Adult Spinal Cord Injury without Major Bone Injury: Effects of Surgical Decompression and Predictors of Neurological Outcomes in American Spinal Injury Association Impairment Scale A, B, or C
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Preoperative Physical Examination and Imaging Examination
2.3. Steroid Protocol
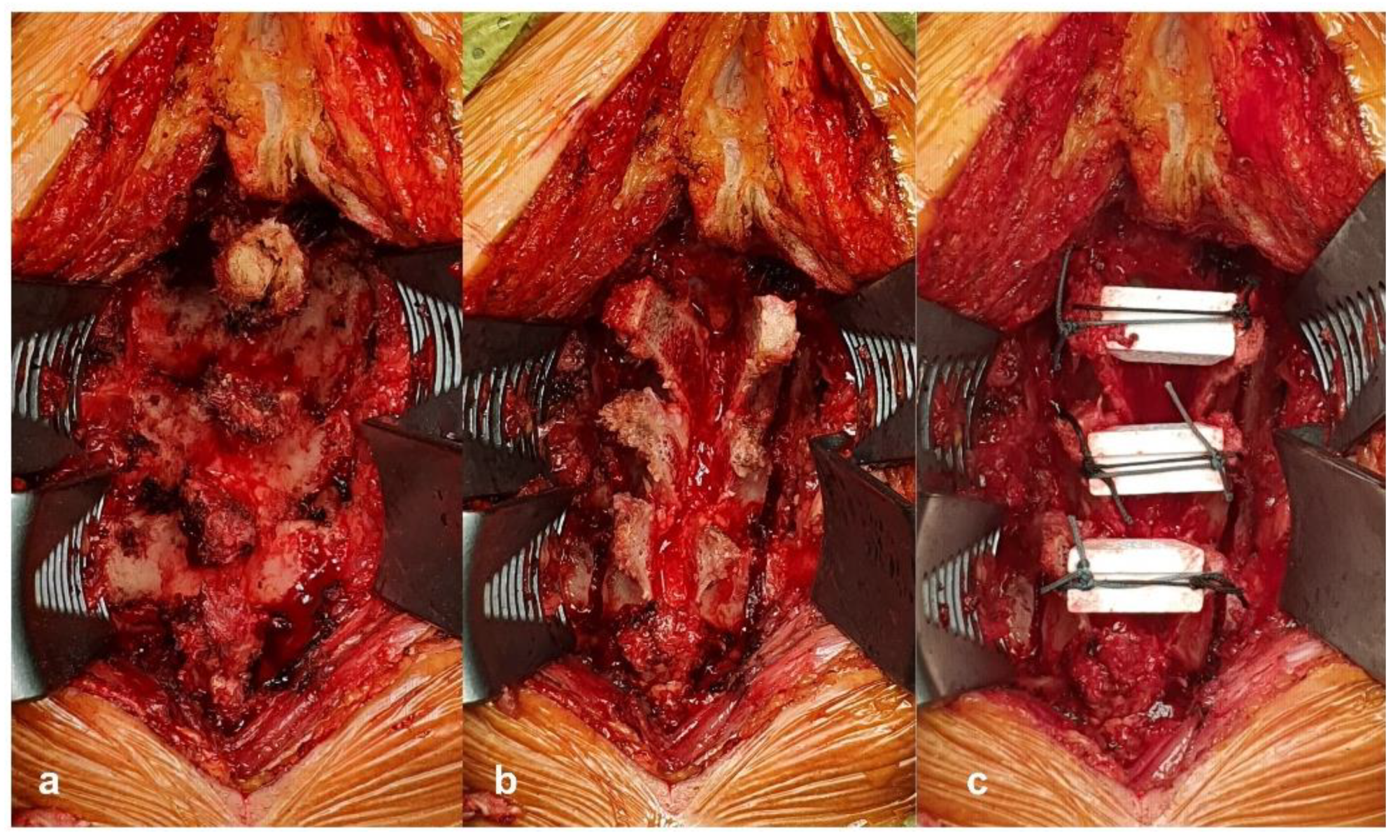
2.4. Surgical Procedure
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Wyndaele, M.; Wyndaele, J.J. Incidence, prevalence and epidemiology of spinal cord injury: What learns a worldwide literature survey? Spinal Cord 2006, 44, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Maeda, T.; Ueta, T.; Mori, E.; Yugue, I.; Kawano, O.; Takao, T.; Sakai, H.; Okada, S.; Shiba, K. Soft-Tissue Damage and Segmental Instability in Adult Patients With Cervical Spinal Cord Injury Without Major Bone Injury. Spine 2012, 37, E1560–E1566. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Takahashi, A.; Kitade, I.; Watanabe, S.; Honjoh, K.; Matsumine, A. Prognostic factors and optimal management for patients with cervical spinal cord injury without major bone injury. J. Orthop. Sci. 2019, 24, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Ter Wengel, P.V.; De Witt Hamer, P.C.; Pauptit, J.C.; Van Der Gaag, N.A.; Oner, F.C.; Vandertop, W.P. Early Surgical Decompression Improves Neurological Outcome after Complete Traumatic Cervical Spinal Cord Injury: A Meta-Analysis. J. Neurotrauma 2019, 36, 835–844. [Google Scholar] [CrossRef] [PubMed]
- Van Middendorp, J.J.; Hosman, A.J.; Doi, S.A. The Effects of the Timing of Spinal Surgery after Traumatic Spinal Cord Injury: A Systematic Review and Meta-Analysis. J. Neurotrauma 2013, 30, 1781–1794. [Google Scholar] [CrossRef] [PubMed]
- ASIA and ISCoS International Standards Committee; Betz, R.; Biering-Sørensen, F. The 2019 revision of the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI)—What’s new? Spinal Cord 2019, 57, 815–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kulkarni, M.V.; Bondurant, F.J.; Rose, S.L.; Narayana, P.A. 1.5 Tesla Magnetic Resonance Imaging of Acute Spinal Trauma. Radiographics 1988, 8, 1059–1082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawano, O.; Ueta, T.; Shiba, K.; Iwamoto, Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: A multicenter prospective study. Spinal Cord 2010, 48, 548–553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarabi, B.; Simard, J.M.; Kufera, J.A.; Alexander, M.; Zacherl, K.M.; Mirvis, S.E.; Shanmuganathan, K.; Schwartzbauer, G.; Maulucci, C.M.; Slavin, J.; et al. Intramedullary lesion expansion on magnetic resonance imaging in patients with motor complete cervical spinal cord injury. J. Neurosurg. Spine 2012, 17, 243–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, T.-Y.; Dickman, C.A.; Eleraky, M.; Sonntag, V.K. The Role of Decompression for Acute Incomplete Cervical Spinal Cord Injury in Cervical Spondylosis. Spine 1998, 23, 2398–2403. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Mizuno, J.; Nakagawa, H.; Inoue, T. Surgery for acute subaxial traumatic central cord syndrome without fracture or dislocation. J. Clin. Neurosci. 2005, 12, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Park, Y.-J.; Song, S.-Y.; Hwang, S.-C.; Kim, K.-T.; Kim, D.-H. The Importance of Early Surgical Decompression for Acute Traumatic Spinal Cord Injury. Clin. Orthop. Surg. 2018, 10, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Pollard, M.E.; Apple, D.F. Factors Associated with Improved Neurologic Outcomes in Patients with Incomplete Tetraplegia. Spine 2003, 28, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, J.W.; Curt, A.; Steeves, J.D.; Coleman, W.P.; Tuszynski, M.H.; Lammertse, D.; Bartlett, P.F.; Blight, A.R.; Dietz, V.; Ditunno, J.; et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: Spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007, 45, 190–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarabi, B.; Sansur, C.A.; Ibrahimi, D.M.; Simard, J.M.; Hersh, D.S.; Le, E.; Diaz, C.; Massetti, J.; Akhtar-Danesh, N. Intramedullary Lesion Length on Postoperative Magnetic Resonance Imaging is a Strong Predictor of ASIA Impairment Scale Grade Conversion Following Decompressive Surgery in Cervical Spinal Cord Injury. Neurosurgery 2017, 80, 610–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuzuki, N.; Zhogshi, L.; Abe, R.; Saiki, K. Paralysis of the arm after posterior decompression of the cervical spinal cord. I. Anatomical investigation of the mechanism of paralysis. Eur. Spine J. 1993, 2, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Hirabayashi, S. Recent Surgical Methods of Double-door Laminoplasty of the Cervical Spine (Kurokawa’s Method). Spine Surg. Relat. Res. 2018, 2, 154–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bozzo, A.; Marcoux, J.; Radhakrishna, M.; Pelletier, J.; Goulet, B. The Role of Magnetic Resonance Imaging in the Management of Acute Spinal Cord Injury. J. Neurotrauma 2011, 28, 1401–1411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramón, S.; Domínguez, R.; Ramírez, L.; Paraira, M.; Olona, M.; Castelló, T.; García Fernández, L. Clinical and magnetic resonance imaging correlation in acute spinal cord injury. Spinal Cord 1997, 35, 664–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarabi, B.; Alexander, M.; Mirvis, S.E.; Shanmuganathan, K.; Chesler, D.; Maulucci, C.; Iguchi, M.; Aresco, C.; Blacklock, T. Predictors of outcome in acute traumatic central cord syndrome due to spinal stenosis. J. Neurosurg. Spine 2011, 14, 122–130. [Google Scholar] [CrossRef] [PubMed]

| Cases | Sex/Age | Injury Mechanism | Degeneration (CS or OPLL) | Time from Injury to Surgery (h) | MRI Type | Compression Rate | Intramedullary Lesion Length | Operation Level | AIS Grade |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 65/male | Car accident | CS | <72 | hemorrhage | 34.6% | 50 mm | C4-7 | A->A |
| 2 | 68/male | Fall down | OPLL | <24 | edema | 16.8% | 42 mm | C3-5 | B->C |
| 3 | 50/male | Car accident | - | <48 | hemorrhage | 10.5% | 59 mm | C4-7 | B->B |
| 4 | 79/male | Fall down | CS | <24 | edema | 18.5% | 55 mm | C3-6 | C->D |
| 5 | 69/male | Fall down | OPLL | <24 | hemorrhage | 35.2% | 62 mm | C4-6 | A->A |
| 6 | 81/male | Fall down | CS | <12 | edema | 27.8% | 41 mm | C4-6 | C->C |
| 7 | 50/male | Fall down | CS | <24 | hemorrhage | 23.9% | 71 mm | C4-6 | A->A |
| 8 | 55/male | Car accident | CS | <12 | edema | 32.9% | 66 mm | C3-6 | A->A |
| 9 | 57/male | Car accident | CS | <12 | hemorrhage | 19.8% | 42 mm | C3-5 | A->B |
| 10 | 62/male | Fall down | - | <12 | edema | 9.4% | 20 mm | C3-4 | A->C |
| 11 | 66/male | Fall down | CS | <72 | edema | 13.2% | 44 mm | C4-5 | A->C |
| Preoperative AIS Grade | 1-Year Follow-up AIS Grade | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| A (n = 7) | 4 | 1 | 2 | 0 | 0 |
| B (n = 2) | 0 | 1 | 1 | 0 | 0 |
| C (n = 2) | 0 | 0 | 1 | 1 | 0 |
| Category | AIS Not Converted (n = 6) | AIS Converted (n = 5) | p Value |
|---|---|---|---|
| Age | 61.7 ± 12.3 | 66.4 ± 8.2 | 0.464 |
| Admission AIS grade | 1.000 | ||
| A | 4 | 3 | |
| B | 1 | 1 | |
| C | 1 | 1 | |
| Admission AMS | 21.0 ± 9.4 | 13.4 ± 14.9 | 0.359 |
| Admission ASS | 56.8 ± 22.9 | 85.6 ± 86.2 | 0.854 |
| Time from injury to surgery | 1.000 | ||
| <12 h | 2 | 2 | |
| 12–24 h | 2 | 2 | |
| >24 h | 2 | 1 | |
| MRI type | 0.242 | ||
| Edema | 2 | 4 | |
| Hemorrhage | 4 | 1 | |
| Compression rate (%) | 27.4 ± 9.4 | 15.5 ± 4.0 | 0.045 * |
| IMLL (mm) | 58.2 ± 11.0 | 40.6 ± 12.7 | 0.047 * |
| AIS Score | Preoperative | 1-Year Follow-up | p Value |
|---|---|---|---|
| AMS | 17.5 ± 12.2 | 30.6 ± 19.3 | 0.005 * |
| ASS | 69.9 ± 58.8 | 117.0 ± 62.7 | 0.007 * |
| Preoperative | 1-Year Follow-up | p Value | |
|---|---|---|---|
| Edema | |||
| AMS | 18.7 ± 12.4 | 38.8 ± 17.8 | 0.028 * |
| ASS | 69.9 ± 58.8 | 117.0 ± 62.7 | 0.052 |
| Hemorrhage | |||
| AMS | 16.2 ± 13.2 | 20.8 ± 17.7 | 0.090 |
| ASS | 40.0 ± 15.0 | 73.6 ± 31.1 | 0.057 |
| Compression rate ≤ 20% | |||
| AMS | 14.8 ± 13.8 | 35.8 ± 22.8 | 0.035 * |
| ASS | 78.0 ± 79.3 | 131.0 ± 58.6 | 0.035 * |
| Compression rate > 20% | |||
| AMS | 20.8 ± 10.5 | 24.4 ± 13.8 | 0.057 |
| ASS | 60.2 ± 23.8 | 100.2 ± 69.9 | 0.090 |
| IMLL ≤ 50 mm | |||
| AMS | 14.8 ± 13.2 | 34.3 ± 22.8 | 0.035 * |
| ASS | 59.3 ± 37.2 | 134.3 ± 53.0 | 0.035 * |
| IMLL > 50 mm | |||
| AMS | 20.8 ± 11.3 | 26.2 ± 15.2 | 0.057 |
| ASS | 82.6 ± 81.0 | 96.2 ± 73.0 | 0.090 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Na, B.-R.; Seo, H.-Y. Adult Spinal Cord Injury without Major Bone Injury: Effects of Surgical Decompression and Predictors of Neurological Outcomes in American Spinal Injury Association Impairment Scale A, B, or C. J. Clin. Med. 2021, 10, 1106. https://doi.org/10.3390/jcm10051106
Na B-R, Seo H-Y. Adult Spinal Cord Injury without Major Bone Injury: Effects of Surgical Decompression and Predictors of Neurological Outcomes in American Spinal Injury Association Impairment Scale A, B, or C. Journal of Clinical Medicine. 2021; 10(5):1106. https://doi.org/10.3390/jcm10051106
Chicago/Turabian StyleNa, Bo-Ram, and Hyoung-Yeon Seo. 2021. "Adult Spinal Cord Injury without Major Bone Injury: Effects of Surgical Decompression and Predictors of Neurological Outcomes in American Spinal Injury Association Impairment Scale A, B, or C" Journal of Clinical Medicine 10, no. 5: 1106. https://doi.org/10.3390/jcm10051106
APA StyleNa, B. -R., & Seo, H. -Y. (2021). Adult Spinal Cord Injury without Major Bone Injury: Effects of Surgical Decompression and Predictors of Neurological Outcomes in American Spinal Injury Association Impairment Scale A, B, or C. Journal of Clinical Medicine, 10(5), 1106. https://doi.org/10.3390/jcm10051106






