Newborn Hearing Screening and Intervention in Children with Unilateral Hearing Impairment: Clinical Practices in Three Nordic Countries
Abstract
:1. Introduction
1.1. Definitions, Prevalence and Outcomes
1.2. Healthcare Systems in Norway, Sweden and Finland
1.3. Best Practice and Clinical Decision Making
1.4. Aims
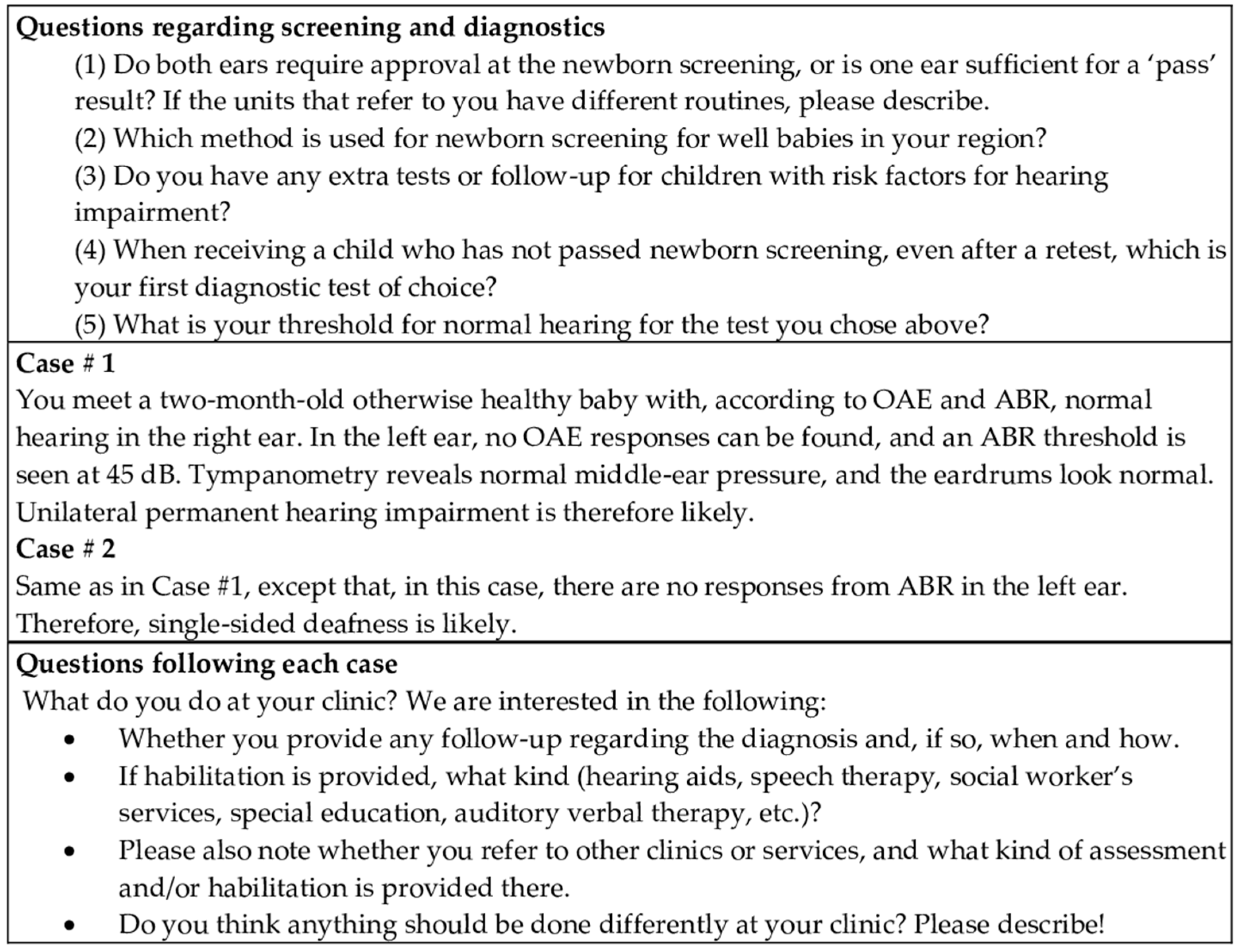
2. Materials and Methods
2.1. Recruitment and Participants
2.2. Survey Development
2.3. Data Analysis
3. Results
3.1. Respondents
3.2. Screening and Diagnostic Methods
3.3. Clinical Decisions for Habilitation
3.3.1. Hearing Diagnostics and Follow-Up Procedures for Hearing
- ‘Proceed with diagnostic ABR in natural sleep once possible’ (Case #1 and 2).
- ‘We shall make an appointment for a follow-up visit at the age of around five years when, as the primary form of examination, there will be pure tone and speech audiometry’ (Case #1).
- ‘Speech development would be monitored as a part of follow-up visits, speech therapy would be organised if needed, but, in this kind of hearing impairment, there is only seldom such a delay in speech development that would require speech therapy’ (Cases #1 and 2).
3.3.2. Conditional Access to Habilitation
- ‘Hearing aids when the child can sit’ (Case #1);
- ‘No hearing aids before preschool’ (Case #1);
- ‘Regarding UHI in a newborn, we do NOT start any habilitation’ (Case #1 and 2);
- ‘For moderate and severe HI, hearing aids are important to stimulate the auditory nerve to enable cochlear implantation in the future’ (Case #2).
3.3.3. Referral for Other Diagnostic Investigations
- ‘It is important to check the vision when hearing is impaired’ (Case #2).
3.3.4. Other Habilitation Actions and Teamwork Approaches
- ‘If we provide hearing aids, they will be referred to audio-pedagogical unit for follow-up by a special education teacher or teacher of the deaf’ (Case #1).
- ‘We do not provide habilitation; we do not refer the child to speech and language therapist’ (Case #1).
- ‘Auditory Verbal Therapy (AVT) can be provided by a speech and language therapist or other professional with AVT training’ (Case #1).
3.3.5. Differences in Actions and Treatment between Cases #1 and 2
3.3.6. Variation across Countries and Regions
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bussé, A.M.L.; Hoeve, H.L.J.; Nasserinejad, K.; Mackey, A.R.; Simonsz, H.J.; Goedegebure, A. Prevalence of permanent neonatal hearing impairment: Systematic review and Bayesian meta-analysis. Int. J. Audiol. 2020, 59, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Dalzell, L.; Orlando, M.; MacDonald, M.; Berg, A.; Bradley, M.; Cacace, A.; Campbell, D.; DeCristofaro, J.; Gravel, J.; Greenberg, E.; et al. The New York State Universal Newborn Hearing Screening Demonstration Project: Ages of Hearing Loss Identification, Hearing Aid Fitting, and Enrollment in Early Intervention. Ear Hear. 2000, 21, 118–130. [Google Scholar] [CrossRef] [PubMed]
- Uhlén, I.; Mackey, A.; Rosenhall, U. Prevalence of childhood hearing impairment in the County of Stockholm–a 40-year perspective from Sweden and other high-income countries. Int. J. Audiol. 2020, 59, 866–873. [Google Scholar] [CrossRef]
- Fitzpatrick, E.M.; Al-Essa, R.S.; Whittingham, J.; Fitzpatrick, J. Characteristics of children with unilateral hearing loss. Int. J. Audiol. 2017, 56, 819–828. [Google Scholar] [CrossRef]
- Huttunen, K.; Erixon, E.; Löfkvist, U.; Mäki-Torkko, E. The impact of permanent early-onset unilateral hearing impairment in children–A systematic review. Int. J. Pediatr. Otorhinolaryngol. 2019, 120, 173–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bagatto, M.; Desgeorges, J.; King, A.; Kitterick, P.; Laurnagaray, D.; Lewis, D.; Roush, P.; Sladen, D.P.; Tharpe, A.M. Consensus practice parameter: Audiological assessment and management of unilateral hearing loss in children. Int. J. Audiol. 2019, 58, 805–815. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Report on Hearing; World Health Organization: Geneva, Switzerland, 2021; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Berninger, E.; Westling, B. Outcome of a universal newborn hearing-screening programme based on multiple transient-evoked otoacoustic emissions and clinical brainstem response audiometry. Acta Oto-Laryngol. 2011, 131, 728–739. [Google Scholar] [CrossRef]
- Ghirri, P.; Liumbruno, A.; Lunardi, S.; Forli, F.; Boldrini, A.; Baggiani, A.; Berrettini, S. Universal neonatal audiological screening: Experience of the University Hospital of Pisa. Ital. J. Pediatr. 2011, 37, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumpik, D.; King, A.J. A review of the effects of unilateral hearing loss on spatial hearing. Hear. Res. 2018, 372, 17–28. [Google Scholar] [CrossRef]
- Priwin, C.; Jönsson, R.; Magnusson, L.; Hultcrantz, M.; Granström, G. Audiological evaluation and self-assessed hearing problems in subjects with single-sided congenital external ear malformations and associated conductive hearing loss. Int. J. Audiol. 2007, 46, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Snapp, H.A.; Ausili, S.A. Hearing with One Ear: Consequences and Treatments for Profound Unilateral Hearing Loss. J. Clin. Med. 2020, 9, 1010. [Google Scholar] [CrossRef] [Green Version]
- Sokolov, M.; Gordon, K.A.; Polonenko, M.; Blaser, S.I.; Papsin, B.C.; Cushing, S.L. Vestibular and balance function is often impaired in children with profound unilateral sensorineural hearing loss. Hear. Res. 2019, 372, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Douglas, S.A.; Yeung, P.; Daudia, A.; Gatehouse, S.; O’Donoghue, G.M. Spatial Hearing Disability After Acoustic Neuroma Removal. Laryngoscope 2007, 117, 1648–1651. [Google Scholar] [CrossRef]
- Lucas, L.; Katiri, R.; Kitterick, P.T. The psychological and social consequences of single-sided deafness in adulthood. Int. J. Audiol. 2017, 57, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Nordvik, Ø.; Heggdal, P.O.L.; Brännström, J.K.; Hjermstad, M.J.; Aarstad, A.K.; Aarstad, H.J. Quality of life in persons with hearing loss: A study of patients referred to an audiological service. Int. J. Audiol. 2019, 58, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Roland, L.; Fischer, C.; Tran, K.; Rachakonda, T.; Kallogjeri, D.; Lieu, J.E.C. Quality of Life in Children with Hearing Impairment: Systematic Review and Metaanalysis. Otolaryngol. Neck Surg. 2016, 155, 208–219. [Google Scholar] [CrossRef] [PubMed]
- Borton, S.A.; Mauze, E.; Lieu, J.E.C. Quality of Life in Children With Unilateral Hearing Loss: A Pilot Study. Am. J. Audiol. 2010, 19, 61–72. [Google Scholar] [CrossRef] [Green Version]
- Umansky, A.M.; Jeffe, D.; Lieu, J. The HEAR-QL: Quality of Life Questionnaire for Children with Hearing Loss. J. Am. Acad. Audiol. 2011, 22, 644–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kishon-Rabin, L.; Kuint, J.; Hildesheimer, M.; Roth, D.A.-E. Delay in auditory behaviour and preverbal vocalization in infants with unilateral hearing loss. Dev. Med. Child Neurol. 2015, 57, 1129–1136. [Google Scholar] [CrossRef]
- Purcell, P.L.; Cushing, S.L.; Papsin, B.C.; Gordon, K.A. Unilateral Hearing Loss and Single-Sided Deafness in Children: An Update on Diagnosis and Management. Curr. Otorhinolaryngol. Rep. 2020, 8, 259–266. [Google Scholar] [CrossRef]
- Ead, B.; Hale, S.; DeAlwis, D.; Lieu, J. Pilot study of cognition in children with unilateral hearing loss. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 1856–1860. [Google Scholar] [CrossRef] [PubMed]
- Lieu, J.E.C. Unilateral hearing loss in children: Speech-language and school performance. B-ENT 2013, 107–115. [Google Scholar]
- Fitzpatrick, E.M.; Durieux-Smith, A.; Gaboury, I.; Coyle, D.; Whittingham, J. Communication Development in Early-Identified Children With Mild Bilateral and Unilateral Hearing Loss. Am. J. Audiol. 2015, 24, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Niedzielski, A.; Humeniuk, E.; Błaziak, P.; Gwizda, G. Intellectual efficiency of children with unilateral hearing loss. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 1529–1532. [Google Scholar] [CrossRef] [PubMed]
- Lieu, J.E.C.; Dewan, K. Assessment of self-selection bias in a pediatric unilateral hearing loss study. Otolaryngol. Head Neck Surg. 2010, 142, 427–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzpatrick, E.M.; Whittingham, J.; Durieux-Smith, A. Mild Bilateral and Unilateral Hearing Loss in Childhood: A 20-year view of hearing characteristics, and audiologic practices before and after newborn hearing screening. Ear Hear. 2014, 35, 10–18. [Google Scholar] [CrossRef]
- Anne, S.; Lieu, J.E.C.; Cohen, M.S. Speech and Language Consequences of Unilateral Hearing Loss: A Systematic Review. Otolaryngol. Neck Surg. 2017, 157, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Folkehelseinstituttet. Medical Birth Registry of Norway. Available online: http://statistikkbank.fhi.no/mfr/ (accessed on 9 September 2021).
- Kolada. Rådet för Främjande av Kommunala Analyser. Available online: https://www.kolada.se/verktyg/fri-sokning/ (accessed on 22 August 2021).
- Finnish Institute for Health and Welfare. Births. Available online: https://www.thl.fi/tilastoliite/tilastoraportit/2020/Liitetaulukot/Tr48_20_liitetaulukot.pdf (accessed on 22 August 2021).
- Mackey, A.; Uhlén, I. Summary: Hearing Screening Sweden (Stockholm Region); Karolinska Institutet. Available online: https://www.euscreen.org/wp-content/uploads/2020/07/Sweden-Stockholm-Region-Hearing-Screening-Report.pdf (accessed on 24 September 2021).
- Mackey, A.; Uhlén, I. Summary: Hearing Screening Finland; Karolinska Institutet. Available online: https://www.euscreen.org/wp-content/uploads/2020/07/Finland-Hearing-Screening-Report.pdf (accessed on 24 September 2021).
- Anderssen, S.-H.; Andresen, J.; Andersen, R.; Sponheim, L. Universell hørselsscreening av nyfødte med otoakustiske emisjoner. [Universal neonatal hearing screening of infants with otoacoustic emissions]. Tidsskr. Nor. Laegeforening 2002, 122, 2187–2189. [Google Scholar]
- Hergils, L. Analysis of measurements from the first Swedish universal neonatal hearing screening program. Int. J. Audiol. 2007, 46, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Helsedirektoratet. Nasjonal Faglig Retningslinje for Utredning og Oppfølging av Hørsel hos Små Barn (0–3 år). Available online: https://helsedirektoratet.no/retningslinjer/horselsutredning-hos-barn-03-ar (accessed on 9 September 2021).
- Aarnisalo, A.; Hyvärinen, A.; Häkli, S.; Mykkänen, S.; Salonen, J.; Peltonen, R.; Rouvinen, J.; Suomela-Markkanen, T. Kuulon Apuvälinettä Käyttävän Lapsen ja Nuoren Hyvä Kuntoutuskäytäntö; Kuntoutussäätiö: Helsinki, Finland, 2017. [Google Scholar]
- Joint Committee on Infant Hearing. Year 2007 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. Pediatrics 2007, 120, 898–921. [Google Scholar] [CrossRef] [Green Version]
- Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar] [CrossRef]
- Joint Committee on Infant Hearing. Year 2000 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2000, 106, 798–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joint Committee on Infant Hearing; Muse, C.; Harrison, J.; Yoshinaga-Itano, C.; Grimes, A.; Brookhouser, P.E.; Epstein, S.; Buchman, C.; Mehl, A.; Vohr, B.; et al. Supplement to the JCIH 2007 position statement: Principles and guidelines for early intervention after confirmation that a child is deaf or hard of hearing. Pediatrics 2013, 131, e1324–e1349. [Google Scholar] [CrossRef] [Green Version]
- Moeller, M.P.; Carr, G.; Seaver, L.; Stredler-Brown, A.; Holzinger, D. Best Practices in Family-Centered Early Intervention for Children Who Are Deaf or Hard of Hearing: An International Consensus Statement. J. Deaf. Stud. Deaf. Educ. 2013, 18, 429–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Hearing Screening: Considerations for Implementation; World Health Organization: Geneva, Switzerland, 2021; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Neumann, K.; Chadha, S.; Tavartkiladze, G.; Bu, X.; White, K.R. Newborn and Infant Hearing Screening Facing Globally Growing Numbers of People Suffering from Disabling Hearing Loss. Int. J. Neonatal Screen. 2019, 5, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Speech-Language and Audiology Canada. SAC Position Paper on Unilateral Hearing Loss in Children; Speech-Language and Audiology Canada: Ottawa, ON, Canada, 2020; p. 10. [Google Scholar]
- Bagatto, M. Audiological Considerations for Managing Mild Bilateral or Unilateral Hearing Loss in Infants and Young Children. Lang. Speech Hear. Serv. Sch. 2020, 51, 68–73. [Google Scholar] [CrossRef]
- Appachi, S.; Specht, J.L.; Raol, N.; Lieu, J.E.C.; Cohen, M.S.; Dedhia, K.; Anne, S. Auditory Outcomes with Hearing Rehabilitation in Children with Unilateral Hearing Loss: A Systematic Review. Otolaryngol. Neck Surg. 2017, 157, 565–571. [Google Scholar] [CrossRef]
- Sloot, F.; Hoeve, H.L.; La De Kroon, M.; Goedegebure, A.; Carlton, J.; Griffiths, H.J.; Simonsz, H.J. Inventory of current EU paediatric vision and hearing screening programmes. J. Med. Screen. 2015, 22, 55–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holstrum, W.J.; Gaffney, M.; Gravel, J.S.; Oyler, R.F.; Ross, D.S. Early Intervention for Children With Unilateral and Mild Bilateral Degrees of Hearing Loss. Trends Amplif. 2008, 12, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzpatrick, E.M.; Roberts, C.; Whittingham, J.; Barreira-Nielsen, C. Amplification Decisions for Children with Mild Bilateral and Unilateral Hearing Loss. Can. J. Speech-Lang. Pathol. Audiol. 2017, 41, 203–226. [Google Scholar]
- Hussain, S.; Pryce, H.; Neary, A.; Hall, A. Exploring how parents of children with unilateral hearing loss make habilitation decisions: A qualitative study. Int. J. Audiol. 2021, 60, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, E.M.; Gaboury, I.; Durieux-Smith, A.; Coyle, D.; Whittingham, J.; Salamatmanesh, M.; Lee, R.; Fitzpatrick, J. Parent Report of Amplification Use in Children with Mild Bilateral or Unilateral Hearing Loss. J. Am. Acad. Audiol. 2019, 30, 093–102. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.B.; Onwuegbuzie, A.J.; Turner, L.A. Toward a Definition of Mixed Methods Research. J. Mix. Methods Res. 2007, 1, 112–133. [Google Scholar] [CrossRef]
- Kyngäs, H. Inductive Content Analysis. In The Application of Content Analysis in Nursing Science Research; Kyngäs, H., Mikkonen, K., Kääriäinen, M., Eds.; Springer Nature: Cham, Switzerland, 2019; pp. 13–21. [Google Scholar]
- Porter, A.; Sheeran, N.; Hood, M.; Creed, P. Decision-making following identification of an Infant’s unilateral hearing loss: Parent and professional perspectives. Int. J. Pediatr. Otorhinolaryngol. 2021, 148, 110822. [Google Scholar] [CrossRef] [PubMed]
- Young, A.; Carr, G.; Hunt, R.; McCracken, W.; Skipp, A.; Tattersall, H. Informed Choice and Deaf Children: Underpinning Concepts and Enduring Challenges. J. Deaf. Stud. Deaf. Educ. 2006, 11, 322–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goderis, J.; De Leenheer, E.; Smets, K.; Van Hoecke, H.; Keymeulen, A.; Dhooge, I. Hearing Loss and Congenital CMV Infection: A Systematic Review. Pediatrics 2014, 134, 972–982. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kummer, P.; Marcrum, S.C. Potential Benefit of Selective CMV Testing after Failed Newborn Hearing Screening. Int. J. Neonatal Screen. 2018, 4, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dedhia, K.; Fifer, R.C.; Muldoon, K.M.; Park, A. A Cross-Sectional Survey Evaluating Awareness of Congenital Cytomegalovirus Among Audiologists and Speech-Language Pathologists. Am. J. Audiol. 2021, 30, 145–159. [Google Scholar] [CrossRef] [PubMed]
| Survey Item | Norway | Sweden | Finland | Total |
|---|---|---|---|---|
| Number of Hospitals | 15 | 29 | 17 | |
| SCREENING | ||||
| Requires Pass in Both Ears | 100 | 100 | 19.4 | 83.6 |
| Screening Method for Well Babies | ||||
| OAE | 100 | 100 | 100 | 100 |
| Extra Tests for Babies at Risk | ||||
| Yes | 87.2 | 97.0 | 79.3 | 92.3 |
| No | 12.8 | 3.0 | 3.8 | 4.9 |
| Missing | 0 | 0 | 16.9 | 2.8 |
| DIAGNOSTICS | ||||
| First Diagnostic Method of Choice | ||||
| Automated ABR (AABR) | 90.5 | 98.8 | 0 | 75.2 |
| Diagnostic ABR | 3.6 | 1.2 | 54.1 | 13.4 |
| ASSR | 0 | 0 | 43.5 | 9.5 |
| Other | 5.9 | 0 | 2.4 | 1.9 |
| Threshold for Normal Hearing | ||||
| 20 dB | 0 | 0 | 44.3 | 9.7 |
| 25 dB | 16.5 | 0 | 6.0 | 5.1 |
| 30 dB | 6.7 | 66.9 | 47.4 | 48.7 |
| 35 dB | 76.7 | 30.1 | 0 | 34.3 |
| Missing | 0 | 3.0 | 2.4 | 2.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laugen, N.J.; Erixon, E.; Huttunen, K.; Mäki-Torkko, E.; Löfkvist, U. Newborn Hearing Screening and Intervention in Children with Unilateral Hearing Impairment: Clinical Practices in Three Nordic Countries. J. Clin. Med. 2021, 10, 5152. https://doi.org/10.3390/jcm10215152
Laugen NJ, Erixon E, Huttunen K, Mäki-Torkko E, Löfkvist U. Newborn Hearing Screening and Intervention in Children with Unilateral Hearing Impairment: Clinical Practices in Three Nordic Countries. Journal of Clinical Medicine. 2021; 10(21):5152. https://doi.org/10.3390/jcm10215152
Chicago/Turabian StyleLaugen, Nina Jakhelln, Elsa Erixon, Kerttu Huttunen, Elina Mäki-Torkko, and Ulrika Löfkvist. 2021. "Newborn Hearing Screening and Intervention in Children with Unilateral Hearing Impairment: Clinical Practices in Three Nordic Countries" Journal of Clinical Medicine 10, no. 21: 5152. https://doi.org/10.3390/jcm10215152
APA StyleLaugen, N. J., Erixon, E., Huttunen, K., Mäki-Torkko, E., & Löfkvist, U. (2021). Newborn Hearing Screening and Intervention in Children with Unilateral Hearing Impairment: Clinical Practices in Three Nordic Countries. Journal of Clinical Medicine, 10(21), 5152. https://doi.org/10.3390/jcm10215152








