Prevalence of Post-Concussion-Like Symptoms in the General Injury Population and the Association with Health-Related Quality of Life, Health Care Use, and Return to Work
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Study Population
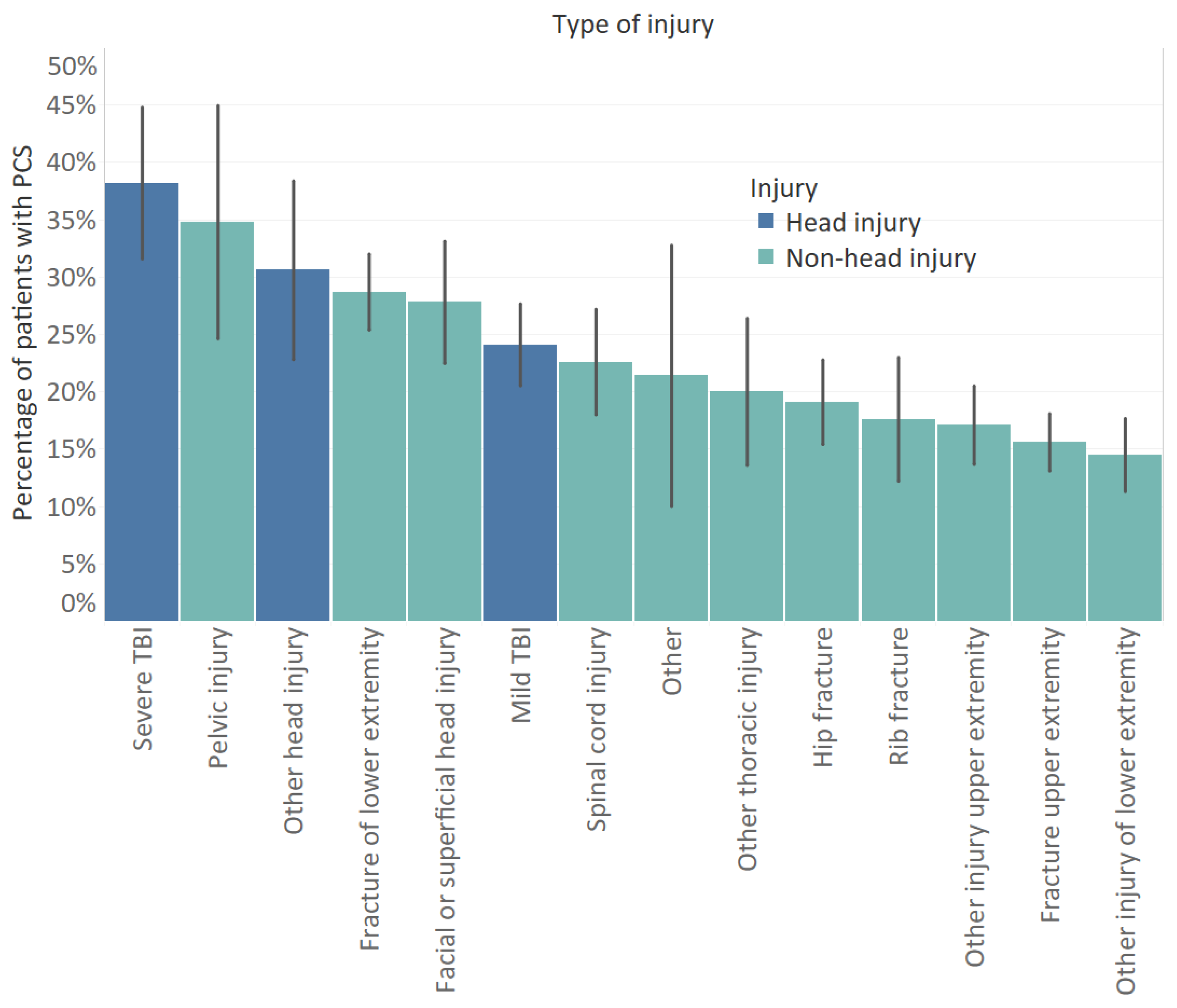
3.2. Prevalence of Post-Concussion-Like Symptoms
3.3. Risk Factors for PCS
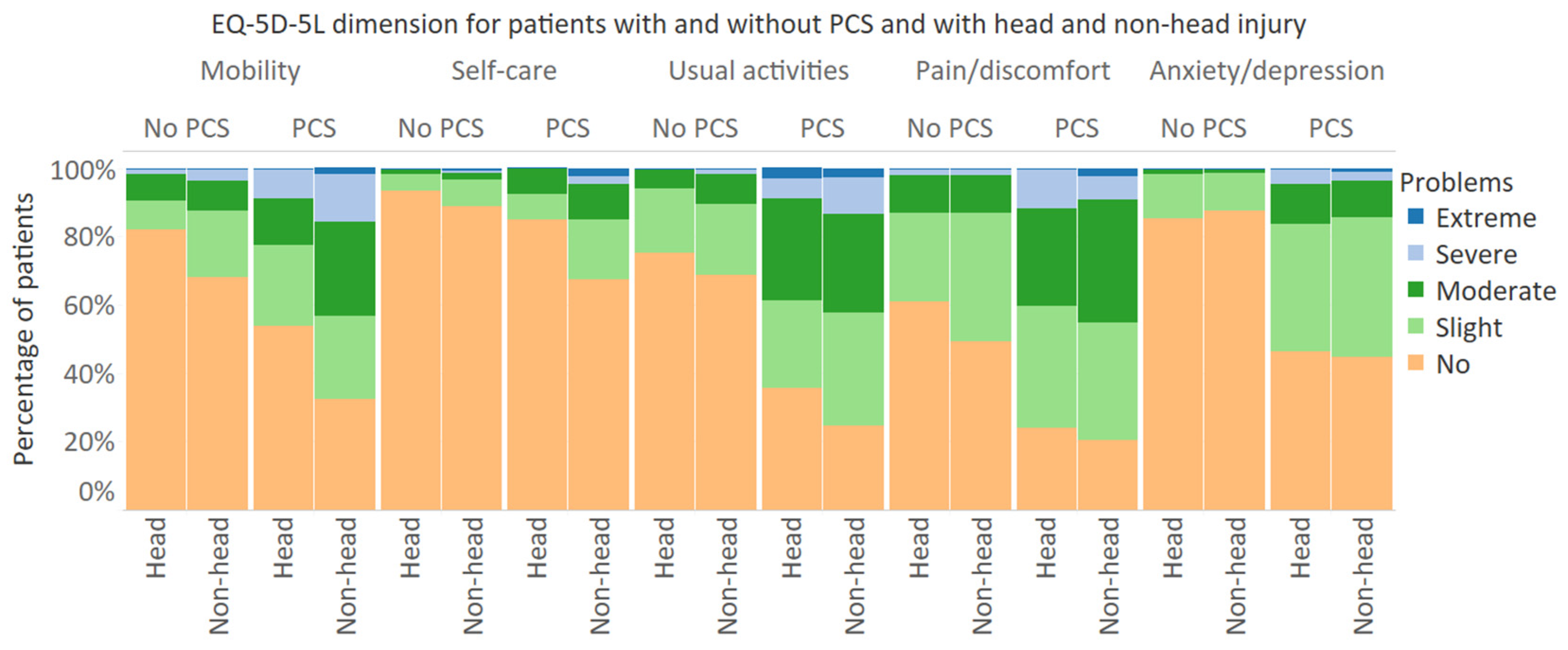
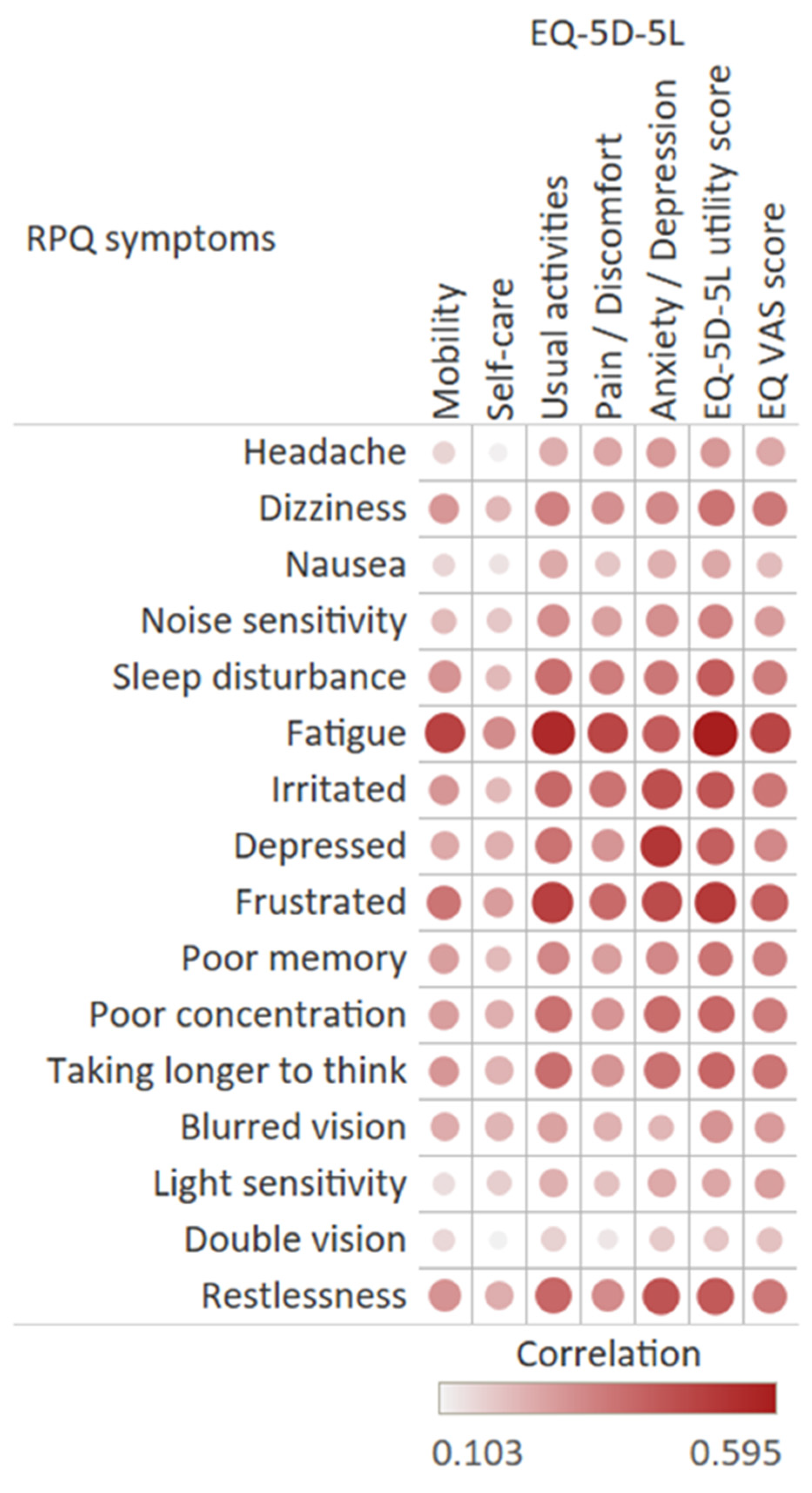
3.4. Health-Related Quality of Life
3.5. Health Care Utilization
3.6. Return to Work
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

| Characteristic | Group | Head Injury Patients | Non-Head Injury Patients | ||
|---|---|---|---|---|---|
| Univariable OR (95% CI) | Multivariable> OR (95% CI) | Univariable OR (95% CI) | Multivariable OR (95% CI) | ||
| Age | 0.990 (0.974; 1.007) | 0.974 * (0.953; 0.995) | 1.013 * (1.002; 1.023) | 0.996 (0.984; 1.009) | |
| Sex | Male | Ref | Ref | ||
| Female | 1.546 (0.875; 2.731) | 1.204 (0.889; 1.632) | |||
| Living situation | Not Alone | Ref | Ref | ||
| Alone | 0.886 (0.469; 1.672) | 1.314 (0.935; 1.846) | |||
| Educational level | Low | Ref | Ref | Ref | Ref |
| Middle | 0.832 (0.412; 1.682) | 0.725 (0.321; 1.643) | 0.641 * (0.442; 0.929) | 0.730 (0.485; 1.098) | |
| High | 0.586 (0.292; 1.175) | 0.574 (0.259; 1.276) | 0.534 * (0.362; 0.787) | 0.627 * (0.410; 0.960) | |
| Injury mechanism | Home and leisure accident | Ref | Ref | Ref | Ref |
| Road traffic accident | 1.090 (0.594; 2.001) | 1.168 (0.574; 2.377) | 1.452 * (1.023; 2.060) | 1.349 (0.918; 1.982) | |
| Sports accident | 0.500 (0.156; 1.604) | 0.449 (0.116; 1.736) | 0.483 * (0.268; 0.870) | 0.714 (0.378; 1.351) | |
| Occupational accident | 1.250 (0.291; 5.375) | 2.046 (0.387; 10.810) | 1.344 (0.750; 2.410) | 1.422 (0.740; 2.734) | |
| Number of injuries | 1 | Ref | Ref | Ref | Ref |
| 2 | 0.573 (0.299; 1.097) | 0.745 (0.367; 1.513) | 1.265 (0.840; 1.906) | 1.053 * (1.021; 1.090) | |
| ≥3 | 0.324 * (0.149; 0.704) | 0.288 * (0.119; 0.694) | 3.631 * (1.982; 6.652) | 3.531 * (1.832; 6.805) | |
| Chronic disease | No chronic disease | ||||
| 1 chronic disease | 2.894 * (1.513; 6.925) | 3.531 * (1.707; 7.300) | 2.240 * (1.562; 3.213) | 2.342 * (1603; 3.423) | |
| 2 or more chronic diseases | 2.952 * (1.258; 6.925) | 3.752 * (1.417; 9.932) | 4.315 * (2.889; 6.446) | 4.607 * (3.000; 7.075) | |
| Length of hospital stay | 1.064 * (1.006; 1.125) | 1.079 * (1.012; 1.151) | 1.065 * (1.033; 1.099) | 1.055 * (1.021; 1.090) | |
| 6 Months after Injury | ||||
|---|---|---|---|---|
| No PCS | PCS | |||
| Health-Related Quality of Life | Non-Head | Head | Non-Head | Head |
| Mean (SD) EQ-5D-5L utility score | 0.83 (0.17) | 0.88 (0.15) | 0.64 (0.24) | 0.68 (0.27) |
| Problems with mobility | 41.9% | 25.6% | 70.5% | 43.9% |
| Problems with self-care | 16.9% | 8.6% | 35.7% | 22.4% |
| Problems with usual activities | 46.9% | 29.7% | 85.0% | 72.3% |
| Pain/discomfort | 65.4% | 51.5% | 85.5% | 72.3% |
| Anxiety/depression | 15.7% | 16.5% | 53.7% | 48.5% |
| Mean (SD) EQ VAS score | 77.4 (15.8) | 79.2 (15.8) | 63.8 (17.2) | 63.1 (18.1) |
| 12 Months after Injury | ||||
| No PCS | PCS | |||
| Health-Related Quality of Life | Non-Head | Head | Non-Head | Head |
| Mean (SD) EQ-5D-5L utility score | 0.88 (0.15) | 0.91 (0.12) | 0.67 (0.25) | 0.72 (0.22) |
| Problems with mobility | 32.0% | 17.8% | 67.4% | 46.3% |
| Problems with self-care | 11.2% | 6.5% | 32.6% | 14.9% |
| Problems with usual activities | 31.3% | 24.9% | 75.3% | 64.2% |
| Pain/discomfort | 50.8% | 39.1% | 79.5% | 76.1% |
| Anxiety/depression | 12.5% | 14.8% | 55.3% | 53.7% |
| Mean (SD) EQ VAS score | 79.2(16.2) | 79.4 (16.5) | 63.6 (18.4) | 68.1 (15.0) |
References
- Polinder, S.; Cnossen, M.C.; Real, R.G.L.; Covic, A.; Gorbunova, A.; Voormolen, D.C.; Master, C.L.; Haagsma, J.A.; Diaz-Arrastia, R.; Von Steinbuechel, N. A Multidimensional Approach to Post-concussion Symptoms in Mild Traumatic Brain Injury. Front. Neurol. 2018, 9, 1113. [Google Scholar] [CrossRef]
- Maas, A.I.R.; Menon, D.K.; Adelson, P.D.; Andelic, N.; Bell, M.J.; Belli, A.; Bragge, P.; Brazinova, A.; Büki, A.; Chesnut, R.M.; et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017, 16, 987–1048. [Google Scholar] [CrossRef]
- Hiploylee, C.; Dufort, P.A.; Davis, H.S.; Wennberg, R.A.; Tartaglia, M.C.; Mikulis, D.; Hazrati, L.-N.; Tator, C.H. Longitudinal Study of Postconcussion Syndrome: Not Everyone Recovers. J. Neurotrauma 2017, 34, 1511–1523. [Google Scholar] [CrossRef] [PubMed]
- Ryan, L.M.; Warden, D.L. Post concussion syndrome. Int. Rev. Psychiatry 2003, 15, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Lagarde, E.; Salmi, L.-R.; Holm, L.W.; Contrand, B.; Masson, F.; Ribéreau-Gayon, R.; Laborey, M.; Cassidy, J.D. Association of Symptoms Following Mild Traumatic Brain Injury With Posttraumatic Stress Disorder vs Postconcussion Syndrome. JAMA Psychiatry 2014, 71, 1032–1040. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.A.; Kirsch, N.L.; Tan-Schriner, C.U.; Sen, A.; Frederiksen, S.; Harris, R.E.; Maixner, W.; Maio, R.F. Health status, not head injury, predicts concussion symptoms after minor injury. Am. J. Emerg. Med. 2009, 27, 182–190. [Google Scholar] [CrossRef]
- Dean, P.J.A.; O’Neill, D.; Sterr, A. Post-concussion syndrome: Prevalence after mild traumatic brain injury in comparison with a sample without head injury. Brain Inj. 2011, 26, 14–26. [Google Scholar] [CrossRef]
- Ponsford, J.; Cameron, P.; Fitzgerald, M.; Grant, M.; Mikocka-Walus, A. Long-Term Outcomes after Uncomplicated Mild Traumatic Brain Injury: A Comparison with Trauma Controls. J. Neurotrauma 2011, 28, 937–946. [Google Scholar] [CrossRef]
- Iverson, G.L.; Lange, R.T. Examination of “Postconcussion-Like” Symptoms in a Healthy Sample. Appl. Neuropsychol. 2003, 10, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chan, R.C.K.; Deng, Y. Examination of postconcussion-like symptoms in healthy university students: Relation-ships to subjective and objective neuropsychological function performance. Arch. Clin. Neuropsychol. 2006, 21, 339–347. [Google Scholar] [CrossRef]
- Voormolen, D.C.; Cnossen, M.C.; Polinder, S.; Gravesteijn, B.Y.; Von Steinbuechel, N.; Real, R.G.; Haagsma, J.A. Prevalence of post-concussion-like symptoms in the general population in Italy, The Netherlands and the United Kingdom. Brain Inj. 2019, 33, 1078–1086. [Google Scholar] [CrossRef]
- Cassidy, J.D.; Cancelliere, C.; Carroll, L.J.; Côté, P.; Hincapié, C.A.; Holm, L.W.; Hartvigsen, J.; Donovan, J.; Nygren-de Boussard, C.; Kristman, V.L. Systematic review of self-reported prognosis in adults after mild traumatic brain injury: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 2014, 95, S132–S151. [Google Scholar] [CrossRef] [PubMed]
- Stålnacke, B.-M. Community integration, social support and life satisfaction in relation to symptoms 3 years after mild traumatic brain injury. Brain Inj. 2007, 21, 933–942. [Google Scholar] [CrossRef]
- Emanuelson, I.; Andersson Holmkvist, E.; Björklund, R.; Stålhammar, D. Quality of life and post-concussion symptoms in adults after mild traumatic brain injury: A population-based study in western Sweden. Acta Neurol. Scand. 2003, 108, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Voormolen, D.C.; Polinder, S.; Von Steinbuechel, N.; Vos, P.E.; Cnossen, M.C.; Haagsma, J.A. The association between post-concussion symptoms and health-related quality of life in patients with mild traumatic brain injury. Injury 2019, 50, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Cancelliere, C.; Kristman, V.L.; Cassidy, J.D.; Hincapié, C.A.; Côté, P.; Boyle, E.; Carroll, L.J.; Stålnacke, B.-M.; Nygren-de Boussard, C.; Borg, J. Systematic review of return to work after mild traumatic brain injury: Results of the International Collabora-tion on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 2014, 95, S201–S209. [Google Scholar] [CrossRef]
- Chu, S.-Y.; Tsai, Y.-H.; Xiao, S.-H.; Huang, S.-J.; Yang, C.-C. Quality of return to work in patients with mild traumatic brain in-jury: A prospective investigation of associations among post-concussion symptoms, neuropsychological functions, working status and stability. Brain Inj. 2017, 31, 1674–1682. [Google Scholar] [CrossRef]
- Panneman, M.; Blatter, B. Letsel Informatie Systeem—Representatief voor alle SEH’s in Nederland; VeiligheidNL: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Lyons, R.A.; Polinder, S.; Larsen, C.F.; Mulder, S.; Meerding, W.J.; Toet, H.; Van Beeck, E.; the Eurocost Reference Group. Methodological issues in comparing injury incidence across countries. Int. J. Inj. Control. Saf. Promot. 2006, 13, 63–70. [Google Scholar] [CrossRef]
- UNESCO (United Nations Educational, Scientific and Cultural Organization). International Standard Classification of Education 2011. Available online: http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf (accessed on 24 November 2020).
- King, N.S.; Crawford, S.; Wenden, F.J.; Moss, N.E.G.; Wade, D.T. The Rivermead Post Concussion Symptoms Questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. J. Neurol. 1995, 242, 587–592. [Google Scholar] [CrossRef]
- Voormolen, D.C.; Cnossen, M.C.; Polinder, S.; Von Steinbuechel, N.; Vos, P.E.; Haagsma, J.A. Divergent Classification Methods of Post-Concussion Syndrome after Mild Traumatic Brain Injury: Prevalence Rates, Risk Factors, and Functional Outcome. J. Neurotrauma 2018, 35, 1233–1241. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.E.; Bonsel, G.J.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Versteegh, M.M.; Vermeulen, K.M.; Evers, S.M.A.A.; de Wit, G.A.; Prenger, R.; Stolk, E.A. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health 2016, 19, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Devlin, N.; Parkin, D.; Browne, J. Using the EQ-5D as a Performance Measurement Tool in the NHS. Available online: https://openaccess.city.ac.uk/id/eprint/1502/ (accessed on 11 December 2020).
- Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–68. [Google Scholar] [CrossRef]
- Smith-Seemiller, L.; Fow, N.R.; Kant, R.; Franzen, M.D. Presence of post-concussion syndrome symptoms in patients with chronic pain vs mild traumatic brain injury. Brain Inj. 2003, 17, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Ponsford, J.; Nguyen, S.; Downing, M.; Bosch, M.; McKenzie, J.E.; Turner, S.; Chau, M.; Mortimer, D.; Gruen, R.L.; Knott, J.; et al. Factors associated with persistent post-concussion symptoms following mild traumatic brain injury in adults. J. Rehabilitation Med. 2019, 51, 32–39. [Google Scholar] [CrossRef]
- Theadom, A.; Parag, V.; Dowell, T.; McPherson, K.; Starkey, N.; Barker-Collo, S.; Jones, K.; Ameratunga, S.; Feigin, V.L.; on behalf of the BIONIC Research Group. Persistent problems 1 year after mild traumatic brain injury: A longitudinal population study in New Zealand. Br. J. Gen. Pr. 2015, 66, e16–e23. [Google Scholar] [CrossRef] [PubMed]
- Zeldovich, M.; Wu, Y.-J.; Gorbunova, A.; Mikolic, A.; Polinder, S.; Plass, A.M.; Covic, A.; Asendorf, T.; Andelic, N.; Voormolen, D.C.; et al. Influence of Sociodemographic, Premorbid, and Injury-Related Factors on Post-Concussion Symptoms after Traumatic Brain Injury. J. Clin. Med. 2020, 9, 1931. [Google Scholar] [CrossRef]
- Silverberg, N.D.; Gardner, A.J.; Brubacher, J.R.; Panenka, W.J.; Li, J.J.; Iverson, G.L. Systematic review of multivariable prognostic models for mild traumatic brain injury. J. Neurotrauma 2015, 32, 517–526. [Google Scholar] [CrossRef]
- Cnossen, M.C.; Winkler, E.A.; Yue, J.K.; Okonkwo, D.O.; Valadka, A.B.; Steyerberg, E.W.; Lingsma, H.F.; Manley, G.T.; the TRACK-TBI Investigators. Development of a Prediction Model for Post-Concussive Symptoms following Mild Traumatic Brain Injury: A TRACK-TBI Pilot Study. J. Neurotrauma 2017, 34, 2396–2409. [Google Scholar] [CrossRef]
- King, N. Permanent post concussion symptoms after mild head injury: A systematic review of age and gender factors. Neurorehabilit. 2014, 34, 741–748. [Google Scholar] [CrossRef]
- Van der Naalt, J.; Timmerman, M.E.; de Koning, M.E.; van der Horn, H.J.; Scheenen, M.E.; Jacobs, B.; Hageman, G.; Yilmaz, T.; Roks, G.; Spikman, J.M. Early predictors of outcome after mild traumatic brain injury (UPFRONT): An observational cohort study. Lancet Neurol. 2017, 16, 532–540. [Google Scholar] [CrossRef]
- Iverson, G.L.; Brooks, B.L.; Ashton, V.L.; Lange, R.T. Interview Versus Questionnaire Symptom Reporting in People With the Postconcussion Syndrome. J. Head Trauma Rehabil. 2010, 25, 23–30. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993; Volume 2. [Google Scholar]
- Caplain, S.; Chenuc, G.; Blancho, S.; Marque, S.; Aghakhani, N. Efficacy of psychoeducation and cognitive re-habilitation after mild traumatic brain injury for preventing post-concussional syndrome in individuals with high risk of poor prognosis: A randomized clinical trial. Front. Neurol. 2019, 10, 929. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Group | Total (n = 1282) | No PCS (n = 1000) | PCS (n = 282) | Respondents (Weighted) a |
|---|---|---|---|---|---|
| Age in years, mean (SD) | 61.9 (15.7) | 61.5 (15.6) | 63.1 (16.1) | 60.9 (15.2) | |
| Sex, n | Male | 595 (46.4%) | 476 (47.6%) | 119 (42.2%) | 44.1% |
| Female | 687 (53.6%) | 524 (52.4%) | 163 (57.8%) | 55.9% | |
| Educational level, n b | Low | 506 (39.5%) | 371 (37.1%) | 135 (47.9%) | 38.7% |
| Middle | 338 (26.4%) | 270 (27.0%) | 68 (24.1%) | 31.8% | |
| High | 367 (28.6%) | 306 (30.6%) | 61 (21.6%) | 29.5% | |
| Living situation, n c | Alone | 317 (24.7%) | 239 (23.9%) | 78 (27.7%) | 29.3% |
| Not alone | 948 (73.9%) | 748 (74.8%) | 200 (70.9%) | 70.7% | |
| Injury mechanism, n | Home and leisure accident | 700 (54.6%) | 553 (55.3%) | 147 (52.1%) | 58.6% |
| Road traffic accident | 350 (27.3%) | 253 (25.3%) | 97 (34.4%) | 23.7% | |
| Sports accident | 155 (12.1%) | 137 (13.7%) | 18 (6.4%) | 10.6% | |
| Occupational accident | 77 (6.0%) | 57 (5.7%) | 20 (7.1%) | 7.1% | |
| Type of injury, n | Head injury | 236 (18.4%) | 169 (16.9%) | 67 (23.8%) | 13.0% |
| Other injuries | 1046 (81.6%) | 831 (83.1%) | 224 (76.2%) | 87.0% | |
| Chronic disease, n d | No chronic disease | 712 (55.5%) | 609 (60.9%) | 103 (36.5%) | 54.5% |
| 1 chronic disease | 350 (27.3%) | 251 (25.1%) | 99 (35.1%) | 25.5% | |
| 2 or more chronic diseases | 188 (14.7%) | 112 (11.2%) | 76 (27.0%) | 20.0% | |
| Post-concussion syndrome (PCS) | Yes | 282 (22.0%) | 19.3% | ||
| No | 1000 (78.0%) | 80.7% | |||
| RPQ total score | |||||
| mean (SD) | 4.9 (7.8) | 1.5 (2.7) | 17.0 (8.2) | 4.5 (7.6) | |
| median (IQR) | 0 (0–7) | 0 (0–2) | 15 (11–21) | 0 (0–6) |
| Characteristic | Group | Univariate | Multivariate | ||
|---|---|---|---|---|---|
| Odds ratio | 95% CI | Odds ratio | 95% CI | ||
| Age | 1.007 | 0.998; 1.016 | |||
| Sex | Male | Ref | |||
| Female | 1.244 | 0.953; 1.625 | |||
| Living situation | Not Alone | Ref | |||
| Alone | 1.219 | 0.903; 1.644 | |||
| Educational level | Low | Ref | Ref | ||
| Middle | 0.679 * | 0.490; 0.940 | 0.807 | 0.573; 1.136 | |
| High | 0.552 * | 0.391; 0.778 | 0.664 * | 0.462; 0.954 | |
| Injury mechanism | Home and leisure accident | Ref | Ref | ||
| Road traffic accident | 1.442 * | 1.072; 1.940 | 1.493 * | 1.079; 2.066 | |
| Sports accident | 0.494 * | 0.293; 0.835 | 0.747 | 0.430; 1.300 | |
| Occupational accident | 1.320 | 0.769; 2.267 | 1.570 | 0.884; 2.789 | |
| Number of injuries | 1 | Ref | |||
| 2 | 1.210 | 0.865; 1.692 | 1.013 | 0.703; 1.460 | |
| ≥3 | 1.555 * | 1.001; 2.415 | 1.174 | 0.707; 1.948 | |
| Type of injury | Other injuries | Ref | Ref | ||
| Head injury | 1.532 * | 1.112; 2.111 | 1.485 * | 1.023; 2.155 | |
| Chronic disease | No chronic disease | Ref | Ref | ||
| 1 chronic disease | 2.337 * | 1.710; 3.194 | 2.403 * | 1.739; 3.319 | |
| 2 or more chronic diseases | 3.932 * | 2.740; 5.642 | 4.126 * | 2.825; 6.026 | |
| Length of hospital stay | 1.066 * | 1.037; 1.095 | 1.058 | 1.029; 1.087 | |
| 6 Months after Injury | 12 Months after Injury | |||
|---|---|---|---|---|
| Health-Related Quality of Life | PCS | No PCS | PCS | No PCS |
| Mean (SD) EQ-5D-5L utility score | 0.65 (0.25) | 0.84 (0.17) | 0.68 (0.24) | 0.88 (0.15) |
| Problems with mobility | 64.1% | 39.2% | 62.4% | 29.6% |
| Problems with self-care | 32.5% | 15.5% | 28.4% | 10.4% |
| Problems with usual activities | 82.1% | 44.0% | 72.7% | 30.2% |
| Pain/discomfort | 82.4% | 63.1% | 78.7% | 48.8% |
| Anxiety/depression | 52.5% | 15.8% | 55.0% | 12.9% |
| Mean (SD) EQ VAS score | 63.7 (17.4) | 77.7 (15.8) | 64.7 (17.4) | 79.2 (16.2) |
| Weighted data a | ||||
| Mean (SD) EQ-5D-5L utility score | 0.67 (0.24) | 0.84 (0.17) | 0.70 (0.23) | 0.88 (0.23) |
| Problems with mobility | 59.2% | 36.8% | 60.2% | 29.5% |
| Problems with self-care | 29.1% | 18.7% | 22.5% | 14.8% |
| Problems with usual activities | 80.3% | 42.2% | 74.6% | 30.6% |
| Pain/discomfort | 84.2% | 63.3% | 77.7% | 46.4% |
| Anxiety/depression | 50.7% | 13.5% | 56.8% | 16.4% |
| Mean (SD) EQ VAS score | 65.9 (16.9) | 77.9 (15.7) | 66.3 (16.8) | 80.0 (16.8) |
| Paretian Classification of Health Change | Total | No PCS | PCS |
|---|---|---|---|
| No problems | 20.7% | 24.7% | 2.6% |
| No change | 8.9% | 10.5% | 7.0% |
| Improve | 42.1% | 41.9% | 43.0% |
| Worsen | 15.4% | 13.4% | 22.2% |
| Mixed change | 12.9% | 9.5% | 25.2% |
| Weighted data a | |||
| No problems | 23.5% | 28.5% | 2.3% |
| No change | 9.2% | 10.3% | 4.6% |
| Improve | 38.4% | 37.3% | 43.2% |
| Worsen | 12.8% | 10.3% | 23.3% |
| Mixed change | 16.1% | 13.6% | 26.6% |
| Service | Total Sample | No Chronic Disease | With Chronic Disease | ||||
|---|---|---|---|---|---|---|---|
| No PCS | PCS | No PCS | PCS | No PCS | PCS | ||
| Hospitalization | 47.0% | 56.7% | 45.2% | 53.4% | 48.5% | 58.3% | |
| Post-discharge health care utilization | |||||||
| Specialist | 62.4% | 73.8% | 61.2% | 76.7% | 63.4% | 72.6% | |
| Outpatient rehabilitation | 7.3% | 18.4% | 6.6% | 27.2% | 9.1% | 13.7% | |
| General practitioner | 32.1% | 60.6% | 30.9% | 63.1% | 34.7% | 60.0% | |
| Physiotherapist | 56.9% | 66.3% | 57.0% | 69.9% | 56.6% | 64.6% | |
| Psychologist | 4.5% | 20.2% | 4.4% | 28.2% | 5.0% | 16.0% | |
| Nursing care at home | 15.2% | 30.5% | 10.7% | 23.3% | 22.6% | 35.4% | |
| Weighted data a | |||||||
| Hospitalization | 26.7% | 29.4% | 20.2% | 24.8% | 35.0% | 31.1% | |
| Post-discharge health care utilization | |||||||
| Specialist | 57.9% | 71.5% | 62.0% | 78.3% | 51.4% | 67.2% | |
| Outpatient rehabilitation | 5.2% | 15.9% | 5.9% | 25.1% | 4.5% | 9.5% | |
| General practitioner | 29.5% | 62.0% | 27.7% | 66.1% | 31.8% | 59.9% | |
| Physiotherapist | 46.7% | 59.5% | 51.4% | 66.1% | 40.0% | 54.9% | |
| Psychologist | 4.6% | 19.6% | 3.6% | 26.9% | 6.2% | 14.6% | |
| Nursing care at home | 9.5% | 23.7% | 6.8% | 16.6% | 12.6% | 29.3% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Vlegel, M.; Polinder, S.; Toet, H.; Panneman, M.J.M.; Haagsma, J.A. Prevalence of Post-Concussion-Like Symptoms in the General Injury Population and the Association with Health-Related Quality of Life, Health Care Use, and Return to Work. J. Clin. Med. 2021, 10, 806. https://doi.org/10.3390/jcm10040806
van der Vlegel M, Polinder S, Toet H, Panneman MJM, Haagsma JA. Prevalence of Post-Concussion-Like Symptoms in the General Injury Population and the Association with Health-Related Quality of Life, Health Care Use, and Return to Work. Journal of Clinical Medicine. 2021; 10(4):806. https://doi.org/10.3390/jcm10040806
Chicago/Turabian Stylevan der Vlegel, Marjolein, Suzanne Polinder, Hidde Toet, Martien J.M. Panneman, and Juanita A. Haagsma. 2021. "Prevalence of Post-Concussion-Like Symptoms in the General Injury Population and the Association with Health-Related Quality of Life, Health Care Use, and Return to Work" Journal of Clinical Medicine 10, no. 4: 806. https://doi.org/10.3390/jcm10040806
APA Stylevan der Vlegel, M., Polinder, S., Toet, H., Panneman, M. J. M., & Haagsma, J. A. (2021). Prevalence of Post-Concussion-Like Symptoms in the General Injury Population and the Association with Health-Related Quality of Life, Health Care Use, and Return to Work. Journal of Clinical Medicine, 10(4), 806. https://doi.org/10.3390/jcm10040806






