Bronchoalveolar Lavage and Blood Markers of Infection in Critically Ill Patients—A Single Center Registry Study
Abstract
1. Introduction
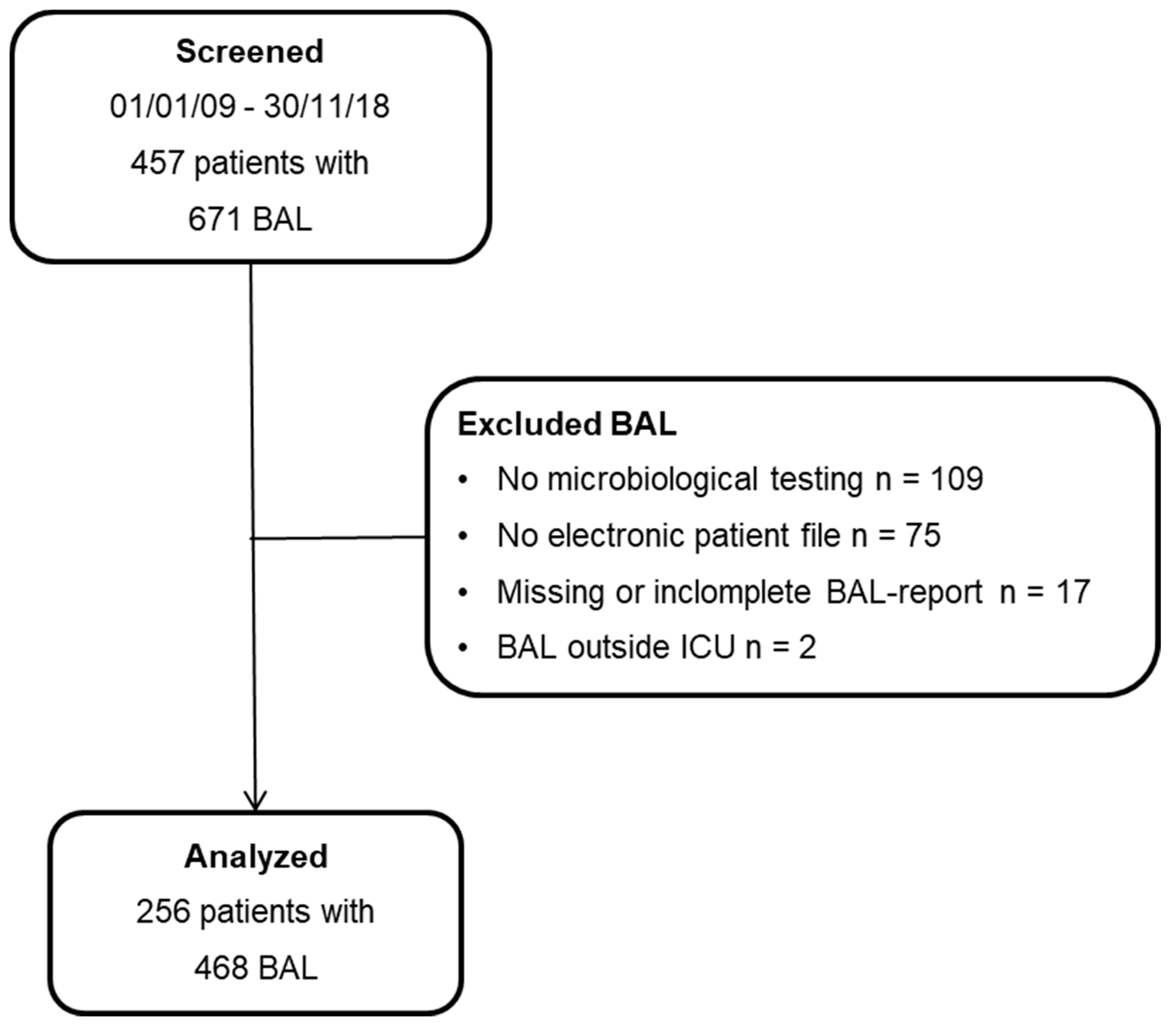
2. Materials and Methods
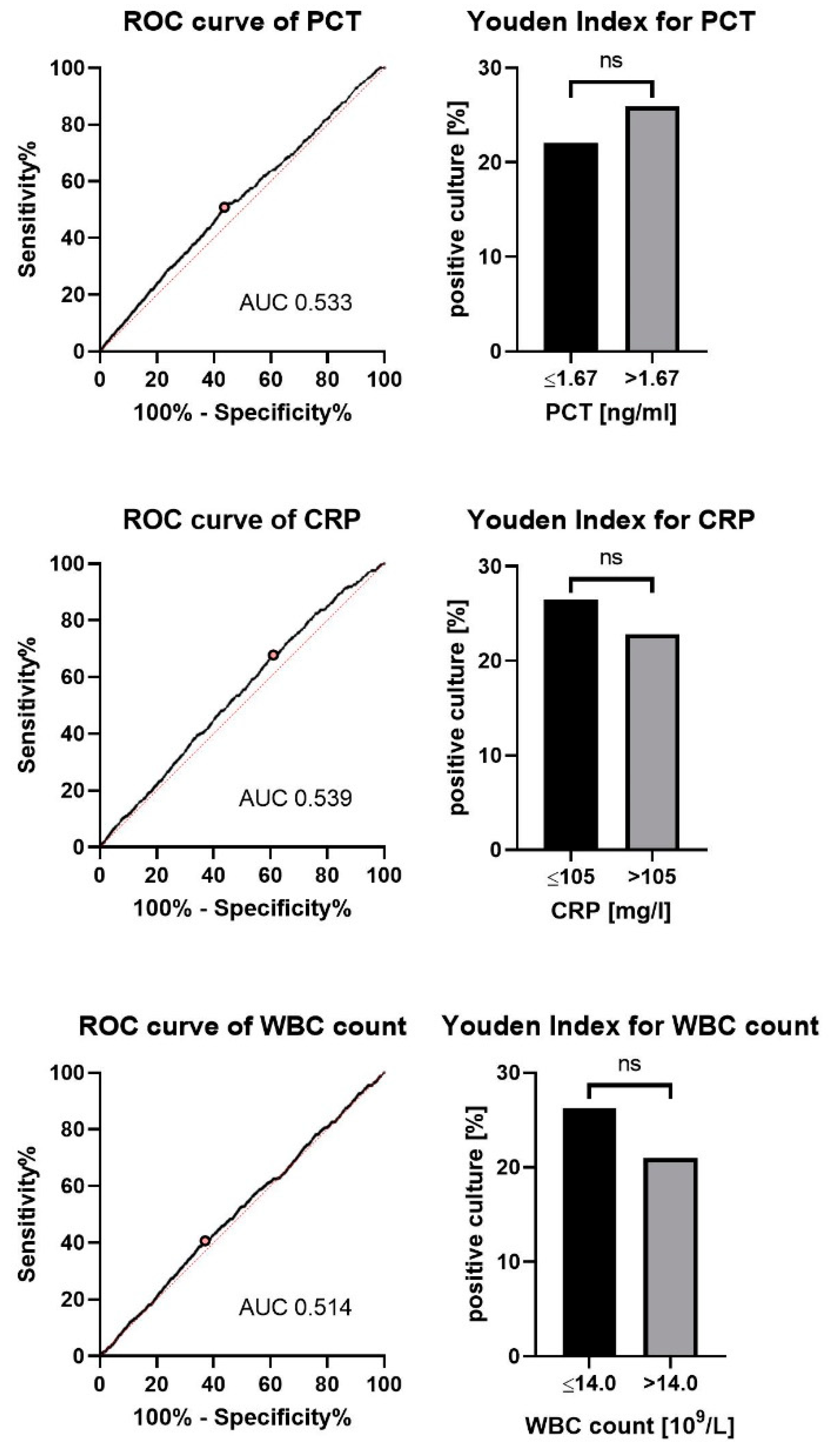
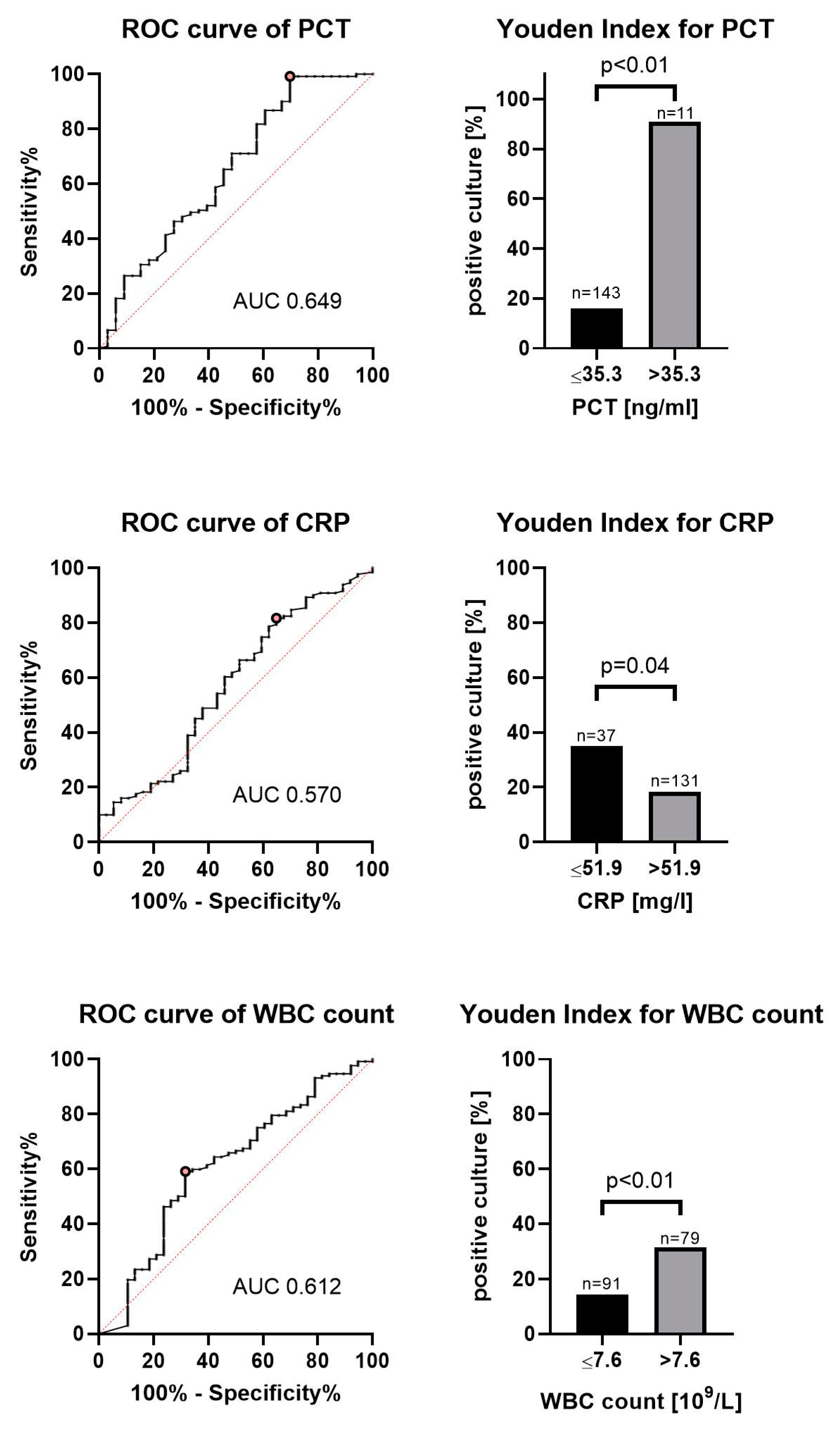
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Olivieri, A.; del Monte, D.; Benacchio, L.; Bonvicini, D.; Biaochim, M.; Allegri, C.; Fornasier, L.; Carlot, A.; Psimadas, I.; Bonato, A.; et al. An Observational Veneto Research on Ventilator-Associated Pneumonia (OVeRVAP): Attributable mortality and cumulative incidence of ventilator-associated pneumonia. Minerva Anestesiol. 2017, 84, 811–819. [Google Scholar]
- Koulenti, D.; Tsigou, E.; Rello, J. Nosocomial pneumonia in 27 ICUs in Europe: Perspectives from the EU-VAP/CAP study. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 1999–2006. [Google Scholar] [CrossRef]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; John-Muscedere, J.; Daniel Sweeney, D.A.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Jordi-Carratalà, J.; et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Dalhoff, K.; Ewig, S. Erwachsene Patienten mit nosokomialer Pneumonie: Epidemiologie. Diagnostik Und Therapie. Dtsch. Arztebl. Int. 2013, 110, 634–640. [Google Scholar]
- Bauer, T.T.; Torres, A.; Ewig, S.; Hernández, C.; Sanchez-Nieto, J.M.; Xaubet, A.; Agustí, C.; Rodriguez-Roisin, R. Effects of bronchoalveolar lavage volume on arterial oxygenation in mechanically ventilated patients with pneumonia. Intensive Care Med. 2001, 27, 384–393. [Google Scholar] [CrossRef]
- Schnabel, R.M.; van der Velden, K.; Osinski, A.; Rohde, G.; Roekaerts, P.; Bergmans, D.C. Clinical course and complications following diagnostic bronchoalveolar lavage in critically ill mechanically ventilated patients. BMC Pulm. Med. 2015, 15, 107. [Google Scholar] [CrossRef]
- Heyland, D.; Cook, D.; Dodek, P.; Muscedere, J.; Day, A. A randomized trial of diagnostic techniques for ventilator-associated pneumonia. N. Engl. J. Med. 2006, 355, 2619–2630. [Google Scholar]
- Karakioulaki, M.; Stolz, D. Biomarkers in pneumonia—Beyond procalcitonin. Int. J. Mol. Sci. 2019, 20, 2004. [Google Scholar] [CrossRef]
- Póvoa, P.; Coelho, L.; Almeida, E.; Fernandes, A.; Mealha, R.; Moreira, P.; Sabino, H. C-reactive protein as a marker of ventilator-associated pneumonia resolution: A pilot study. Eur. Respir. J. 2005, 25, 804–812. [Google Scholar] [CrossRef]
- Póvoa, P.; Coelho, L.; Almeida, E.; Fernandes, A.; Mealha, R.; Moreira, P.; Sabino, H. Early identification of intensive care unit-acquired infections with daily monitoring of C-reactive protein: A prospective observational study. Crit. Care 2006, 10, R63. [Google Scholar] [CrossRef]
- Zissel, G.; Schlaak, M.; Müller-Quernheim, J. Age-related decrease in accessory cell function of human alveolar macrophages. J. Investig. Med. 1999, 47, 51–56. [Google Scholar] [PubMed]
- Bauer, T.T.; Lorenz, J.; Bodmann, K.F.; Vogel, F. Abbreviated guidelines for prevention, diagnostics, and therapy of nosocomial pneumonia. Med. Klin. 2005, 100, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Boussekey, N.; Leroy, O.; Georges, H.; Devos, P.; D’Escrivan, T.; Guery, B. Diagnostic and prognostic values of admission procalcitonin levels in community–acquired pneumonia in an intensive care unit. Infection 2005, 33, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, J.D.; Singanayagam, A.; Hill, A.T. C-Reactive Protein Is an Independent Predictor of Severity in Community-acquired Pneumonia. Am. J. Med. 2008, 121, 219–225. [Google Scholar] [CrossRef]
- Ramirez, P.; Garcia, M.A.; Ferrer, M.; Aznar, J.; Valencia, M.; Sahuquillo, J.M.; Torres, A. Sequential measurements of procalcitonin levels in diagnosing ventilator-associated pneumonia. Eur. Respir. J. 2008, 31, 356–362. [Google Scholar] [CrossRef]
- Dallas, J.; Brown, S.M.; Hock, K.; Scott, M.G.; Skrupky, L.P.; Boyle, W.A.; Kollef, M.H. Diagnostic utility of plasma procalcitonin for nosocomial pneumonia in the intensive care unit setting. Respir. Care 2011, 56, 412–419. [Google Scholar] [CrossRef]
- Duflo, F.; Debon, R.; Monneret, G.; Bienvenu, J.; Chassard, D.; Allaouchiche, B. Alveolar and serum procalcitonin: Diagnostic and prognostic value in ventilator-associated pneumonia. Anesthesiology 2002, 96, 74–79. [Google Scholar] [CrossRef]
- Nobre, V.; Borges, I. Prognostic value of procalcitonin in hospitalized patients with lower respiratory tract infections. Rev. Bras. Ter. Intensiva 2016, 28, 179–189. [Google Scholar] [CrossRef]
- Luyt, C.-E.; Combes, A.; Reynaud, C.; Hekimian, G.; Nieszkowska, A.; Tonnellier, M.; Aubry, A.; Trouillet, J.-L.; Bernard, M.; Chastre, J. Usefulness of procalcitonin for the diagnosis of ventilator-associated pneumonia. Intensive Care Med. 2008, 34, 1434–1440. [Google Scholar] [CrossRef]
- Liao, X.; Kang, Y. Prognostic value of procalcitonin levels in predicting death for patients with ventilator-associated pneumonia. Intensive Care Med. 2010, 36, S102. [Google Scholar]
- Zhou, C.-D.; Lu, Z.-Y.; Ren, N.-Z.; Zhang, G.-C. Diagnostic value of procalcitonin in ventilator associated pneumonia. Chin. Crit. Care Med. 2006, 18, 370–372. (In Chinese) [Google Scholar]
- Linssen, C.F.M.; Bekers, O.; Drent, M.; Jacobs, J.A. C-reactive protein and procalcitonin concentrations in bronchoalveolar lavage fluid as a predictor of ventilator-associated pneumonia. Ann. Clin. Biochem. Int. J. Lab. Med. 2008, 45, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Bèle, N.; Darmon, M.; Coquet, I.; Feugeas, J.-P.; Legriel, S.; Adaoui, N.; Schlemmer, B.; Azoulay, E. Diagnostic accuracy of procalcitonin in critically ill immunocompromised patients. BMC Infect. Dis. 2011, 11, 224. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, L.; Berrens, Z.; Stenson, E.K.; Zackoff, M.; Danziger-Isakov, L.; Lahni, P.; Wong, H.R. Interleukin-27 as a candidate diagnostic biomarker for bacterial infection in immunocompromised pediatric patients. PLoS ONE 2018, 13, e0207620. [Google Scholar] [CrossRef] [PubMed]
- Mikula, T.; Cianciara, J.; Wiercinska-Drapalo, A. Is there any influence of immune deficit on procalcitonin results? Hum. Immunol. 2011, 72, 1194–1197. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.E.; Muir, J.; Kalabalik-Hoganson, J. Procalcitonin in special patient populations: Guidance for anti-microbial therapy. Am. J. Health Syst. Pharm. 2020, 77, 745–758. [Google Scholar]
- Stoma, I.O.; Karpov, I.; Uss, A.; Krivenko, S.; Iskrov, I.; Milanovich, N.; Vlasenkova, S.; Lendina, I.; Belyavskaya, K.; Cherniak, V. Combination of sepsis biomarkers may indicate an invasive fungal infection in haematological patients. Biomarkers 2019, 24, 401–406. [Google Scholar] [CrossRef]
- Morris, A.C.; Kefala, K.; Wilkinson, T.S.; Moncayo-Nieto, O.L.; Dhaliwal, K.; Farrell, L.; Walsh, T.S.; Mackenzie, S.J.; Swann, D.G.; Andrews, P.J.D.; et al. Diagnostic importance of pulmonary interleukin-1beta and interleukin-8 in ventilator-associated pneumonia. Thorax 2010, 65, 201–207. [Google Scholar] [CrossRef]
- Millo, J.L.; Schultz, M.J.; Williams, C.; Weverling, G.J.; Ringrose, T.; Mackinlay, C.I.; van der Poll, T.; Garrard, C.S. Compartmentalisation of cytokines and cytokine inhibitors in ventilator-associated pneumonia. Intensive Care Med. 2004, 30, 68–74. [Google Scholar] [CrossRef]
- Torres, A.; El-Ebiary, M.; Fábregas, N.; González, J.; de la Bellacasa, J.P.; Hernández, C.; Ramírez, J.; Rodriguez-Roisin, R. Value of intracellular bacteria detection in the diagnosis of ventilator associated pneumonia. Thorax 1996, 51, 378–384. [Google Scholar] [CrossRef][Green Version]
| Characteristics | Whole Population | Relevant Bacteria in BAL | No Relevant Bacteria in BAL | p-Value |
|---|---|---|---|---|
| Number of patients | 276 | 62 | 194 | |
| Number of BAL | 468 | 114 | 354 | |
| Average number of BAL per patient | 1.80 | 1.80 | 1.78 | 1 |
| Male gender | 337 (72.0%) | 82 (71.9%) | 255 (72.0%) | 1 |
| ICU-mortality | 195 (41.7%) | 52 (45.6%) | 143 (40.4%) | 0.3282 |
| SAPS 2—Score | 47 (20–95) | 45 (20–79) | 48 (24–95) | 0.1437 |
| TISS 10—Score | 21 (3–40) | 21 (9–36) | 21 (3–40) | 0.9791 |
| Length of ICU stay (days) | 17.8 (0.3–84.3) | 12.8 (0.7–84.3) | 18.2 (0.3–70.8) | 0.4452 |
| Time from admission to BAL (days) | 3.6 (0–64.1) | 2.8 (0–64.1) | 3.8 (0–53) | 0.6754 |
| Pneumonia diagnosed at time of BAL | 435 (92.9%) | 110 (96.5%) | 325 (91.8%) | 0.0963 |
| Immunocompromised | 170 (36.3%) | 38 (33.3%) | 132 (37.3%) | 0.5021 |
| Patients on mechanical ventilation | 442 (94.4%) | 111 (97.4%) | 331 (93.5%) | 0.1579 |
| Duration of mechanical ventilation (days) | 4.6 (0–451) | 3 (0–450.6) | 5.4 (0–378.8) | 0.3233 |
| Patients on corticosteroids at time of BAL | 225 (48.1%) | 41 (36.0%) | 184 (52.0%) | 0.0035 |
| Patients on antibiotics at time of BAL | 450 (96.2%) | 111 (97.4%) | 339 (95.8%) | 0.5812 |
| No. of antibiotics in used at time of BAL | 2 (0–7) | 2 (0–7) | 2 (0–5) | 0.9432 |
| Patients on antimycotic at time of BAL | 138 (29.5%) | 17 (14.9%) | 121 (34.2%) | 0.0001 |
| PCT (ng/mL) | 1.25 (0–601.2) | 1.6 (0–476.9) | 1.2 (0–601.2) | 0.0724 |
| PCT out of normal range | 320 (76.2%) | 78 (78.0%) | 242 (75.6%) | 0.6878 |
| CRP (mg/l) | 136.3 (0–563) | 124 (4–554) | 138 (0–563) | 0.7029 |
| CRP out of normal range | 451 (96.4%) | 110 (98.2%) | 342 (98.0%) | 1 |
| Median WBC (×103/mL) | 11.3 (0–190) | 11 (0–58.4) | 11.3 (0–190) | 0.7683 |
| WBC out of normal range | 321 (68.6%) | 74 (64.9%) | 247 (69.8%) | 0.3541 |
| Whole Population | |
|---|---|
| Number of BAL performed | 468 (100%) |
| Any bacteria cultivated | 220 (47.0%) |
| Relevant bacteria | 114 (24.4%) |
| Any microorganism cultivated * | 303 (64.7%) |
| Relevant microorganism * | 126 (26.9%) |
| No. of microorganisms * | 511 |
| No. of relevant microorganism * | 167 |
| No. of microorganisms per BAL * | 1 (0–5) |
| No. of relevant microorganisms per BAL * | 0 (0–4) |
| Any fungi cultivated | 199 (42.5%) |
| Relevant fungi | 18 (4.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kronberger, J.F.; Köhler, T.C.; Lang, C.N.; Jäckel, M.; Bemtgen, X.; Wengenmayer, T.; Supady, A.; Meschede, W.; Bode, C.; Zotzmann, V.; et al. Bronchoalveolar Lavage and Blood Markers of Infection in Critically Ill Patients—A Single Center Registry Study. J. Clin. Med. 2021, 10, 486. https://doi.org/10.3390/jcm10030486
Kronberger JF, Köhler TC, Lang CN, Jäckel M, Bemtgen X, Wengenmayer T, Supady A, Meschede W, Bode C, Zotzmann V, et al. Bronchoalveolar Lavage and Blood Markers of Infection in Critically Ill Patients—A Single Center Registry Study. Journal of Clinical Medicine. 2021; 10(3):486. https://doi.org/10.3390/jcm10030486
Chicago/Turabian StyleKronberger, Jarno F., Thomas C. Köhler, Corinna N. Lang, Markus Jäckel, Xavier Bemtgen, Tobias Wengenmayer, Alexander Supady, Wolfram Meschede, Christoph Bode, Viviane Zotzmann, and et al. 2021. "Bronchoalveolar Lavage and Blood Markers of Infection in Critically Ill Patients—A Single Center Registry Study" Journal of Clinical Medicine 10, no. 3: 486. https://doi.org/10.3390/jcm10030486
APA StyleKronberger, J. F., Köhler, T. C., Lang, C. N., Jäckel, M., Bemtgen, X., Wengenmayer, T., Supady, A., Meschede, W., Bode, C., Zotzmann, V., & Staudacher, D. L. (2021). Bronchoalveolar Lavage and Blood Markers of Infection in Critically Ill Patients—A Single Center Registry Study. Journal of Clinical Medicine, 10(3), 486. https://doi.org/10.3390/jcm10030486






