Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval
2.3. Participants
2.4. Outcome Measures
2.5. Data Sources/Measurement
2.6. Sample Size
2.7. Statistical Methods
3. Results
3.1. Participants
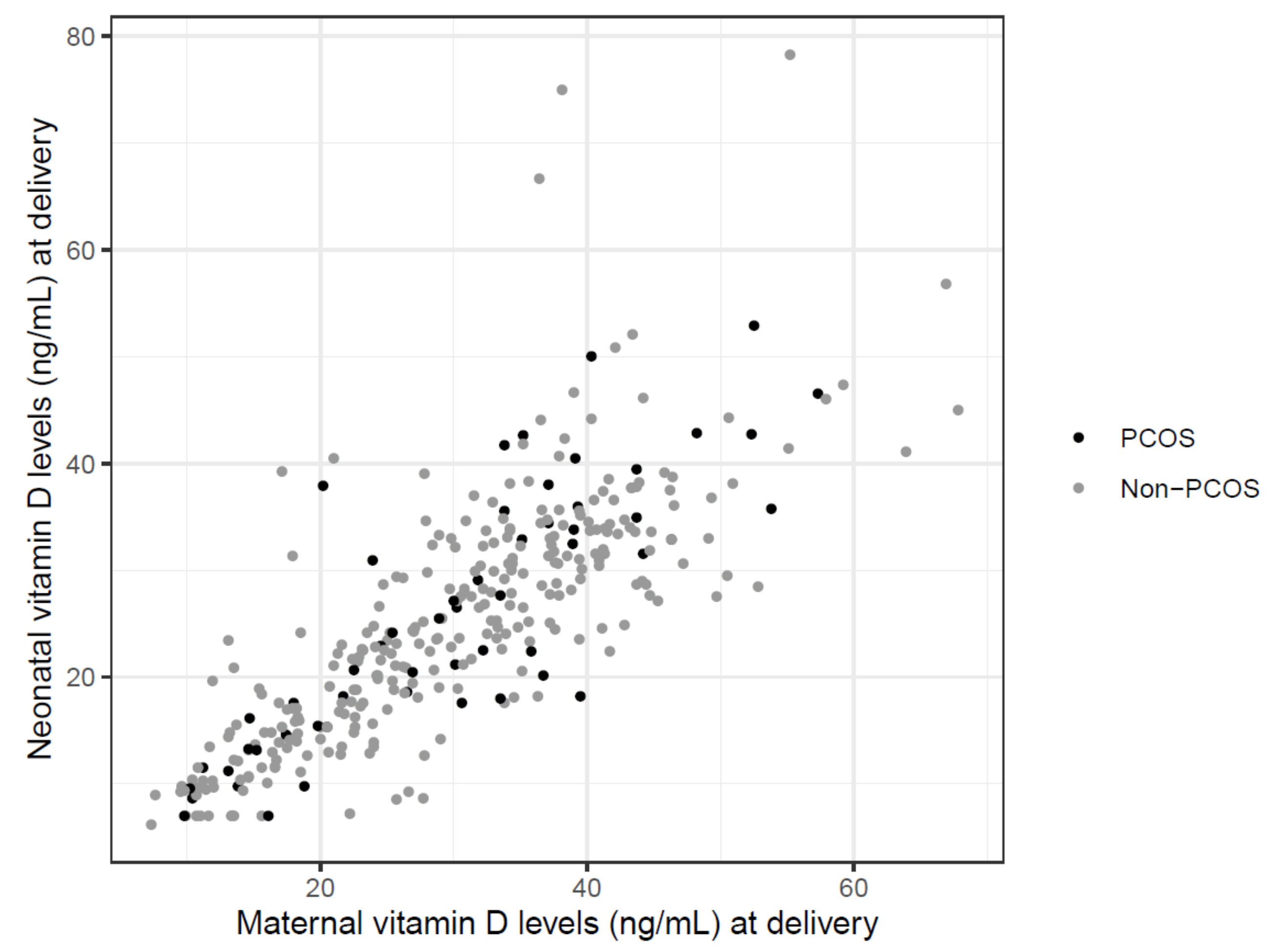
3.2. Primary Results
3.3. Secondary Results
4. Discussion
4.1. Key Results
4.2. Interpretation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Norman, R.J.; Dewailly, D.; Legro, R.S.; Hickey, T.E. Polycystic ovary syndrome. Lancet 2007, 370, 685–697. [Google Scholar] [CrossRef]
- Fauser, B.; Tarlatzis, B.C.; Rebar, R.W.; Legro, R.S.; Balen, A.H.; Lobo, R.; Carmina, E.; Chang, J.; Yildiz, B.O.; Laven, J.S.; et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): The Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil. Steril. 2012, 97, 28–38.e5. [Google Scholar] [CrossRef] [PubMed]
- Wild, R.A. Long-term health consequences of PCOS. Hum. Reprod. Updat. 2002, 8, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Kollmann, M.; Klaritsch, P.; Martins, W.; Guenther, F.; Schneider, V.; Herzog, S.; Craciunas, L.; Lang, U.; Obermayer-Pietsch, B.; Lerchbaum, E.; et al. Maternal and neonatal outcomes in pregnant women with PCOS: Comparison of different diagnostic definitions. Hum. Reprod. 2015, 30, 2396–2403. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; De Wilde, M.A.; Falbo, A.; Koster, M.P.; La Sala, G.B.; Fauser, B.C. Pregnancy complications in women with polycystic ovary syndrome. Hum. Reprod. Updat. 2015, 21, 575–592. [Google Scholar] [CrossRef]
- Boomsma, C.; Eijkemans, M.J.C.; Hughes, E.; Visser, G.; Fauser, B.; Macklon, N.S. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum. Reprod. Updat. 2006, 12, 673–683. [Google Scholar] [CrossRef]
- Qin, J.Z.; Pang, L.H.; Li, M.J.; Fan, X.J.; Huang, R.D.; Chen, H.Y. Obstetric complications in women with polycystic ovary syndrome: A systematic review and meta-analysis. Reprod. Biol. Endocrinol. 2013, 11, 1–56. [Google Scholar] [CrossRef]
- Purswani, J.M.; Gala, P.; Dwarkanath, P.; Larkin, H.M.; Kurpad, A.V.; Mehta, S. The role of vitamin D in pre-eclampsia: A systematic review. BMC Pregnancy Childbirth 2017, 17, 231. [Google Scholar] [CrossRef]
- O’Callaghan, K.M.; Kiely, M. Systematic Review of Vitamin D and Hypertensive Disorders of Pregnancy. Nutrients 2018, 10, 294. [Google Scholar] [CrossRef]
- Akbari, S.; Khodadadi, B.; Ahmadi, S.A.Y.; Abbaszadeh, S.; Shahsavar, F. Association of vitamin D level and vitamin D deficiency with risk of preeclampsia: A systematic review and updated meta-analysis. Taiwan J. Obstet. Gynecol. 2018, 57, 241–247. [Google Scholar] [CrossRef]
- Tabesh, M.; Salehi-Abargouei, A.; Tabesh, M.; Esmaillzadeh, A. Maternal Vitamin D Status and Risk of Pre-Eclampsia: A Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2013, 98, 3165–3173. [Google Scholar] [CrossRef] [PubMed]
- Hyppönen, E.; Cavadino, A.; Williams, D.; Fraser, A.; Vereczkey, A.; Fraser, W.D.; Bánhidy, F.; Lawlor, D.A.; Czeizel, A.E. Vitamin D and Pre-Eclampsia: Original Data, Systematic Review and Meta-Analysis. Ann. Nutr. Metab. 2013, 63, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Amraei, M.; Mohamadpour, S.; Sayehmiri, K.; Mousavi, S.F.; Shirzadpour, E.; Moayeri, A. Effects of Vitamin D Deficiency on Inci-dence Risk of Gestational Diabetes Mellitus: A Systematic Review and Meta-analysis. Front. Endocrinol. 2018, 9, 7. [Google Scholar] [CrossRef]
- Zhang, M.-X.; Pan, G.-T.; Guo, J.-F.; Li, B.; Qin, L.-Q.; Zhang, Z.-L. Vitamin D Deficiency Increases the Risk of Gestational Diabetes Mellitus: A Meta-Analysis of Observational Studies. Nutrients 2015, 7, 8366–8375. [Google Scholar] [CrossRef]
- Zhang, Y.; Gong, Y.; Xue, H.; Xiong, J.; Cheng, G. Vitamin D and gestational diabetes mellitus: A systematic review based on data free of Hawthorne effect. BJOG 2018, 125, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Xu, Y.; Lv, L.; Zhang, M. Association between vitamin D status and the risk of gestational diabetes mellitus: A meta-analysis. Arch. Gynecol. Obstet. 2016, 293, 959–966. [Google Scholar] [CrossRef]
- Poel, Y.; Hummel, P.; Lips, P.; Stam, F.; Van Der Ploeg, T.; Simsek, S. Vitamin D and gestational diabetes: A systematic review and meta-analysis. Eur. J. Intern. Med. 2012, 23, 465–469. [Google Scholar] [CrossRef]
- Thomson, R.L.; Spedding, S.; Buckley, J.D. Vitamin D in the aetiology and management of polycystic ovary syndrome. Clin. Endocrinol. 2012, 77, 343–350. [Google Scholar] [CrossRef]
- He, C.; Lin, Z.; Wagner, S.E.; Ezeamama, A.E. Serum Vitamin D Levels and Polycystic Ovary syndrome: A Systematic Review and Meta-Analysis. Nutrients 2015, 7, 4555–4577. [Google Scholar] [CrossRef]
- O’Callaghan, K.M.; Hennessy, Á.; Hull, G.L.J.; Healy, K.; Ritz, C.; Kenny, L.C.; Kiely, M.E. Estimation of the maternal vitamin D intake that maintains circulating 25-hydroxyvitamin D in late gestation at a concentration sufficient to keep umbilical cord sera ≥25–30 nmol/L: A dose-response, double-blind, randomized placebo-controlled trial in pregnant women at northern latitude. Am. J. Clin. Nutr. 2018, 108, 77–91. [Google Scholar]
- Pilz, S.; Zittermann, A.; Obeid, R.; Hahn, A.; Pludowski, P.; Trummer, C.; Lerchbaum, E.; Pérez-López, F.R.; Karras, S.; März, W. The Role of Vitamin D in Fertility and during Pregnancy and Lactation: A Review of Clinical Data. Int. J. Environ. Res. Public Health 2018, 15, 2241. [Google Scholar] [CrossRef] [PubMed]
- Hollis, B.W.; Wagner, C.L. New insights into the vitamin D requirements during pregnancy. Bone Res. 2017, 5, 17030. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.L.; Hollis, B.W.; Kotsa, K.; Fakhoury, H.; Karras, S. Vitamin D administration during pregnancy as prevention for pregnancy, neonatal and postnatal complications. Rev. Endocr. Metab. Disord. 2017, 18, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Karras, S.N.; Wagner, C.L.; Castracane, V.D. Understanding vitamin D metabolism in pregnancy: From physiology to patho-physiology and clinical outcomes. Metabolism 2018, 86, 112–123. [Google Scholar] [CrossRef]
- Ganguly, A.; Tamblyn, J.A.; Finn-Sell, S.; Chan, S.-Y.; Westwood, M.; Gupta, J.; Kilby, M.D.; Gross, S.R.; Hewison, M. Vitamin D, the placenta and early pregnancy: Effects on trophoblast function. J. Endocrinol. 2018, 236, R93–R103. [Google Scholar] [CrossRef]
- Dovnik, A.; Mujezinović, F. The Association of Vitamin D Levels with Common Pregnancy Complications. Nutrients 2018, 10, 867. [Google Scholar] [CrossRef]
- Van der Pligt, P.; Willcox, J.; Szymlek-Gay, E.A.; Murray, E.; Worsley, A.; Daly, R.M. Associations of Maternal Vitamin D Deficiency with Pregnancy and Neonatal Complications in Developing Countries: A Systematic Review. Nutrients 2018, 10, 640. [Google Scholar] [CrossRef]
- Amegah, A.K.; Klevor, M.K.; Wagner, C.L. Maternal vitamin D insufficiency and risk of adverse pregnancy and birth outcomes: A systematic review and meta-analysis of longitudinal studies. PLoS ONE 2017, 12, e0173605. [Google Scholar] [CrossRef]
- Aghajafari, F.; Nagulesapillai, T.; Ronksley, P.E.; Tough, S.C.; O’Beirne, M.; Rabi, D.M. Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: Systematic review and meta-analysis of observational studies. BMJ 2013, 346, f1169. [Google Scholar] [CrossRef]
- The Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil. Steril. 2004, 81, 19–25. [Google Scholar] [CrossRef]
- Kollmann, M.; Obermayer-Pietsch, B.; Lerchbaum, E.; Lang, U.; Herzog, S.A.; Trummer, C.; Scheuchenegger, A.; Ulrich, D.; Klaritsch, P. Androgen and Anti-Mullerian Hormone Concentrations at Term in Newborns and Their Mothers with and without Polycystic Ovary Syndrome. J. Clin. Med. 2019, 8, 1817. [Google Scholar] [CrossRef] [PubMed]
- Lips, P.; Cashman, K.D.; Lamberg-Allardt, C.; Bischoff-Ferrari, H.A.; Obermayer-Pietsch, B.; Bianchi, M.L.; Bouillon, R. Current Vitamin D Status in European and Middle East Countries and Strategies to Prevent Vitamin D Deficiency: A Position Statement of the European Calcified Tissue Society. Eur. J. Endocrinol. 2019, 180, P23–P54. [Google Scholar] [CrossRef] [PubMed]
- Team RC. R: A Language and Environment for Statistical Computing; Team RC: Vienna, Austria, 2017. [Google Scholar]
- Cashman, K.D.; Dowling, K.G.; Škrabáková, Z.; Gonzalez-Gross, M.; Valtueña, J.; De Henauw, S.; Moreno, L.; Damsgaard, C.T.; Michaelsen, K.F.; Mølgaard, C.; et al. Vitamin D deficiency in Europe: Pandemic? Am. J. Clin. Nutr. 2016, 103, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Lerchbaum, E.; Rabe, T. Vitamin D and female fertility. Curr. Opin. Obstet. Gynecol. 2014, 26, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Merhi, Z.; Büyük, E.; Cipolla, M.J. Advanced glycation end products alter steroidogenic gene expression by granulosa cells: An effect partially reversible by vitamin D. Mol. Hum. Reprod. 2018, 24, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Merhi, Z. Crosstalk between advanced glycation end products and vitamin D: A compelling paradigm for the treatment of ovarian dysfunction in PCOS. Mol. Cell. Endocrinol. 2019, 479, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Larqué, E.; Morales, E.; Leis, R.; Blanco-Carnero, J.E. Maternal and Foetal Health Implications of Vitamin D Status during Preg-nancy. Ann. Nutr. Metab. 2018, 72, 179–192. [Google Scholar] [CrossRef]
- Rosen, C.J.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; Kovacs, C.S.; et al. IOM Committee Members Respond to Endocrine Society Vitamin D Guideline. J. Clin. Endocrinol. Metab. 2012, 97, 1146–1152. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An En-docrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- De-Regil, L.M.; Palacios, C.; Lombardo, L.K.; Peña-Rosas, J.P. Vitamin D supplementation for women during pregnancy. Sao Paulo Med. J. 2016, 134, 274–275. [Google Scholar] [CrossRef]
- Akbari, M.; Moosazadeh, M.; Lankarani, K.B.; Tabrizi, R.; Samimi, M.; Karamali, M.; Jamilian, M.; Kolahdooz, F.; Asemi, Z. Correction: The Effects of Vitamin D Supplementation on Glucose Metabolism and Lipid Profiles in Patients with Gestational Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Horm. Metab. Res. 2017, 49, 647–653. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vahdaninia, M.; Mackenzie, H.; Helps, S.; Dean, T. Prenatal Intake of Vitamins and Allergic Outcomes in the Offspring: A Sys-tematic Review and Meta-Analysis. J. Allergy Clin. Immunol. Pract. 2017, 5, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Netting, M.J.; Middleton, P.F.; Makrides, M. Does maternal diet during pregnancy and lactation affect outcomes in offspring? A systematic review of food-based approaches. Nutrition 2014, 30, 1225–1241. [Google Scholar] [CrossRef] [PubMed]
- Harvey, N.C.; Holroyd, C.; Ntani, G.; Javaid, K.; Cooper, P.; Moon, R.; Cole, Z.; Tinati, T.; Godfrey, K.; Dennison, E.; et al. Vitamin D supplementation in pregnancy: A systematic review. Health Technol. Assess. 2014, 18, 1–190. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.-M.; Ma, Z.-Z.; Liu, G.-J.; Wang, L.-L.; Guo, Y. Vitamins supplementation affects the onset of preeclampsia. J. Formos. Med. Assoc. 2018, 117, 6–13. [Google Scholar] [CrossRef]
- Khaing, W.; Vallibhakara, S.A.-O.; Tantrakul, V.; Vallibhakara, O.; Rattanasiri, S.; McEvoy, M.A.; Attia, J.; Thakkinstian, A. Calcium and Vitamin D Supplementation for Prevention of Preeclampsia: A Systematic Review and Network Meta-Analysis. Nutrients 2017, 9, 1141. [Google Scholar] [CrossRef]
- Thorne-Lyman, A.; Fawzi, W.W. Vitamin D during pregnancy and maternal, neonatal and infant health outcomes: A systemat-ic review and meta-analysis. Paediatr. Perinat. Epidemiol. 2012, 26 (Suppl. 1), 75–90. [Google Scholar] [CrossRef]
- Rostami, M.; Tehrani, F.R.; Simbar, M.; Yarandi, R.B.; Minooee, S.; Hollis, B.W.; Hosseinpanah, F. Effectiveness of Prenatal Vitamin D Deficiency Screening and Treatment Program: A Stratified Randomized Field Trial. J. Clin. Endocrinol. Metab. 2018, 103, 2936–2948. [Google Scholar] [CrossRef]
- Ali, A.M.; Alobaid, A.; Malhis, T.N.; Khattab, A.F. Effect of vitamin D3 supplementation in pregnancy on risk of pre-eclampsia—Randomized controlled trial. Clin. Nutr. 2019, 38, 557–563. [Google Scholar] [CrossRef]
- Magnus, M.C.; Miliku, K.; Bauer, A.; Engel, S.M.; Felix, J.F.; Jaddoe, V.W.; Fraser, A. Vitamin D and risk of pregnancy related hypertensive disorders: Mendelian random-isation study. BMJ 2018, 361, k2167. [Google Scholar] [CrossRef]
- Roth, D.E.; Morris, S.K.; Zlotkin, S.; Gernand, A.D.; Ahmed, T.; Shanta, S.S.; Papp, E.; Korsiak, J.; Shi, J.; Islam, M.M.; et al. Vitamin D Supplementation in Pregnancy and Lactation and Infant Growth. N. Engl. J. Med. 2018, 379, 535–546. [Google Scholar] [CrossRef] [PubMed]
- Hollis, B.W.; Johnson, D.; Hulsey, T.C.; Ebeling, M.; Wagner, C.L. Vitamin D supplementation during pregnancy: Double-blind, randomized clinical trial of safety and effectiveness. J. Bone Miner. Res. 2011, 26, 2341–2357. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.E.; Leung, M.; Mesfin, E.; Qamar, H.; Watterworth, J.; Papp, E. Vitamin D supplementation during pregnancy: State of the evidence from a systematic review of randomised trials. BMJ 2017, 359, j5237. [Google Scholar] [CrossRef] [PubMed]
- Bi, W.G.; Nuyt, A.M.; Weiler, H.; LeDuc, L.; Santamaria, C.; Wei, S.Q. Association between Vitamin D Supplementation during Pregnancy and Offspring Growth, Morbidity, and Mortality: A Systematic Review and Meta-analysis. JAMA Pediatr. 2018, 172, 635–645. [Google Scholar] [CrossRef]
| 25(OH)D Deficiency | p-Value | ||
|---|---|---|---|
| n | % | ||
| PCOS women | 18 | 26.9 | 0.43 |
| Non-PCOS women | 71 | 22.5 | |
| Neonates of PCOS women | 21 | 37.5 | 0.88 |
| Neonates on Non-PCOS women | 107 | 35.7 | |
| PCOS girls | 10 | 37 | 1.0 |
| Non-PCOS girls | 58 | 38.4 | |
| PCOS boys | 11 | 37.9 | 0.70 |
| Non-PCOS boys | 49 | 32.9 | |
| PCOS Women | p-Value | Non-PCOS Women | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Maternal Complications | Yes | No | Yes | No | ||||||
| Gestational diabetes | 30.4 | 14.6–53.8 | 30.2 | 9.8–57.3 | 0.735 | 34.5 | 11.9–66.9 | 28.8 | 7.3–68.2 | 0.190 |
| PIH | 30.4 | 16.2–48.2 | 30.2 | 9.8–57.3 | 0.790 | 23.6 | 11.9–40.1 | 29.8 | 7.3–68.2 | 0.128 |
| Pre-eclampsia | 32.8 | 30.4–35.2 | 30.1 | 9.8–57.3 | 0.658 | 30.4 | 11.9–34.1 | 29.1 | 7.3–68.2 | 0.476 |
| Operative delivery | 30.5 | 10.4–57.3 | 30.1 | 9.8–52.5 | 0.320 | 29.4 | 7.6–67.8 | 29.3 | 7.3–68.2 | 0.871 |
| Any complication | 32.0 | 10.4–57.3 | 28.9 | 9.8–52.5 | 0.132 | 29.1 | 7.6–67.8 | 29.8 | 7.3–68.2 | 0.622 |
| Neonates of PCOS Women | p-Value | Neonates of Non-PCOS Women | p-Value | |||||||
| Neonatal Complications | Yes | No | Yes | No | ||||||
| SGA (<10th percentile) | 21.3 | 15.4–39.4 | 24.8 | 7.0–52.9 | 0.832 | 29.6 | 10.3–56.8 | 23.8 | 6.2–78.3 | 0.082 |
| LGA (>90th percentile) | 24.8 | 14.6–34.9 | 23.5 | 7.0–52.9 | 0.912 | 19.8 | 7.0–37.7 | 24.6 | 6.2–78.3 | 0.213 |
| Fetal growth restriction | - | - | 23.5 | 7.0–52.9 | - | 46.0 | 35.1–56.8 | 24.3 | 6.2–78.3 | 0.039 |
| Fetal acidosis | 44.1 | 41.7–46.5 | 22.7 | 7.0–52.9 | 0.040 | 27.1 | 13.9–46.1 | 24.3 | 6.2–78.3 | 0.394 |
| ICU | 34.9 | 34.9–34.9 | 22.9 | 7.0–52.9 | 0.421 | 37.5 | 35.1–46.1 | 24.2 | 6.2–78.3 | 0.015 |
| Any complication | 32.2 | 14.6–46.5 | 22.7 | 7.0–52.9 | 0.219 | 27.6 | 7.0–56.8 | 23.8 | 6.2–78.3 | 0.199 |
| Maternal complications | PCOS women 25(OH)D < 20 ng/mL | PCOS women 25(OH)D ≥ 20 ng/mL | p-value |
| 11 (61.1) | 33 (67.3) | 0.773 | |
| Non-PCOS women 25(OH)D < 20 ng/mL | Non-PCOS women 25(OH)D ≥ 20 ng/mL | ||
| 34 (47.9) | 121 (49.4) | 0.893 | |
| Neonatal complications | Neonates of PCOS women 25(OH)D < 20 ng/mL | Neonates of PCOS women 25(OH)D ≥ 20 ng/mL | |
| 3 (14.3) | 9 (25.7) | 0.503 | |
| Neonates of Non-PCOS women 25(OH)D < 20 ng/mL | Neonates of Non-PCOS women 25(OH)D ≥ 20 ng/mL | ||
| 19 (17.8) | 43 (22.3) | 0.376 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kollmann, M.; Obermayer-Pietsch, B.; Lerchbaum, E.; Feigl, S.; Hochstätter, R.; Pregartner, G.; Trummer, C.; Klaritsch, P. Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome. J. Clin. Med. 2021, 10, 537. https://doi.org/10.3390/jcm10030537
Kollmann M, Obermayer-Pietsch B, Lerchbaum E, Feigl S, Hochstätter R, Pregartner G, Trummer C, Klaritsch P. Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome. Journal of Clinical Medicine. 2021; 10(3):537. https://doi.org/10.3390/jcm10030537
Chicago/Turabian StyleKollmann, Martina, Barbara Obermayer-Pietsch, Elisabeth Lerchbaum, Sarah Feigl, Rüdiger Hochstätter, Gudrun Pregartner, Christian Trummer, and Philipp Klaritsch. 2021. "Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome" Journal of Clinical Medicine 10, no. 3: 537. https://doi.org/10.3390/jcm10030537
APA StyleKollmann, M., Obermayer-Pietsch, B., Lerchbaum, E., Feigl, S., Hochstätter, R., Pregartner, G., Trummer, C., & Klaritsch, P. (2021). Vitamin D Concentrations at Term Do Not Differ in Newborns and Their Mothers with and without Polycystic Ovary Syndrome. Journal of Clinical Medicine, 10(3), 537. https://doi.org/10.3390/jcm10030537







