Impact of Heart Failure on In-Hospital Outcomes after Surgical Femoral Neck Fracture Treatment
Abstract
1. Introduction
2. Methods
2.1. Study Design, Data Source, and Patient Population
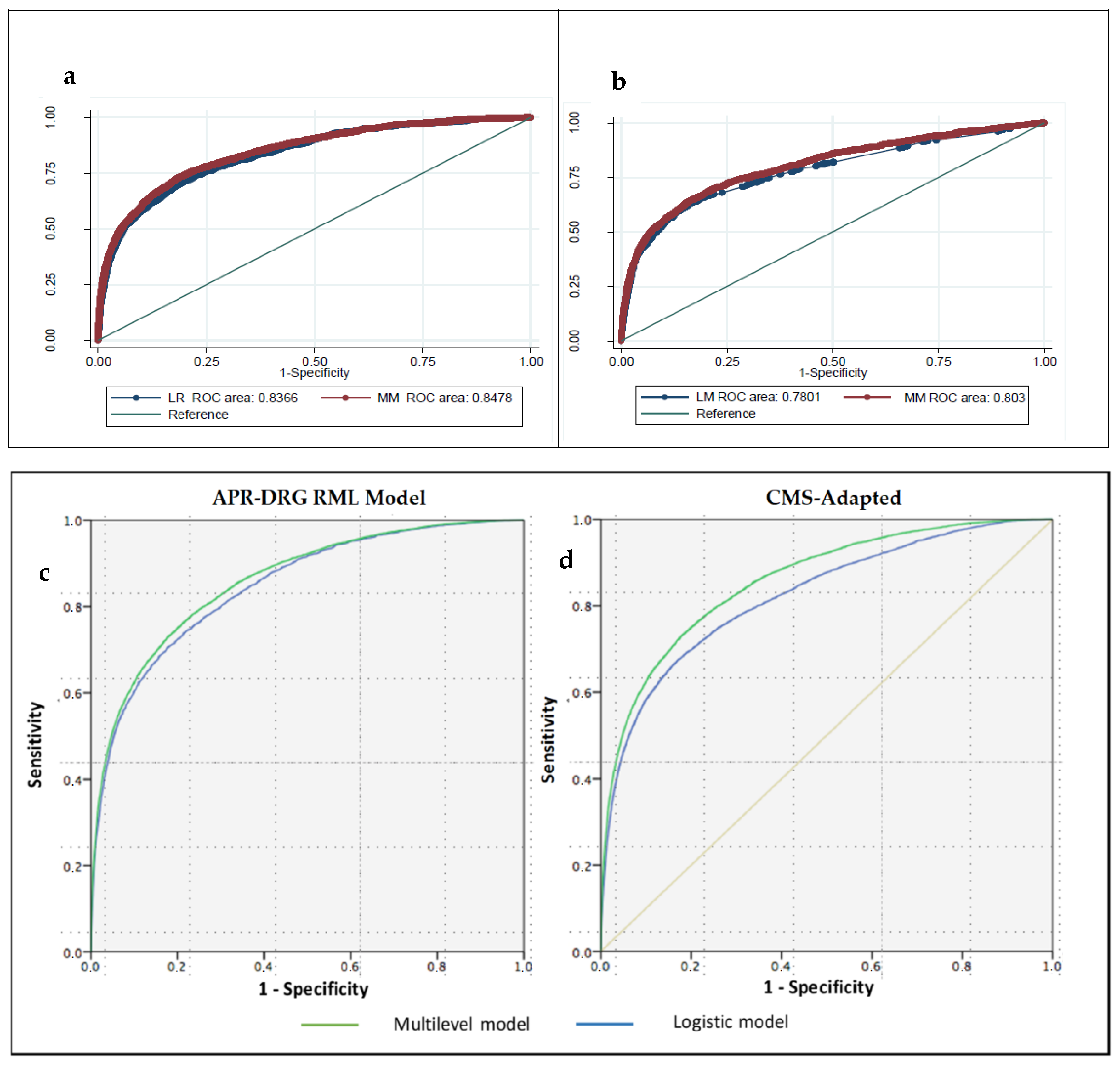
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Cooper, C.; Campion, G.; Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Schneider, K.; Audige, L.; Kuehnel, S.P.; Helmy, N. The direct anterior approach in hemiarthroplasty for displaced femoral neck fractures. Int. Orthop. 2012, 36, 1773–1781. [Google Scholar] [CrossRef] [PubMed]
- Richmond, J.; Aharonof, G.B.; Zuckerman, J.D.; Koval, K.J. Mortality risk after hip fracture. J. Orthop. Trauma. 2003, 17 (Suppl. 8), S2–S5. [Google Scholar] [CrossRef] [PubMed]
- Shiga, T.; Wajima, Z.; Ohe, Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can. J. Anaesth. 2008, 55, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Scottish Intercollegiate Guidelines Network (SIGN). Prevention and management of hip fractures in older people; SIGN Publication No 56; SIGN: Edinburgh, UK, 2002; pp. 1–40. [Google Scholar]
- Cooney, L.M., Jr. Hip fracture outcomes. Arch. Intern. Med. 1997, 157, 485–486. [Google Scholar] [CrossRef]
- Ponikowski, P.; Anker, S.D.; AlHabib, K.F.; Cowie, M.R.; Force, T.L.; Hu, S.; Jaarsma, T.; Krum, H.; Rastogi, V.; Rohde, L.E.; et al. Heart failure: Preventing disease and death worldwide. ESC Heart Fail. 2014, 1, 4–25. [Google Scholar] [CrossRef] [PubMed]
- Zapatero-Gaviria, A.; Barba-Martín, R.; Canora Lebrato, J.; Fernández-Pérez, C.; Gómez-Huelgas, R.; Bernal-Sobrino, J.L.; Díez-Manglano, J.; Marco-Martínez, J.; Elola-Somoza, F.J. RECALMIN, I.I. Eight years of hospitalisation in Internal Medicine Units (2007–2014). What has changed? Rev. Clin. Esp. 2017, 217, 446–453. [Google Scholar] [CrossRef]
- Carbone, L.; Buzkova, P.; Fink, H.A.; Lee, J.S.; Chen, Z.; Ahmed, A.; Parashar, S.; Robbins, J.R. Hip fractures and heart failure: Findings from the Cardiovascular Health Study. Eur. Heart J. 2010, 31, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Alhambra, D.; Reyes, C.; Sainz, M.S.; González-Macías, J.; Delgado, L.G.; Bouzón, C.A.; Gañan, M.S.; Miedes, M.D.; Vaquero-Cervino,, E.; Bardaji, M.F.B.; et al. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: The Spanish registry of osteoporotic femur fractures prospective cohort study. Arch. Osteoporos. 2018, 13. [Google Scholar] [CrossRef]
- Sanz-Reig, J.; Salvador Marín, J.; Ferrández Martínez, J.; Orozco Beltrán, D.; Martínez López, J.F.; Quesada Rico, J.A. Prognostic factors and predictive model for in-hospital mortality following hip fractures in the elderly. Chin. J. Traumatol. 2018, 21, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Bartra, A.; Caeiro, M.; Mesa-Ramos, M.; Etxebarría-Foronda, I.; Montejo, J.; Carpintero, P.; Sorio-Vilela, F.; Gatell, S.; Canals, L.; en Representación de los Investigadores del Estudio PROA. Coste de la fractura de cadera osteoporótica en España por comunidad autónoma. Rev. Esp. Cir. Ortop. Traumatol. 2018, 63, 56–68. [Google Scholar] [CrossRef]
- Lizaur-Utrilla, A.; Calduch Broseta, J.V.; Miralles Munoz, F.A.; Segarra Soria, M.; Diaz Castellano, M.; Andreu Gimenez, L. Effectiveness of co-management between orthopedic surgeons and internists for inpatient elders with hip fracture. Med. Clin. 2014, 143, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Registro de altas de Hospitalización: CMBD del Sistema Nacional de Salud. Glosario de Términos y Definiciones. Portal Estadístico del SNS [actualizado September 2016]. pp. 5–6. Available online: http://pestadistico.inteligenciadegestion.msssi.es/publicoSNS/comun/DescargaDocumento.aspx?IdNodo=6415 (accessed on 16 January 2018).
- Averill, R.F.; McCullough, E.C.; Goldfield, N.; Hughes, J.S.; Bonazelli, J.; Bentley, L. APR-DRG Definition Manual v.31.0 2013. Available online: https://www.hcup-us.ahrq.gov/db/nation/nis/grp031_aprdrg_meth_ovrview.pdf (accessed on 15 August 2018).
- Krumholz, H.M.; Wang, Y.; Mattera, J.A.; Wang, Y.; Han, L.F.; Ingber, M.J.; Roman, S.; Normand, S.-L.T. An administrative claims model suitable for profiling hospital performance based on 30 day mortality rates among patients with an acute myocardial infarction. Circulation 2006, 113, 168392. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I. Dimensions of risk. In Risk Adjustment for Measuring Health Care Outcomes, 2nd ed.; Iezzoni, L.I., Ed.; Health Administration Press: Ann Arbor, MI, USA, 1997; p. 43168. [Google Scholar]
- Normand, S.L.T.; Glickman, M.E.; Gatsonis, C.A. Statistical methods for profiling providers of medical care: Issues and applications. J. Am. Stat. Assoc. 1997, 92, 80314. [Google Scholar] [CrossRef]
- Goldstein, H.; Spiegelhalter, D.J. League tables and their limitations: Statistical aspects of institutional performance. J. R. Stat. Soc. 1996, 159, 385444. [Google Scholar] [CrossRef]
- Romano, P.S.; Chan, B.K. Risk-adjusting acute myocardial infarction mortality: Are APR-DRGs the right tool? Health Serv. Res. 2000, 34, 1469–1489. [Google Scholar]
- Measures Updates and Specifications: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measure (Version 7.0). Yale New Haven Health Services Corporation/Centre for Outcomes Research and Evaluation (YNHHSC/CORE). Centres for Medicare & Medicaid Services (CMS); 2013. Available online: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Mortality_AMI-HF-PN_Measures_Updates_Report_FINAL_06-13-2013.pdf (accessed on 15 August 2018).
- Pope, G.C.; Ellis, R.P.; Ash, A.S.; Liu, C.F.; Ayanian, J.Z.; Bates, D.W.; Burstin, H.; Iezzoni, L.I.; Ingber, M.J. Principal inpatient diagnostic cost group model for Medicare risk adjustment. Health Care Financ. Rev. 2000, 21, 93–118. [Google Scholar]
- AHRQ QITM Version v6.0 ICD9CM, Inpatient quality indicators #91, Technical Specifications, Mortality for Selected Conditions. Available online: www.qualityindicators.ahrq.gov (accessed on 15 August 2018).
- Shahian, D.M.; Normand, S.L.; Torchiana, D.F.; Lewis, S.M.; Pastore, J.O.; Kuntz, R.E.; Dreyer, P.I. Cardiac surgery report cards: Comprehensive review and statistical critique. Ann. Thorac. Surg. 2001, 72, 215568. [Google Scholar]
- Damrauer, S.; Gaffey, A.C.; DeBord Smith, A.; Fairman, R.M.; Nguyen, L.L. Comparison of risk factors for length of stay and readmission following lower extremity bypass surgery. J. Vasc. Surg. 2015, 62, 1192–1200. [Google Scholar] [CrossRef] [PubMed]
- Zapatero Gaviria, A.; Barba Martín, R.; Román Sánchez, P.; Casariego Vales, E.; Diez Manglano, J.; García Cors, M.; Jusdado Ruiz-Capillas, J.J.; Suárez Fernández, C.; Bernal, J.L.; Elola Somoza, F.J. RECALMIN. La atención al paciente en las unidades de Medicina Interna del Sistema Nacional de Salud. Rev. Clínica Española 2016, 216, 175–182. [Google Scholar] [CrossRef]
- Endo, A.; Bear, H.J.; Nagao, M.; Weaver, M.J. Prediction model of in-hospital mortality after hip fracture surgery. J. Orthop. Trauma. 2018, 32, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Van Diepen, S.; Bakal, J.A.; McAlister, F.A.; Ezekowitz, J.A. Mortality and readmission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery: An analysis of 38 047 patients. Circulation 2011, 124, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Cullen, M.W.; Gullerud, R.E.; Larson, D.R.; Melton, L.J., 3rd; Huddleston, J.M. Impact of heart failure on hip fracture outcomes: A population-based study. J. Hosp. Med. 2011, 6, 507–512. [Google Scholar] [CrossRef]
- Anguita Sánchez, M.; Crespo Leiro, M.G.; deTeresa Galván, E.; Jiménez Navarro, M.; Alonso-Pulpón, L.; Muñiz García, J.; PRICE Study Investigators. Prevalence of heart failure in the Spanish general population aged over 45 years. The PRICE Study. Rev. Esp. Cardiol. 2008, 61, 1041–1049. [Google Scholar] [CrossRef]
- Pareja Sierra, T.; Bartolomé Martín, I.; Rodríguez Solís, J.; Bárcena Goitiandia, L.; Torralba González de Suso, M.; Morales Sanz, M.D.; Hornillos Calvo, M. Predictive factors of hospital stay, mortality and functional recovery after surgery for hip fracture in elderly patients. Rev. Esp. Cir. Ortop. Traumatol. 2017, 61, 427–435. [Google Scholar] [CrossRef]
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and mortality of hip fractures in the United States. JAMA 2009, 302, 1573–1579. [Google Scholar] [CrossRef] [PubMed]
- Instituto de Información Sanitaria. Estadísticas Comentadas: La Atención a la Fractura de Cadera en los Hospitales del SNS [Publicación en Internet]. Madrid: Ministerio de Sanidad y Política Social. 2010. Available online: http://www.msps.es/estadEstudios/estadisticas/cmbdhome.htm (accessed on 22 November 2018).
- Nikkel, L.; Kates, S.L.; Schreck, M.; Maceroli, M.; Mahmood, B.; Elfar, J.C. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: Retrospective cohort study. BMJ 2015, 351, h6246. [Google Scholar] [CrossRef] [PubMed]
- Hammill, B.G.; Curtis, L.H.; Bennett-Guerrero, E.; O’Connor, C.M.; Jollis, J.G.; Schulman, K.A.; Hernandez, A.F. Impact of heart failure on patients undergoing major noncardiac surgery. Anesthesiology. 2008, 108, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Upshaw, J.; Kiernan, M.S. Preoperative cardiac risk assessment for noncardiac surgery in patients with heart failure. Curr. Heart Fail. Rep. 2013, 10, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Reginelli, J.P.; Mills, R.M. Non-cardiac surgery in the heart failure patient. Heart 2001, 85, 505–507. [Google Scholar] [CrossRef]
- Rostagno, C.; Buzzi, R.; Campanacci, D.; Boccacini, A.; Cartei, A.; Virgili, G.; Belardinelli, A.; Matarrese, D.; Ungar, A.; Rafanelli, M.; et al. In Hospital and 3-Month Mortality and Functional Recovery Rate in Patients Treated for Hip Fracture by a Multidisciplinary Team. PLoS ONE 2016, 11, e0158607. [Google Scholar] [CrossRef]
- Marco Martínez, J.; Montero Ruíz, E.; Fernández Pérez, C.; Méndez Bailón, M.; García Klepzig, J.L.; Garrachón Vallo, F. Encuesta nacional sobre la actividad de los internistas en asistencia compartida–interconsultas en los hospitales españoles. Rev. Clínica Española 2016, 216, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Itagaki, A.; Kakizaki, A.; Funahashi, M.; Sato, K.; Yasuhara, K.; Ishikawa, A. Impact of heart failure on functional recovery after hip fracture. J. Phys. Ther. Sci. 2019, 31, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Tamamura, Y.; Matsuura, M.; Shiba, S.; Nishikimi, T. Heart failure assessed based on plasma B-type natriuretic peptide (BNP) levels negatively impacts activity of daily living in patients with hip fracture. PLoS ONE 2020, 15, e0237387. [Google Scholar] [CrossRef] [PubMed]
| Secondary Diagnosis | CIE-9-MC Codes |
|---|---|
| Acute Myocardial Infarction | 410.0, 410.1 |
| Acute Pulmonary Edema or Shock | 427.41, 427.42, 427.5, 518.4, 518.5, 518.51, 518.52, 518.53, 518.81, 518.82, 518.83, 518.84,785.50, 785.51, 798.0, 798.1, 798.2, 798.9, 799.01, 799.02, 998.01 |
| Stroke | 433.01; 433.11; 433.21; 433.31; 433.81; 433.91; 434.01; 434.11; 434.91; 436) |
| Pulmonary Thromboembolism | 415.1, 415.11, 415.12, 415.13, 415.19 |
| Non-HF Group | HF Group | Total | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Mean age (SD) | 83.5 | ±7.1 | 86.1 | ±6.3 | 83.7 | ±7 | <0.001 |
| Women | 169,543 | 77.2 | 10,406 | 77.6 | 179,949 | 77.2 | 0.271 |
| History of PTCA | 2215 | 1.0 | 181 | 1.3 | 2396 | 1.0 | <0.001 |
| History of CABG | 1111 | 0.5 | 81 | 0.6 | 1192 | 0.5 | 0.221 |
| Stroke | 756 | 0.3 | 111 | 0.8 | 867 | 0.4 | <0.001 |
| Pulmonary thromboembolism | 378 | 0.2 | 94 | 0.7 | 472 | 0.2 | <0.001 |
| Acute pulmonary edema or cardiogenic shock | 5164 | 2.3 | 2439 | 18.2 | 7603 | 3.3 | <0.001 |
| Chronic atherosclerosis | 15,912 | 7.2 | 1774 | 13.2 | 17,686 | 7.6 | <0.001 |
| Cardio-respiratory failure and shock | 5625 | 2.6 | 2508 | 18.7 | 8133 | 3.5 | <0.001 |
| Valvular and rheumatic heart disease | 7608 | 3.5 | 1742 | 13.0 | 9350 | 4.0 | <0.001 |
| Hypertension | 118,243 | 53.8 | 7788 | 58.0 | 126,031 | 54.1 | <0.001 |
| Renal failure | 17,509 | 8.0 | 3532 | 26.3 | 21,041 | 9.0 | <0.001 |
| COPD | 14,278 | 6.5 | 1767 | 13.2 | 16,045 | 6.9 | <0.001 |
| Pneumonia | 31,601 | 14.4 | 3298 | 24.6 | 34,899 | 15.0 | <0.001 |
| Diabetes Mellitus and complications | 52,006 | 23.7 | 3753 | 28.0 | 55,759 | 23.9 | <0.001 |
| Protein_calorie malnutrition | 4501 | 2.0 | 630 | 4.7 | 5131 | 2.2 | <0.001 |
| Dementia and senility | 44,402 | 20.2 | 2991 | 22.3 | 47,393 | 20.3 | <0.001 |
| Hemiplegia, paraplegia, paralysis, functional disability 67–69, 100–102, 177–178 | 5715 | 2.6 | 348 | 2.6 | 6063 | 2.6 | 0.961 |
| Peripheral vascular disease | 125,538 | 57.1 | 9169 | 68.3 | 134,707 | 57.8 | <0.001 |
| Severe cancers | 2619 | 1.2 | 192 | 1.4 | 2811 | 1.2 | 0.014 |
| Trauma CC154–156, 158–161 | 8143 | 3.7 | 603 | 4.5 | 8746 | 3.8 | <0.001 |
| Mayor psychiatric disorders | 2319 | 1.1 | 149 | 1.1 | 2468 | 1.1 | 0.544 |
| Chronic liver disease | 849 | 0.4 | 58 | 0.4 | 907 | 0.4 | 0.406 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marco-Martínez, J.; Bernal-Sobrino, J.L.; Fernández-Pérez, C.; Elola-Somoza, F.J.; Azaña-Gómez, J.; García-Klepizg, J.L.; Andrès, E.; Zapatero-Gaviria, A.; Barba-Martin, R.; Marco-Martinez, F.; et al. Impact of Heart Failure on In-Hospital Outcomes after Surgical Femoral Neck Fracture Treatment. J. Clin. Med. 2021, 10, 969. https://doi.org/10.3390/jcm10050969
Marco-Martínez J, Bernal-Sobrino JL, Fernández-Pérez C, Elola-Somoza FJ, Azaña-Gómez J, García-Klepizg JL, Andrès E, Zapatero-Gaviria A, Barba-Martin R, Marco-Martinez F, et al. Impact of Heart Failure on In-Hospital Outcomes after Surgical Femoral Neck Fracture Treatment. Journal of Clinical Medicine. 2021; 10(5):969. https://doi.org/10.3390/jcm10050969
Chicago/Turabian StyleMarco-Martínez, Javier, José Luis Bernal-Sobrino, Cristina Fernández-Pérez, Francisco Javier Elola-Somoza, Javier Azaña-Gómez, José Luis García-Klepizg, Emmanuel Andrès, Antonio Zapatero-Gaviria, Raquel Barba-Martin, Fernando Marco-Martinez, and et al. 2021. "Impact of Heart Failure on In-Hospital Outcomes after Surgical Femoral Neck Fracture Treatment" Journal of Clinical Medicine 10, no. 5: 969. https://doi.org/10.3390/jcm10050969
APA StyleMarco-Martínez, J., Bernal-Sobrino, J. L., Fernández-Pérez, C., Elola-Somoza, F. J., Azaña-Gómez, J., García-Klepizg, J. L., Andrès, E., Zapatero-Gaviria, A., Barba-Martin, R., Marco-Martinez, F., Canora-Lebrato, J., Lorenzo-Villalba, N., & Méndez-Bailón, M. (2021). Impact of Heart Failure on In-Hospital Outcomes after Surgical Femoral Neck Fracture Treatment. Journal of Clinical Medicine, 10(5), 969. https://doi.org/10.3390/jcm10050969







