Fetal Cardiac Interventions—Are They Safe for the Mothers?
Abstract
:1. Introduction
2. Materials and Methods
2.1. General Study Design
2.2. Patients/Study Population
2.3. Management
2.4. Anesthesia
2.5. Cordocentesis and Cardiac Puncture
2.6. Transplacental Fetal Treatment
2.7. Data Collection
2.8. Statistical Analysis
3. Results
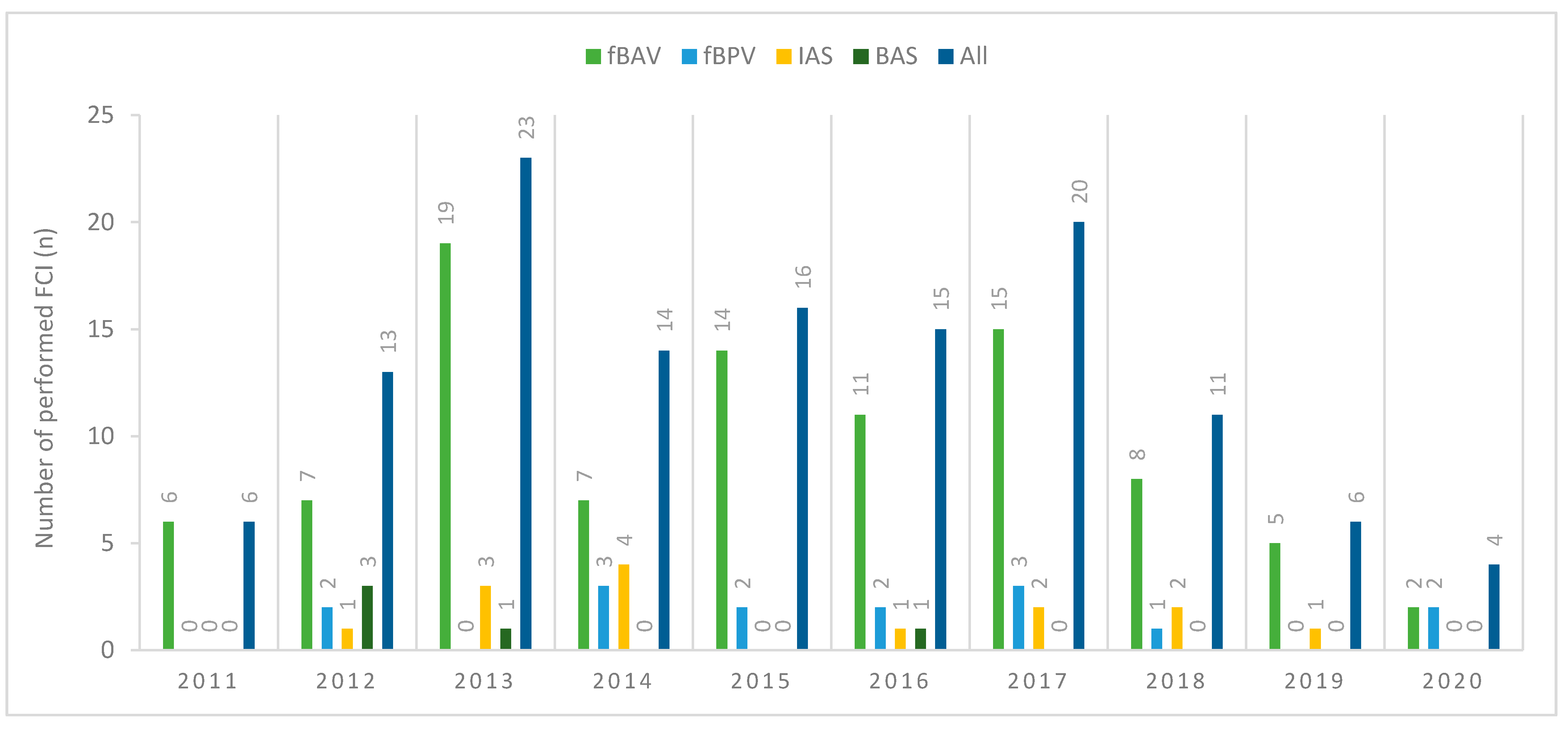
3.1. Number and Types of FCI
3.2. Characteristics of the Patients
3.3. Technical Aspects of FCI
3.4. Threatened Premature Labor
3.5. pPROM
3.6. Postoperative Events
3.7. Digoxin Transplacental Therapy
3.8. Pregnancy Outcomes
3.8.1. All Patients
3.8.2. Patients Who Underwent More than One FCI
4. Discussion
4.1. Anesthesia
4.2. Approach
4.3. Uterine Punctures
4.4. Digoxin
4.5. The Course of Pregnancy and Delivery
4.6. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arzt, W.; Wertaschnigg, D.; Veit, I.; Klement, F.; Gitter, R.; Tulzer, G. Intrauterine aortic valvuloplasty in fetuses with critical aortic stenosis: Experience and results of 24 procedures. Ultrasound Obstet. Gynecol. 2011, 37, 689–695. [Google Scholar] [CrossRef]
- McElhinney, D.B.; Marshall, A.C.; Wilkins-Haug, L.E.; Brown, D.W.; Benson, C.B.; Silva, V.; Marx, G.R.; Mizrahi-Arnaud, A.; Lock, J.E.; Tworetzky, W. Predictors of technical success and postnatal biventricular outcome after in utero aortic valvuloplasty for aortic stenosis with evolving hypoplastic left heart syndrome. Circulation 2009, 120, 1482–1490. [Google Scholar] [CrossRef] [PubMed]
- Tworetzky, W.; McElhinney, D.B.; Marx, G.R.; Benson, C.B.; Brusseau, R.; Morash, D.; Wilkins-Haug, L.E.; Lock, J.E.; Marshall, A.C. In utero valvuloplasty for pulmonary atresia with hypoplastic right ventricle: Techniques and outcomes. Pediatrics 2009, 124, e510–e518. [Google Scholar] [CrossRef] [Green Version]
- Wilkins-Haug, L.E.; Tworetzky, W.; Benson, C.B.; Marshall, A.C.; Jennings, R.W.; Lock, J.E. Factors affecting technical success of fetal aortic valve dilation. Ultrasound Obstet. Gynecol. 2006, 28, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Marshall, A.C.; van der Velde, M.E.; Tworetzky, W.; Gomez, C.A.; Wilkins-Haug, L.; Benson, C.B.; Jennings, R.W.; Lock, J.E. Creation of an Atrial Septal Defect In Utero for Fetuses With Hypoplastic Left Heart Syndrome and Intact or Highly Restrictive Atrial Septum. Circulation 2004, 110, 253–258. [Google Scholar] [CrossRef]
- Arzt, W.; Tulzer, G. Fetal surgery for cardiac lesions. Prenat Diagn 2011, 31, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Galindo, A.; Gómez-Montes, E.; Gómez, O.; Bennasar, M.; Crispi, F.; Herraiz, I.; Mendoza, A.; Escribano, D.; García-Torres, E.; Carretero, J.M.; et al. Fetal Aortic Valvuloplasty: Experience and Results of Two Tertiary Centers in Spain. Fetal Diagn Ther. 2017, 42, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Crucean, A.; Alqahtani, A.; Barron, D.J.; Brawn, W.J.; Richardson, R.V.; O’Sullivan, J.; Anderson, R.H.; Henderson, D.J.; Chaudhry, B. Re-evaluation of hypoplastic left heart syndrome from a developmental and morphological perspective. Orphanet J. Rare Dis. 2017, 12, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jantzen, D.W.; Moon-Grady, A.J.; Morris, S.A.; Armstrong, A.K.; Berg, C.; Dangel, J.; Fifer, C.G.; Frommelt, M.; Gembruch, U.; Herberg, U. Hypoplastic Left Heart Syndrome With Intact or Restrictive Atrial Septum: A Report From the International Fetal Cardiac Intervention Registry. Circulation 2017, 136, 1346–1349. [Google Scholar] [CrossRef] [PubMed]
- Lowenthal, A.; Kipps, A.K.; Brook, M.M.; Meadows, J.; Azakie, A.; Moon-Grady, A.J. Prenatal diagnosis of atrial restriction in hypoplastic left heart syndrome is associated with decreased 2-year survival. Prenat Diagn. 2012, 32, 485–490. [Google Scholar] [CrossRef]
- Vida, V.L.; Bacha, E.A.; Larrazabal, A.; Gauvreau, K.; Thiagaragan, R.; Fynn-Thompson, F.; Pigula, F.A.; Mayer, J.E.; Del Nido, P.J.; Tworetzky, W.; et al. Hypoplastic left heart syndrome with intact or highly restrictive atrial septum: Surgical experience from a single center. Ann Thorac. Surg. 2007, 84, 581–585. [Google Scholar] [CrossRef]
- Glatz, J.A.; Tabbutt, S.; Gaynor, J.W.; Rome, J.J.; Montenegro, L.; Spray, T.L.; Rychik, J. Hypoplastic left heart syndrome with atrial level restriction in the era of prenatal diagnosis. Ann. Thorac. Surg. 2007, 84, 1633–1638. [Google Scholar] [CrossRef] [PubMed]
- Hogan, W.J.; Grinenco, S.; Armstrong, A.; Devlieger, R.; Dangel, J.; Ferrer, Q.; Frommelt, M.; Galindo, A.; Gardiner, H.; Gelehrter, S.; et al. Fetal Cardiac Intervention for Pulmonary Atresia with Intact Ventricular Septum: International Fetal Cardiac Intervention Registry. FDT 2020, 47, 731–739. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.-M. Fetal cardiac interventions: An update of therapeutic options. Rev. Bras. Cir. Cardiovasc. 2014. [Google Scholar] [CrossRef] [Green Version]
- Debska, M.; Kolesnik, A.; Rebizant, B.; Sekowska, A.; Grzyb, A.; Chaberek, K.; Witwicki, J.; Debski, R.; Dangel, J. Fetal Cardiac Interventions-Polish Experience from “Zero” to the Third World Largest Program. J. Clin. Med. 2020, 9, 2888. [Google Scholar] [CrossRef]
- Kovacevic, A.; Öhman, A.; Tulzer, G.; Herberg, U.; Dangel, J.; Carvalho, J.S.; Fesslova, V.; Jicinska, H.; Sarkola, T.; Pedroza, C.; et al. Fetal hemodynamic response to aortic valvuloplasty and postnatal outcome: A European multicenter study. Ultrasound Obstet. Gynecol. 2018, 52, 221–229. [Google Scholar] [CrossRef] [PubMed]
- McElhinney, D.B.; Tworetzky, W.; Lock, J.E. Current Status of Fetal Cardiac Intervention. Circulation 2010, 121, 1256–1263. [Google Scholar] [CrossRef] [Green Version]
- Makikallio, K.; Levine, J.C.; Marx, G.R.; Colan, S.D.; Marshall, A.C.; Lock, J.E.; Tworetzky, W. Fetal aortic valve stenosis and the evolution of hypoplastic left heart syndrome: Patient selection for fetal intervention. Circulation 2006, 113, 1401–1405. [Google Scholar] [CrossRef] [Green Version]
- Manchikanti, L.; Colliver, J.A.; Marrero, T.C.; Roush, J.R. Ranitidine and metoclopramide for prophylaxis of aspiration pneumonitis in elective surgery. Anesth Analg. 1984, 63, 903–910. [Google Scholar] [CrossRef]
- Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016, 124, 270–300. [CrossRef] [PubMed]
- Hoagland, M.A.; Chatterjee, D. Anesthesia for fetal surgery. Paediatr. Anaesth. 2017, 27, 346–357. [Google Scholar] [CrossRef]
- Van de Velde, M.; De Buck, F. Fetal and maternal analgesia/anesthesia for fetal procedures. Fetal Diagn 2012, 31, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.M. Anesthesia for fetal surgery. Semin Fetal Neonatal Med. 2010, 15, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Dębska, M.; Szymkiewicz-Dangel, J.; Koleśnik, A.; Kretowicz, P.; Rebizant, B.; Witwicki, J.; Dębski, R. Fetal cardiac interventions—Are we ready for them? Ginekol. Pol. 2015, 86, 280–286. [Google Scholar] [CrossRef]
- Tita, A.T.N.; Andrews, W.W. Diagnosis and management of clinical chorioamnionitis. Clin. Perinatol. 2010, 37, 339–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayhew, D.; Mendonca, V.; Murthy, B.V.S. A review of ASA physical status—Historical perspectives and modern developments. Anaesthesia 2019, 74, 373–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansmann, M.; Gembruch, U.; Bald, R.; Manz, M.; Redel, D.A. Fetal tachyarrhythmias: Transplacental and direct treatment of the fetus—A report of 60 cases. Ultrasound Obstet. Gynecol. 1991, 1, 162–170. [Google Scholar] [CrossRef]
- Saxena, K.N. Anaesthesia for Fetal Surgeries. Indian J. Anaesth. 2009, 53, 554–559. [Google Scholar]
- Wohlmuth, C.; Tulzer, G.; Arzt, W.; Gitter, R.; Wertaschnigg, D. Maternal aspects of fetal cardiac intervention. Ultrasound Obstet. Gynecol. 2014, 44, 532–537. [Google Scholar] [CrossRef]
- Tworetzky, W.; Wilkins-Haug, L.; Jennings, R.W.; van der Velde, M.E.; Marshall, A.C.; Marx, G.R.; Colan, S.D.; Benson, C.B.; Lock, J.E.; Perry, S.B. Balloon dilation of severe aortic stenosis in the fetus: Potential for prevention of hypoplastic left heart syndrome: Candidate selection, technique, and results of successful intervention. Circulation 2004, 110, 2125–2131. [Google Scholar] [CrossRef] [Green Version]
- Mushambi, M.C.; Kinsella, S.M.; Popat, M.; Swales, H.; Ramaswamy, K.K.; Winton, A.L.; Quinn, A.C. Obstetric Anaesthetists’ Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia 2015, 70, 1286–1306. [Google Scholar] [CrossRef]
- Biro, P. Difficult intubation in pregnancy. Curr. Opin. Anaesthesiol. 2011, 24, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Reitman, E.; Flood, P. Anaesthetic considerations for non-obstetric surgery during pregnancy. Br. J. Anaesth. 2011, 107 (Suppl. 1), i72–i78. [Google Scholar] [CrossRef] [Green Version]
- Djabatey, E.A.; Barclay, P.M. Difficult and failed intubation in 3430 obstetric general anaesthetics. Anaesthesia 2009, 64, 1168–1171. [Google Scholar] [CrossRef] [PubMed]
- Nejdlova, M.; Johnson, T. Anaesthesia for non-obstetric procedures during pregnancy. Contin. Educ. Anaesth. Crit. Care Pain. 2012, 12, 203–206. [Google Scholar] [CrossRef] [Green Version]
- Kuczkowski, K.M. The safety of anaesthetics in pregnant women. Expert Opin. Drug Saf. 2006, 5, 251–264. [Google Scholar] [CrossRef]
- Gardiner, H.M. In utero intervention for severe congenital heart disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2019, 58, 42–54. [Google Scholar] [CrossRef]
- Gómez Montes, E.; Herraiz, I.; Mendoza, A.; Galindo, A. Fetal Intervention in Right Outflow Tract Obstructive Disease: Selection of Candidates and Results. Cardiol. Res. Pract. 2012, 2012, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuan, S.-M.; Humuruola, G. Fetal cardiac interventions: Clinical and experimental research. Postepy Kardiol. Interwencyjnej. 2016, 12, 99–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marshall, A.C.; Tworetzky, W.; Bergersen, L.; McElhinney, D.B.; Benson, C.B.; Jennings, R.W.; Wilkins-Haug, L.E.; Marx, G.R.; Lock, J.E. Aortic valvuloplasty in the fetus: Technical characteristics of successful balloon dilation. J. Pediatr. 2005, 147, 535–539. [Google Scholar] [CrossRef]
- Merz, W.; Tchatcheva, K.; Gembruch, U.; Kohl, T. Maternal complications of fetoscopic laser photocoagulation (FLP) for treatment of twin-twin transfusion syndrome (TTTS). J. Perinat. Med. 2010, 38, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Moldenhauer, J.S.; Soni, S.; Rintoul, N.E.; Spinner, S.S.; Khalek, N.; Martinez-Poyer, J.; Flake, A.W.; Hedrick, H.L.; Peranteau, W.H.; Rendon, N.; et al. Fetal Myelomeningocele Repair: The Post-MOMS Experience at the Children’s Hospital of Philadelphia. FDT 2015, 37, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Belfort, M.A. Predicting premature preterm rupture of the membranes after fetal surgery. BJOG Int. J. Obstet. Gynaecol. 2018, 125, 1293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strzelecka, I.; Respondek-Liberska, M.; Słodki, M.; Zych-Krekora, K.; Cuneo, B. Transplacental digoxin treatment in prenatal cardiac problems in singleton pregnancies—Meta analysis (based on literature: 1992–2015). Prenat. Cardiol. 2019, 2016, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Bravo-Valenzuela, N.J.; Rocha, L.A.; Machado Nardozza, L.M.; Júnior, E.A. Fetal cardiac arrhythmias: Current evidence. Ann. Pediatr. Cardiol. 2018, 11, 148–163. [Google Scholar] [PubMed]
- Rebizant, B.; Chaberek, K.; Kolesnik, A.; Czapska, A.; Dangel, J.; Debska, M. VP14.15: Transplacental treatment: Digoxin levels in the mother and the fetus. Ultrasound Obstet. Gynecol. 2020, 56, 111–112. [Google Scholar] [CrossRef]
| Characteristic | fBAV (n = 88) | fBPV (n = 13) | IAS (n = 14) | BAS (n = 5) | All (n = 113) | p-Value |
|---|---|---|---|---|---|---|
| Maternal age at FCI (years) | 30 (18–41) | 33 (26–39) | 29 (22–35) | 27 (25–34) | 30 (18–41) | 0.070 |
| BMI (kg/m2) | 24.7 (17.8–38.7) | 24.1 (19.3–29.7) | 24.4 (18.8–30.1) | 24.6 (20.8–28.1) | 24.6 (17.8–38.7) | 0.650 |
| Obesity (BMI > 30 kg/m2) | 14 (15.9%) | 0 (0%) | 1 (7.1%) | 0 (0%) | 15 (13.3%) | 0.279 |
| Gravidity | 2 (1–5) | 2 (1–5) | 2 (1–3) | 2 (2–5) | 2 (1–5) | 0.433 |
| Parity | 1 (0–3) | 0 (0–2) | 1 (0–2) | 2 (1–2) | 1 (0–3) | 0.091 |
| Active smoker | 4 (4.5%) | 0 (0%) | 0 (0%) | 0 (0%) | 4 (3.5%) | 0.684 |
| Paternal age (years) | 32 (20–46) | 34 (26–54) | 32 (24–36) | 34 (26–39) | 32 (20–54) | 0.702 |
| Family history of CHD | 8 (9.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 8 (7.1%) | 0.378 |
| ASA physical status | ASA 2–100% | ASA 2–100% | ASA 2–100% | ASA 2–100% | ASA 2–100% | 1.000 |
| fBAV (n = 94) | fBPV (n = 15) | IAS (n = 14) | BAS (n = 5) | Total (n = 128) | p-Value | |
|---|---|---|---|---|---|---|
| Total number of uterus punctures (cordocentesis, cardiac puncture, decompression of tamponade, drug administration) | 3 (2–5) | 3 (2–11) | 3 (2–8) | 3 (2–4) | 3 (2–11) | 0.103 |
| Tocolysis | 2 (2.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (1.6%) | 0.866 |
| Procedure-related pPROM & | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Procedure-related placental abruption $ | 1 (1.1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.8%) | 0.948 |
| Postoperative nausea and vomiting | 2 (2.1%) | 0 (0%) | 0 (0%) | 1 (20%) | 3 (2.3%) | 0.058 |
| Postoperative pain | 3 (3.2%) # | 3 (20%) # | 1 (7.1%) | 1 (20%) | 8 (6.3%) | 0.048 |
| Bleeding requiring blood transfusion | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Chorioamnionitis | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Wound infection | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Post-FCI hospitalization (days) | 4 (1–84) | 5 (1–7) | 5 (2–70) | 3 (2–19) | 4 (1–84) | 0.412 |
| Intensive care unit admission | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| Intra-/perioperative maternal mortality | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1.000 |
| fBAV | fBPV | IAS | BAS | Total | p-Value | |
|---|---|---|---|---|---|---|
| Number of procedures/number of fetuses | 94/88 | 15/13 | 14/14 | 5/5 | 128/113 | NA |
| Gestational age at FCI (weeks) | 25 (20–32) | 24 (22–30) | 27 (22–33) | 24 (22–29) | 25 (20–33) | 0.407 |
| Procedure-related death of the fetus/neonate † | 7 | 1 | 2 | 1 | 10 | 0.655 |
| Procedure non-related death of the fetus | 3 | 0 | 0 | 0 | 3 | 0.776 |
| Live birth | 78 | 12 | 12 | 4 | 100 | 0.889 |
| Gestational age at birth (weeks) | 39 (29–41) § | 38 (33–40) | 37 (29–41) | 33.5 (29–39) § | 39 (29–41) | 0.041 |
| Mode of delivery VD/CS | 42/36 54%/46% | 6/6 50%/50% | 7/5 58%/42% | 3/1 75%/25% | 54/46 54%/46% | 0.837 |
| Time interval between intervention and birth (days) | 92 (17–162) | 100 (46–117) | 75 (11–109) | 57.5 (17–114) | 92 (11–162) | 0.025 |
| Birth weight (g) | 3330 (950–4950) # | 3130 (2100–3920) ^ | 3130 (1770–4090) | 2640 (1800–2860) #,^ | 3320 (950–4950) | 0.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rebizant, B.; Koleśnik, A.; Grzyb, A.; Chaberek, K.; Sękowska, A.; Witwicki, J.; Szymkiewicz-Dangel, J.; Dębska, M. Fetal Cardiac Interventions—Are They Safe for the Mothers? J. Clin. Med. 2021, 10, 851. https://doi.org/10.3390/jcm10040851
Rebizant B, Koleśnik A, Grzyb A, Chaberek K, Sękowska A, Witwicki J, Szymkiewicz-Dangel J, Dębska M. Fetal Cardiac Interventions—Are They Safe for the Mothers? Journal of Clinical Medicine. 2021; 10(4):851. https://doi.org/10.3390/jcm10040851
Chicago/Turabian StyleRebizant, Beata, Adam Koleśnik, Agnieszka Grzyb, Katarzyna Chaberek, Agnieszka Sękowska, Jacek Witwicki, Joanna Szymkiewicz-Dangel, and Marzena Dębska. 2021. "Fetal Cardiac Interventions—Are They Safe for the Mothers?" Journal of Clinical Medicine 10, no. 4: 851. https://doi.org/10.3390/jcm10040851







