Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic?
Abstract
:1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
3. Description of Long COVID (LC)
4. Mechanism of Action of SARS-CoV-2 in the Etiopathogenesis of Long COVID (LC)
4.1. Alterations of the Immune Response
4.1.1. Dysregulation of the Immune System
4.1.2. Presence of Autoantibodies
4.1.3. Thyroid Dysfunction
4.1.4. Nutritional Deficiencies
4.2. Inflammatory State
4.2.1. Continued Inflammatory Response
4.2.2. Gut Microbiota Imbalance
4.3. Viral Persistence
Metabolic Alterations
4.4. Coagulopathies
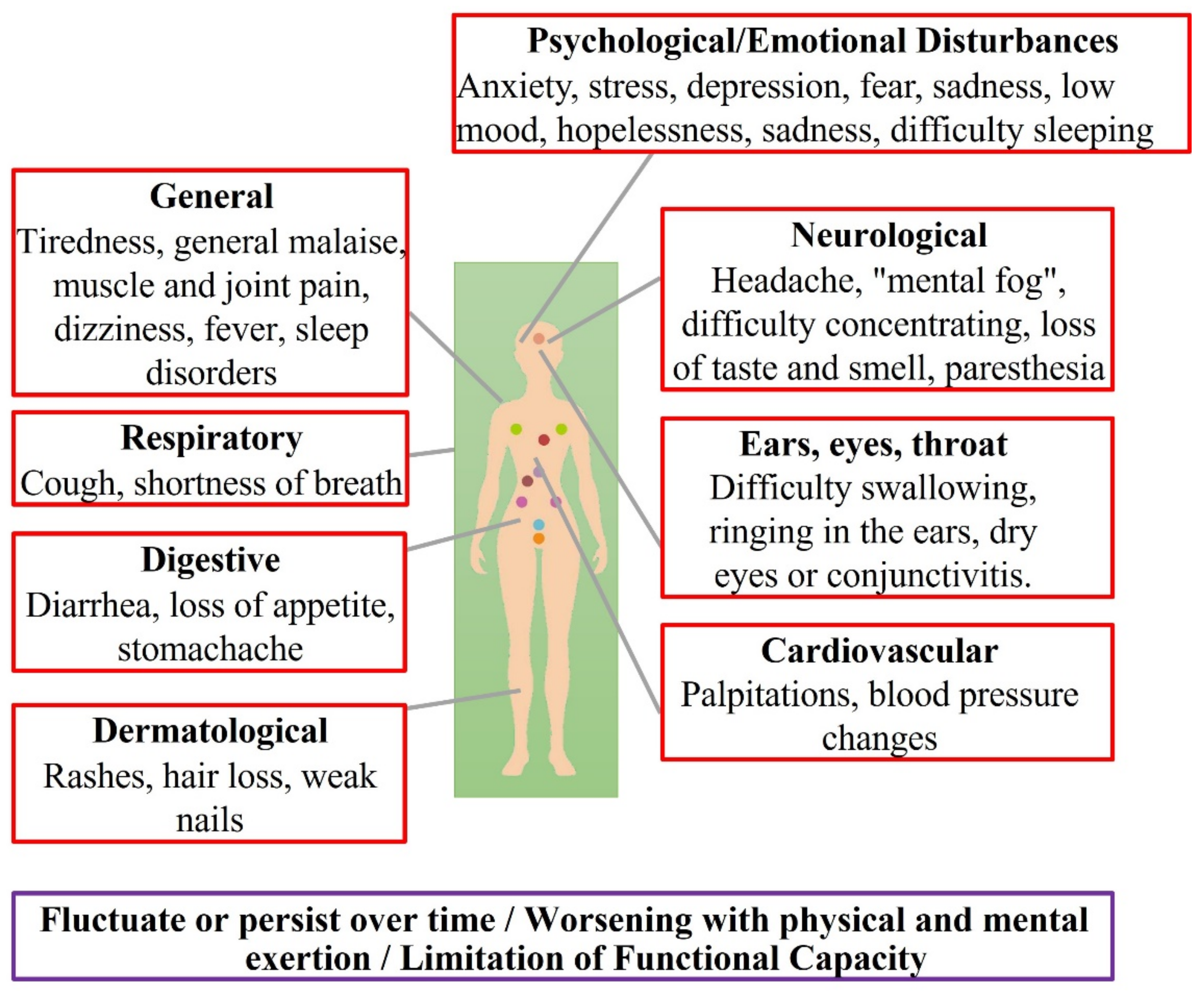
5. Clinical Characteristics of Long COVID
5.1. Incidence
5.2. Symptomatology
6. Pediatric Long COVID
7. What Is the Likelihood of Long COVID?
8. Disability Associated with Long COVID
9. Basic Biomarkers in Long COVID
10. Potential Treatment of Long COVID
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef]
- Tabish, S.A. COVID-19 pandemic: Emerging perspectives and future trends. J. Public Health Res. 2020, 9, 19–26. [Google Scholar] [CrossRef]
- COVID-19 Map—Johns Hopkins Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 18 August 2021).
- Fernández-Lázaro, D.; Fernandez-Lazaro, C.I.; Mielgo-Ayuso, J.; Adams, D.P.; García Hernández, J.L.; González-Bernal, J.; González-Gross, M. Glycophosphopeptical AM3 Food Supplement: A Potential Adjuvant in the Treatment and Vaccination of SARS-CoV-2. Front. Immunol. 2021, 12, 1–13. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Gómez, N.S.; Serrano, N.S.; Sosse, A.A.; Aldea-Mansilla, C. Emergency Standardization for SARS-CoV-2 Virus Diagnosis by Real-Time Reverse Transcription-Reverse Polymerase Chain Reaction (RT-PCR) in a COVID-19 Pandemic Situation. Rev. Madrileña Salud Pública 2020, 4, 1–11. [Google Scholar] [CrossRef]
- Lai, C.C.; Ko, W.C.; Lee, P.I.; Jean, S.S.; Hsueh, P.R. Extra-respiratory manifestations of COVID-19. Int. J. Antimicrob. Agents 2020, 56, 106024. [Google Scholar] [CrossRef] [PubMed]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long Covid-mechanisms, risk factors, and management. BMJ 2021, 374, n1648. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Knight, M.; A’Court, C.; Buxton, M.; Husain, L. Management of post-acute Covid-19 in primary care. BMJ 2020, 370, m3026. [Google Scholar] [CrossRef]
- World Health Organization (WHO). What We Know about Long-Term Effects of COVID-19. 2020. Available online: https://scholar.google.es/scholar?hl=es&as_sdt=0%2C5&q=What+we+know+about+long-term+effects+of+COVID-19.+The+latest+on+the+COVID-19+global+situation+and+long-term+sequelae&btnG= (accessed on 24 August 2021).
- Datta, S.D.; Talwar, A.; Lee, J.T. A Proposed Framework and Timeline of the Spectrum of Disease Due to SARS-CoV-2 Infection: Illness Beyond Acute Infection and Public Health Implications. JAMA 2020, 324, 2251–2252. [Google Scholar] [CrossRef] [PubMed]
- The National Institute for Health and Care Excellence (NICE). COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19; NICE Guideline [NG188]; The National Institute for Health and Care Excellence (NICE): London, UK, 2021; pp. 1–111. [Google Scholar]
- Ministry of Health, Government of Spain, Health Alerts and Emergencies Coordination Center. Contributions of This Update Scientific-Technical Information Coronavirus Disease, COVID-19. 2021; pp. 1–111. Available online: https://www.aemps.gob.es/https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/covid19/vacunasCovid19.htm (accessed on 24 August 2021).
- World Health Organization (WHO). What Is Health Policy and Systems Research. 2021. Available online: https://ahpsr.who.int/what-we-do/what-is-health-policy-and-systems-research-(hpsr) (accessed on 24 August 2021).
- Andrade, B.S.; Siqueira, S.; Soares, W.R.d.A.; Rangel, F.d.S.; Santos, N.O.; Freitas, A.d.S.; Silveira, P.R.d.; Tiwari, S.; Alzahrani, K.J.; Góes-Neto, A.; et al. Long-COVID and Post-COVID Health Complications: An Up-to-Date Review on Clinical Conditions and Their Possible Molecular Mechanisms. Viruses 2021, 13, 700. [Google Scholar] [CrossRef] [PubMed]
- Proal, A.D.; VanElzakker, M.B. Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol. 2021, 12, 698169. [Google Scholar] [CrossRef]
- Rodríguez Ledo, P.; Armenteros del Olmo, L.; Guerrero Caballero, S.; Bilbao Fernández, S. The persistence of COVID-19 symptoms and its diagnosis in the first wave of the pandemic in Spain. Med. Gen. Y Fam. 2021, 10, 53–59. [Google Scholar] [CrossRef]
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules 2020, 26, 39. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). International Classification of Diseases, 11th Revision (IDC-11). 2020. Available online: https://icd.who.int/es (accessed on 26 August 2021).
- L´Assurance Maladie (ameli.fr). Symptômes Prolongés Suite à la Covid-19: Diagnostic et Prise en Charge. Médecin. 2021. Available online: https://www.ameli.fr/medecin/actualites/symptomes-prolonges-suite-la-covid-19-diagnostic-et-prise-en-charge (accessed on 28 August 2021).
- Chippa, V.; Aleem, A.; Anjum, F. Post-Acute Coronavirus (COVID-19) Syndrome. StatPearls Publishing: Treasure Island, FL, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570608/ (accessed on 26 August 2021).
- Patterson, B.K.; Guevara-Coto, J.; Yogendra, R.; Francisco, E.B.; Long, E.; Pise, A.; Rodrigues, H.; Parikh, P.; Mora, J.; Mora-Rodríguez, R.A. l Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning. Front. Immunol. 2021, 12, 700782. [Google Scholar] [CrossRef] [PubMed]
- Gaebler, C.; Wang, Z.; Lorenzi, J.C.C.; Frauke Muecksch, F.; Finkin, S.; Tokuyama, M.; Cho, A.; Jankovic, M.; Schaefer-Babajew, D.; Oliveira, D.Y.; et al. Evolution of antibody immunity to SARS-CoV-2. Nature 2021, 591, 639–644. [Google Scholar] [CrossRef]
- Ong, S.W.X.; Fong, S.W.; Young, B.E.; Chan, Y.H.; Lee, B.; Amrun, S.N.; Chee, R.S.-L.; Yeo, N.K.-W.; Tambyah, P.; Pada, S.; et al. Persistent Symptoms and Association with Inflammatory Cytokine Signatures in Recovered Coronavirus Disease 2019 Patients. Open Forum Infect. Dis. 2021, 8, ofab156. [Google Scholar] [CrossRef]
- Suárez Reyes, A.; Villegas Valverde, C.A.; Suárez Reyes, A.; Villegas Valverde, C.A. Characteristics and specialization of the immune response in COVID-19. Rev. Fac. Med. 2020, 63, 7–18. [Google Scholar]
- Bergamaschi, L.; Mescia, F.; Turner, L.; Hanson, A.; Kotagiri, P.; Dunmore, B.J.; Ruffieux, H.; De Sa, A.; Oisin Huhn, O.; Wills, M.R.; et al. Early Immune Pathology and Persistent Dysregulation Characterise Severe COVID-19. medRxiv 2021, 1, 01J. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Zuo, Y.; Estes, S.K.; Ali, R.A.; Gandhi, A.A.; Yalavarthi, S.; Shi, H.; Sule, G.; Gockman, K.; Madison, J.A.; Zuo, M.; et al. Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci. Transl. Med. 2020, 12, eabd3876. [Google Scholar] [CrossRef]
- Wang, E.Y.; Mao, T.; Klein, J.; Dai, Y.; Huck, J.D.; Liu, F.; Zheng, N.S.; Zhou, T.; Israelow, B.; Wong, P.; et al. Diverse Functional Autoantibodies in Patients with COVID-19. medRxiv Prepr. Serv. Heal Sci. 2021, preprint. [Google Scholar] [CrossRef]
- Li, Q.; Wang, B.; Mu, K.; Zhang, J.A. The pathogenesis of thyroid autoimmune diseases: New T lymphocytes—Cytokines circuits beyond the Th1-Th2 paradigm. J Cell Physiol. 2019, 234, 2204–2216. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.T.W.; Lee, C.H.; Chow, W.S.; Lee, A.C.H.; Tam, A.R.; Fong, C.H.Y.; Law, C.Y.; Hong Leung, E.K.; Wang To, K.K.; Beng Tan, K.C.; et al. Thyroid Dysfunction in Relation to Immune Profile, Disease Status, and Outcome in 191 Patients with COVID-19. J. Clin. Endocrinol. Metab. 2021, 106, e926–e935. [Google Scholar] [CrossRef]
- Dalli, J. Does promoting resolution instead of inhibiting inflammation represent the new paradigm in treating infections? Mol. Asp. Med. 2017, 58, 12–20. [Google Scholar] [CrossRef]
- Serhan, C.N. Treating inflammation and infection in the 21st century: New hints from decoding resolution mediators and mechanisms. FASEB J. 2017, 31, 1273–1288. [Google Scholar] [CrossRef] [Green Version]
- Regidor, P.A.; Santos, F.G.; Rizo, J.M.; Egea, F.M. Pro resolving inflammatory effects of the lipid mediators of omega 3 fatty acids and its implication in SARS COVID-19. Med. Hypotheses 2020, 145, 110340. [Google Scholar] [CrossRef]
- Regidor, P.A. Covid-19 management with inflammation resolving mediators? Perspectives and potential. Med. Hypotheses 2020, 142, 109813. [Google Scholar] [CrossRef]
- Kumar, R.; Rathi, H.; Haq, A.; Wimalawansa, S.J.; Sharma, A. Putative roles of vitamin D in modulating immune response and immunopathology associated with COVID-19. Virus Res. 2021, 292, 198235. [Google Scholar] [CrossRef]
- Rogero, M.M.; de Leão, M.C.; Santana, T.M.; de Pimentel, M.V.M.B.; Carlini, G.C.G.; Silveira, T.F.F.; Gonçalves, R.C.; Castro, I.A. Potential benefits and risks of omega-3 fatty acids supplementation to patients with COVID-19. Free Radic. Biol. Med. 2020, 156, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Clemente-Suárez, V.J.; Ramos-Campo, D.J.; Mielgo-Ayuso, J.; Dalamitros, A.A.; Nikolaidis, P.A.; Hormeño-Holgado, A.; Tornero-Aguilera, J.F. Nutrition in the Actual COVID-19 Pandemic. A Narrative Review. Nutrients 2021, 13, 1924. [Google Scholar] [CrossRef] [PubMed]
- Shakoor, H.; Feehan, J.; Dhaheri, A.S.; Al Ali, H.I.; Platat, C.; Ismail, L.C.; Apostolopoulos, V.; Stojanovska, L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19? Maturitas 2021, 143, 1–9. [Google Scholar] [CrossRef]
- Maraver-Romero, R. Could the Mediterranean lifestyle prevent complications from Covid-19 infection? Actual. Med. 2020, 105, 66–68. [Google Scholar] [CrossRef]
- Haig, D.M.K.; McInnes, C.; Deane, D.; Reid, H.; Mercer, A. The immune and inflammatory response to orf virus. Comp. Immunol. Microbiol. Infect. Dis. 1997, 20, 197–204. [Google Scholar] [CrossRef]
- Duan, L.; Rao, X.; Sigdel, K.R. Regulation of inflammation in autoimmune disease. J. Immunol. Res. 2019, 1, 7403796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Sollini, M.; Ciccarelli, M.; Cecconi, M.; Aghemo, A.; Morelli, P.; Gelardi, F.; Chiti, A. Vasculitis changes in COVID-19 survivors with persistent symptoms: An [18F]FDG-PET/CT study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 1460–1466. [Google Scholar] [CrossRef]
- Siddiqi, H.K.; Mehra, M.R. COVID-19 illness in native and immunosuppressed states: A clinical–therapeutic staging proposal. J. Heart Lung Transpl. 2020, 39, 405–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, B.; Han, J.; Cheng, X.; Yu, L.; Zhang, L.; Wang, W.; Ni, L.; Wei, C.; Yafei Huang, Y.; Cheng, Z. Reduced numbers of T cells and B cells correlates with persistent SARS-CoV-2 presence in non-severe COVID-19 patients. Sci. Rep. 2020, 10, 17718. [Google Scholar] [CrossRef]
- Belkaid, Y.; Hand, T.W. Role of the microbiota in immunity and inflammation. Cells 2014, 157, 121–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuo, T.; Zhan, H.; Zhan, F.; Liu, Q.; Tso, E.Y.; Lui, G.C.; Chen, N.; Li, A.; Lu, W.; Chan, F.K.L.; et al. Alterations in Fecal Fungal Microbiome of Patients with COVID-19 during Time of Hospitalization until Discharge. Gastroenterology 2020, 159, 1302–1310. [Google Scholar] [CrossRef]
- Marazzato, M.; Ceccarelli, G.; d’Ettorre, G. Dysbiosis in SARS-CoV-2–Infected Patients. Gastroenterology 2021, 160, 2195. [Google Scholar] [CrossRef]
- Guerrero Caballero, S.; Bilbao Fernández, S. Persistence of SARS-CoV-2 virus as an etiologic cause of long-lasting symptomatology in patients with persistent COVID-19. Med. Gen. Y Fam. 2021, 10, 85–90. [Google Scholar] [CrossRef]
- Wu, Y.; Guo, C.; Tang, L.; Hong, Z.; Zhou, J.; Dong, X.; Yin, H.; Xiao, Q.; Tang, Y.; Qu, X.; et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020, 5, 434–435. [Google Scholar] [CrossRef]
- Xiao, F.; Tang, M.; Zheng, X.; Liu, Y.; Li, X.; Shan, H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020, 158, 1831–1833. [Google Scholar] [CrossRef]
- Bruzzone, C.; Bizkarguenaga, M.; Gil-Redondo, R.; Diercks, T.; Arana, E.; García de Vicuña, A.; Seco, M.; Bosch, A.; Palazón, A.; San Juan, I.; et al. SARS-CoV-2 Infection Dysregulates the Metabolomic and Lipidomic Profiles of Serum. iScience 2020, 23, 101645. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Lee, S.G.; Fralick, M.; Sholzberg, M. Coagulopathy associated with COVID-19. CMAJ 2020, 192, e583. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.C. COVID-19 update: Covid-19-associated coagulopathy. J. Thromb. Thrombolysis 2020, 50, 54–67. [Google Scholar] [CrossRef]
- Pretorius, E.; Vlok, M.; Venter, C.; Bezuidenhout, J.A.; Laubscher, G.J.; Steenkamp, J.; Kell, D.B. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021, 20, 172. [Google Scholar] [CrossRef] [PubMed]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef]
- Office for National Statistics. The Prevalence of Long COVID Symptoms and COVID-19 Complications. 2020. Available online: https://www.ons.gov.uk/news/statementsandletters/theprevalenceoflongcovidsymptomsandcovid19complications (accessed on 29 August 2021).
- Office for National Statistics. Updated Estimates of the Prevalence of Prolonged COVID-19 Symptoms. 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/adhocs/12788updatedestimatesoftheprevalenceoflongcovidsymptoms (accessed on 29 August 2021).
- Cirulli, E.T.; Barrett, K.M.S.; Riffle, S.; Bolze, A.; Neveux, I.; Dabe, S.; Grzymski, J.J.; Lu, J.T.; Washington, N.L. Long-term COVID-19 symptoms in a large unselected population. medRxiv 2020. preprint. [Google Scholar]
- Rajan, S.; Khunti, K.; Alwan, N.; Steves, C.; MacDermott, N.; Morsella, A.; Angulo, E.; Winkelmann, J.; Bryndová, L.; Fronteira , I.; et al. The Wake of the Pandemic: Preparing for Long COVID; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2021; Available online: http://europepmc.org/books/NBK569598 (accessed on 29 August 2021).
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef]
- Ministry of Health Government of Spain. Clinical Information COVID-19. 2021; pp. 1–34. Available online: https://www.mscbs.gob.es/en/profesionales/saludPublica/ (accessed on 29 August 2021).
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Signe Redfield, S.; Austin, J.-P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Rodríguez Ledo, P.; Armenteros del Olmo, L.; Rodríguez Rodríguez, E.; Gómez Acebo, F. Description of the 201 symptoms of multiorgan involvement in patients affected by persistent COVID-19. Med. Gen. Y Fam. 2021, 10, 60–68. [Google Scholar] [CrossRef]
- Fernández-Lázaro, D.; Garrosa, M. Identification, Mechanism, and Treatment of Skin Lesions in COVID-19: A Review. Viruses 2021, 13, 1916. [Google Scholar] [CrossRef]
- Martins, M.M.; Prata-Barbosa, A.; Ledo Alves da Cunha, A.J. Update on SARS-CoV-2 infection in children. Paediatr. Int. Child Health 2021, 41, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Nogueira López, J.; Grasa, C.; Calvo, C.; García López-Hortelano, M. Long-term symptoms of COVID-19 in children. Acta Paediatr. 2021, 110, 2282–2283. [Google Scholar] [CrossRef] [PubMed]
- Brackel, C.L.; Lap, C.R.; Buddingh, E.P.; van Houten, M.A.; van der Sande, L.J.; Langereis, E.J.; Bannier, M.A.G.E.; Pijnenburg, M.W.H.; Hashimoto, S.; Suzanne W., J.; et al. Pediatric long-COVID: An overlooked phenomenon? Pediatr. Pulmonol. 2021, 56, 2495–2502. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 2021, 110, 914–921. [Google Scholar] [CrossRef]
- Petersen, M.S.; Kristiansen, M.F.; Hanusson, K.D.; Danielsen, M.E.; Gaini, S.; Strøm, M.; Marin Strøm, M.; Weihe, P. Long COVID in the Faroe Islands—A longitudinal study among non-hospitalized patients. Clin. Infect. Dis. 2020, 73, e4058–e4063. [Google Scholar] [CrossRef] [PubMed]
- Buonsenso, D.; Munblit, D.; De Rose, C.; Sinatti, D.; Ricchiuto, A.; Carfi, A.; Valentini, P. Preliminary evidence on long COVID in children. Acta Paediatr. 2021, 110, 2208–2211. [Google Scholar] [CrossRef]
- Radtke, T.; Ulyte, A.; Puhan, M.A.; Kriemler, S. Long-term symptoms after SARS-CoV-2 infection in children and adolescents. JAMA 2021, 326, 869–871. [Google Scholar] [CrossRef] [PubMed]
- Sadarangani, M.; Marchant, A.; Kollmann, T.R. Immunological mechanisms of vaccine-induced protection against COVID-19 in humans. Nat. Rev. Immunol. 2021, 21, 475–484. [Google Scholar] [CrossRef] [PubMed]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Capdevila Pujol, J.; Klaser, K.; Antonelli, M.; LCanas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Maxwell, E. Unpacking post-covid symptoms. BMJ 2021, 373, n1173. [Google Scholar] [CrossRef]
- Stavem, K.; Ghanima, W.; Olsen, M.K.; Gilboe, H.M.; Einvik, G. Persistent symptoms 1.5–6 months after COVID-19 in non-hospitalised subjects: A population-based cohort study. Thorax 2021, 76, 405–407. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Lázaro, D.; Seco-Calvo, J.; Fernandez-Lazaro, C.I.; Sánchez-Serrano, N. XVII Scientific Meeting: Science, technology and innovation at the service of the pandemic response plan in Colombia. The puzzling new condition associated with SARS-CoV-2 infection: Long COVID. Oral Commun. Biomed. 2021, 41, 79. [Google Scholar]
- Poyraz, B.Ç.; Poyraz, C.A.; Olgun, Y.; Gürel, Ö.; Alkan, S.; Özdemir, Y.E.; Balkan, I.I.; Karaali, R. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry Res. 2021, 295, 113604. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Pérez, O.; Merino, E.; Leon-Ramirez, J.M.; Andres, M.; Ramos, J.M.; Arenas-Jiménez, J.; Asensio, S.; Sanchez, R.; Ruiz-Torregrosa, P.; Galan, I.; et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J. Infect. 2021, 82, 378–383. [Google Scholar]
- Miyazato, Y.; Morioka, S.; Tsuzuki, S.; Akashi, M.; Osanai, Y.; Tanaka, K.; Terada, M.; Suzuki, M.; Kutsuna, S.; Saito, S.; et al. Prolonged and Late-Onset Symptoms of Coronavirus Disease 2019. Open Forum Infect. Dis. 2020, 7, ofaa507. [Google Scholar] [CrossRef]
- Yelin, D.; Margalit, I.; Yahav, D.; Runold, M.; Bruchfeld, J. Long COVID-19—It’s not over until? Clini. Microbiol. Infect. 2021, 27, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Van den Borst, B.; Peters, J.B.; Brink, M.; Schoon, Y.; Bleeker-Rovers, C.P.; Schers, H.; van Hees, H.W.H.; van Helvoort, H.; van den Boogaard, M.; van der Hoeven, H.; et al. Comprehensive health assessment three months after recovery from acute COVID-19. Clin. Infect. Dis. 2020, 73, e1089–e1098. [Google Scholar] [CrossRef]
- Taboada, M.; Cariñena, A.; Moreno, E.; Rodríguez, N.; Domínguez, M.J.; Casal, A.; Vanessa Riveiro, V.; Diaz-Vieito, M.; Valdés, L.; Álvarez, J.; et al. Post-COVID-19 functional status six-months after hospitalization. J. Infect. 2021, 82, e31–e33. [Google Scholar] [CrossRef]
- Spanish Society of General and Family Physicians (SEMG). Survey of Symptoms and Disability Produced by the Same, in Those Affected by Persistent COVID. 2021, pp. 1–33. Available online: https://www.semg.es (accessed on 1 September 2021).
- Baecke, J.A.; Burema, J.; Frijters, J.E. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am. J. Clin. Nutr. 1982, 36, 936–942. [Google Scholar] [CrossRef]
- Vilagut, G.; Ferrer, M.; Rajmil, L.; Rebollo, P.; Permanyer-Miralda, G.; Quintana, J.M.; Rosalía Santeda, R.; Valderasa, J.M.; Riberad, A.; Domingo-Salvanya, A.; et al. The Spanish SF-36 Health Questionnaire: A decade of experience and new developments by researchers of the Red-IRYSS. Gac. Sanit. 2005, 19, 135–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doykov, I.; Hällqvist, J.; Gilmour, K.C.; Grandjean, L.; Mills, K.; Heywood, W.E. “The long tail of Covid-19”—The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Research 2020, 9, 1349. [Google Scholar] [CrossRef] [PubMed]
- Cojocarum, M.; Cojocarum, I.M.; Silos, I.; Vrabie, C.D. Manifestations of Systemic Lupus Erythematosus. Mædica 2011, 6, 330. [Google Scholar]
- Li, H.; Liu, S.-M.; Yu, X.-H.; Tang, S.-L.; Tang, C.-K. Coronavirus disease 2019 (COVID-19): Current status and future perspectives. Int. J. Antimicrob. Agents 2020, 55, 105951. [Google Scholar] [CrossRef] [PubMed]
- Spanish Society of General and Family Physicians (SEMG). Clinical Guideline for the Care of the Persistent Long COVID/COVID Patient. 2021. Available online: https://www.semg.es/index.php/consensos-guias-y-protocolos/363-guia-clinica-para-la-atencion-al-paciente-long-covid-covid-persistente (accessed on 1 September 2021).
- Muench, P.; Jochum, S.; Wenderoth, V.; Ofenloch-Haehnle, B.; Hombach, M.; Strobl, M.; Henrik Sadlowski, H.; Sachse, C.; Torriani, G.; Isabella Eckerle, I.; et al. Development and Validation of the Elecsys Anti-SARS-CoV-2 Immunoassay as a Highly Specific Tool for Determining Past Exposure to SARS-CoV-2. J. Clin. Microbiol. 2020, 58, 1694–1714. [Google Scholar] [CrossRef]
- Braun, J.; Loyal, L.; Frentsch, M.; Wendisch, D.; Georg, P.; Kurth, F.; Hippenstiel, S.; Dingeldey, M.; Kruse, B.; Fauchere, F.; et al. SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature 2020, 587, 270–274. [Google Scholar] [CrossRef]
- US Food and Drug (FDA). Coronavirus (COVID-19) Update: FDA Authorizes Adaptive Biotechnologies T-Detect COVID Test. FDA. 2021. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-adaptive-biotechnologies-t-detect-covid-test (accessed on 1 September 2021).
- Spanish Society of General and Family Physicians (SEMG). Basic Care Kit for Patients with Persistent COVID-19 Disease. 2021. Available online: https://semst.org/kit-de-atencion-basica-al-paciente-con-enfermedad-covid-19-persistente/ (accessed on 1 September 2021).
- Fernández-Lázaro, D.; González-Bernal, J.J.; Sánchez-Serrano, N.; Navascués, L.J.; Ascaso-del-Río, A.; Mielgo-Ayuso, J. Physical Exercise as a Multimodal Tool for COVID-19: Could It Be Used as a Preventive Strategy? Int. J. Environ. Res. Public Health 2020, 17, 8496. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Lázaro, D.; Sánchez-Serrano, N.; Mielgo-Ayuso, J.; García-Hernández, J.L.; González-Bernal, J.J.; Seco-Calvo, J. Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? J. Clin. Med. 2021, 10, 5799. https://doi.org/10.3390/jcm10245799
Fernández-Lázaro D, Sánchez-Serrano N, Mielgo-Ayuso J, García-Hernández JL, González-Bernal JJ, Seco-Calvo J. Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? Journal of Clinical Medicine. 2021; 10(24):5799. https://doi.org/10.3390/jcm10245799
Chicago/Turabian StyleFernández-Lázaro, Diego, Nerea Sánchez-Serrano, Juan Mielgo-Ayuso, Juan Luis García-Hernández, Jerónimo J. González-Bernal, and Jesús Seco-Calvo. 2021. "Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic?" Journal of Clinical Medicine 10, no. 24: 5799. https://doi.org/10.3390/jcm10245799
APA StyleFernández-Lázaro, D., Sánchez-Serrano, N., Mielgo-Ayuso, J., García-Hernández, J. L., González-Bernal, J. J., & Seco-Calvo, J. (2021). Long COVID a New Derivative in the Chaos of SARS-CoV-2 Infection: The Emergent Pandemic? Journal of Clinical Medicine, 10(24), 5799. https://doi.org/10.3390/jcm10245799









