Ground Reaction Forces during Vertical Hops Are Correlated with the Number of Supervised Physiotherapy Visits after Achilles Tendon Surgery
Abstract
1. Introduction
2. Materials and Methods
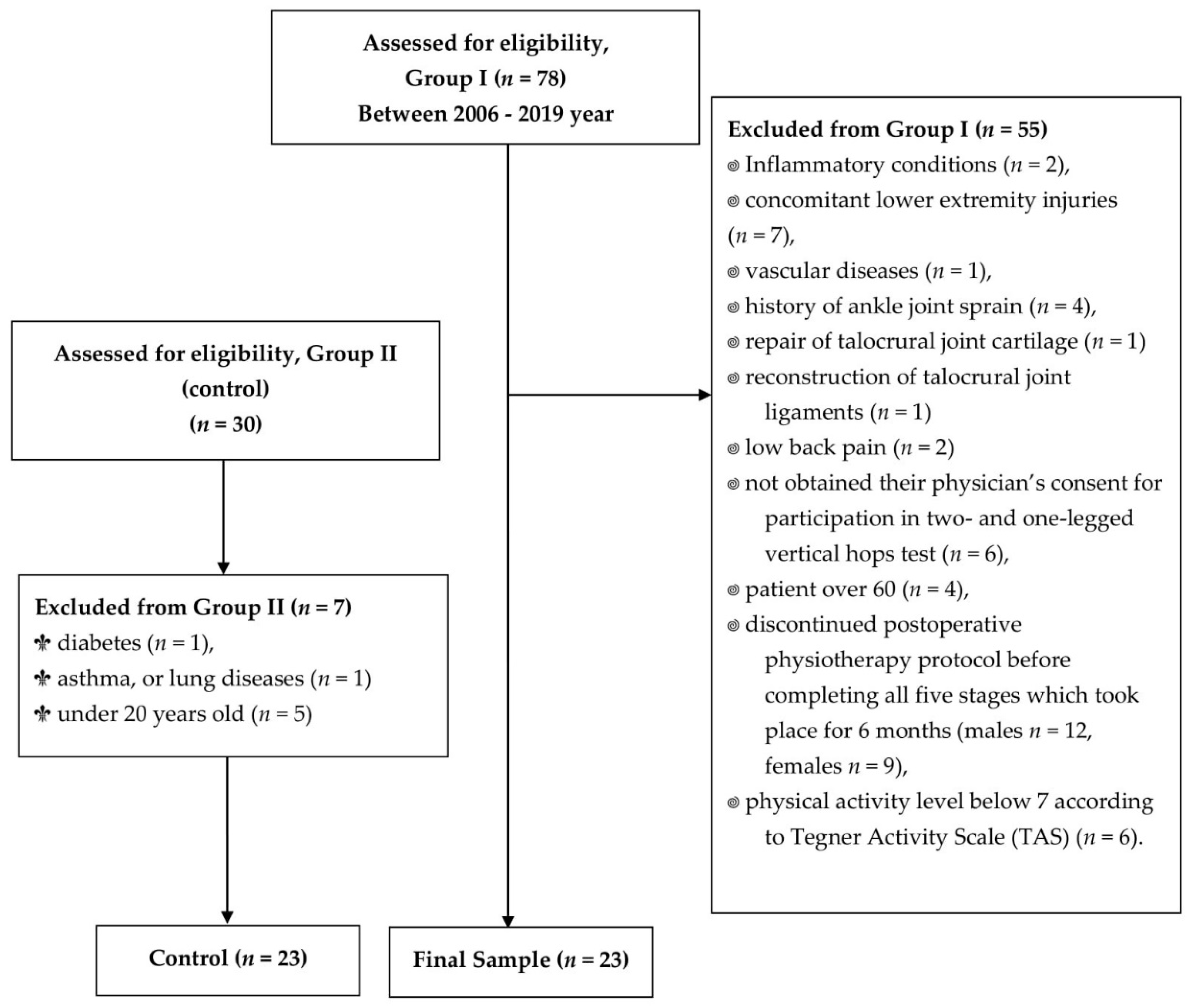
2.1. Participants
2.2. Postoperative Physiotherapy
2.3. Clinical Trial
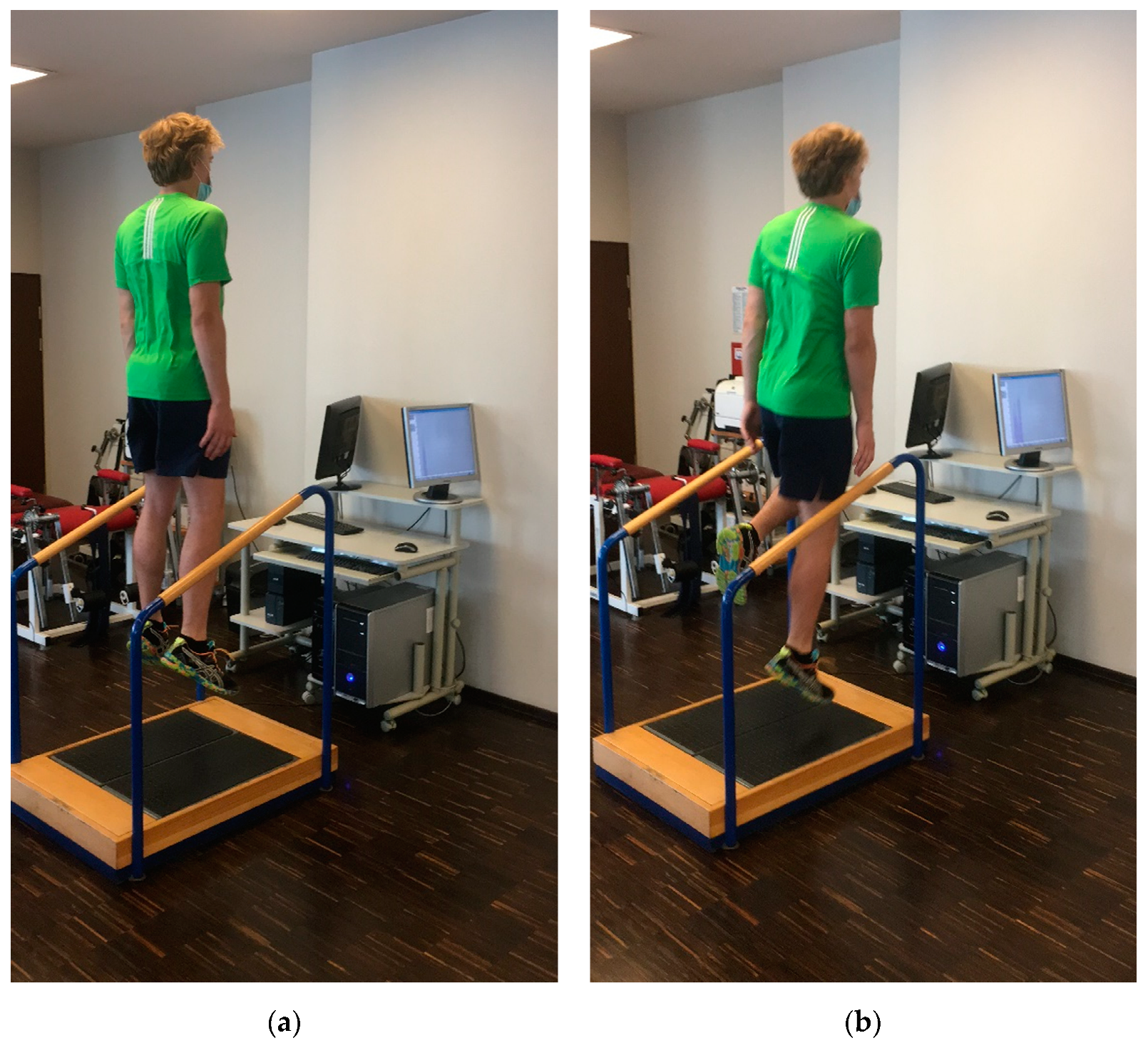
2.4. Measurements of the Vertical Ground Reaction Forces Component
2.5. Measurements of Circumferences of Ankle Joint and Shin and Range of Motion of the Foot
2.6. Statistical Analysis
3. Results
3.1. Comparison of Pain Assessment, Thompson’s Test Results, 10 m Unassisted Walking, Obtained Ankle Joint and Shin Circumferences, and Range of Motion (ROM) of the Foot in the Between-Limb and Between-Group Analyses
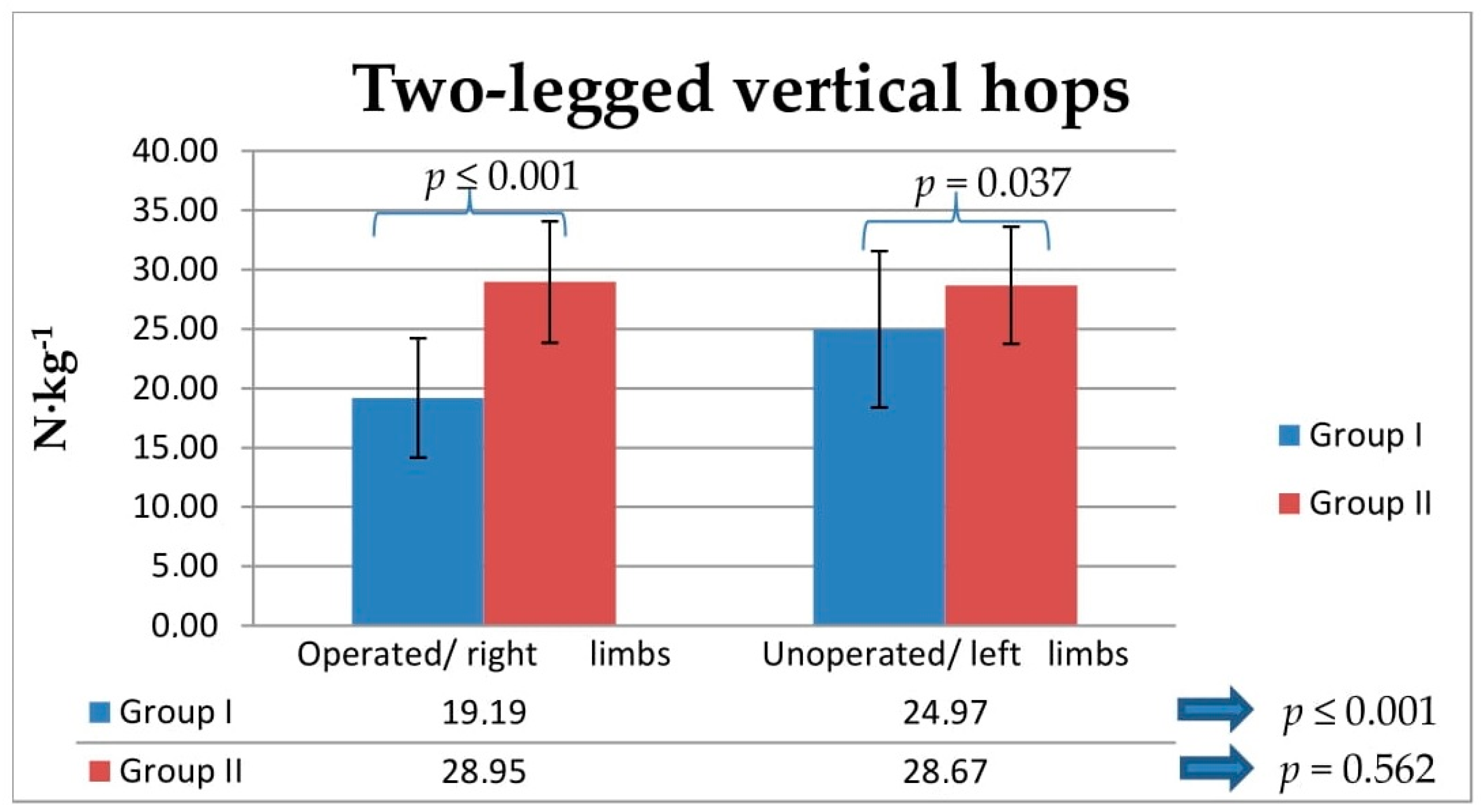
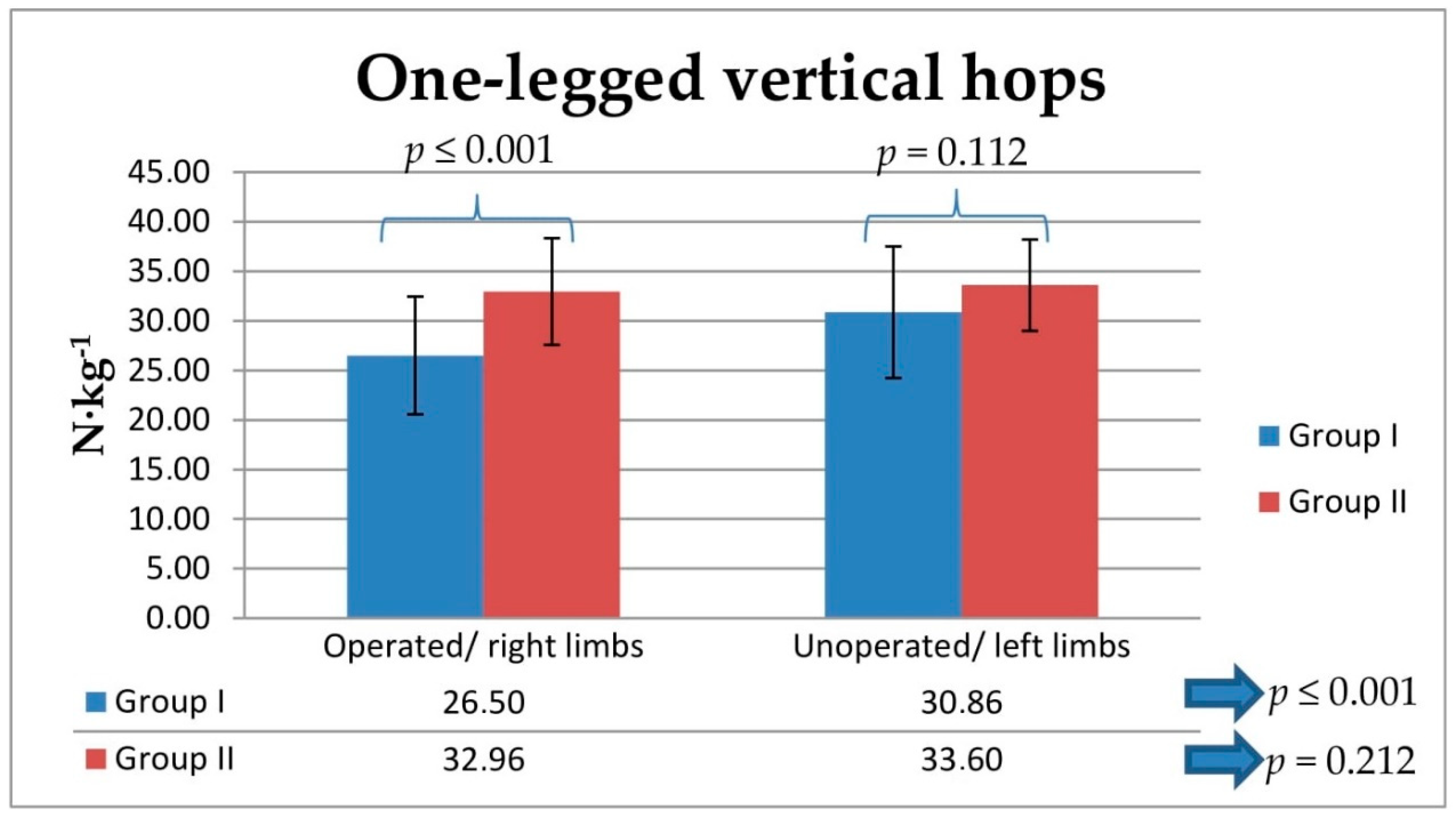
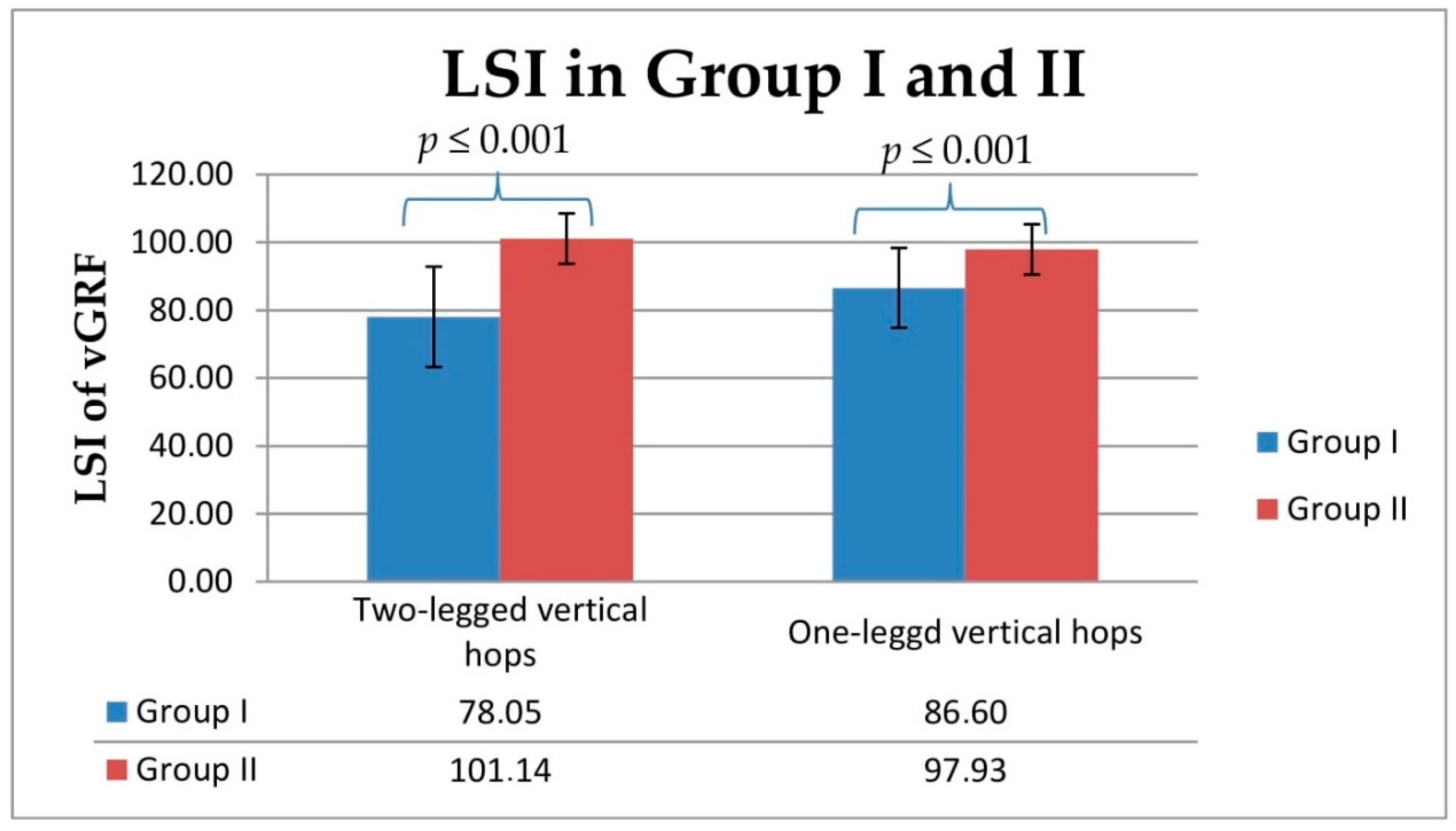
3.2. Comparison of Obtained Relative Vertical Ground Reaction Force during Two- and One-Legged Vertical Hops and Their LSI in the Between-Limb and Between-Group Analyses
3.3. Association of Number of Supervised Postoperative Physiotherapy Visits with Relative Vertical Ground Reaction Forces and Limb Symmetry Index (LSI) of Vertical Ground Reaction Forces during Two- and One-Legged Vertical Hops
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malvankar, S.; Khan, W. Evolution of the Achilles tendon: The athlete’s Achilles heel? Foot 2011, 21, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Longo, U.G.; Maffulli, G.D.; Khanna, A.; Denaro, V. Achilles Tendon Ruptures in Elite Athletes. Foot Ankle Int. 2011, 32, 9–15. [Google Scholar] [CrossRef]
- Egger, A.C.; Berkowitz, M.J. Achilles tendon injuries. Curr. Rev. Musculoskelet. Med. 2017, 10, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Via, A.G.; Oliva, F. Chronic Achilles Tendon Rupture. Open Orthop. J. 2017, 11, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Chianca, V.; Zappia, M.; Oliva, F.; Luca, B.; Maffulli, N. Post-operative MRI and US appearance of the Achilles tendons. J. Ultrasound 2020, 23, 387–395. [Google Scholar] [CrossRef]
- Romero-Morales, C.; Martín-Llantino, P.J.; Calvo-Lobo, C.; Palomo-López, P.; López-López, D.; Pareja-Galeano, H.; Rodríguez-Sanz, D. Comparison of the sonographic features of the Achilles Tendon complex in patients with and without achilles tendinopathy: A case–control study. Phys. Ther. Sport 2019, 35, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, D.; Palermi, S.; Sirico, F.; Corrado, B. Achilles Tendon Rupture: Mechanisms of Injury, Principles of Rehabilitation and Return to Play. J. Funct. Morphol. Kinesiol. 2020, 5, 95. [Google Scholar] [CrossRef] [PubMed]
- Oliva, F.; Rugiero, C.; Via, A.G.; Baldassarri, M.; Bernardi, G.; Biz, C.; Bossa, M.; Buda, R.; Buonocore, D.; Chianca, V.; et al. IS Mu. LT Achilles tendon ruptures guidelines. Muscle Ligaments Tendons J. 2019, 8, 310. [Google Scholar] [CrossRef]
- Lantto, I.; Heikkinen, J.; Flinkkila, T.; Ohtonen, P.; Siira, P.; Laine, V.; Leppilahti, J. A Prospective Randomized Trial Comparing Surgical and Nonsurgical Treatments of Acute Achilles Tendon Ruptures. Am. J. Sports Med. 2016, 44, 2406–2414. [Google Scholar] [CrossRef]
- Maffulli, G.; Del Buono, A.; Richards, P.; Oliva, F.; Maffulli, N. Conservative, minimally invasive and open surgical repair for management of acute ruptures of the Achilles tendon: A clinical and functional retrospective study. Muscle Ligaments Tendons J. 2017, 7, 46–52. [Google Scholar] [CrossRef]
- Maffulli, N.; D’Addona, A.; Maffulli, G.D.; Gougoulias, N.; Oliva, F. Delayed (14–30 Days) Percutaneous Repair of Achilles Tendon Ruptures Offers Equally Good Results as Compared with Acute Repair. Am. J. Sports Med. 2020, 48, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-H.; Lee, H.S.; Young, K.W.; Seo, S.G. Treatment of Acute Achilles Tendon Rupture. Clin. Orthop. Surg. 2020, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, R.; Imaya, T.; Katsuki, S.; Sanada, T.; Fukai, A.; Honda, E.; Yoshitomi, H. Factors Associated to Return to Sport after Surgical Repair of Achilles Tendon Ruptures. A Clinical and Functional Retrospective Study. Muscle Ligaments Tendons J. 2021, 11, 584. [Google Scholar] [CrossRef]
- Yang, X.; Meng, H.; Quan, Q.; Peng, J.; Lu, S.; Wang, A. Management of acute Achilles tendon ruptures. Bone Jt. Res. 2018, 7, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.D.; Shadbolt, B. Randomized controlled trial of accelerated rehabilitation versus standard protocol following surgical repair of ruptured Achilles tendon. ANZ J. Surg. 2014, 85, 373–377. [Google Scholar] [CrossRef]
- Zhao, J.-G.; Meng, X.-H.; Liu, L.; Zeng, X.-T.; Kan, S.-L. Early functional rehabilitation versus traditional immobilization for surgical Achilles tendon repair after acute rupture: A systematic review of overlapping meta-analyses. Sci. Rep. 2017, 7, 39871. [Google Scholar] [CrossRef]
- Gould, H.P.; Bano, J.M.; Akman, J.L.; Fillar, A.L. Postoperative Rehabilitation Following Achilles Tendon Repair: A Systematic Review. Sports Med. Arthrosc. Rev. 2021, 29, 130–145. [Google Scholar] [CrossRef]
- Gruber, J.; Giza, E.; Zachazewski, J.; Mandelbaum, B.R. Achilles Tendon Repair and Rehabilitation. Rehabilitation for the Postsurgical Orthopedic Patient, 3rd ed.; Maxey, L., Magnusson, J., Eds.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 554–578. [Google Scholar] [CrossRef]
- Czamara, A. Physiotherapeutic Treatments after Surgery of Total Achilles Tendon Rupture. J. Orthop. Trauma Surg. Relat. Res. 2007, 1, 75–93. [Google Scholar]
- Schenck, R.C.; Blaschak, M.; Lance, E.D.; Turturro, T.C.; Holmes, C.F. A prospective outcome study of rehabilitation programs and anterior cruciate ligament reconstruction. Arthrosc. J. Arthrosc. Relat. Surg. 1997, 13, 285–290. [Google Scholar] [CrossRef]
- Huang, J.; Wang, C.; Ma, X.; Wang, X.; Zhang, C.; Chen, L. Rehabilitation Regimen After Surgical Treatment of Acute Achilles Tendon Ruptures: A systematic review with meta-analysi. Am. J. Sports Med. 2014, 43, 1008–1016. [Google Scholar] [CrossRef]
- Królikowska, A.; Sikorski, Ł.; Czamara, A.; Reichert, P. Effects of Postoperative Physiotherapy Supervision Duration on Clinical Outcome, Speed, and Agility in Males 8 Months After Anterior Cruciate Ligament Reconstruction. Med. Sci. Monit. 2018, 24, 6823–6831. [Google Scholar] [CrossRef] [PubMed]
- Ebert, J.R.; Edwards, P.; Yi, L.; Joss, B.; Ackland, T.; Carey-Smith, R.; Buelow, J.-U.; Hewitt, B. Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 2353–2361. [Google Scholar] [CrossRef] [PubMed]
- Glazebrook, M.; Rubinger, D. Functional Rehabilitation for Nonsurgical Treatment of Acute Achilles Tendon Rupture. Foot Ankle Clin. 2019, 24, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Dams, O.C.; Akker-Scheek, I.V.D.; Diercks, R.L.; Wendt, K.W.; Bosma, E.; Van Raaij, T.M.; Munzebrock, A.V.; Zijlstra, W.P.; Zwerver, J.; Reininga, I.H.F. The recovery after Achilles tendon rupture: A protocol for a multicenter prospective cohort study. BMC Musculoskelet. Disord. 2019, 20, 69. [Google Scholar] [CrossRef] [PubMed]
- Zellers, J.A.; Carmont, M.R.; Silbernagel, K.G. Return to play post-Achilles tendon rupture: A systematic review and meta-analysis of rate and measures of return to play. Br. J. Sports Med. 2016, 50, 1325–1332. [Google Scholar] [CrossRef] [PubMed]
- Olsson, N.; Nilsson-Helander, K.; Karlsson, J.; Eriksson, B.I.; Thomée, R.; Faxén, E.; Silbernagel, K.G. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1385–1393. [Google Scholar] [CrossRef]
- Willy, R.W.; Brorsson, A.; Powell, H.C.; Willson, J.; Tranberg, R.; Silbernagel, K.G. Elevated Knee Joint Kinetics and Reduced Ankle Kinetics Are Present During Jogging and Hopping After Achilles Tendon Ruptures. Am. J. Sports Med. 2017, 45, 1124–1133. [Google Scholar] [CrossRef]
- Jandacka, D.; Plesek, J.; Skypala, J.; Uchytil, J.; Silvernail, J.F.; Hamill, J. Knee Joint Kinematics and Kinetics During Walking and Running After Surgical Achilles Tendon Repair. Orthop. J. Sports Med. 2018, 6, 2325967118779862. [Google Scholar] [CrossRef]
- Nilsson-Helander, K.; Silbernagel, K.G.; Thomeé, R.; Faxén, E.; Olsson, N.; Eriksson, B.I.; Karlsson, J. Acute Achilles Tendon Rupture. Am. J. Sports Med. 2010, 38, 2186–2193. [Google Scholar] [CrossRef]
- Wearing, S.C.; Kuhn, L.; Pohl, T.; Horstmann, T.; Brauner, T. Transmission-Mode Ultrasound for Monitoring the Instantaneous Elastic Modulus of the Achilles Tendon During Unilateral Submaximal Vertical Hopping. Front. Physiol. 2020, 11, 1579. [Google Scholar] [CrossRef]
- Van Meer, B.L.; Meuffels, D.E.; Reijman, M. A Comparison of the Standardized Rating Forms for Evaluation of Anterior Cruciate Ligament Injured or Reconstructed Patients. In The Anterior Cruciate Ligament: Reconstruction and Basic Science, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 484–489.e2. [Google Scholar] [CrossRef]
- Henríquez, H.; Muñoz, R.; Carcuro, G.; Bastías, C. Is Percutaneous Repair Better Than Open Repair in Acute Achilles Tendon Rupture? Clin. Orthop. Relat. Res. 2012, 470, 998–1003. [Google Scholar] [CrossRef]
- Czamara, A. Biomechanical assessment of unilateral and bilateral landing symmetry during rehabilitation following anterior cruciate ligament reconstruction (ACLR). Pol. J. Sports Med. 2011, 27, 183–194. [Google Scholar] [CrossRef]
- Baechle, T.R.; Earle, R.W. Essentials of Strength Training and Conditioning, 3rd ed.; National Strength & Conditioning Association: Champain, IL, USA, 2008; pp. 413–457. [Google Scholar]
- Królikowska, A.; Czamara, A.; Szuba, Ł.; Reichert, P. The Effect of Longer versus Shorter Duration of Supervised Physiotherapy after ACL Reconstruction on the Vertical Jump Landing Limb Symmetry. BioMed Res. Int. 2018, 2018, 7519467. [Google Scholar] [CrossRef] [PubMed]
- Matheson, A.L.; Duffy, S.; Maroof, A.; Gibbons, R.; Duffy, C.; Roth, J. Intra- and inter-rater reliability of jumping mechanography muscle function assessments. J. Musculoskelet Neuronal Interact. 2013, 13, 480–486. [Google Scholar] [PubMed]
- Sikorski, Ł.; Czamara, A. Assessment of Effectiveness of 15 Weeks of Physical Therapy on Biplanar Ankle Mobility, Gait and Pain Level in Patients Following Operative Repair of the Achilles Tendon. Ortop. Traumatol. Rehabil. 2021, 23, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Kuo, A.D. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Hum. Mov. Sci. 2007, 26, 617–656. [Google Scholar] [CrossRef]
- Somford, M.P.; Hoornenborg, D.; Wiegerinck, J.I.; Weme, R.A.N. Are You Positive That the Simmonds-Thompson Test Is Negative? A Historical and Biographical Review. J. Foot Ankle Surg. 2016, 55, 682–683. [Google Scholar] [CrossRef][Green Version]
- Mukaka, M.M. Statistics corner: A guide to the appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Tengman, T.; Riad, J. Three-Dimensional Gait Analysis Following Achilles Tendon Rupture with Nonsurgical Treatment Reveals Long-Term Deficiencies in Muscle Strength and Function. Orthop. J. Sports Med. 2013, 1, 1–9. [Google Scholar] [CrossRef]
- Burdett, R.G. Forces predicted at the ankle during running. Med. Sci. Sports Exerc. 1982, 14, 308–316. [Google Scholar] [CrossRef]
- Powell, H.C.; Silbernagel, K.G.; Brorsson, A.; Tranberg, R.; Willy, R. Individuals Post Achilles Tendon Rupture Exhibit Asymmetrical Knee and Ankle Kinetics and Loading Rates During a Drop Countermovement Jump. J. Orthop. Sports Phys. Ther. 2018, 48, 34–43. [Google Scholar] [CrossRef]
- Thomopoulos, S.; Parks, W.C.; Rifkin, D.B.; Derwin, K.A. Mechanisms of tendon injury and repair. J. Orthop. Res. 2015, 33, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Brumann, M.; Baumbach, S.; Mutschler, W.; Polzer, H. Accelerated rehabilitation following Achilles tendon repair after acute rupture—Development of an evidence-based treatment protocol. Injury 2014, 45, 1782–1790. [Google Scholar] [CrossRef] [PubMed]
- Zellers, J.A.; Christensen, M.; Kjær, I.L.; Rathleff, M.S.; Silbernagel, K.G. Defining Components of Early Functional Rehabilitation for Acute Achilles Tendon Rupture: A Systematic Review. Orthop. J. Sports Med. 2019, 7, 2325967119884071. [Google Scholar] [CrossRef] [PubMed]
- Mark-Christensen, T.; Troelsen, A.; Kallemose, T.; Barfod, K.W. Functional rehabilitation of patients with acute Achilles tendon rupture: A meta-analysis of current evidence. Knee Surg. Sports Traumatol. Arthrosc. 2014, 24, 1852–1859. [Google Scholar] [CrossRef]
- Ryu, C.H.; Lee, H.S.; Seo, S.G.; Kim, H.Y. Results of tenorrhaphy with early rehabilitation for acute tear of Achilles tendon. J. Orthop. Surg. 2018, 26, 2309499018802483. [Google Scholar] [CrossRef]
- Hutchison, A.M.; Topliss, C.; Beard, D.; Evans, R.M.; Williams, P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Jt. J. 2015, 97, 510–515. [Google Scholar] [CrossRef]
- Kadakia, A.R.; Short, K.; Myerson, M.S. Rehabilitation After Acute Ruptures of the Achilles Tendon. In The Achilles Tendon: Treatment and Rehabilitation; Springer: New York, NY, USA, 2008; pp. 93–105. [Google Scholar] [CrossRef]
- Zellers, J.A.; Marmon, A.R.; Ebrahimi, A.; Silbernagel, K.G. Lower extremity work along with triceps surae structure and activation is altered with jumping after Achilles tendon repair. J. Orthop. Res. 2019, 37, 933–941. [Google Scholar] [CrossRef]
- Carmont, M.R.; Brorsson, A.; Karlsson, J.; Nilsson-Helander, K. No difference in Achilles Tendon Resting Angle, Patient-reported outcome or Heel-rise height Index between Non- and Early weightbearing the First Year after an Achilles Tendon Rupture. Muscle Ligaments Tendons J. 2020, 10, 651. [Google Scholar] [CrossRef]
- Czamara, A.; Krzemińska, K.; Widuchowski, W.; Dragan, S.L. The Muscle Strength of the Knee Joint after ACL Reconstruction Depends on the Number and Frequency of Supervised Physiotherapy Visits. Int. J. Environ. Res. Public Health 2021, 18, 10588. [Google Scholar] [CrossRef]
- Królikowska, A.; Czamara, A.; Reichert, P. Between-Limb Symmetry during Double-Leg Vertical Hop Landing in Males an Average of Two Years after ACL Reconstruction is Highly Correlated with Postoperative Physiotherapy Supervision Duration. Appl. Sci. 2018, 8, 2586. [Google Scholar] [CrossRef]
- Zwolski, C.; Schmitt, L.C.; Thomas, S.; Hewett, T.E.; Paterno, M.V. The Utility of Limb Symmetry Indices in Return-to-Sport Assessment in Patients with Bilateral Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 2030–2038. [Google Scholar] [CrossRef]
- Myer, G.D.; Paterno, M.V.; Ford, K.; Hewett, E.T. Neuromuscular Training Techniques to Target Deficits Before Return to Sport After Anterior Cruciate Ligament Reconstruction. J. Strength Cond. Res. 2008, 22, 987–1014. [Google Scholar] [CrossRef] [PubMed]
- Souissi, S.; Chaouachi, A.; Burnett, A.; Hue, O.; Bouhlel, E.; Chtara, M.; Chamari, K. Leg asymmetry and muscle function recovery after anterior cruciate ligament reconstruction in elite athletes: A pilot study on slower recovery of the dominant leg. Biol. Sport 2020, 37, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Markström, J.L.; Tengman, E.; Häger, C.K. ACL-reconstructed and ACL-deficient individuals show differentiated trunk, hip, and knee kinematics during vertical hops more than 20 years post-injury. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.C.; Hubbard-Turner, T.; Wikstrom, E.; Palmieri-Smith, R.M. Epidemiology of Posttraumatic Osteoarthritis. J. Athl. Train. 2017, 52, 491–496. [Google Scholar] [CrossRef]
- Brorsson, A.; Silbernagel, K.G.; Olsson, N.; Helander, K.N. Calf Muscle Performance Deficits Remain 7 Years After an Achilles Tendon Rupture. Am. J. Sports Med. 2017, 46, 470–477. [Google Scholar] [CrossRef]
- Markovic, G.; Mikulic, P. Neuro-Musculoskeletal and Performance Adaptations to Lower-Extremity Plyometric Training. Sports Med. 2010, 40, 859–895. [Google Scholar] [CrossRef]
- Schepull, T.; Kvist, J.; Andersson, C.; Aspenberg, P. Mechanical properties during healing of Achilles tendon ruptures to predict final outcome: A pilot Roentgen stereophotogrammetric analysis in 10 patients. BMC Musculoskelet. Disord. 2007, 8, 116. [Google Scholar] [CrossRef]
- Lamontagne, M.; Kennedy, M.J. The Biomechanics of Vertical Hopping: A Review. Res. Sports Med. 2013, 21, 380–394. [Google Scholar] [CrossRef]
| Experimental Group | I (n = 23) | II (n = 23) | p |
|---|---|---|---|
| Age (years) | 35.61 ± 8.99 | 31.87 ± 4.85 | 0.088 |
| Body mass (kg) | 87.57 ± 10.22 | 81.13 ± 11.27 | 0.019 |
| Body height (cm) | 184.65 ± 7.83 | 178.57 ± 5.58 | 0.004 |
| BMI (kg∙m−2) | 25.63 ± 1.82 | 25.36 ± 2.43 | 0.312 |
| Duration of SVPPh (months) | 6 months | n/a | – |
| Number of SVPPh sessions | 42.22 ± 15.62 | n/a | – |
| Operated leg | Right (n = 11), Left (n = 12) | Right (n = 0), Left (n = 0) | – |
| Dominant leg | Right (n = 21), Left (n = 2) | Right (n = 22), Left (n = 1) | – |
| Tested Parameters | Group | Operated/Right Legs | Unoperated/Left Legs | p |
|---|---|---|---|---|
| Pain in VAS | I | 0.00 ± 0.00 | 0.00 ± 0.00 | - |
| II | 0.00 ± 0.00 | 0.00 ± 0.00 | - | |
| p | – | – | – | |
| Negative Thomson’s test results | I | 23 | 23 | – |
| II | 23 | 23 | – | |
| p | – | – | – | |
| 10 m unassisted walking | I | 23 | 23 | – |
| II | 23 | 23 | – | |
| p | – | – | – | |
| Ankle circumference (cm) | I | 27.66 ± 1.27 | 27.24 ± 1.39 | p ≤ 0.001 |
| II | 26.91 ± 1.50 | 26.91 ± 1.50 | 1.00 | |
| p | 0.061 | 0.303 | ||
| Shine circumference (cm) | I | 38.38 ± 1.79 | 39.33 ± 1.56 | p ≤ 0.001 |
| II | 39.48 ± 5.20 | 39.26 ± 5.25 | 0.236 | |
| p | 0.574 | 0.103 | ||
| Full ROM of ankle joint in sagittal plane (°) | I | 58.26 ± 9.69 | 59.43 ± 10.51 | 0.233 |
| II | 61.89 ± 6.44 | 61.98 ± 6.40 | 0.747 | |
| p | 0.143 | 0.388 | ||
| DF ROM of ankle joint (°) | I | −14.13 ± 3.99 | 13.74 ± 8.14 | 0.572 |
| II | −14.02 ± 4.94 | −14.37 ± 4.37 | 0.213 | |
| p | 0.935 | 0.697 | ||
| PF ROM of ankle joint (°) | I | 44.13 ± 8.56 | 45.70 ± 6.64 | 0.273 |
| II | 47.87 ± 6.03 | 47.61 ± 5.40 | 0.655 | |
| p | 0.067 | 0.160 |
| ANOVA | ||||
| Operated Leg in Group I | Right Leg in Group II | Left Leg in Group II | p | |
| RvGRF–TLH (N·kg−1) | 19.19 ± 5.03 | 28.95 ± 5.12 | 28.67 ± 4.94 | p ≤ 0.001 |
| RvGRF–OLH (N·kg−1) | 26.50 ± 5.94 | 32.96 ± 5.38 | 33.60 ± 4.61 | p ≤ 0.001 |
| TUKEY’S TEST | ||||
| Assessed Groups | Assessed Legs | RvGRF–OLH (N·kg−1) | RvGRF–TLH (N·kg−1) | |
| Group I and II | Operated to Right | p ≤ 0.001 | p ≤ 0.001 | |
| Group I and II | Operated to Left | p ≤ 0.001 | p ≤ 0.001 | |
| Group II and II | Right to Left | p = 0.913 | p = 0.981 | |
| Test Correlation | RvGRF TLH Operated Leg | RvGRF TLH Unoperated Leg | RvGRF OLH Operated Leg | RvGRF OLH Unoperated Leg | LSI of vGRF TLH | LSI of vGRF OLH | |
|---|---|---|---|---|---|---|---|
| Number of SVPPh visits | r | 0.503 | 0.175 | 0.505 | 0.268 | 0.399 | 0.332 |
| p | 0.014 | 0.424 | 0.014 | 0.217 | 0.059 | 0.122 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sikorski, Ł.; Czamara, A. Ground Reaction Forces during Vertical Hops Are Correlated with the Number of Supervised Physiotherapy Visits after Achilles Tendon Surgery. J. Clin. Med. 2021, 10, 5299. https://doi.org/10.3390/jcm10225299
Sikorski Ł, Czamara A. Ground Reaction Forces during Vertical Hops Are Correlated with the Number of Supervised Physiotherapy Visits after Achilles Tendon Surgery. Journal of Clinical Medicine. 2021; 10(22):5299. https://doi.org/10.3390/jcm10225299
Chicago/Turabian StyleSikorski, Łukasz, and Andrzej Czamara. 2021. "Ground Reaction Forces during Vertical Hops Are Correlated with the Number of Supervised Physiotherapy Visits after Achilles Tendon Surgery" Journal of Clinical Medicine 10, no. 22: 5299. https://doi.org/10.3390/jcm10225299
APA StyleSikorski, Ł., & Czamara, A. (2021). Ground Reaction Forces during Vertical Hops Are Correlated with the Number of Supervised Physiotherapy Visits after Achilles Tendon Surgery. Journal of Clinical Medicine, 10(22), 5299. https://doi.org/10.3390/jcm10225299






