Short (6 mm) and Regular Dental Implants in the Posterior Maxilla–7-Years Follow-up Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design
- Adult patients (>18 years old)
- Single missing tooth (first or second molar) in the lateral aspect of the maxilla to be replaced with a single implant-supported crown at the beginning of the study.
- Tooth loss due to caries, root canal treatment failure, no history of periodontal disease
- Minimal height of the alveolar ridge of 6 mm in the region of the implant insertion in the pre-surgical qualification
- Minimal width of the alveolar ridge of 6–7 mm in the region of interest
- API £35 (approximal plaque index)
- PI £25 (plaque index)
- Previous graft procedures in the area of interest
- Systemic or local diseases that could compromise healing or osteointegration
- Heavy smokers
- Patients with bruxism
2.2. Clinical Procedures: Randomization, Surgery, Implant Loading
2.3. Follow-up
2.4. Clinical Outcome
2.5. Marginal Bone Level
2.6. Crown-to-Implant Ratio (C/I Ratio)
2.7. Soft Tissue Measurement
2.8. Primary and Secondary Outcome Variables
2.9. Statistical Analysis
3. Results
3.1. Implant Survival Rate
3.2. Clinical Outcome Measures
3.3. Crown to Implant Ratio (C/I Ratio)
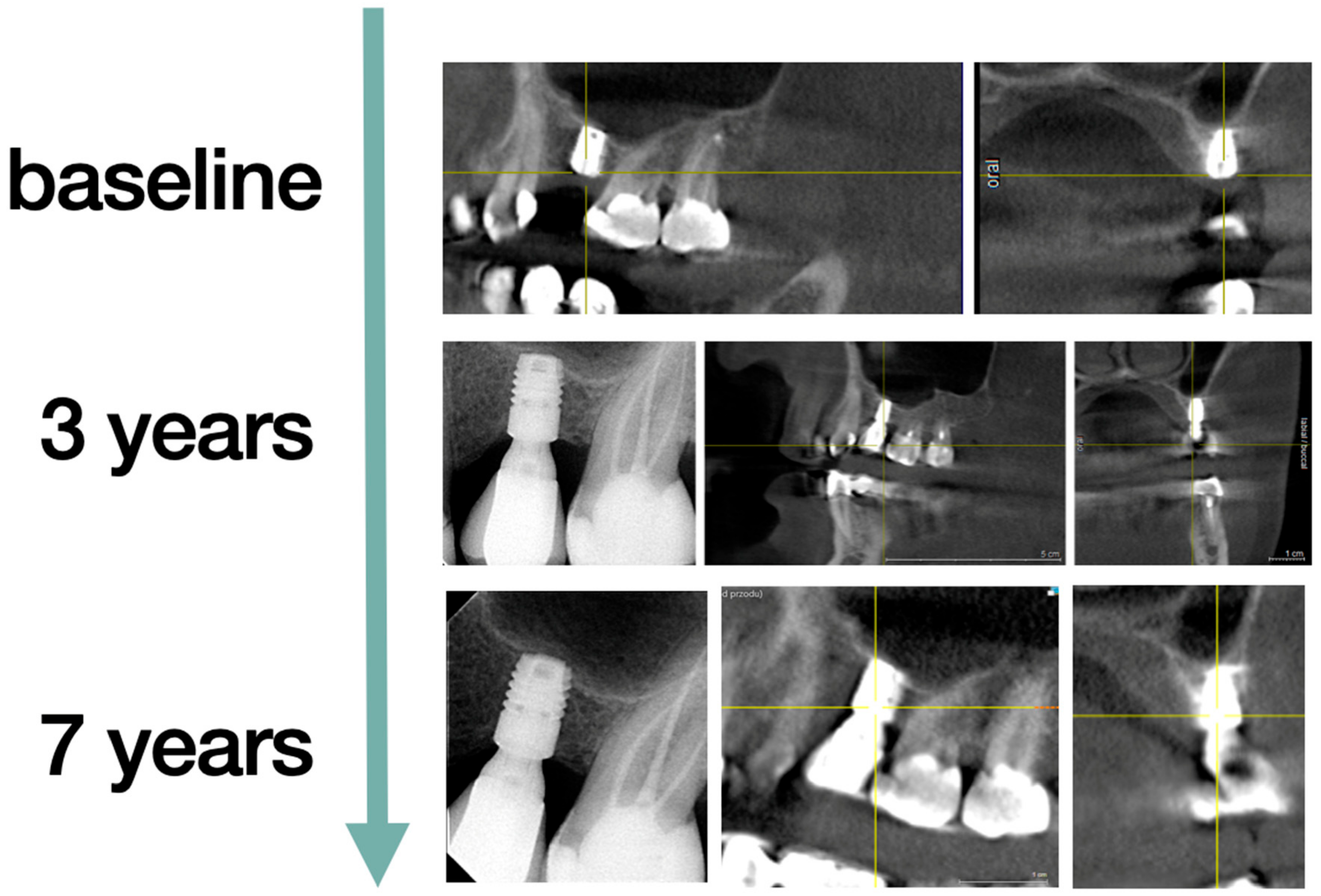
3.4. Marginal Bone Loss
3.5. Technical Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chappuis, V.; Araújo, M.G.; Buser, D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontology 2000 2017, 73, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Aludden, H.; Hallman, M.; Dahlin, C.; Christensen, A.E.; Mordenfeld, A. A systematic review and meta-analysis of long-term studies (five or more years) assessing maxillary sinus floor augmentation. Int. J. Oral Maxillofac. Surg. 2018, 47, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Tatum, H. Maxillary and sinus implant reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar]
- Boyne, P.J. Grafting of the maxillary sinus floor with autogenous marrow and bone. Oral Surg. 1980, 38, 613–616. [Google Scholar]
- Esposito, M.; Grusovin, M.G.; Rees, J.; Karasoulos, D.; Felice, P.; Alissa, R.; Worthington, H.V.; Coulthard, P. Interventions for replacing missing teeth: Augmentation procedures of the maxillary sinus. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2010. [Google Scholar]
- Silva, L.D.; de Lima, V.N.; Faverani, L.P.; de Mendonça, M.R.; Okamoto, R.; Pellizzer, E.P. Maxillary sinus lift surgery—with or without graft material? A systematic review. Int. J. Oral Maxillofac. Surg. 2016, 45, 1570–1576. [Google Scholar] [CrossRef] [Green Version]
- Matys, J.; Hadzik, J.; Dominiak, M. Schneiderian Membrane Perforation Rate and Increase in Bone Temperature during Maxillary Sinus Floor Elevation by Means of Er: YAG Laser-An Animal Study in Pigs. Implant Dent. 2017, 26, 238–244. [Google Scholar] [CrossRef]
- Giesenhagen, B.; Martin, N.; Jung, O.; Barbeck, M. Bone Augmentation and Simultaneous Implant Placement with Allogenic Bone Rings and Analysis of Its Purification Success. Materials 2019, 12, 1291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramírez Fernández, M.; Gehrke, S.; Mazón, P.; Calvo-Guirado, J.; De Aza, P. Implant Stability of Biological Hydroxyapatites Used in Dentistry. Materials 2017, 10, 644. [Google Scholar] [CrossRef] [Green Version]
- Iezzi, G.; Perrotti, V.; Felice, P.; Barausse, C.; Piattelli, A.; Del Fabbro, M. Are <7-mm long implants in native bone as effective as longer implants in augmented bone for the rehabilitation of posterior atrophic jaws? A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2020, 22, 552–566. [Google Scholar] [CrossRef]
- Torres-Alemany, A.; Fernández-Estevan, L.; Agustín-Panadero, R.; Montiel-Company, J.M.; Labaig-Rueda, C.; Mañes-Ferrer, J.F. Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3271. [Google Scholar] [CrossRef]
- Hadzik, J.; Krawiec, M.; Kubasiewicz-Ross, P.; Prylińska-Czyżewska, A.; Gedrange, T.; Dominiak, M. Short implants and conventional implants in the residual maxillary alveolar ridge: A 36-month follow-up observation. Med. Sci. Monit. 2018, 24, 5645–5652. [Google Scholar] [CrossRef] [PubMed]
- Hadzik, J.; Krawiec, M.; Sławecki, K.; Kunert-Keil, C.; Dominiak, M.; Gedrange, T. The Influence of the Crown-Implant Ratio on the Crestal Bone Level and Implant Secondary Stability: 36-Month Clinical Study. BioMed Res. Int. 2018, 2018, 4246874. [Google Scholar] [CrossRef]
- Derks, J.; Schaller, D.; Håkansson, J.; Wennström, J.L.; Tomasi, C.; Berglundh, T. Peri-implantitis—Onset and pattern of progression. J. Clin. Periodontol. 2016, 43, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Puzio, M.; Błaszczyszyn, A.; Hadzik, J.; Dominiak, M. Ultrasound assessment of soft tissue augmentation around implants in the aesthetic zone using a connective tissue graft and xenogeneic collagen matrix—1-year randomised follow-up. Ann. Anat. 2018, 217, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Tawil, G.; Younan, R. Clinical Evaluation of Short, Machined-Surface Implants Followed for 12 to 92 Months. Int. J. Oral Maxillofac Implants 2003, 18, 894–901. [Google Scholar] [CrossRef]
- Nisand, D.; Renouard, F. Short implant in limited bone volume. Periodontology 2000 2014, 66, 72–96. [Google Scholar] [CrossRef]
- Thoma, D.S.; Haas, R.; Sporniak-Tutak, K.; Garcia, A.; Taylor, T.D.; Hämmerle, C.H.F. Randomized controlled multicentre study comparing short dental implants (6 mm) versus longer dental implants (11–15 mm) in combination with sinus floor elevation procedures: 5-Year data. J. Clin. Periodontol. 2018, 45, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, M.; Wallace, S.; Testori, T. Long-Term Implant Survival in the Grafted Maxillary Sinus: A Systematic Review. Int. J. Periodontics Restor. Dent. 2013, 33, 773–783. [Google Scholar] [CrossRef]
- Pohl, V.; Thoma, D.S.; Sporniak-Tutak, K.; Garcia-Garcia, A.; Taylor, T.D.; Haas, R.; Hämmerle, C.H. Short dental implants (6 mm) versus long dental implants (11–15 mm) in combination with sinus floor elevation procedures: 3-year results from a multicentre, randomized, controlled clinical trial. J. Clin. Periodontol. 2017, 44, 438–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papaspyridakos, P.; De Souza, A.; Vazouras, K.; Gholami, H.; Pagni, S.; Weber, H.P. Hans-Peter Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis. Clin. Oral Implant. Res. 2018, 29, 8–20. [Google Scholar] [CrossRef]
- Pistilli, R.; Felice, P.; Piattelli, M.; Gessaroli, M.; Soardi, E.; Barausse, C.; Buti, J.; Corvino, V.; Esposito, M. Posterior atrophic jaws rehabilitated with prostheses supported by 5 × 5 mm implants with a novel nanostructured calcium-incorporated titanium surface or by longer implants in augmented bone. One-year results from a randomised controlled trial. Eur. J. Oral Implant. 2013, 6, 343–357. [Google Scholar]
- Gastaldi, G.; Felice, P.; Pistilli, R.; Barausse, C.; Trullenque-Eriksson, A.; Esposito, M. Short implants as an alternative to crestal sinus lift: A 3-year multicentre randomised controlled trial. Eur. J. Oral Implant. 2017, 10, 391–400. [Google Scholar]
- Akram, Z.; Vohra, F.; Sheikh, S.A.; Albaijan, R.; Bukhari, I.A.; Hussain, M. Clinical and radiographic peri-implant outcomes of short dental implants placed in posterior jaws of patients with treated generalized aggressive periodontitis: A 3-year follow-up study. Clin. Implant Dent. Relat. Res. 2019, 21, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Koldsland, O.C.; Scheie, A.A.; Aass, A.M. Prevalence of Peri-Implantitis Related to Severity of the Disease with Different Degrees of Bone Loss. J. Periodontol. 2010, 81, 231–238. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Clin. Periodontol. 2018, 45, S286–S291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.L.; Cochran, D.; Sculean, A.; Canullo, L. How frequent does peri-implantitis occur? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 1805–1816. [Google Scholar] [CrossRef]
- Wada, M.; Mameno, T.; Onodera, Y.; Matsuda, H.; Daimon, K.; Ikebe, K. Prevalence of peri-implant disease and risk indicators in a Japanese population with at least 3 years in function-A multicentre retrospective study. Clin. Oral Implant. Res. 2019, 30, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Papi, P.; Di Carlo, S.; Mencio, F.; Rosella, D.; De Angelis, F.; Pompa, G. Dental Implants Placed in Patients with Mechanical Risk Factors: A Long-term Follow-up Retrospective Study. J. Int. Soc. Prev. Community Dent. 2017, 7, S48–S51. [Google Scholar] [CrossRef] [Green Version]
- Puisys, A.; Linkevicius, T. The influence of mucosal tissue thickening on crestal bone stability around bone-level implants. A prospective controlled clinical trial. Clin. Oral Implant. Res. 2015, 26, 123–129. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant Dent. Relat. Res. 2015, 17, 1228–1236. [Google Scholar] [CrossRef] [PubMed]
- Linkevicius, T.; Apse, P.; Grybauskas, S.; Puisys, A. The influence of soft tissue thickness on crestal bone changes around implants: A 1-year prospective controlled clinical trial. Int. J. Oral Maxillofac. Implant. 2009, 24, 712–719. [Google Scholar]
- Bhat, P.; Thakur, S.; Kulkarni, S. The influence of soft tissue biotype on the marginal bone changes around dental implants: A 1-year prospective clinico-radiological study. J. Indian Soc. Periodontol. 2015, 19, 640–644. [Google Scholar] [CrossRef]
- Lissek, M.; Boeker, M.; Happe, A. How thick is the oral mucosa around implants after augmentation with different materials: A systematic review of the effectiveness of substitute matrices in comparison to connective tissue grafts. Int. J. Mol. Sci. 2020, 21, 5043. [Google Scholar] [CrossRef] [PubMed]






| Demographics of the Study Population | ||||
|---|---|---|---|---|
| Short Implants (G1) | Regular Implants (G2) | Total | p-Value | |
| Number of implants (Baseline) | 15 | 15 | 30 | |
| Number of implants (seven years) | 13 | 15 | 27 | |
| Implants survived (seven years) | 87% | 100% | 93% | 0.4828 Fisher’s exact test |
| Age in years at base line mean ± SD (Range) | 48.8 ± 11.4 (26–64) | 42.3 ± 13.5 (26–63) | 45.5 ± 12.7 (26–64) | 0.1623 unpaired t test |
| Age in years after seven years mean ± SD (Range) | 54.9 ± 11.4 (33–70) | 49.3 ± 13.5 (33–70) | 51.9 ± 12.7 (33–70) | 0.2451 unpaired t test |
| Gender | 10 Females, 5 Males | 10 Females, 5 Males | ||
| Implant length | 6 mm | 11 and 13 mm | ||
| Short Implants G1 | Regular Implants G2 | p-Value | ||
|---|---|---|---|---|
| HKT (mm) | Mean: | 2.95 | 2.55 | 0.4126 unpaired t test |
| SD: | 1.42 | 1.18 | ||
| Range: | 1.0–6.0 | 1.0–5.0 | ||
| PD (mm) | Mean: | 2.62 | 2.63 | 0.9456 unpaired t test |
| SD: | 0.51 | 0.81 | ||
| Range: | 2.0–3.0 | 1.0–5.0 | ||
| STT (mm) | Mean: | 1.78 | 1.79 | 0.9497 unpaired t test |
| SD: | 0.58 | 0.61 | ||
| Range: | 1.0–2.6 | 0.9–2.5 | ||
| BOP | No % | 53.85% | 40.00% | 0.7051 Fisher’s exact test |
| Yes % | 46.15% | 60.00% |
| Short Implants G1 | Regular Implants G2 | p-Value | ||
|---|---|---|---|---|
| C/I ratio | Min | 1.36 | 0.68 | <0.0001 * unpaired t test significant different |
| Max | 1.97 | 1.65 | ||
| Mean: | 1.64 | 1.06 | ||
| SD: | 0.20 | 0.29 | ||
| Median: | 1.68 | 1.05 |
| Short Implants G1 | Regular Implants G2 | p-Value | ||
|---|---|---|---|---|
| MBL seven years | Min | 0.10 | 0.00 | 0.3263 Mann–Whitney U |
| Max | 1.30 | 2.20 | ||
| Mean: | 0.50 | 0.53 | ||
| SD: | 0.35 | 0.75 |
| Correlation | C/I Ratio: MBL | MBL:HKT | MBL:STT | HKT:STT |
|---|---|---|---|---|
| r | −0.02666 | −0.1548 | −0.3899 | 0.5201 |
| Test | Spearman | Spearman | Spearman | Pearson |
| Significance | No | No | Yes (negative correlation) | Yes (positive correlation) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadzik, J.; Kubasiewicz-Ross, P.; Nawrot-Hadzik, I.; Gedrange, T.; Pitułaj, A.; Dominiak, M. Short (6 mm) and Regular Dental Implants in the Posterior Maxilla–7-Years Follow-up Study. J. Clin. Med. 2021, 10, 940. https://doi.org/10.3390/jcm10050940
Hadzik J, Kubasiewicz-Ross P, Nawrot-Hadzik I, Gedrange T, Pitułaj A, Dominiak M. Short (6 mm) and Regular Dental Implants in the Posterior Maxilla–7-Years Follow-up Study. Journal of Clinical Medicine. 2021; 10(5):940. https://doi.org/10.3390/jcm10050940
Chicago/Turabian StyleHadzik, Jakub, Paweł Kubasiewicz-Ross, Izabela Nawrot-Hadzik, Tomasz Gedrange, Artur Pitułaj, and Marzena Dominiak. 2021. "Short (6 mm) and Regular Dental Implants in the Posterior Maxilla–7-Years Follow-up Study" Journal of Clinical Medicine 10, no. 5: 940. https://doi.org/10.3390/jcm10050940
APA StyleHadzik, J., Kubasiewicz-Ross, P., Nawrot-Hadzik, I., Gedrange, T., Pitułaj, A., & Dominiak, M. (2021). Short (6 mm) and Regular Dental Implants in the Posterior Maxilla–7-Years Follow-up Study. Journal of Clinical Medicine, 10(5), 940. https://doi.org/10.3390/jcm10050940







