Predicting Quality of Life and Behavior and Emotion from Functional Auditory and Pragmatic Language Abilities in 9-Year-Old Deaf and Hard-of-Hearing Children
Abstract
:1. Introduction
1.1. Psychosocial Abilities and Functional Language Use
1.2. Quality of Life and Functional Language Use
1.3. Aims of the Current Study
- Do nine-year-old children with hearing loss who use spoken language to communicate differ from their hearing peers in behavior and emotion and QOL?
- To what extent does performance on tests of functional abilities and structural language abilities predict concurrent behavior and emotion and QOL in nine-year-old children with hearing loss who use spoken language to communicate?
2. Materials and Methods
2.1. Procedure
2.2. Participants
2.3. Predictor Measures: Language Assessments, Nonverbal Cognitive Ability, Pragmatic Skills, Auditory Functional Performance, and Speech Intelligibility
2.3.1. Spoken Language Ability
2.3.2. Nonverbal Cognitive Ability
2.3.3. Pragmatic Use of Spoken Language
2.3.4. Auditory Functional Performance
2.3.5. Speech Intelligibility
2.4. Dependent Measures: Behavior and Emotion and Health-Related Quality of Life
2.4.1. Behavior and Emotion
2.4.2. Health-Related Quality of Life
2.5. Statistical Analysis
3. Results
3.1. Outcomes of DHH Children Compared to Norms
3.1.1. Functional and Language Outcomes
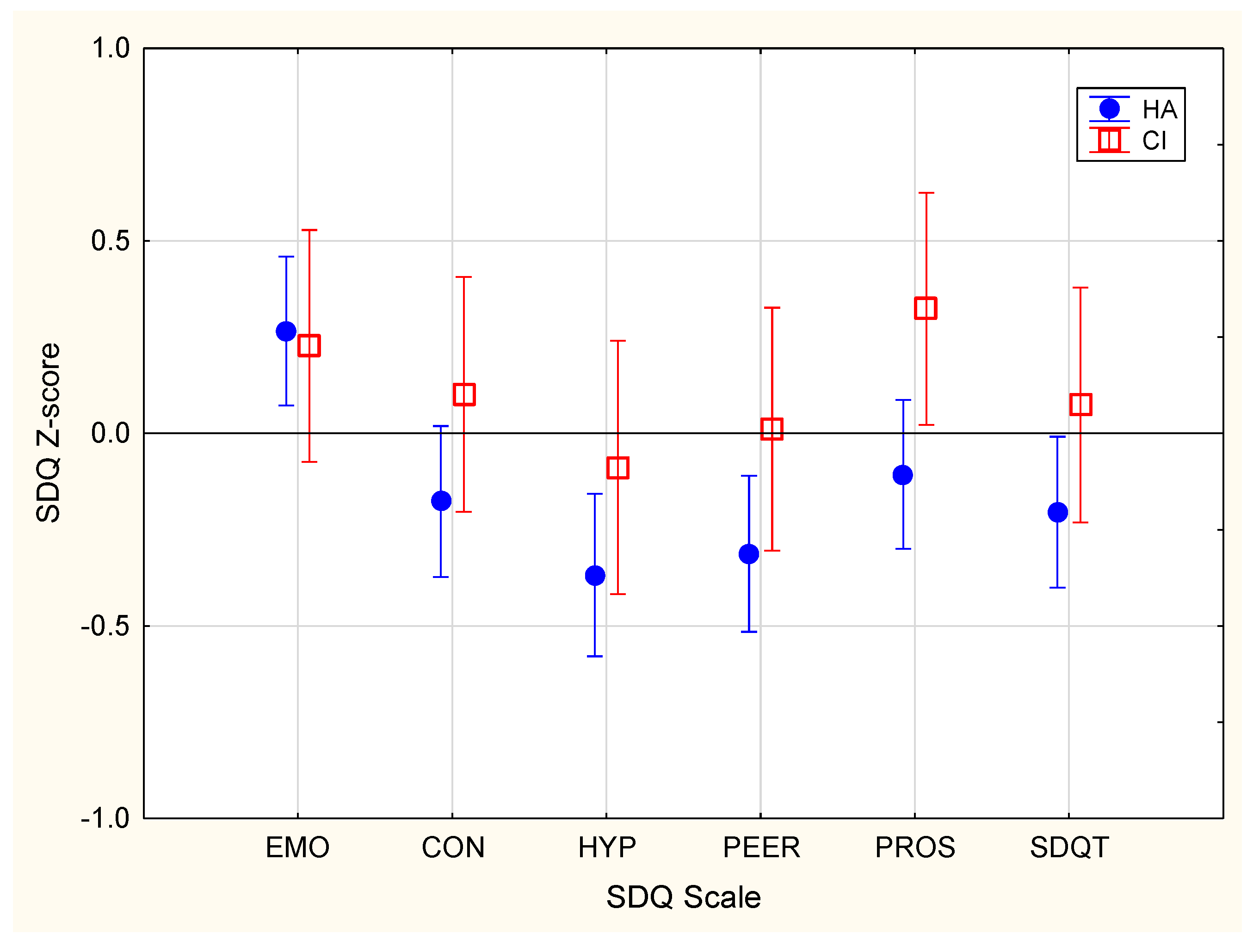
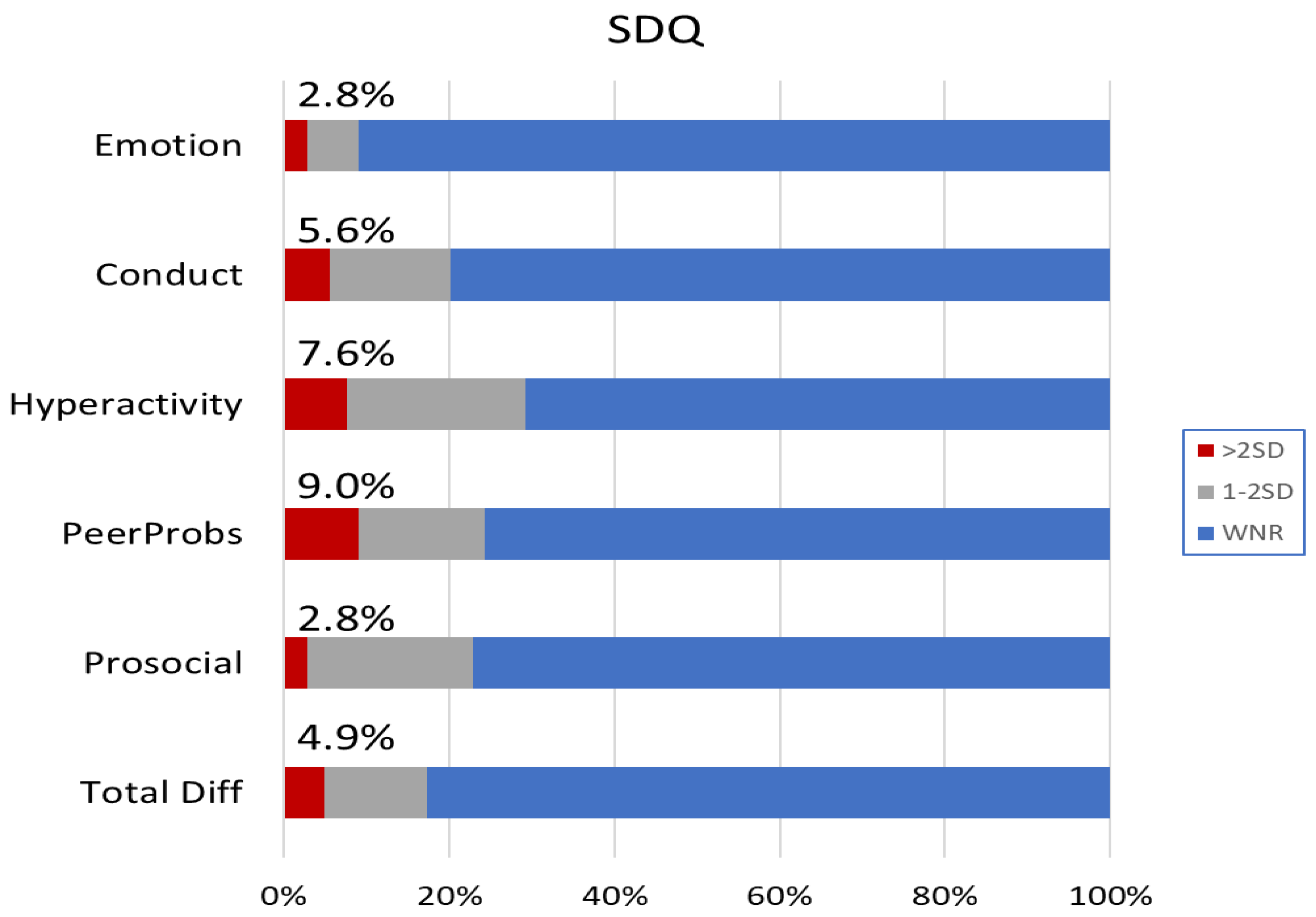
3.1.2. Behavior and Emotion
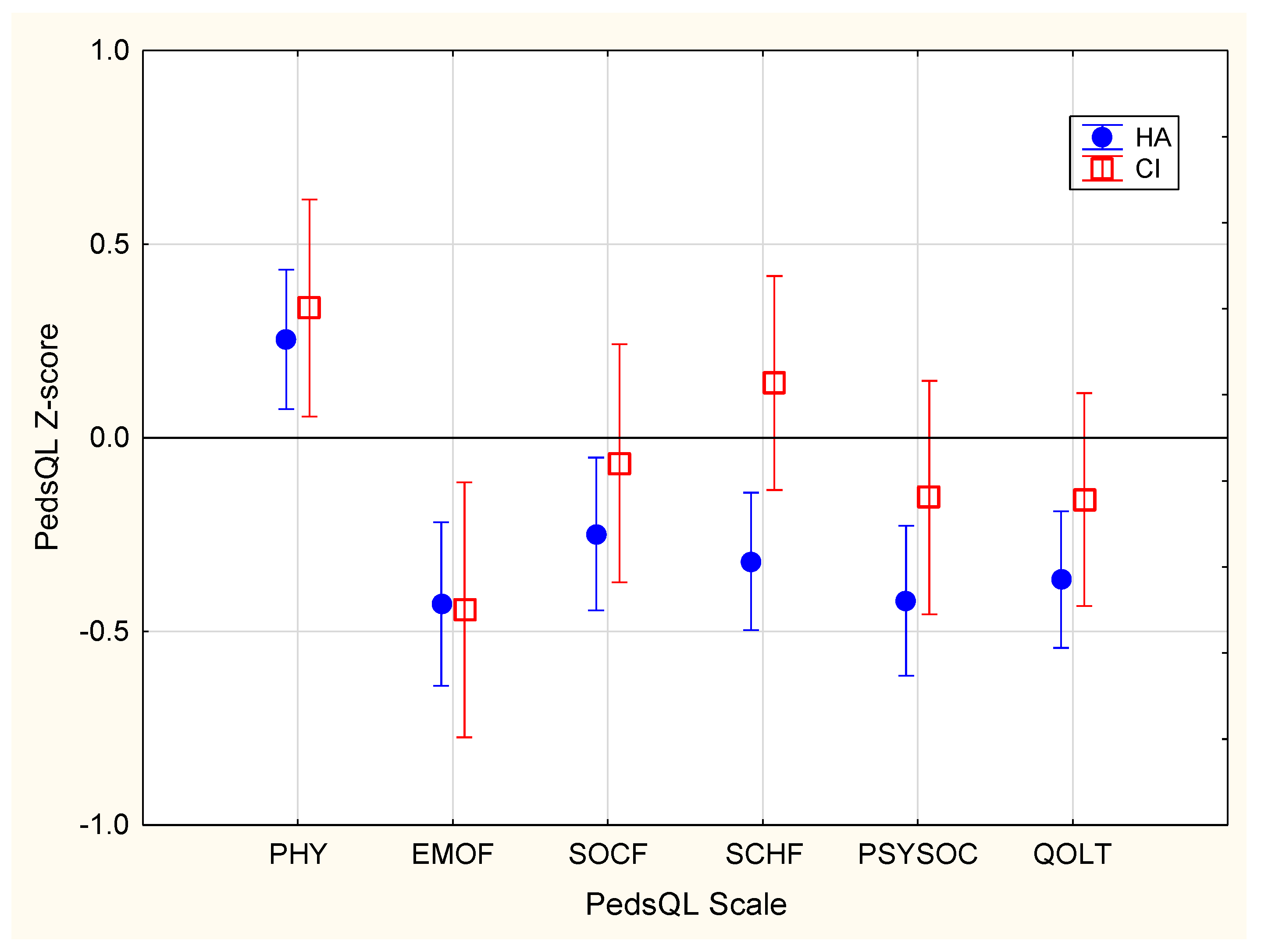
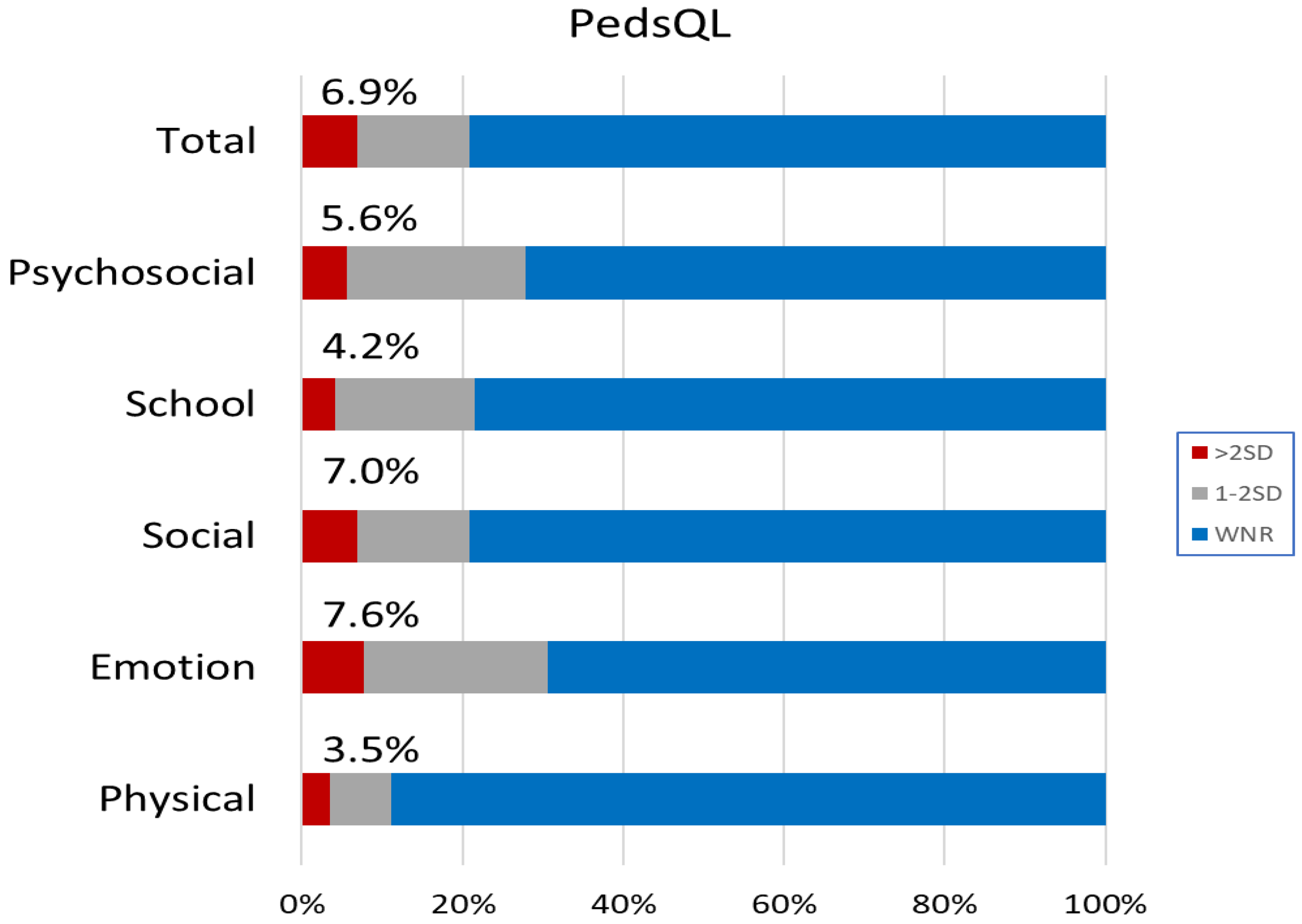
3.1.3. Quality of Life
3.2. Factors Influencing Behavior and Emotion, and Quality of Life
3.2.1. Correlations among Measures
3.2.2. Behavior and Emotion
3.2.3. Quality of Life
4. Discussion
4.1. Behavior and Emotion
4.2. Quality of Life
4.3. Summary and Clinical Implications
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Castellanos, I.; Kronenberger, W.G.; Pisoni, D.B. Psychosocial Outcomes in Long-Term Cochlear Implant Users. Ear Hear. 2018, 39, 527–539. [Google Scholar] [CrossRef]
- Dammeyer, J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J. Deaf. Stud. Deaf. Educ. 2010, 15, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fellinger, J.; Holzinger, D.; Beitel, C.; Laucht, M.; Goldberg, D.P. The impact of language skills on mental health in teenagers with hearing impairments. Acta Psychiatr. Scand. 2009, 120, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Overgaard, K.R.; Oerbeck, B.; Wagner, K.; Friis, S.; Ohre, B.; Zeiner, P. Youth with hearing loss: Emotional and behavioral problems and quality of life. Int. J. Pediatr. Otorhinolaryngol. 2021, 145, 110718. [Google Scholar] [CrossRef] [PubMed]
- Stika, C.J.; Eisenberg, L.S.; Carter, A.S.; Johnson, K.C.; Hammes Ganguly, D.M.; Henning, S.C.; DesJardin, J.L. Developmental Outcomes in Early-Identified Children Who Are Hard of Hearing at 2 to 3 Years of Age. Ear Hear. 2021, 42, 1238–1252. [Google Scholar] [CrossRef]
- Zaidman-Zait, A.; Most, T. Pragmatics and Peer Relationships Among Deaf, Hard of Hearing, and Hearing Adolescents. Pediatrics 2020, 146, S298–S303. [Google Scholar] [CrossRef]
- Haukedal, C.L.; von Koss Torkildsen, J.; Lyxell, B.; Wie, O.B. Parents’ Perception of Health-Related Quality of Life in Children With Cochlear Implants: The Impact of Language Skills and Hearing. J. Speech Lang. Hear. Res. 2018, 61, 2084–2098. [Google Scholar] [CrossRef]
- Haukedal, C.L.; Lyxell, B.; Wie, O.B. Health-Related Quality of Life With Cochlear Implants: The Children’s Perspective. Ear Hear. 2020, 41, 330–343. [Google Scholar] [CrossRef]
- Roland, L.; Fischer, C.; Tran, K.; Rachakonda, T.; Kallogjeri, D.; Lieu, J.E. Quality of Life in Children with Hearing Impairment: Systematic Review and Meta-analysis. Otolaryngol. Head Neck Surg. 2016, 155, 208–219. [Google Scholar] [CrossRef]
- Hofmann, M.; Meloche, M.; Zwolan, T.A. Health related quality of life in adolescent cochlear implant users. Cochlear Implants Int. 2020, 21, 198–205. [Google Scholar] [CrossRef]
- Martin, D.; Bat-Chava, Y.; Lalwani, A.; Waltzman, S.B. Peer relationships of deaf children with cochlear implants: Predictors of peer entry and peer interaction success. J. Deaf. Stud. Deaf. Educ. 2011, 16, 108–120. [Google Scholar] [CrossRef] [Green Version]
- Sarant, J.Z.; Harris, D.C.; Galvin, K.L.; Bennet, L.A.; Canagasabey, M.; Busby, P.A. Social Development in Children With Early Cochlear Implants: Normative Comparisons and Predictive Factors, Including Bilateral Implantation. Ear Hear. 2018, 39, 770–782. [Google Scholar] [CrossRef]
- Leigh, G.; Ching, T.Y.; Crowe, K.; Cupples, L.; Marnane, V.; Seeto, M. Factors Affecting Psychosocial and Motor Development in 3-Year-Old Children Who Are Deaf or Hard of Hearing. J. Deaf. Stud. Deaf. Educ. 2015, 20, 331–342. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Programme on Mental Health: WHOQOL User Manual; Revision 2012; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Wong, C.L.; Ching, T.Y.; Leigh, G.; Cupples, L.; Button, L.; Marnane, V.; Whitfield, J.; Gunnourie, M.; Martin, L. Psychosocial development of 5-year-old children with hearing loss: Risks and protective factors. Int. J. Audiol. 2018, 57, S81–S92. [Google Scholar] [CrossRef]
- Wong, C.L.; Ching, T.Y.C.; Cupples, L.; Button, L.; Leigh, G.; Marnane, V.; Whitfield, J.; Gunnourie, M.; Martin, L. Psychosocial Development in 5-Year-Old Children With Hearing Loss Using Hearing Aids or Cochlear Implants. Trends Hear. 2017, 21, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Szarkowski, A.; Toe, D. Pragmatics in Deaf and Hard of Hearing Children: An Introduction. Pediatrics 2020, 146, S231–S236. [Google Scholar] [CrossRef]
- American Psychological Association. APA Dictionary of Psychology. Available online: https://dictionary.apa.org/ (accessed on 20 September 2021).
- Ireton, H. Child Development Inventory; Child Development Review: Minneapolis, MN, USA, 2005. [Google Scholar]
- Zimmerman, I.L.; Steiner, V.G.; Pond, R.E. Preschool Language Scale, 4th ed.; The Psychological Corporation: San Antonio, TX, USA, 2002. [Google Scholar]
- Ching, T.Y.; Hill, M. The Parents’ Evaluation of Aural/Oral Performance of Children (PEACH) scale: Normative data. J. Am. Acad. Audiol. 2007, 18, 220–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, V.; Pisoni, D.B.; Kronenberger, W.G.; Castellanos, I. Speech Intelligibility and Psychosocial Functioning in Deaf Children and Teens with Cochlear Implants. J. Deaf. Stud. Deaf. Educ. 2017, 22, 278–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reynolds, C.R.; Kamphaus, R.W. Behavior Assessment System for Children Manual; Pearson: Bloomington, MN, USA, 2004. [Google Scholar]
- Kushalnagar, P.; Topolski, T.D.; Schick, B.; Edwards, T.C.; Skalicky, A.M.; Patrick, D.L. Mode of communication, perceived level of understanding, and perceived quality of life in youth who are deaf or hard of hearing. J. Deaf. Stud. Deaf. Educ. 2011, 16, 512–523. [Google Scholar] [CrossRef]
- Most, T. Speech intelligibility, loneliness, and sense of coherence among deaf and hard-of-hearing children in individual inclusion and group inclusion. J. Deaf. Stud. Deaf. Educ. 2007, 12, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Zaidman-Zait, A.; Dotan, A. Everyday Stressors in Deaf and Hard of Hearing Adolescents: The Role of Coping and Pragmatics. J. Deaf. Stud. Deaf. Educ. 2017, 22, 257–268. [Google Scholar] [CrossRef]
- Ching, T.Y.; Leigh, G.; Dillon, H. Introduction to the longitudinal outcomes of children with hearing impairment (LOCHI) study: Background, design, sample characteristics. Int. J. Audiol. 2013, 52, S4–S9. [Google Scholar] [CrossRef]
- Semel, E.; Wiig, E.H.; Secord, W. Clinical Evaluation of Language Fundamentals, 4th ed.; Australian Standardised Edition (CELF-4 Australian); Harcourt Assessment: Marrickville, Australia, 2003. [Google Scholar]
- Wechsler, D.; Naglieri, J. Wechsler Nonverbal Scale of Ability: WNV; Harcourt Assessment: San Antonio, TX, USA, 2006. [Google Scholar]
- Bishop, D.V. The Children’s Communication Checklist; Psychological Corporation London: London, UK, 2003; Volume 2. [Google Scholar]
- Norbury, C.F.; Nash, M.; Baird, G.; Bishop, D. Using a parental checklist to identify diagnostic groups in children with communication impairment: A validation of the Children’s Communication Checklist–2. Int. J. Lang. Commun. Disord. 2004, 39, 345–364. [Google Scholar] [CrossRef] [PubMed]
- Ching, T.Y.; Hill, M.; Dillon, H. Effect of variations in hearing-aid frequency response on real-life functional performance of children with severe or profound hearing loss. Int. J. Audiol. 2008, 47, 461–475. [Google Scholar] [CrossRef] [PubMed]
- Bagatto, M.P.; Scollie, S.D. Validation of the Parents’ Evaluation of Aural/Oral Performance of Children (PEACH) Rating Scale. J. Am. Acad. Audiol. 2013, 24, 121–125. [Google Scholar] [CrossRef]
- Golding, M.; Pearce, W.; Seymour, J.; Cooper, A.; Ching, T.; Dillon, H. The relationship between obligatory cortical auditory evoked potentials (CAEPs) and functional measures in young infants. J. Am. Acad. Audiol. 2007, 18, 117–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikolopoulos, T.P.; Archbold, S.M.; Gregory, S. Young deaf children with hearing aids or cochlear implants: Early assessment package for monitoring progress. Int. J. Pediatr. Otorhinolaryngol. 2005, 69, 175–186. [Google Scholar] [CrossRef]
- Allen, C.; Nikolopoulos, T.P.; Dyar, D.; O’Donoghue, G.M. Reliability of a rating scale for measuring speech intelligibility after pediatric cochlear implantation. Otol. Neurotol. 2001, 22, 631–633. [Google Scholar] [CrossRef]
- Yoshinaga-Itano, C. Successful outcomes for deaf and hard-of-hearing children. Semin. Hear. 2000, 21, 309–326. [Google Scholar] [CrossRef]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Niclasen, J.; Dammeyer, J. Psychometric Properties of the Strengths and Difficulties Questionnaire and Mental Health Problems Among Children With Hearing Loss. J. Deaf. Stud. Deaf. Educ. 2016, 21, 129–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hintermair, M. Prevalence of socioemotional problems in deaf and hard of hearing children in Germany. Am. Ann. Deaf. 2007, 152, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Mellor, D. Normative data for the Strengths and Difficulties Questionnaire in Australia. Aust. Psychol. 2005, 40, 215–222. [Google Scholar] [CrossRef] [Green Version]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef]
- Varni, J.W.; Burwinkle, T.M.; Seid, M.; Skarr, D. The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambul. Pediatr. 2003, 3, 329–341. [Google Scholar] [CrossRef]
- Wang, J.; Quach, J.; Sung, V.; Carew, P.; Edwards, B.; Grobler, A.; Gold, L.; Wake, M. Academic, behavioural and quality of life outcomes of slight to mild hearing loss in late childhood: A population-based study. Arch. Dis. Child 2019, 104, 1056–1063. [Google Scholar] [CrossRef] [PubMed]
- Wake, M.; Tobin, S.; Cone-Wesson, B.; Dahl, H.H.; Gillam, L.; McCormick, L.; Poulakis, Z.; Rickards, F.W.; Saunders, K.; Ukoumunne, O.C.; et al. Slight/mild sensorineural hearing loss in children. Pediatrics 2006, 118, 1842–1851. [Google Scholar] [CrossRef]
- StatSoft Inc. Statistica Software; Version 10; Statsoft Inc.: Tulsa, OK, USA, 2011. [Google Scholar]
- Ching, T.Y.C.; Dillon, H.; Button, L.; Seeto, M.; Van Buynder, P.; Marnane, V.; Cupples, L.; Leigh, G. Age at Intervention for Permanent Hearing Loss and 5-Year Language Outcomes. Pediatrics 2017, 140, e20164274. [Google Scholar] [CrossRef] [Green Version]
- Stevenson, J.; McCann, D.; Watkin, P.; Worsfold, S.; Kennedy, C.; Team, H.O.S. The relationship between language development and behaviour problems in children with hearing loss. J. Child Psychol. Psychiatry 2010, 51, 77–83. [Google Scholar] [CrossRef]
- Theunissen, S.C.; Rieffe, C.; Netten, A.P.; Briaire, J.J.; Soede, W.; Schoones, J.W.; Frijns, J.H. Psychopathology and its risk and protective factors in hearing-impaired children and adolescents: A systematic review. JAMA Pediatr. 2014, 168, 170–177. [Google Scholar] [CrossRef]
- Stevenson, J.; Kreppner, J.; Pimperton, H.; Worsfold, S.; Kennedy, C. Emotional and behavioural difficulties in children and adolescents with hearing impairment: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2015, 24, 477–496. [Google Scholar] [CrossRef] [Green Version]
- Dye, M.W.; Bavelier, D. Attentional enhancements and deficits in deaf populations: An integrative review. Restor. Neurol. Neurosci. 2010, 28, 181–192. [Google Scholar] [CrossRef] [Green Version]
- Corina, D.; Singleton, J. Developmental social cognitive neuroscience: Insights from deafness. Child Dev. 2009, 80, 952–967. [Google Scholar] [CrossRef]
- Cummings, L. Pragmatic Disorders; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar]
- Borton, S.A.; Mauze, E.; Lieu, J.E. Quality of life in children with unilateral hearing loss: A pilot study. Am. J. Audiol. 2010, 19, 61–72. [Google Scholar] [CrossRef] [Green Version]
- Lovett, R.E.; Kitterick, P.T.; Hewitt, C.E.; Summerfield, A.Q. Bilateral or unilateral cochlear implantation for deaf children: An observational study. Arch. Dis. Child 2010, 95, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Umansky, A.M.; Jeffe, D.B.; Lieu, J.E. The HEAR-QL: Quality of life questionnaire for children with hearing loss. J. Am. Acad. Audiol. 2011, 22, 644–653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, C.Y.; Jeffe, D.B.; Kenna, M.A.; Germiller, J.A.; Lieu, J.E.C. Validation of a Parent Proxy Quality-of-Life Measure for Young Children With Hearing Loss. Laryngoscope 2021, 131, 663–670. [Google Scholar] [CrossRef]
- Netten, A.P.; Rieffe, C.; Theunissen, S.C.; Soede, W.; Dirks, E.; Korver, A.M.; Konings, S.; Oudesluys-Murphy, A.M.; Dekker, F.W.; Frijns, J.H.; et al. Early identification: Language skills and social functioning in deaf and hard of hearing preschool children. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 2221–2226. [Google Scholar] [CrossRef] [PubMed]
- Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar] [CrossRef]
- Yoshinaga-Itano, C.; Sedey, A.L.; Mason, C.A.; Wiggin, M.; Chung, W. Early Intervention, Parent Talk, and Pragmatic Language in Children With Hearing Loss. Pediatrics 2020, 146, S270–S277. [Google Scholar] [CrossRef]
- Goberis, D.; Beams, D.; Dalpes, M.; Abrisch, A.; Baca, R.; Yoshinaga-Itano, C. The missing link in language development of deaf and hard of hearing children: Pragmatic language development. Semin. Speech Lang. 2012, 33, 297–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antia, S.D.; Kreimeyer, K.H. The generalization and maintenance of the peer social behaviors of young children who are deaf or hard of hearing. Lang. Speech Hear. Serv. Sch. 1997, 28, 59–69. [Google Scholar] [CrossRef]
- Freni, F.; Gazia, F.; Slavutsky, V.; Scherdel, E.P.; Nicenboim, L.; Posada, R.; Portelli, D.; Galletti, B.; Galletti, F. Cochlear Implant Surgery: Endomeatal Approach versus Posterior Tympanotomy. Int. J. Environ. Res. Public Health 2020, 17, 4187. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | No. of Participants (%) | |
|---|---|---|
| Sex | ||
| Female | 74 (51.4%) | |
| Male | 70 (48.6%) | |
| Hearing device | ||
| Hearing aid (HA) | 102 (70.8%) | |
| Cochlear implant (CI) | 42 (29.2%) | |
| Degree of hearing loss | ||
| ≤40 dB HL (mild) | 33 (22.9%) | |
| 41–60 dB HL (moderate) | 50 (34.7%) | |
| 61–80 dB HL (severe) | 18 (12.5%) | |
| ≥80 dB HL (profound) | 43 (29.9%) | |
| Age at first HA fitting (months) | ||
| Mean (SD) | 11.7 (11.1) | |
| Median | 6.2 | |
| Interquartile range | 2.9–20.3 | |
| Age at first CI (months) | ||
| Mean (SD) | 26.2 (17.4) | |
| Median | 20.5 | |
| Interquartile range | 12.5–38.1 | |
| Primary mode of communication | ||
| Oral only | 132 (91.7%) | |
| Mixed (spoken and sign-supported) | 12 (8.3%) | |
| Education setting | ||
| Mainstream | 123 (85.4%) | |
| Special | 5 (3.5%) | |
| Unknown | 16 (11.1%) | |
| Maternal education | ||
| University or Diploma | 62 (43.1%) | |
| Diploma/certificate | 46 (31.9%) | |
| 12 years or less of schooling | 36 (25.0%) |
| Measure | Scale | Normative | All Participants | HA (n = 102) | CI (n = 42) | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Nonverbal IQ | ||||||
| WNV | Full scale | 100 (15) | 99.9 (13.5) | 99.1 (14.8) | 101.6 (9.8) | |
| Language | ||||||
| CELF-4 | ReLang | 100 (15) | 84.3 (15.0) | 83.9 (15.3) | 85.1 (14.5) | |
| ExLang | 100 (15) | 84.6 (20.0) | 85.0 (19.7) | 83.6 (20.8) | ||
| Functional auditory performance | ||||||
| PEACH | Total score @ | 87.0 (13.2) | 78.4 (13.1) | 76.4 (13.6) | 83.1 (10.7) | |
| Pragmatic use of language | ||||||
| CCC-2 | Global composite score # | >45 | 57.5 (25.0) | 56.7 (25.1) | 59.6 (25.0) | |
| Speech intelligibility rating | ||||||
| SIR | Rating $ | 1.1 (0.3) | 1.6 (0.8) | 1.6 (0.9) | 1.5 (0.8) | |
| Quality of life | ||||||
| PedsQL | Total ^ | 81.3 (15.9) | 76.5 (14.4) | 75.5 (14.6) | 78.8 (13.7) | |
| Physical ^ | 83.3 (20.0) | 88.8 (18.3) | 88.3 (17.8) | 90.0 (19.6) | ||
| Psychosocial ^ | 80.2 (15.8) | 74.8 (15.7) | 73.6 (16.3) | 77.8 (14.0) | ||
| Emotional ^ | 80.3 (17.0) | 72.9 (18.3) | 73.0 (18.5) | 72.7 (17.9) | ||
| Social ^ | 82.2 (20.1) | 78.2 (20.2) | 77.2 (21.7) | 80.8 (16.1) | ||
| School ^ | 76.9 (20.2) | 73.2 (18.7) | 70.5 (18.8) | 79.8 (16.8) | ||
| Behavior and emotion | ||||||
| SDQ | Total * | −0.12 (1.0) | −0.20 (1.0) | 0.07 (0.9) | ||
| Emotion * | 0.25 (0.98) | 0.27 (1.0) | 0.23 (1.0) | |||
| Conduct * | −0.10 (1.0) | −0.18 (1.1) | 0.10 (0.9) | |||
| Hyperactivity * | −0.29 (1.1) | −0.37 (1.1) | −0.09 (1.0) | |||
| Peer Problem * | −0.22 (1.0) | −0.31 (1.0) | 0.01 (1.1) | |||
| Prosocial * | 0.02 (1.0) | −0.11 (1.0) | 0.32 (0.9) | |||
| AgeFit | BE4FA | IQ | PEACH | SIR | GCC | ReLang | ExLang | PHY | EMOF | SOCF | SCHF | PSYSOC | QOLT | EMO | CON | HYP | PEER | PROS | SDQT | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AgeFit | 1.00 | |||||||||||||||||||
| BE4FA | −0.17 | 1.00 | ||||||||||||||||||
| IQ | −0.07 | 0.08 | 1.00 | |||||||||||||||||
| PEACH | −0.10 | 0.14 | 0.16 | 1.00 | ||||||||||||||||
| SIR | 0.11 | −0.05 | −0.28 ** | −0.18 | 1.00 | |||||||||||||||
| GCC | −0.17 | 0.04 | 0.28 ** | 0.52 ** | −0.37 ** | 1.00 | ||||||||||||||
| ReLang | −0.19 | −0.04 | 0.54 ** | 0.20 | −0.52 ** | 0.49 ** | 1.00 | |||||||||||||
| ExLang | −0.20 | −0.06 | 0.41 ** | 0.28 * | −0.50 ** | 0.61 ** | 0.84 ** | 1.00 | ||||||||||||
| PHY | 0.05 | 0.06 | 0.16 | 0.28 * | −0.18 | 0.32 ** | 0.18 | 0.21 | 1.00 | |||||||||||
| EMOF | 0.01 | 0.06 | 0.15 | 0.32 ** | −0.04 | 0.19 | 0.09 | 0.08 | 0.34 ** | 1.00 | ||||||||||
| SOCF | −0.04 | 0.07 | 0.15 | 0.40 ** | −0.15 | 0.39 ** | 0.18 | 0.18 | 0.56 ** | 0.51 ** | 1.00 | |||||||||
| SCHF | −0.08 | 0.23 ** | 0.22 ** | 0.47 ** | −0.16 | 0.49 ** | 0.29 ** | 0.31 ** | 0.52 ** | 0.44 ** | 0.60 ** | 1.00 | ||||||||
| PSYSOC | −0.04 | 0.15 | 0.21 | 0.48 ** | −0.14 | 0.43 ** | 0.23 * | 0.23 | 0.57 ** | 0.78 ** | 0.86 ** | 0.82 ** | 1.00 | |||||||
| QOLT | −0.01 | 0.12 | 0.21 | 0.45 ** | −0.18 | 0.44 ** | 0.24 * | 0.25 | 0.83 ** | 0.65 ** | 0.84 ** | 0.80 ** | 0.93 ** | 1.00 | ||||||
| EMO | −0.02 | 0.05 | 0.09 | 0.33 ** | −0.09 | 0.29 ** | 0.09 | 0.10 | 0.30 ** | 0.64 ** | 0.34 ** | 0.42 ** | 0.56 ** | 0.50 ** | 1.00 | |||||
| CON | −0.03 | 0.17 | 0.25 ** | 0.37 ** | −0.11 | 0.29 ** | 0.21 | 0.22 | 0.25 * | 0.36 ** | 0.35 ** | 0.41 ** | 0.45 ** | 0.41 ** | 0.28 * | 1.00 | ||||
| HYP | −0.01 | 0.16 | 0.34 ** | 0.35 ** | −0.15 | 0.46 ** | 0.26 * | 0.27 | 0.19 | 0.30 ** | 0.31 ** | 0.61 ** | 0.49 ** | 0.42 ** | 0.35 ** | 0.46 ** | 1.00 | |||
| PEER | −0.09 | 0.14 | 0.15 | 0.34 ** | −0.23 * | 0.36 ** | 0.23 * | 0.25 | 0.37 ** | 0.42 ** | 0.66 ** | 0.47 ** | 0.63 ** | 0.60 ** | 0.36 ** | 0.52 ** | 0.37 ** | 1.00 | ||
| PROS | −0.20 | 0.22 ** | 0.19 | 0.37 ** | −0.18 | 0.34 ** | 0.12 | 0.22 | 0.17 | 0.20 * | 0.25 * | 0.30 ** | 0.30 ** | 0.28 * | 0.19 | 0.53 ** | 0.32 ** | 0.43 ** | 1.00 | |
| SDQT | −0.05 | 0.18 | 0.29 ** | 0.47 ** | −0.20 | 0.49 ** | 0.27 * | 0.29 ** | 0.37 ** | 0.58 ** | 0.56 ** | 0.66 ** | 0.73 ** | 0.65 ** | 0.67 ** | 0.73 ** | 0.79 ** | 0.75 ** | 0.49 ** | 1.00 |
| SDQT | EMO | CON | HYP | PEER | PROS | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | |
| AgeFit | 0.05 | (−0.09, 0.20) | 0.45 | 0.02 | (−0.14, 0.18) | 0.84 | 0.05 | (−0.11, 0.21) | 0.51 | 0.08 | (−0.07, 0.23) | 0.27 | 0.001 | (−0.16, 0.16) | 0.99 | −0.13 | (−0.29, 0.02) | 0.09 |
| BE4FA | 0.47 | (0.16, 0.78) | 0.003 | 0.45 | (0.10, 0.80) | 0.01 | 0.42 | (0.07, 0.76) | 0.018 | 0.33 | (0.01, 0.66) | 0.04 | 0.20 | (−0.15, 0.55) | 0.26 | 0.22 | (−0.12, 0.56) | 0.20 |
| Device | 0.40 | (0.08, 0.71) | 0.01 | 0.52 | (0.15, 0.88) | 0.005 | 0.33 | (−0.13, 0.68) | 0.07 | 0.24 | (−0.09, 0.57) | 0.16 | 0.11 | (−0.25, 0.47) | 0.55 | 0.09 | (−0.26, 0.44) | 0.61 |
| IQ | 0.13 | (−0.03, 0.30) | 0.11 | −0.01 | (−0.19, 0.18) | 0.95 | 0.14 | (−0.04, 0.32) | 0.14 | 0.23 | (0.05, 0.40) | 0.01 | 0.001 | (−0.18, 0.19) | 0.99 | 0.15 | (−0.03, 0.33) | 0.09 |
| ReLg | 0.13 | (−0.15, 0.42) | 0.36 | 0.17 | (−0.16, 0.50) | 0.31 | 0.11 | (−0.21, 0.44) | 0.48 | 0.05 | (−0.12, 0.22) | 0.75 | 0.07 | (−0.24, 0.40) | 0.65 | −0.32 | (−0.63, 0.00) | 0.05 |
| ExpLg | −0.13 | (−0.41, 0.16) | 0.38 | −0.25 | (−0.57, 0.07) | 0.13 | −0.01 | (−0.33, 0.30) | 0.94 | −0.06 | (−0.36, 0.24) | 0.68 | −0.03 | (−0.36, 0.29) | 0.84 | 0.22 | (−0.09, 0.53) | 0.16 |
| GCC | 0.29 | (0.10, 0.49) | 0.004 | 0.19 | (−0.03, 0.41) | 0.09 | 0.06 | (−0.16, 0.27) | 0.6 | 0.35 | (0.15, 0.55) | <0.001 | 0.20 | (−0.03, 0.42) | 0.08 | 0.14 | (−0.07, 0.36) | 0.19 |
| PEACH | 0.33 | (0.17, 0.50) | <0.001 | 0.31 | (0.12, 0.50) | 0.002 | 0.32 | (0.14, 0.51) | <0.001 | 0.17 | (−0.01, 0.34) | 0.06 | 0.21 | (0.02, 0.40) | 0.03 | 0.23 | (0.05, 0.41) | 0.01 |
| SIR | −0.01 | (−0.18, 0.15) | 0.87 | −0.04 | (−0.22, 0.15) | 0.69 | 0.04 | (−0.14, 0.22) | 0.65 | 0.05 | (−0.12, 0.22) | 0.55 | 0.11 | (−0.25, 0.47) | 0.55 | −0.08 | (−0.26, 0.09) | 0.36 |
| Adj R2 | 0.332 | 0.129 | 0.166 | 0.262 | 0.135 | 0.194 |
| QOLT | PSYSOC | SCHF | SOCF | EMOF | PHY | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | Est | (95% CI) | p-Value | |
| AgeFit | 0.08 | (−0.06, 0.23) | 0.26 | 0.05 | (−0.10, 0.20) | 0.52 | 0.05 | (−0.10, 0.19) | 0.51 | 0.03 | (−0.13, 0.19) | 0.7 | 0.04 | (−0.13, 0.20) | 0.67 | 0.12 | (−0.05, 0.28) | 0.16 |
| BE4FA | 0.29 | (−0.03, 0.62) | 0.08 | 0.34 | (0.02, 0.66) | 0.04 | 0.28 | (−0.03, 0.60) | 0.08 | 0.11 | (−0.23, 0.46) | 0.52 | 0.46 | (0.10, 0.82) | 0.01 | 0.22 | (−0.14, 0.58) | 0.22 |
| Device | 0.25 | (−0.08, 0.59) | 0.14 | 0.29 | (−0.04, 0.62) | 0.09 | 0.1 | (−0.22, 0.42) | 0.53 | 0.11 | (−0.25, 0.46) | 0.55 | 0.52 | (0.15, 0.88) | 0.006 | 0.2 | (−0.17, 0.57) | 0.28 |
| IQ | 0.06 | (−0.12, 0.23) | 0.53 | 0.05 | (−0.12, 0.22) | 0.56 | 0.02 | (−0.15, 0.19) | 0.82 | 0.03 | (−0.15, 0.21) | 0.74 | 0.08 | (−0.11, 0.27) | 0.42 | 0.05 | (−0.14, 0.24) | 0.63 |
| ReLg | 0.16 | (−0.15, 0.46) | 0.31 | 0.21 | (−0.10, 0.51) | 0.18 | 0.2 | (−0.10, 0.49) | 0.18 | 0.12 | (−0.21, 0.44) | 0.47 | 0.20 | (−0.13, 0.53) | 0.23 | 0.03 | (−0.30, 0.37) | 0.84 |
| ExpLg | −0.14 | (−0.44, 0.16) | 0.36 | −0.19 | (−0.48, 0.11) | 0.21 | −0.07 | (−0.36, 0.22) | 0.63 | −0.17 | (−0.49, 0.14) | 0.28 | −0.22 | (−0.55, 0.10) | 0.18 | −0.01 | (−0.34, 0.32) | 0.93 |
| GCC | 0.27 | (0.06, 0.48) | 0.01 | 0.25 | (0.05, 0.46) | 0.02 | 0.30 | (0.10, 0.50) | 0.003 | 0.28 | (0.06, 0.50) | 0.01 | 0.03 | (−0.19, 0.26) | 0.78 | 0.21 | (−0.02, 0.43) | 0.07 |
| PEACH | 0.33 | (0.16, 0.51) | <0.001 | 0.38 | (0.20, 0.55) | <0.001 | 0.29 | (0.12, 0.46) | <0.001 | 0.28 | (0.09, 0.46) | 0.004 | 0.370 | (0.18, 0.57) | 0.004 | 0.180 | (−0.02, 0.37) | 0.080 |
| SIR | −0.01 | (−0.19, 0.16) | 0.87 | 0.02 | (−0.14, 0.19) | 0.78 | 0.07 | (−0.10, 0.23) | 0.42 | −0.02 | (−0.20, 0.16) | 0.82 | 0.01 | (−0.17, 0.20) | 0.88 | −0.07 | (−0.26, 0.12) | 0.45 |
| Adj R2 | 0.249 | 0.268 | 0.308 | 0.160 | 0.114 | 0.094 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ching, T.Y.C.; Cupples, L.; Leigh, G.; Hou, S.; Wong, A. Predicting Quality of Life and Behavior and Emotion from Functional Auditory and Pragmatic Language Abilities in 9-Year-Old Deaf and Hard-of-Hearing Children. J. Clin. Med. 2021, 10, 5357. https://doi.org/10.3390/jcm10225357
Ching TYC, Cupples L, Leigh G, Hou S, Wong A. Predicting Quality of Life and Behavior and Emotion from Functional Auditory and Pragmatic Language Abilities in 9-Year-Old Deaf and Hard-of-Hearing Children. Journal of Clinical Medicine. 2021; 10(22):5357. https://doi.org/10.3390/jcm10225357
Chicago/Turabian StyleChing, Teresa Y. C., Linda Cupples, Greg Leigh, Sanna Hou, and Angela Wong. 2021. "Predicting Quality of Life and Behavior and Emotion from Functional Auditory and Pragmatic Language Abilities in 9-Year-Old Deaf and Hard-of-Hearing Children" Journal of Clinical Medicine 10, no. 22: 5357. https://doi.org/10.3390/jcm10225357
APA StyleChing, T. Y. C., Cupples, L., Leigh, G., Hou, S., & Wong, A. (2021). Predicting Quality of Life and Behavior and Emotion from Functional Auditory and Pragmatic Language Abilities in 9-Year-Old Deaf and Hard-of-Hearing Children. Journal of Clinical Medicine, 10(22), 5357. https://doi.org/10.3390/jcm10225357








