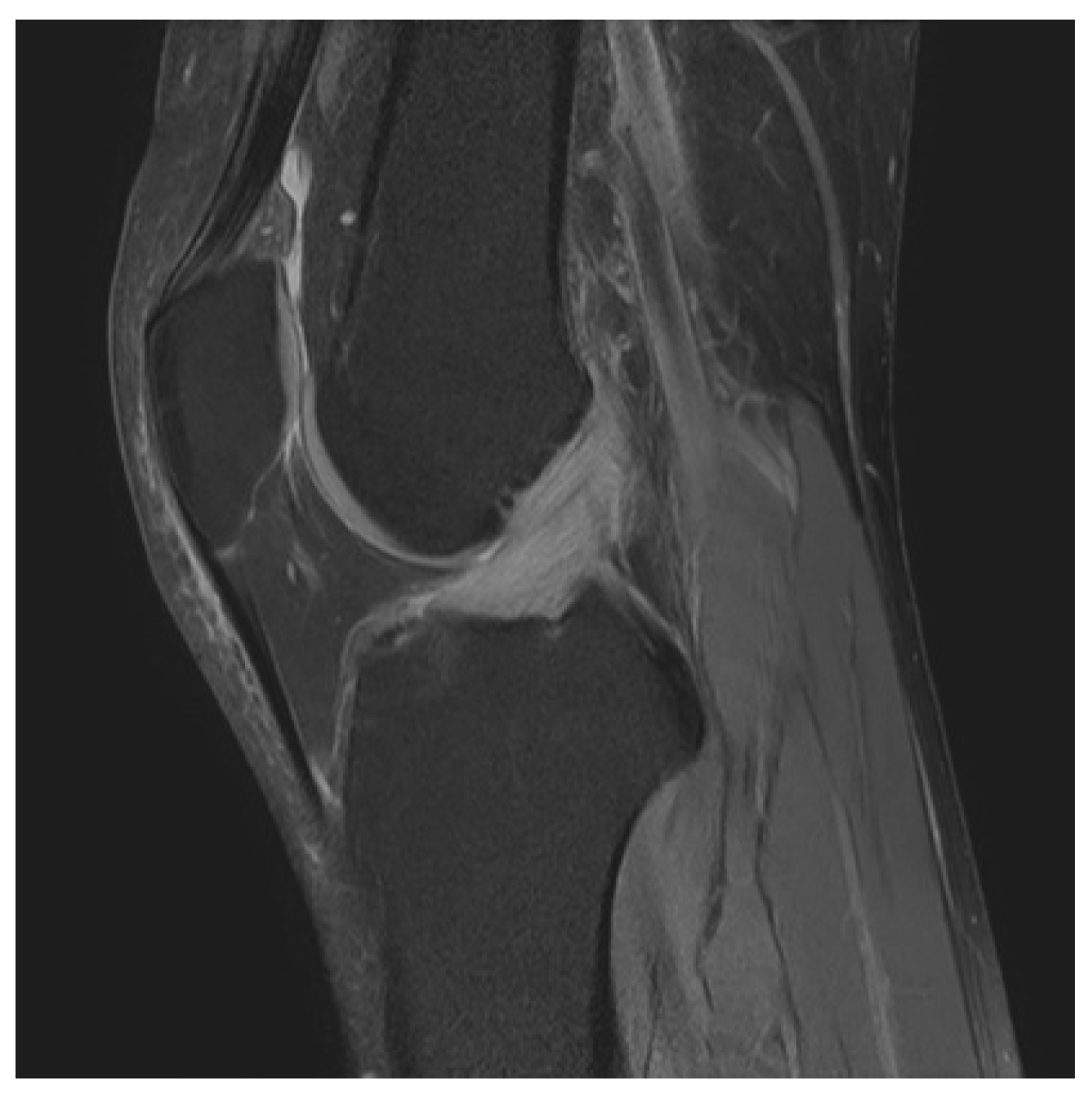
:1. Introduction
2. Materials and Methods
2.1. Clinical Data of Patients
2.2. Surgical Procedure
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kumar, A.; Bickerstaff, D.R.; Grimwood, J.S.; Suvarna, S.K. Mucoid cystic degeneration of the cruciate ligament. J. Bone Joint Surg. Br. 1999, 81, 304–305. [Google Scholar] [CrossRef]
- McIntyre, J.; Moelleken, S.; Tirman, P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol. 2001, 30, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Narvekar, A.; Gajjar, S. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy 2004, 20, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; Pujol, N.; Dejour, D.; Boisrenoult, P.; Beaufils, P. Anterior cruciate ligament mucoid degeneration: Selecting the best treatment option. Orthop. Traumatol. Surg. Res. 2010, 96, 400–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lintz, F.; Pujol, N.; Boisrenoult, P.; Bargoin, K.; Beaufils, P.; Dejour, D. Anterior cruciate ligament mucoid degeneration: A review of the literature and management guidelines. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1326–1333. [Google Scholar] [CrossRef] [PubMed]
- Cha, J.H.; Lee, S.H.; Shin, M.J.; Choi, B.K.; Bin, S.I. Relationship between mucoid hypertrophy of the anterior cruciate ligament (acl) and morphologic change of the intercondylar notch: Mri and arthroscopy correlation. Skeletal Radiol. 2008, 37, 821–826. [Google Scholar] [CrossRef]
- Bergin, D.; Morrison, W.B.; Carrino, J.A.; Nallamshetty, S.N.; Bartolozzi, A.R. Anterior cruciate ligament ganglia and mucoid degeneration: Coexistence and clinical correlation. AJR Am. J. Roentgenol. 2004, 182, 1283–1287. [Google Scholar] [CrossRef]
- Salvati, F.; Rossi, F.; Limbucci, N.; Pistoia, M.L.; Barile, A.; Masciocchi, C. Mucoid metaplastic-degeneration of anterior cruciate ligament. J. Sports Med. Phys. Fitness 2008, 48, 483–487. [Google Scholar]
- Krudwig, W.K.; Schulte, K.K.; Heinemann, C. Intra-articular ganglion cysts of the knee joint: A report of 85 cases and review of the literature. Knee Surg. Sports Traumatol. Arthrosc. 2004, 12, 123–129. [Google Scholar] [CrossRef]
- Pandey, V.; Suman, C.; Sharma, S.; Rao, S.P.; Kiran Acharya, K.; Sambaji, C. Mucoid degeneration of the anterior cruciate ligament: Management and outcome. Indian J. Orthop. 2014, 48, 197–202. [Google Scholar] [CrossRef]
- Zikria, B.; Johnson, A.; Hafezi-Nejad, N.; Siddiqui, Y.; Kwee, R.M.; Ahlawat, S.; Morelli, J.N.; Fayad, L.M.; Kompel, A.J.; Haj-Mirzaian, A.; et al. Association between mri-based tibial slope measurements and mucoid degeneration of the anterior cruciate ligament: A propensity score-matched case-control study. Orthop. J. Sports Med. 2020, 8, 2325967120962804. [Google Scholar] [CrossRef] [PubMed]
- Souryal, T.O.; Moore, H.A.; Evans, J.P. Bilaterality in anterior cruciate ligament injuries: Associated intercondylar notch stenosis. Am. J. Sports Med. 1988, 16, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Hotchen, A.J.; Demetriou, C.; Edwards, D.; Melton, J.T.K. Mucoid degeneration of the anterior cruciate ligament: Characterization of natural history, femoral notch width index, and patient reported outcome measures. J. Knee Surg. 2019, 32, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Lee, D.H.; Lee, S.H.; Kim, J.M.; Kim, C.W.; Bin, S.I. Arthroscopic treatment of mucoid hypertrophy of the anterior cruciate ligament. Arthroscopy 2008, 24, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Ventura, D.; Nunez, J.H.; Joshi-Jubert, N.; Castellet, E.; Minguell, J. Outcome of arthroscopic treatment of mucoid degeneration of the anterior cruciate ligament. Clin. Orthop. Surg. 2018, 10, 307–314. [Google Scholar] [CrossRef]
- Morice, A.; Coupry, A.; Lintz, F.; Robert, H. Reduction plasty for hypertrophic anterior cruciate ligament mucoid degeneration: Clinical and knee laxity outcomes in 23 cases. Orthop. Traumatol. Surg. Res. 2013, 99, 693–697. [Google Scholar] [CrossRef] [Green Version]
- Ahn, J.H.; Ha, C.W. Posterior trans-septal portal for arthroscopic surgery of the knee joint. Arthroscopy 2000, 16, 774–779. [Google Scholar] [CrossRef]
- Ahn, J.; Choi, B.; Lee, Y.S.; Lee, K.W.; Lee, J.W.; Lee, B.K. The mechanism and cause of anterior cruciate ligament tear in the korean military environment. Knee Surg. Relat. Res. 2019, 31, 13. [Google Scholar] [CrossRef]
- Noh, J.H.; Nam, W.D.; Roh, Y.H. Anterior tibial displacement on preoperative stress radiography of acl-injured knee depending on knee flexion angle. Knee Surg. Relat. Res. 2019, 31, 14. [Google Scholar] [CrossRef]
- Sood, M.; Kulshrestha, V.; Sachdeva, J.; Ghai, A.; Sud, A.; Singh, S. Poor functional outcome in patients with voluntary knee instability after anterior cruciate ligament reconstruction. Clin. Orthop. Surg. 2020, 12, 312–317. [Google Scholar] [CrossRef]
- Cha, J.R.; Lee, C.C.; Cho, S.D.; Youm, Y.S.; Jung, K.H. Symptomatic mucoid degeneration of the anterior cruciate ligament. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Do-Dai, D.D.; Youngberg, R.A.; Lanchbury, F.D.; Pitcher, J.D., Jr.; Garver, T.H. Intraligamentous ganglion cysts of the anterior cruciate ligament: Mr findings with clinical and arthroscopic correlations. J. Comput. Assist. Tomogr. 1996, 20, 80–84. [Google Scholar] [CrossRef]
- Parish, E.N.; Dixon, P.; Cross, M.J. Ganglion cysts of the anterior cruciate ligament: A series of 15 cases. Arthroscopy 2005, 21, 445–447. [Google Scholar] [CrossRef] [PubMed]
- Sayampanathan, A.A.; Koh, T.H.; Lee, K.T. Anterior cruciate ligament ganglion causing flexion restriction: A case report and review of literature. Ann. Transl. Med. 2016, 4, 219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Y.; Dong, Q.; Wang, Y. Ganglion cysts of the cruciate ligaments: A series of 31 cases and review of the literature. BMC Musculoskelet Disord. 2012, 13, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaishya, R.; Esin Issa, A.; Agarwal, A.K.; Vijay, V. Anterior cruciate ligament ganglion cyst and mucoid degeneration: A review. Cureus 2017, 9, e1682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, T.Y.; Yang, Y.S.; Tseng, F.J.; Lin, K.Y.; Liu, C.W.; Shen, H.C.; Lee, C.H.; Lin, L.C.; Pan, R.Y. Arthroscopic excision of ganglion cysts of the posterior cruciate ligaments using posterior trans-septal portal. Arthroscopy 2012, 28, 95–99. [Google Scholar] [CrossRef] [PubMed]


| Number of Patients (%) | |
|---|---|
| Posterior knee pain Pain on terminal flexion Pain on terminal extension | 37 (84.1%) 38 (86.4%) 34 (77.3%) |
| Limitation of range of motion Flexion deficit Extension deficit | 21 (50%) 20 (47.6%) |
| Pathology | No. of Patients (%) |
|---|---|
| Combined ACL ganglion cyst | 28 (66.7%) |
| Meniscal tears Medial Lateral Medial and Lateral Chondral lesion ICRS grade ≥2 | 28 (66.7%) 14 (33.3%) 4 (9.5%) 10 (23.8%) 23 (54.8%) |
| Medial condyle Lateral condyle Medial and Lateral condyle | 10 (23.8%) 1 (2.3%) 12 (28.6%) |
| Patellofemoral chondral lesion Popliteal cyst | 20 (47.6%) 5 (11.9%) |
| Number of Patients (%) | |
|---|---|
| Resected volume of ACL <25% of ACL volume 25–50% of ACL volume | 15 (35.7%) 27 (64.3%) |
| Concomitant notchplasty Using posterior septal portal | 36 (81.8%) 20 (47.6%) |
| Parameter | Preoperative | Final Follow-Up | p-Values b (95% CI) |
|---|---|---|---|
| Flexion contracture a | 5.12° ± 1.07° (range, 0–30°) | 0.6° ± 0.30° (range, 0–10°) | <0.001 |
| Further flexion a | 128.21° ± 2.36° (range, 80–140°) | 137.62° ± 0.80° (range, 120–140°) | <0.001 |
| Range of motion a | 123.1° ± 2.65° | 137.02° ± 0.98° | <0.001 |
| Lysholm knee score a | 64.62 ± 2.81 | 87.76 ± 1.94 | <0.001 |
| HSS score a | 71.74 ± 2.68 | 94.14 ± 0.99 | <0.001 |
| Parameters | Group 1 (n = 15) | Group 2 (n = 27) | p-Value c (95%CI) |
|---|---|---|---|
| Flexion contracture b | 1.0° ± 2.80° (range, 0–10°) | 0.4° ± 1.33° (range, 0–5°) | 0.423 |
| Further flexion b | 137.3° ± 5.94° (range, 120–140°) | 137.7° ± 4.80° (range, 120–140°) | 0.795 |
| Lysholm knee score b | 136.3 ± 8.12 | 137.4 ± 5.26 | 0.606 |
| HSS score b | 93.4 ± 6.53 | 94.56 ± 6.43 | 0.582 |
| Notchplasty a | 10 (66.7%) | 26 (96.3%) | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.W.; Ahn, J.T.; Gwak, H.G.; Lee, S.H. Clinical Outcomes of Arthroscopic Notchplasty and Partial Resection for Mucoid Degeneration of the Anterior Cruciate Ligament. J. Clin. Med. 2021, 10, 315. https://doi.org/10.3390/jcm10020315
Lee JW, Ahn JT, Gwak HG, Lee SH. Clinical Outcomes of Arthroscopic Notchplasty and Partial Resection for Mucoid Degeneration of the Anterior Cruciate Ligament. Journal of Clinical Medicine. 2021; 10(2):315. https://doi.org/10.3390/jcm10020315
Chicago/Turabian StyleLee, Joong Won, Jung Tae Ahn, Hyun Gon Gwak, and Sang Hak Lee. 2021. "Clinical Outcomes of Arthroscopic Notchplasty and Partial Resection for Mucoid Degeneration of the Anterior Cruciate Ligament" Journal of Clinical Medicine 10, no. 2: 315. https://doi.org/10.3390/jcm10020315
APA StyleLee, J. W., Ahn, J. T., Gwak, H. G., & Lee, S. H. (2021). Clinical Outcomes of Arthroscopic Notchplasty and Partial Resection for Mucoid Degeneration of the Anterior Cruciate Ligament. Journal of Clinical Medicine, 10(2), 315. https://doi.org/10.3390/jcm10020315





