Hospital at Home for Intrathecal Pump Refills: A Prospective Effectiveness, Safety and Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
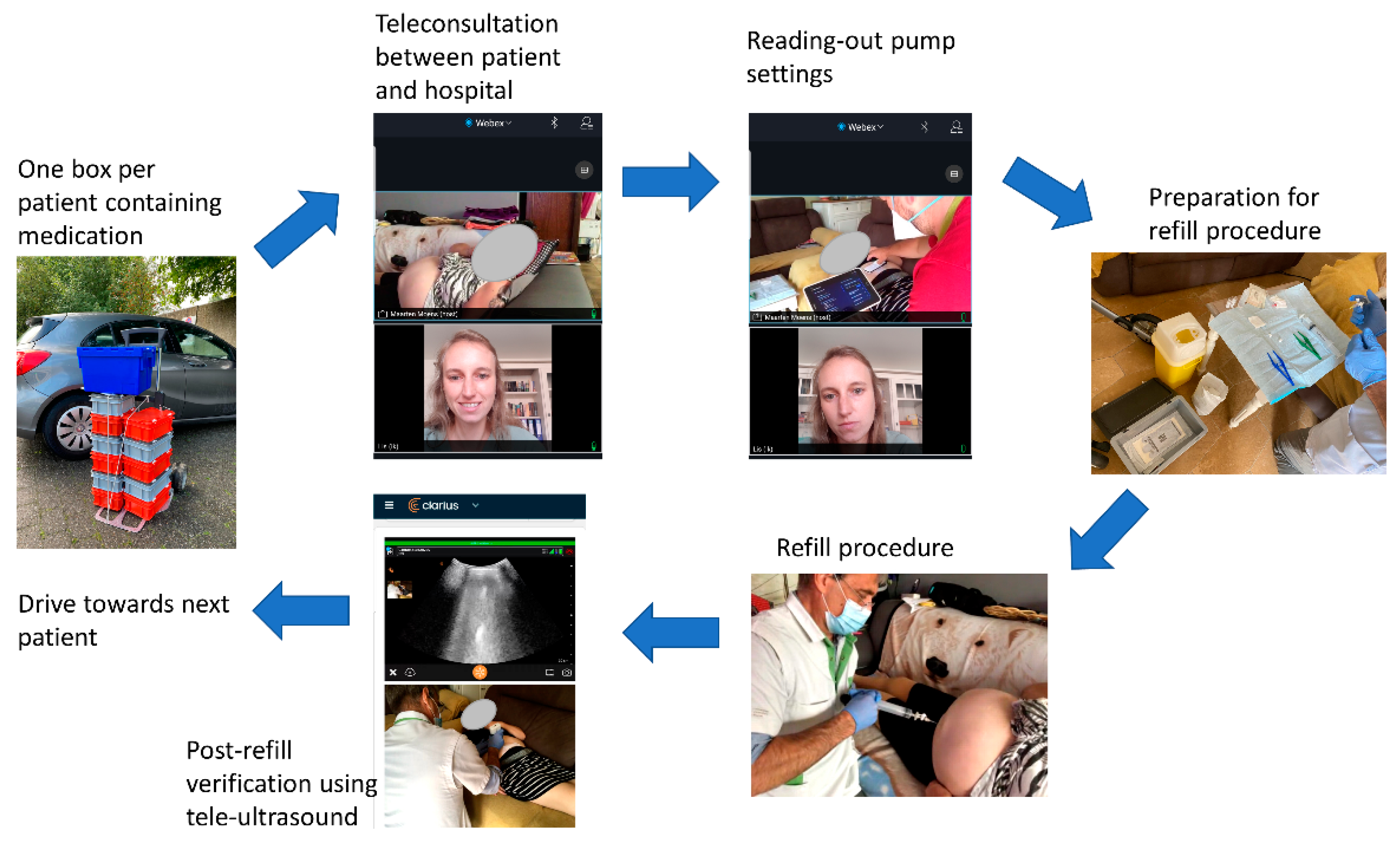
2.2. Protocol
2.3. Questionnaires
2.3.1. Primary Outcome Measurements: Effectiveness and Safety
2.3.2. Secondary Outcome Measurements: Safety
2.3.3. Secondary Outcome Measurements: Feasibility
2.3.4. Secondary Outcome Measurements: Patient Preference
2.4. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Effectiveness and Safety
3.3. Feasibility
3.4. Patient Preference
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 16 August 2021).
- Geldsetzer, P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: A cross-sectional survey on COVID-19. J. Med. Internet Res. 2020, 22, e18790. [Google Scholar] [CrossRef]
- de Moraes, E.B.; Santos Garcia, J.B.; de Macedo Antunes, J.; Daher, D.V.; Seixas, F.L.; Muniz Ferrari, M.F. Chronic pain management during the COVID-19 pandemic: A scoping review. Pain Manag. Nurs. 2021, 22, 103–110. [Google Scholar] [CrossRef]
- Puntillo, F.; Giglio, M.; Brienza, N.; Viswanath, O.; Urits, I.; Kaye, A.D.; Pergolizzi, J.; Paladini, A.; Varrassi, G. Impact of COVID-19 pandemic on chronic pain management: Looking for the best way to deliver care. Best Pract. Res. Clin. Anaesthesiol. 2020, 34, 529–537. [Google Scholar] [CrossRef]
- Catalist, N.E. What is telehealth? NEJM 2018, 4. [Google Scholar]
- Martorella, G.; Boitor, M.; Berube, M.; Fredericks, S.; Le May, S.; Gelinas, C. Tailored web-based interventions for pain: Systematic review and meta-analysis. J. Med. Internet Res. 2017, 19, e385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eccleston, C.; Blyth, F.M.; Dear, B.F.; Fisher, E.A.; Keefe, F.J.; Lynch, M.E.; Palermo, T.M.; Reid, M.C.; Williams, A.C.C. Managing patients with chronic pain during the COVID-19 outbreak: Considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain 2020, 161, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Fisher, E.; Craig, L.; Duggan, G.B.; Rosser, B.A.; Keogh, E. Psychological therapies (Internet-delivered) for the management of chronic pain in adults. Cochrane Database Syst. Rev. 2014, CD010152. [Google Scholar] [CrossRef]
- Dario, A.B.; Moreti Cabral, A.; Almeida, L.; Ferreira, M.L.; Refshauge, K.; Simic, M.; Pappas, E.; Ferreira, P.H. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: A systematic review with meta-analysis. Spine J. 2017, 17, 1342–1351. [Google Scholar] [CrossRef]
- Buhrman, M.; Gordh, T.; Andersson, G. Internet interventions for chronic pain including headache: A systematic review. Internet Interv. 2016, 4, 17–34. [Google Scholar] [CrossRef]
- Saulino, M.; Ivanhoe, C.B.; McGuire, J.R.; Ridley, B.; Shilt, J.S.; Boster, A.L. Best practices for intrathecal baclofen therapy: Patient selection. Neuromodulation 2016, 19, 607–615. [Google Scholar] [CrossRef]
- Deer, T.R.; Pope, J.E.; Hayek, S.M.; Lamer, T.J.; Veizi, I.E.; Erdek, M.; Wallace, M.S.; Grider, J.S.; Levy, R.M.; Prager, J.; et al. The Polyanalgesic Consensus Conference (PACC): Recommendations for intrathecal drug delivery: Guidance for improving safety and mitigating risks. Neuromodulation 2017, 20, 155–176. [Google Scholar] [CrossRef]
- Gofeld, M.; McQueen, C.K. Ultrasound-guided intrathecal pump access and prevention of the pocket fill. Pain Med. 2011, 12, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.K.; Dowling, M.; Purcell, A.; O’Brien, J.; Moore, D.M. Managing a national intrathecal pump service during the COVID-19 pandemic. Neuromodulation 2020, 23, 922–925. [Google Scholar] [CrossRef] [PubMed]
- Coffey, R.J.; Ridgely, P.M. Abrupt intrathecal baclofen withdrawal: Management of potentially life-threatening sequelae. Neuromodulation 2001, 4, 142–146. [Google Scholar] [CrossRef]
- Shanthanna, H.; Strand, N.H.; Provenzano, D.A.; Lobo, C.A.; Eldabe, S.; Bhatia, A.; Wegener, J.; Curtis, K.; Cohen, S.P.; Narouze, S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020, 75, 935–944. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Goslinga-Gaag, S.M.E.; Delhaas, E.M.; Frankema, S.P.G.; Huygen, F. Efficiency and safety of aftercare with intrathecal baclofen on location. Neuromodulation 2019, 22, 828–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef] [Green Version]
- Preston, C.C.; Colman, A.M. Optimal number of response categories in rating scales: Reliability, validity, discriminating power, and respondent preferences. Acta Psychol. 2000, 104, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Symonds, P.M. On the loss of reliability in ratings due to coarseness of the scale. J. Exp. Psychol. 1924, 7, 456–461. [Google Scholar] [CrossRef]
- Finstad, K. Response interpolation and scale sensitivity: Evidence against 5-point scales. J. Usability Stud. 2010, 5, 104–110. [Google Scholar]
- Yperzeele, L.; Van Hooff, R.J.; De Smedt, A.; Valenzuela Espinoza, A.; Van Dyck, R.; Van de Casseye, R.; Convents, A.; Hubloue, I.; Lauwaert, D.; De Keyser, J.; et al. Feasibility of AmbulanCe-Based Telemedicine (FACT) study: Safety, feasibility and reliability of third generation in-ambulance telemedicine. PLoS ONE 2014, 9, e110043. [Google Scholar] [CrossRef]
- Chua, C.M.S.; Ko, S.Q.; Lai, Y.F.; Lim, Y.W.; Shorey, S. Perceptions of stakeholders toward “hospital at home” program in singapore: A descriptive qualitative study. J. Patient Saf. 2021. [Google Scholar] [CrossRef] [PubMed]
- Barker, R.E.; Brighton, L.J.; Maddocks, M.; Nolan, C.M.; Patel, S.; Walsh, J.A.; Polgar, O.; Wenneberg, J.; Kon, S.S.C.; Wedzicha, J.A.; et al. Integrating home-based exercise training with a hospital at home service for patients hospitalised with acute exacerbations of COPD: Developing the model using accelerated experience-based co-design. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 1035–1049. [Google Scholar] [CrossRef] [PubMed]
- Rajaiah, N.; Kainth, H.K.; Knight, T.; Clare, S. EPICENTRE—Delivery of high quality acute medical care without transfer to hospital. Acute Med. 2021, 20, 235. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Centurión, I.; Oarbeascoa, G.; García, M.C.; López Fresneña, M.C.; Martínez Carreño, M.J.; Escudero Vilaplana, V.; González-Haba, E.; Bailén, R.; Dorado, N.; Juárez, L.M.; et al. Implementation of a hospital-at-home (HAH) unit for hematological patients during the COVID-19 pandemic: Safety and feasibility. Int. J. Hematol. 2021, 1–8. [Google Scholar] [CrossRef]
- Arsenault-Lapierre, G.; Henein, M.; Gaid, D.; Le Berre, M.; Gore, G.; Vedel, I. Hospital-at-home interventions vs. in-hospital stay for patients with chronic disease who present to the emergency department: A systematic review and meta-analysis. JAMA Netw. Open 2021, 4, e2111568. [Google Scholar] [CrossRef]
- Qaddoura, A.; Yazdan-Ashoori, P.; Kabali, C.; Thabane, L.; Haynes, R.B.; Connolly, S.J.; Van Spall, H.G. Efficacy of hospital at home in patients with heart failure: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0129282. [Google Scholar] [CrossRef]
- Patel, H.; Shafazand, M.; Ekman, I.; Hojgard, S.; Swedberg, K.; Schaufelberger, M. Home care as an option in worsening chronic heart failure—A pilot study to evaluate feasibility, quality adjusted life years and cost-effectiveness. Eur. J. Heart Fail. 2008, 10, 675–681. [Google Scholar] [CrossRef]
- Tibaldi, V.; Isaia, G.; Scarafiotti, C.; Gariglio, F.; Zanocchi, M.; Bo, M.; Bergerone, S.; Ricauda, N.A. Hospital at home for elderly patients with acute decompensation of chronic heart failure: A prospective randomized controlled trial. Arch. Intern. Med. 2009, 169, 1569–1575. [Google Scholar] [CrossRef] [Green Version]
- Shepperd, S.; Goncalves-Bradley, D.C.; Straus, S.E.; Wee, B. Hospital at home: Home-based end-of-life care. Cochrane Database Syst. Rev. 2021, 3, CD009231. [Google Scholar] [CrossRef]
- Goncalves-Bradley, D.C.; Iliffe, S.; Doll, H.A.; Broad, J.; Gladman, J.; Langhorne, P.; Richards, S.H.; Shepperd, S. Early discharge hospital at home. Cochrane Database Syst. Rev. 2017, 6, CD000356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez Verjan, C.; Augusto, V.; Xie, X.; Buthion, V. Economic comparison between Hospital at Home and Traditional Hospitalization using a simulation-based approach. J. Enterp. Inf. Manag. 2012, 26, 135–153. [Google Scholar] [CrossRef] [Green Version]
- Jakubiak-Lasocka, J.; Jakubczyk, M. Cost-effectiveness versus cost-utility analyses: What are the motives behind using each and how do their results differ?—A polish example. Value Health Reg. Issues 2014, 4, 66–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knight, T.; Harris, C.; Mas, M.; Shental, O.; Ellis, G.; Lasserson, D. The provision of hospital at home care: Results of a national survey of UK hospitals. Int. J. Clin. Pract. 2021, e14814. [Google Scholar] [CrossRef]
- Brody, A.A.; Arbaje, A.I.; DeCherrie, L.V.; Federman, A.D.; Leff, B.; Siu, A.L. Starting up a hospital at home program: Facilitators and barriers to implementation. J. Am. Geriatr. Soc. 2019, 67, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Britton, N.; Miller, M.A.; Safadi, S.; Siegel, A.; Levine, A.R.; McCurdy, M.T. Tele-ultrasound in resource-limited settings: A systematic review. Front. Public Health 2019, 7, 244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delhaas, E.M.; Huygen, F. Complications associated with intrathecal drug delivery systems. BJA Educ. 2020, 20, 51–57. [Google Scholar] [CrossRef] [PubMed]
| Perfect. No Distortion or Noise Discernible. | Speech Easily Understandable. Little Noise or Distortion. | Speech Understandable with Slight Effort. Requires Occasional Repetition due to Noise or Distortion. | Speech Understandable with Considerable Effort. Requires Frequent Repetition due To Noise or Distortion. | Unusable. Speech Present but Not Understandable. | |
|---|---|---|---|---|---|
| Audio quality | Physician: 15 (75%) Teleconsultant: 7 (35%) | Physician: 4 (20%) Teleconsultant: 10 (50%) | Physician: 1 (5%) Teleconsultant: 1 (5%) | Physician: 0 Teleconsultant: 2 (10%) | Physician: 0 Teleconsultant: 0 |
| Very good | Good | Barely acceptable | Poor | Very poor | |
| Video quality | Physician: 12 (60%) Teleconsultant: 12 (60%) | Physician: 7 (35%) Teleconsultant: 6 (30%) | Physician: 1 (5%) Teleconsultant: 1 (5%) | Physician: 0 Teleconsultant: 1 (5%) | Physician: 0 Teleconsultant: 0 |
| Very good | Good | Barely acceptable | Poor | Very poor | |
| Overall quality of the teleconsultation | Physician: 12 (60%) Teleconsultant: 8 (40%) | Physician: 7 (35%) Teleconsultant: 10 (50%) | Physician: 0 Teleconsultant: 1 (5%) | Physician: 1 (5%) Teleconsultant: 1 (5%) | Physician: 0 Teleconsultant: 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goudman, L.; De Smedt, A.; Huygens, R.; Noppen, M.; Vanschoenwinkel, M.; Hatem, S.M.; Moens, M. Hospital at Home for Intrathecal Pump Refills: A Prospective Effectiveness, Safety and Feasibility Study. J. Clin. Med. 2021, 10, 5353. https://doi.org/10.3390/jcm10225353
Goudman L, De Smedt A, Huygens R, Noppen M, Vanschoenwinkel M, Hatem SM, Moens M. Hospital at Home for Intrathecal Pump Refills: A Prospective Effectiveness, Safety and Feasibility Study. Journal of Clinical Medicine. 2021; 10(22):5353. https://doi.org/10.3390/jcm10225353
Chicago/Turabian StyleGoudman, Lisa, Ann De Smedt, René Huygens, Marc Noppen, Maria Vanschoenwinkel, Samar M. Hatem, and Maarten Moens. 2021. "Hospital at Home for Intrathecal Pump Refills: A Prospective Effectiveness, Safety and Feasibility Study" Journal of Clinical Medicine 10, no. 22: 5353. https://doi.org/10.3390/jcm10225353






