Factors Associated with 90-Day Mortality in Invasively Ventilated Patients with COVID-19 in Marseille, France
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Statistical Analysis
3. Results
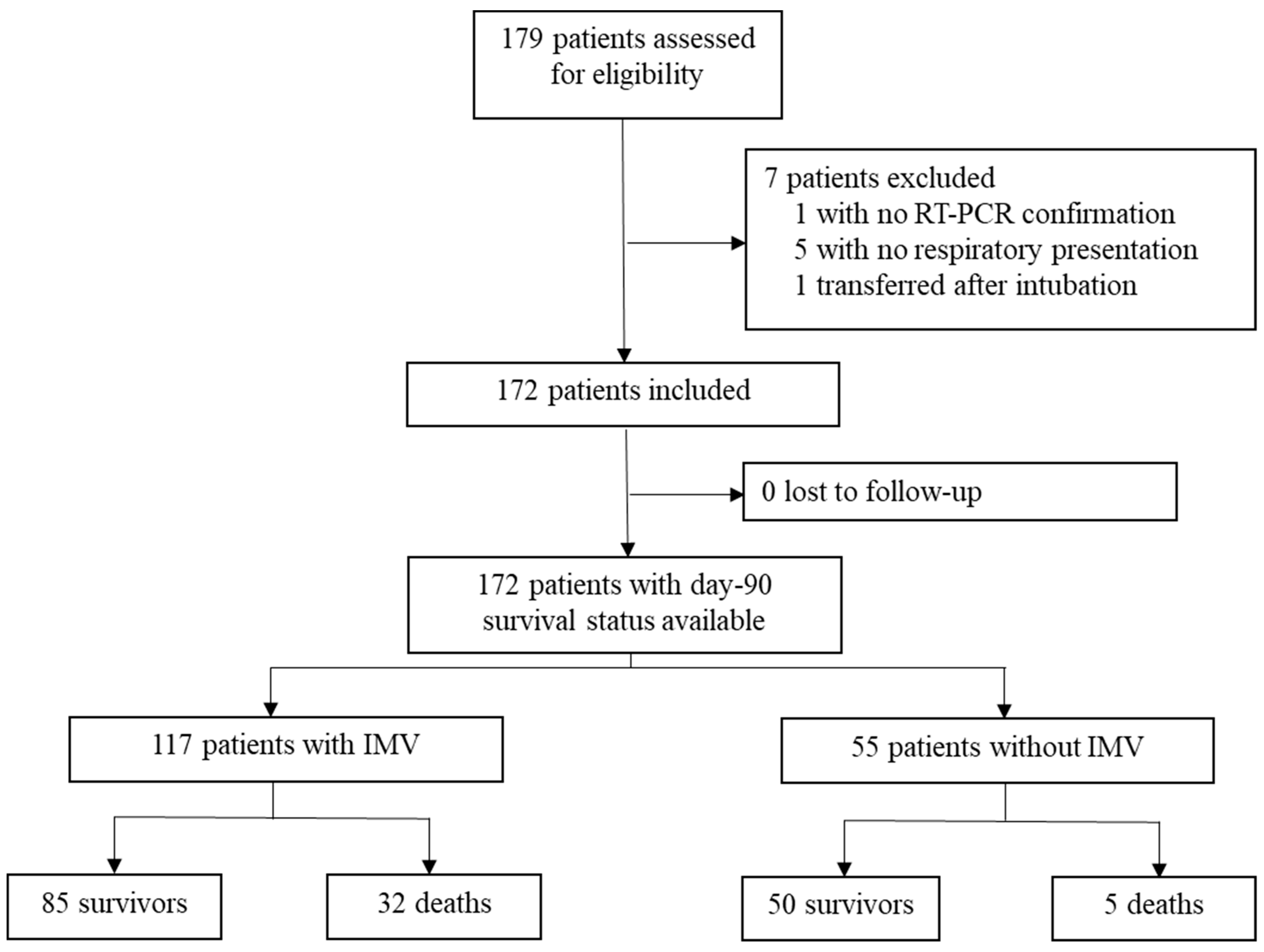
3.1. Enrolled Patients and Characteristics
3.2. Severity of ARDS and Respiratory Support
3.3. Complications and Outcomes
4. Discussion
4.1. Mortality
4.2. Risk Factors
4.3. Management
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Methodology of the Chest Computed Tomography Analysis
References
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 5 August 2021).
- Santé Publique France—COVID-19, Point Épidémiologique Hebdomadaire du 3 Juin 2021. Available online: www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-3-juin-2021 (accessed on 5 August 2021).
- Armstrong, R.A.; Kane, A.D.; Cook, T.M. Outcomes from intensive care in patients with COVID-19: A systematic review and meta-analysis of observational studies. Anaesthesia 2020, 75, 1340–1349. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Quah, P.; Li, A.; Phua, J. Mortality rates of patients with COVID-19 in the intensive care unit: A systematic review of the emerging literature. Crit. Care 2020, 24, 285. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef]
- Mitra, A.; Fergusson, N.A.; Lloyd-Smith, E.; Wormsbecker, A.; Foster, D.; Karpov, A.; Crowe, S.; Haljan, G.; Chittock, D.R.; Kanji, H.D.; et al. Baseline characteristics and outcomes of patients with COVID-19 admitted to intensive care units in Vancouver, Canada: A case series. CMAJ 2020, 192, E694–E701. [Google Scholar] [CrossRef]
- COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study. Intensive Care Med. 2020, 47, 60–73. [Google Scholar] [CrossRef]
- Botta, M.; Tsonas, A.M.; Pillay, J.; Boers, L.S.; Algera, A.G.; Bos, L.D.; Dongelmans, D.A.; Hollmann, M.W.; Horn, J.; Vlaar, A.P.; et al. Ventilation management and clinical outcome in invasively ventilated COVID-19 patients (PRoVENT-COVID)—A national, multicentre, observational cohort study. Lancet Respir. Med. 2020, 9, 139–148. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Liao, X.; Wang, B.; Kang, Y. Novel coronavirus infection during the 2019–2020 epidemic: Preparing intensive care units—The experience in Sichuan Province, China. Intensive Care Med. 2020, 46, 357–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Gattinoni, L.; Tonetti, T.; Cressoni, M.; Cadringher, P.; Herrmann, P.; Moerer, O.; Protti, A.; Gotti, M.; Chiurazzi, C.; Carlesso, E.; et al. Ventilator-related causes of lung injury: The mechanical power. Intensive Care Med. 2016, 42, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Leone, M.; Bouadma, L.; Bouhemad, B.; Brissaud, O.; Dauger, S.; Gibot, S.; Hraiech, S.; Jung, B.; Kipnis, E.; Launey, Y.; et al. Hospital-acquired pneumonia in ICU. Anaesth. Crit. Care Pain Med. 2018, 37, 83–98. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Yu, Y.; Xu, D.; Fu, S.; Zhang, J.; Yang, X.; Xu, L.; Xu, J.; Wu, Y.; Huang, C.; Ouyang, Y.; et al. Patients with COVID-19 in 19 ICUs in Wuhan, China: A cross-sectional study. Crit. Care 2020, 24, 219. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hayek, S.S.; Wang, W.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J.; et al. Factors Associated with Death in Critically Ill Patients with Coronavirus Disease 2019 in the US. JAMA Intern. Med. 2020, 180, 1436–1446. [Google Scholar] [CrossRef]
- Kooistra, E.J.; de Nooijer, A.H.; Claassen, W.J.; Grondman, I.; Janssen, N.A.F.; Netea, M.G.; van de Veerdonk, F.L.; van der Hoeven, J.G.; Kox, M.; Pickkers, P. A higher BMI is not associated with a different immune response and disease course in critically ill COVID-19 patients. Int. J. Obes. 2021, 45, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Hoiland, R.L.; Fergusson, N.A.; Mitra, A.R.; Griesdale, D.E.G.; Devine, D.V.; Stukas, S.; Cooper, J.; Thiara, S.; Foster, D.; Chen, L.Y.C.; et al. The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19. Blood Adv. 2020, 4, 4981–4989. [Google Scholar] [CrossRef]
- Cheng, Y.; Cheng, Y.; Cheng, G.; Chui, C.H.; Lau, F.Y.; Chan, P.K.S.; Ng, M.H.L.; Sung, J.J.Y.; Wong, R.S.M. ABO Blood Group and Susceptibility to Severe Acute Respiratory Syndrome. JAMA 2005, 293, 1447–1451. [Google Scholar] [CrossRef]
- Latz, C.A.; Decarlo, C.; Boitano, L.; Png, C.Y.M.; Patell, R.; Conrad, M.F.; Eagleton, M.; Dua, A. Blood type and outcomes in patients with COVID-19. Ann. Hematol. 2020, 99, 2113–2118. [Google Scholar] [CrossRef] [PubMed]
- Colombi, D.; Bodini, F.C.; Petrini, M.; Maffi, G.; Morelli, N.; Milanese, G.; Silva, M.; Sverzellati, N.; Michieletti, E. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology 2020, 296, E86–E96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fergusson, N.A.; Ahkioon, S.; Nagarajan, M.; Park, E.; Ding, Y.; Ayas, N.; Dhingra, V.K.; Chittock, D.R.; Griesdale, D.E.G. Association of intensive care unit occupancy during admission and inpatient mortality: A retrospective cohort study. Can. J. Anaesth. 2019, 67, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Helms, J.; Tacquard, C.; Severac, F.; Leonard-Lorant, I.; Ohana, M.; Delabranche, X.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Gandet, F.F.; et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020, 46, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Susen, S.; Tacquard, C.A.; Godon, A.; Mansour, A.; Garrigue, D.; Nguyen, P.; Godier, A.; Testa, S.; Albaladejo, P.; Gruel, Y. Traitement Anticoagulant pour la Prévention du Risque Thrombotique Chez Un Patient Hospitalisé avec COVID-19 et Surveillance de L’hémostase. Propositions du GIHP et du GFHT. Available online: https://sfar.org/download/traitement-anticoagulant-pour-la-prevention-du-risque-thrombotique-chez-un-patient-hospitalise-avec-covid-19-et-surveillance-de-lhemostase (accessed on 10 September 2021).
- Tobin, M.J.; Laghi, F.; Jubran, A. Caution about early intubation and mechanical ventilation in COVID-19. Ann. Intensive Care 2020, 10, 78. [Google Scholar] [CrossRef]
- Gattinoni, L.; Chiumello, D.; Caironi, P.; Busana, M.; Romitti, F.; Brazzi, L.; Camporota, L. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020, 46, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, C.; Suarez-Sipmann, F.; Mellado-Artigas, R.; Hernández, M.; Gea, A.; Arruti, E.; Aldecoa, C.; Martínez-Pallí, G.; Martínez-González, M.A.; Slutsky, A.S.; et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med. 2020, 46, 2200–2211. [Google Scholar] [CrossRef]
- IHU Méditerranée Infection—Statistics of Testing and Hospitalization for SARS-CoV-2 Infection in the Area of Marseille, France. Available online: https://www.mediterranee-infection.com/ (accessed on 14 September 2021).
- Liang, L.-L.; Tseng, C.-H.; Ho, H.J.; Wu, C.-Y. Covid-19 mortality is negatively associated with test number and government effectiveness. Sci. Rep. 2020, 10, 12567. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Rello, J.; Marshall, J.K.; Silva, E.; Anzueto, A.; Martin, C.D.; Moreno, R.; Lipman, J.; Gomersall, C.; Sakr, Y.; et al. International Study of the Prevalence and Outcomes of Infection in Intensive Care Units. JAMA 2009, 302, 2323–2329. [Google Scholar] [CrossRef] [Green Version]

| Total (N = 117) | Survivors (N = 85) | Non-Survivors (N = 32) | p-Value | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age | 63 (56–72) | 61 (54–67) | 71.5 (62.75–77) | <0.001 |
| Male | 88 (75.2) | 64 (75.3) | 24 (75.0) | 0.974 |
| ABO blood group | ||||
| A | 42 (35.9) | 32 (37.6) | 10 (31.2) | 0.605 |
| B | 17 (14.5) | 13 (15.3) | 4 (12.5) | 0.419 |
| O | 41 (35) | 30 (35.3) | 11 (34.4) | 0.366 |
| AB | 2 (1.7) | 1 (1.2) | 1 (3.1) | 0.218 |
| BMI > 25 kg·m2 | 73 (62.4) | 59 (69.4) | 14 (43.8) | 0.011 |
| Hypertension | 68 (58.1) | 48 (56.5) | 20 (62.5) | 0.556 |
| Diabetes | 24 (20.5) | 15 (17.6) | 9 (28.1) | 0.211 |
| Metabolic syndrome | 34 (29.1) | 29 (34.1) | 5 (15.6) | 0.05 |
| Chronic respiratory disease | 22 (18.8) | 15 (17.6) | 7 (21.9) | 0.602 |
| Chronic kidney disease | 11 (9.4) | 8 (9.4) | 3 (9.4) | 0.995 |
| Immunodeficiency | 24 (20.5) | 15 (17.6) | 9 (28.1) | 0.211 |
| Statins intake | 23 (19.7) | 12 (14.1) | 11 (34.4) | 0.014 |
| Systemic steroids intake | 9 (7.7) | 6 (7.1) | 3 (9.4) | 0.675 |
| Charlson index | 3 (2–4) | 2 (1–3) | 4 (2–6) | <0.001 |
| SAPS II score | 34 (27–40) | 30.5 (25–38.25) | 38 (35–45) | 0.02 |
| SOFA score | 5 (3–7) | 4 (3–7) | 5 (3–6) | 0.966 |
| Total lungs volume on CT (cm3) | 3257 (2447–4016) | 3142 (2285–3804) | 3742 (3275–4158) | 0.01 |
| Lesions/lungs ratio on CT (%) | ||||
| Ground glass/lungs ratio | 24.8 (12.6–34.4) | 26.9 (13.6–36.6) | 21.5 (7.1–28.2) | 0.862 |
| Condensations/lungs ratio | 5.1 (2.1–12.4) | 6.6 (3.1–16) | 2.1 (0.3–8.2) | 0.495 |
| All lesions/lungs ratio | 31.8 (15.6–46.6) | 34.1 (19.9–49.7) | 26.8 (9.2–36.3) | 0.034 |
| Days from symptoms onset to intubation | 9 (6–11.25) | 8.5 (6–11) | 9 (6–12) | 0.3 |
| Days from ICU admission to intubation | 0 (0–1) | 1 (0–1) | 0 (0–1) | 0.364 |
| Biology (worst value during first 48H after ICU admission) | ||||
| Lymphocyte count (×109/L) | 0.69 (0.5–0.95) | 0.7 (0.53–1) | 0.61 (0.44–0.78) | 0.382 |
| Neutrophil to Lymphocyte Ratio | 11.1 (8.3–15.5) | 10.6 (7.5–15.3) | 12.6 (10.5–19.8) | 0.005 |
| D-Dimers (mg/L) | 3.44 (1.64–5) | 3.34 (1.52–5) | 4 (1.84–5) | 0.9 |
| Fibrinogen (g/L) | 8.1 (6.9–9.4) | 8.1 (7.1–9.5) | 8 (6.9–9.4) | 0.995 |
| CRP (mg/L) | 201(126–302) | 179 (120–248) | 283 (162–324) | 0.29 |
| Creatinine (µmol/L) | 85 (67–138) | 84 (65–127) | 98 (78–153) | 0.048 |
| LDH (UI/L) | 447 (368–535) | 435 (347–491) | 539 (443–635) | 0.005 |
| Ferritin (ng/mL) | 1418 (968–2321) | 1175 (950–1778) | 2728 (2342–6049) | 0.021 |
| Invasive ventilation parameters during first 24 h | ||||
| PaO2/FiO2 | 130 (100–180) | 140 (100–180) | 120 (100–160) | 0.457 |
| PEEP (cmH2O) | 12 (10.3–14) | 12 (12–14) | 12 (10–15) | 0.483 |
| Plateau pressure (cm H2O) | 25 (21.7–28.3) | 23.5 (21.0–28.2) | 26.0 (23.6–28.8) | 0.353 |
| Respiratory compliance (mL/cmH2O) | 33 (28.2–45) | 40 (29–46) | 31 (27–40) | 0.018 |
| Mechanical power (J/min) | 15.6 (13.3–19.6) | 15.5 (13.5–19.1) | 15.9 (12–19.8) | 0.836 |
| Total (N = 117) | Survivors (N = 85) | Non-Survivors (N = 32) | p-Value | |
|---|---|---|---|---|
| Management in ICU | ||||
| Use of non-invasive ventilation before intubation | 16 (13.7) | 12 (14.1) | 4 (12.5) | 0.693 |
| Use of high-flow oxygen before intubation | 69 (59) | 51 (60) | 18 (56.2) | 0.589 |
| Neuromuscular blockade | 113 (96.6) | 82 (96.5) | 31 (96.9) | 0.923 |
| Prone positioning | 99 (84.6) | 72 (84.7) | 27 (84.4) | 0.965 |
| ECMO | 23 (19.7) | 18 (21.2) | 5 (15.6) | 0.501 |
| Vasopressors | 105 (89.7) | 74 (87.1) | 31 (96.9) | 0.122 |
| Renal replacement therapy | 20 (17.1) | 12 (14.1) | 8 (25) | 0.167 |
| Corticosteroids a | 23 (19.7) | 14 (12.0) | 9 (7.7) | 0.157 |
| Hydroxychloroquine (10 days) with azithromycin (5 days) | 45 (38.5%) | 36(42.4) | 9 (28.1) | 0.159 |
| Remdesivir | 0 (0) | 0(0) | 0 (0) | - |
| Lopinavir-ritonavir | 18 (15.4) | 13(15.3) | 5 (15.6) | 0.965 |
| Complications | ||||
| Ventilator associated pneumonia | 71 (60.7) | 53 (62.4) | 18 (56.2) | 0.547 |
| Septic shock | 47 (40.2) | 32 (37.6) | 15 (46.9) | 0.364 |
| Venous thrombosis or pulmonary embolism | 35 (29.9) | 29 (34.1) | 6 (18.8) | 0.106 |
| Arterial thrombosis | 10 (8.5) | 4 (4.7) | 6 (18.8) | 0.015 |
| Severe bleeding event | 25 (21.4) | 17 (20) | 8 (25) | 0.556 |
| Outcomes | ||||
| Duration of ventilation (days) | 20 (9–33) | 21 (11–34) | 18 (6.75–25.25) | 0.06 |
| Ventilator-free days at d28 (days) | 2 (1–7) | 4 (1–7) | 0 (0–1) | <0.001 |
| Length of stay in ICU (days) | 29 (17–46) | 33 (19–53) | 21 (6.75–31.75) | 0.02 |
| Length of in hospital (days) | 37 (24–53) | 42 (29–57) | 25 (8.75–38.25) | <0.001 |
| 28-day mortality | 21 (17.9) | 0 (0) | 21 (60) | - |
| Associated Factors | Univariate HR (95% CI) | p-Value | Multivariate 1 HR (95% CI) | p-Value | Multivariate 2 HR (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Age ≥ 65 years | 3.27 (1.51–7.08) | 0.007 | 4.17 (1.48–11.73) | 0.010 | - | - |
| Male | 0.86 (0.39–1.92) | 0.718 | - | - | - | - |
| Charlson Index ≥ 3 | 5.58 (1.96–15.90) | 0.005 | - | - | 3.72 (1.07–12.92) | 0.05 |
| Arterial thrombosis | 2.22 (0.91–5.42) | 0.098 | 3.79 (1.22–11.80) | 0.022 | 2.86 (1.00–8.20) | 0.05 |
| Statins intake | 2.55 (1.23–5.31) | 0.020 | 3.78 (1.51–9.43) | 0.010 | 3.59 (1.44–8.93) | 0.186 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Volff, M.; Tonon, D.; Bommel, Y.; Peres, N.; Lagier, D.; Agard, G.; Jacquier, A.; Bartoli, A.; Carvelli, J.; Max, H.; et al. Factors Associated with 90-Day Mortality in Invasively Ventilated Patients with COVID-19 in Marseille, France. J. Clin. Med. 2021, 10, 5650. https://doi.org/10.3390/jcm10235650
Volff M, Tonon D, Bommel Y, Peres N, Lagier D, Agard G, Jacquier A, Bartoli A, Carvelli J, Max H, et al. Factors Associated with 90-Day Mortality in Invasively Ventilated Patients with COVID-19 in Marseille, France. Journal of Clinical Medicine. 2021; 10(23):5650. https://doi.org/10.3390/jcm10235650
Chicago/Turabian StyleVolff, Maxime, David Tonon, Youri Bommel, Noémie Peres, David Lagier, Geoffray Agard, Alexis Jacquier, Axel Bartoli, Julien Carvelli, Howard Max, and et al. 2021. "Factors Associated with 90-Day Mortality in Invasively Ventilated Patients with COVID-19 in Marseille, France" Journal of Clinical Medicine 10, no. 23: 5650. https://doi.org/10.3390/jcm10235650
APA StyleVolff, M., Tonon, D., Bommel, Y., Peres, N., Lagier, D., Agard, G., Jacquier, A., Bartoli, A., Carvelli, J., Max, H., Simeone, P., Blasco, V., Pastene, B., Loundou, A., Boyer, L., Leone, M., Velly, L., Bourenne, J., Boussen, S., ... Bruder, N., on behalf of the GRAM+ (Groupe de Recherche en Réanimation et Anesthésie de Marseille Pluridisciplinaire). (2021). Factors Associated with 90-Day Mortality in Invasively Ventilated Patients with COVID-19 in Marseille, France. Journal of Clinical Medicine, 10(23), 5650. https://doi.org/10.3390/jcm10235650





