Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. | Able to breathe easy |
| 2. | Been able to enjoy food |
| 3. | Feeling rested |
| 4. | Have had a good sleep |
| 5. | Able to look after personal toilet and hygiene unaided |
| 6. | Able to communicate with family or friends |
| 7. | Getting support from hospital doctors and nurse |
| 8. | Able to return to work or usual home activities |
| 9. | Feeling comfortable and in control |
| 10. | Having a feeling of general well-being |
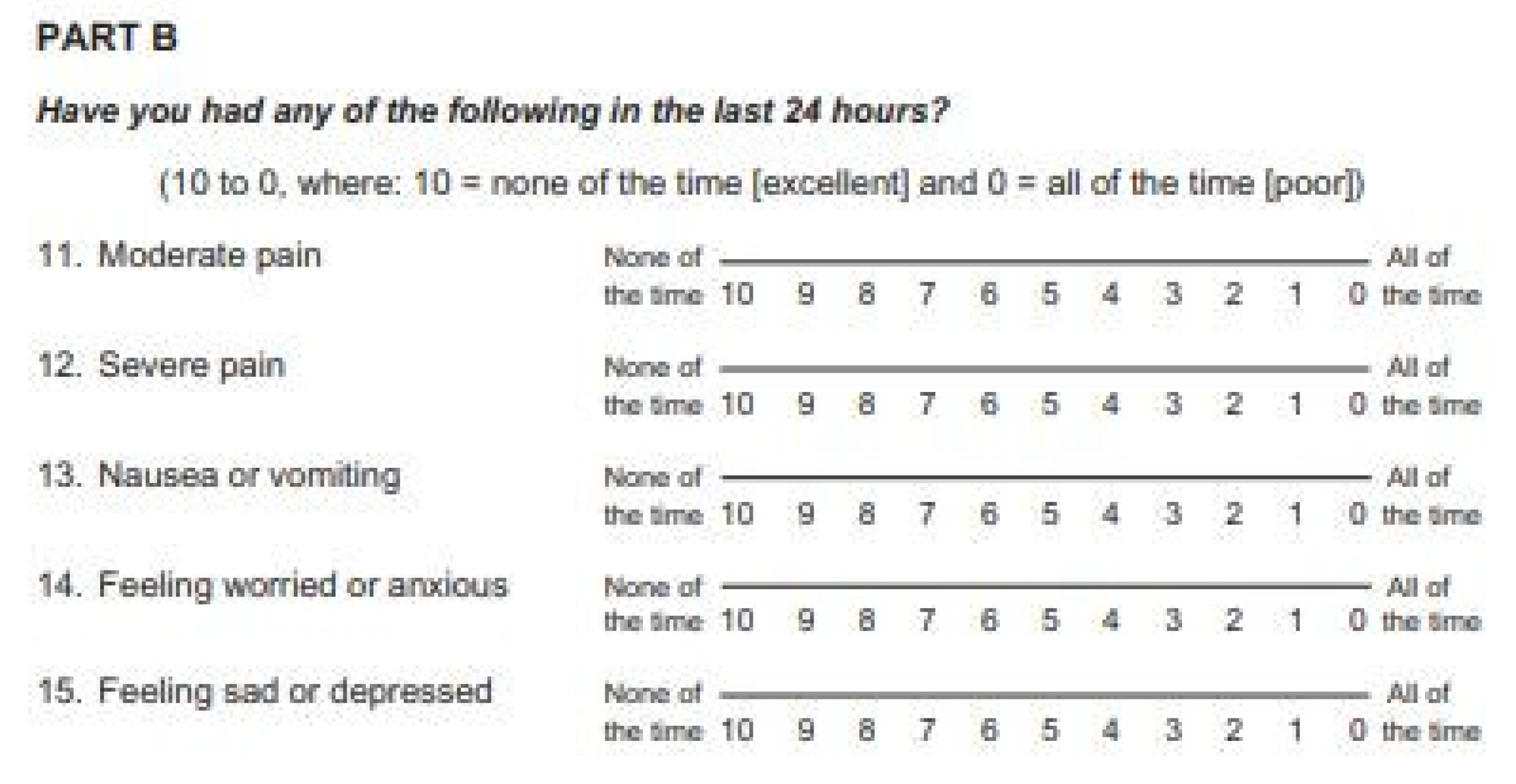
| 11. | Moderate pain |
| 12. | Severe pain |
| 13. | Nausea or vomiting |
| 14. | Feeling worried or anxious |
| 15. | Feeling sad or depressed |
Appendix B

Appendix C
| Neostigmine | Sugammadex | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preop n = 38 | POD1 n = 38 | POD2 n = 38 | Preop n = 39 | POD1 n = 39 | POD2 n = 37 | Preop | POD1 | POD2 | |
| Physical comfort | |||||||||
| Breath | 9.7 ± 0.7 | 8.2 ± 2.7 | 8.7 ± 2.4 | 9.6 ± 1.0 | 7.5 ± 2.6 | 9.4 ± 1.0 | 0.73 | 0.21 | 0.11 |
| Eat | 8.0 ± 3.3 | 5.2 ± 4.0 | 7.0 ± 3.0 | 8.9 ± 2.1 | 5.1 ± 3.9 | 7.7 ± 2.5 | 0.19 | 0.84 | 0.31 |
| Rest | 8.8 ± 2.0 | 5.7 ± 3.3 | 7.9 ± 2.6 | 9.3 ± 1.4 | 6.4 ± 3.0 | 8.5 ± 1.5 | 0.20 | 0.33 | 0.21 |
| Sleep | 8.3 ± 2.3 | 5.9 ± 3.2 | 7.7 ± 2.6 | 8.3 ± 2.1 | 6.1 ± 3.0 | 8.5 ± 1.4 | 0.97 | 0.86 | 0.13 |
| Nausea | 8.1 ± 2.9 | 7.1 ± 3.5 | 7.8 ± 3.2 | 8.9 ± 2.5 | 6.7 ± 3.4 | 7.7 ± 3.0 | 0.21 | 0.56 | 0.93 |
| Physical independence | |||||||||
| Wash | 9.3 ± 1.5 | 6.2 ± 3.6 | 8.2 ± 2.5 | 9.6 ± 1.0 | 6.1 ± 3.6 | 8.3 ± 1.9 | 0.35 | 0.82 | 0.79 |
| Work | 8.7 ± 2.7 | 3.0 ± 3.5 | 5.9 ± 3.5 | 8.8 ± 2.4 | 3.8 ± 3.5 | 6.1 ± 3.0 | 0.12 | 0.30 | 0.72 |
| Pain | |||||||||
| Moderate pain | 7.1 ± 3.1 | 3.2 ± 3.0 | 6.1 ± 2.6 | 8.0 ± 2.3 | 3.6 ± 3.0 | 5.5 ± 2.3 | 0.16 | 0.51 | 0.34 |
| Severe pain | 8.3 ± 2.8 | 4.9 ± 2.9 | 7.1 ± 3.2 | 8.6 ± 2.3 | 5.0 ± 3.1 | 7.1 ± 2.2 | 0.67 | 0.94 | 0.96 |
| Psychological support | |||||||||
| Talk | 9.5 ± 1.1 | 7.3 ± 3.0 | 8.7 ± 2.2 | 9.6 ± 1.1 | 7.4 ± 2.9 | 9.0 ± 1.6 | 0.58 | 0.92 | 0.45 |
| Help | 9.6 ± 1.0 | 9.0 ± 2.0 | 9.1 ± 2.0 | 9.7 ± 0.6 | 9.1 ± 1.8 | 9.0 ± 2.0 | 0.39 | 0.77 | 0.78 |
| Emotional state | |||||||||
| Emotion | 9.2 ± 1.4 | 7.7 ± 2.8 | 8.5 ± 2.4 | 9.3 ± 1.3 | 8.4 ± 1.9 | 9.0 ± 1.3 | 0.62 | 0.17 | 0.22 |
| Well-being | 8.7 ± 2.0 | 5.8 ± 3.0 | 7.6 ± 2.7 | 8.5 ± 1.6 | 5.9 ± 2.7 | 8.1 ± 1.6 | 0.68 | 0.87 | 0.31 |
| Anxiety | 7.7 ± 2.5 | 7.1 ± 3.2 | 8.2 ± 2.9 | 83 ± 2.3 | 6.8 ± 3.1 | 8.9 ± 1.7 | 0.32 | 0.72 | 0.22 |
| Depression | 8.5 ± 2.3 | 8.0 ± 2.5 | 7.8 ± 3.1 | 8.3 ± 2.2 | 7.4 ± 2.8 | 9.0 ± 1.5 | 0.71 | 0.30 | 0.41 |
| Total | 129.3 ± 25.2 | 94.4 ± 30.7 | 116.3 ± 31.1 | 133.6 ± 16.5 | 95.5 ± 27.7 | 122 ± 17.3 | 0.38 | 0.87 | 0.33 |
References
- Myles, P.S.; Weitkamp, B.; Jones, K.; Melick, J.; Hensen, S. Validity and reliability of a postoperative quality of recovery score: The QoR-40. Br. J. Anaesth. 2000, 84, 11–15. [Google Scholar] [CrossRef] [Green Version]
- Gornall, B.; Myles, P.; Smith, C.; Burke, J.; Leslie, K.; Pereira, M.; Bost, J.; Kluivers, K.; Nilsson, U.; Tanaka, Y.; et al. Measurement of quality of recovery using the QoR-40: A quantitative systematic review. Br. J. Anaesth. 2013, 111, 161–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mittal, G. Pain Management after Laparoscopic Cholecystectomy-A Randomized Prospective Trial of Low Pressure and Standard Pressure Pneumoperitoneum. J. Clin. Diagn.Res. 2014, 8, 92–94. [Google Scholar] [CrossRef]
- Wallace, D.H.; Serpell, M.G.; Baxter, J.N.; O’Dwyer, P.J. Randomized trial of different insufflation pressures for laparoscopic cholecystectomy. Br. J. Surg. 1997, 84, 455–458. [Google Scholar]
- Arslan, M.; Çiçek, R.; Kalender, H.Ü.; Yilmaz, H. Preventing Postoperative Nausea and Vomiting After Laparoscopic Cholecystectomy: A Prospective, Randomized, Double-Blind Study. Curr Ther Res. Clin. Exp. 2011, 72, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Hristovska, A.-M.; Duch, P.; Allingstrup, M.; Afshari, A. Efficacy and safety of Sugammadex versus Neostigmine in reversing neuromuscular blockade in adults. Acta Anaesthesiol. Scand. 2017, 8, CD012763. [Google Scholar] [CrossRef] [PubMed]
- Kirmeier, E.; Eriksson, L.I.; Lewald, H.; Fagerlund, M.J.; Hoeft, A.; Hollmann, M.; Meistelman, C.; Hunter, J.M.; Ulm, K.; Blobner, M.; et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): A multicentre, prospective observational study. Lancet Respir. Med. 2019, 7, 129–140. [Google Scholar] [CrossRef]
- Kheterpal, S.; Vaughn, M.T.; Dubovoy, T.Z.; Shah, N.J.; Bash, L.D.; Colquhoun, D.A.; Shanks, A.M.; Mathis, M.R.; Soto, R.G.; Bardia, A.; et al. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER). Anesthesiology 2020, 132, 1371–1381. [Google Scholar] [CrossRef]
- Oh, T.K.; Oh, A.-Y.; Ryu, J.-H.; Koo, B.-W.; Song, I.-A.; Nam, S.W.; Jee, H.-J. Retrospective analysis of 30-day unplanned readmission after major abdominal surgery with reversal by sugammadex or neostigmine. Br. J. Anaesth. 2019, 122, 370–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, R.D. Miller’s Anesthesia, 9th ed.; Glopper, M.A., Cohen, N.H., Eriksson, L.I., Fleisher, L.A., Leslie, K., Wiener-Kronish, J.P., Eds.; Elsevier: Philadelphia, PA, USA, 2015; Volume 1, pp. 846–847. [Google Scholar]
- Lee, J.H.; Kim, D.; Seo, D.; Son, J.-S.; Kim, D.-C. Validity and reliability of the Korean version of the Quality of Recovery-40 questionnaire. Korean J. Anesthesiol. 2018, 71, 467–475. [Google Scholar] [CrossRef]
- Yoon, S.; Joo, H.; Oh, Y.M.; Lee, J.; Bahk, J.-H.; Lee, H.-J. Validation and clinical utility of the Korean version of the Quality of Recovery-15 with enhanced recovery after surgery: A prospective observational cohort study. Br. J. Anaesth. 2020, 125, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Myles, P.S.; Myles, D.B.; Galagher, W.; Chew, C.; MacDonald, N.; Dennis, A. Minimal Clinically Important Difference for Three Quality of Recovery Scales. Anesthesiology 2016, 125, 39–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herrera, F.J.; Wong, J.; Chung, F. A Systematic Review of Postoperative Recovery Outcomes Measurements After Ambulatory Surgery. Anesth. Analg. 2007, 105, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Stark, P.A.; Myles, P.S.; Burke, J.A. Development and psychometric evaluation of a postoperative quality of recovery score: The QoR-15. Anesthesiology 2013, 118, 1332–1340. [Google Scholar] [CrossRef] [Green Version]
- Kleif, J.; Waage, J.; Christensen, K.B.; Gögenur, I. Systematic review of the QoR-15 score, a patient- reported outcome measure measuring quality of recovery after surgery and anaesthesia. Brit. J. Anaesth. 2018, 120, 28–36. [Google Scholar] [CrossRef] [Green Version]
- Kim, N.Y.; Koh, J.C.; Lee, K.-Y.; Kim, S.S.; Hong, J.H.; Nam, H.J.; Bai, S.-J. Influence of reversal of neuromuscular blockade with sugammadex or neostigmine on postoperative quality of recovery following a single bolus dose of rocuronium: A prospective, randomized, double-blinded, controlled study. J. Clin. Anesthesia 2019, 57, 97–102. [Google Scholar] [CrossRef]
- Amorim, P.; Lagarto, F.; Gomes, B.; Esteves, S.; Bismarck, J.; Rodrigues, N.; Nogueira, M. Neostigmine vs. sugammadex: Observational cohort study comparing the quality of recovery using the Postoperative Quality Recovery Scale. Acta Anaesthesiol. Scand. 2014, 58, 1101–1110. [Google Scholar] [CrossRef]
- Murphy, G.S.; Szokol, J.W.; Marymont, J.H.; Greenberg, S.B.; Avram, M.J.; Vender, J.S. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesthesia Analg. 2008, 107, 130–137. [Google Scholar] [CrossRef]
- Sauer, M.; Stahn, A.; Soltesz, S.; Noeldge-Schomburg, G.; Mencke, T. The influence of residual neuromuscular block on the incidence of critical respiratory events. A randomised, prospective, placebo-controlled trial. Eur. J. Anaesthesiol. 2011, 28, 842–848. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Oh, A.-Y.; Koo, B.-W.; Han, J.; Park, J.-H.; Hong, J.-P.; Seo, K.-S. Postoperative residual neuromuscular blockade after reversal based on a qualitative peripheral nerve stimulator response. Eur. J. Anaesthesiol. 2020, 37, 196–202. [Google Scholar] [CrossRef]
- Schepens, T.; Cammu, G.; Saldien, V.; De Neve, N.; Jorens, P.G.; Foubert, L.; Vercauteren, M. Electromyographic activity of the diaphragm during neostigmine or sugammadex-enhanced recovery after neuromuscular blockade with rocuronium: A randomised controlled study in healthy volunteers. Eur. J. Anaesthesiol. 2015, 32, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Cammu, G.; Schepens, T.; De Neve, N.; Wildemeersch, D.; Foubert, L.; Jorens, P.G. Diaphragmatic and intercostal electromyographic activity during neostigmine, sugammadex and neostigmine-sugammadex-enhanced recovery after neuromuscular blockade: A randomised controlled volunteer study. Eur. J. Anaesthesiol. 2017, 34, 8–15. [Google Scholar] [CrossRef]
- Buchanan, F.F.; Myles, P.S.; Cicuttini, F. Effect of patient sex on general anaesthesia and recovery. Br. J. Anaesth. 2011, 106, 832–839. [Google Scholar] [CrossRef] [Green Version]
- Scott, A.J.; Mason, S.E.; Langdon, A.J.; Patel, B.; Mayer, E.; Moorthy, K.; Purkayastha, S. Prospective Risk Factor Analysis for the Development of Post-operative Urinary Retention Following Ambulatory General Surgery. World J. Surg. 2018, 42, 3874–3879. [Google Scholar] [CrossRef] [Green Version]
- Selius, B.A.; Subedi, R. Urinary retention in adults: Diagnosis and initial management. Am. Fam Physician 2008, 77, 643–650. [Google Scholar] [PubMed]
- Cha, J.-E.; Park, S.W.; Choi, Y.I.; Oh, I.D.; Kang, H.Y.; Lee, S.H.; Choi, J.-H. Sugammadex use can decrease the incidence of post-operative urinary retention by avoiding anticholinergics: A retrospective study. Anesth. Pain Med. 2018, 13, 40–46. [Google Scholar] [CrossRef] [Green Version]


| Neostigmine, n = 38 | Sugammadex, n = 39 | |
|---|---|---|
| Age (years) | 51.3 ± 11.5 | 54.1 ± 10.7 |
| Weight (kg) | 69.1 ± 12.5 | 68.1 ± 15.5 |
| Height (cm) | 164.5 ± 9.1 | 166.6 ± 8.6 |
| Sex; male | 18 (47.4%) | 22 ± 56.4% |
| Operation time (min) | 41.2 ± 19.2 | 43.0 ± 21.2 |
| Anesthesia time (min) | 58.3 ± 22.2 | 63.6 ± 22.6 |
| Diagnosis | ||
| Chronic cholecystitis | 16 (42.1%) | 23 (59%) |
| Acute cholecystitis | 12 (31.6%) | 10 (25.6%) |
| Acute pancreatitis | 2 (5.3%) | 0 (0%) |
| GB Polyp | 6 (15.8%) | 5 (12.8%) |
| GB Adenomatosis | 1 (2.6%) | 1 (2.6%) |
| GB stone | 1 (2.6%) | 0 (0%) |
| ASA physical status | ||
| 1 | 18 (47.4%) | 15 (38.5%) |
| 2 | 18 (47.4%) | 19 (48.7%) |
| 3 | 2 (5.3%) | 5 (12.8%) |
| Hypertension | 12 (31.6%) | 9 (23.1%) |
| Diabetes mellitus | 4 (10.5%) | 6 (15.4%) |
| Coronary artery disease | 3 (7.9%) | 8 (20.5%) |
| Cerebral vascular disease | 1 (2.6%) | 2 (5.1%) |
| Cancer | 6 (15.8%) | 10 (25.6%) |
| Neostigmine, n = 38 | Sugammadex, n = 39 | p-Value | |
|---|---|---|---|
| Modified Aldrete score | 7.5 ± 0.6 | 7.4 ± 0.5 | 0.48 |
| PACU stay (min) | 27.7 ± 8.7 | 29.8 ± 9.4 | 0.32 |
| Pain score (NRS) | |||
| 30 min | 6.5 ± 1.4 | 6.6 ± 1.2 | 0.76 |
| 6 h | 3.6 ± 1.1 | 3.4 ± 1.0 | 0.41 |
| 24 h | 3.0 ± 0.7 | 2.9 ± 0.6 | 0.22 |
| Rescue analgesics * | 3.2 ± 1.9 | 3.3 ± 1.2 | 0.79 |
| Morphine equivalent dose (mg) | 14.5 ± 7.3 | 15.6 ± 6.2 | 0.46 |
| Rescue anti-emetics * | 0.4 ± 0.7 | 0.4 ± 0.7 | 0.92 |
| Urinary retention | 6 (15.8%) | 1 (2.6%) | 0.04 † |
| Length of hospital stay (days) | 3.5 ± 0.95 | 3.7 ± 1.0 | 0.29 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, J.; Oh, A.-Y.; Jeon, Y.-T.; Koo, B.-W.; Kim, B.Y.; Kim, D.; Hwang, I. Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2021, 10, 938. https://doi.org/10.3390/jcm10050938
Han J, Oh A-Y, Jeon Y-T, Koo B-W, Kim BY, Kim D, Hwang I. Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial. Journal of Clinical Medicine. 2021; 10(5):938. https://doi.org/10.3390/jcm10050938
Chicago/Turabian StyleHan, Jiwon, Ah-Young Oh, Yong-Tae Jeon, Bon-Wook Koo, Bo Young Kim, Donghyun Kim, and Insung Hwang. 2021. "Quality of Recovery after Laparoscopic Cholecystectomy Following Neuromuscular Blockade Reversal with Neostigmine or Sugammadex: A Prospective, Randomized, Controlled Trial" Journal of Clinical Medicine 10, no. 5: 938. https://doi.org/10.3390/jcm10050938






