Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Database
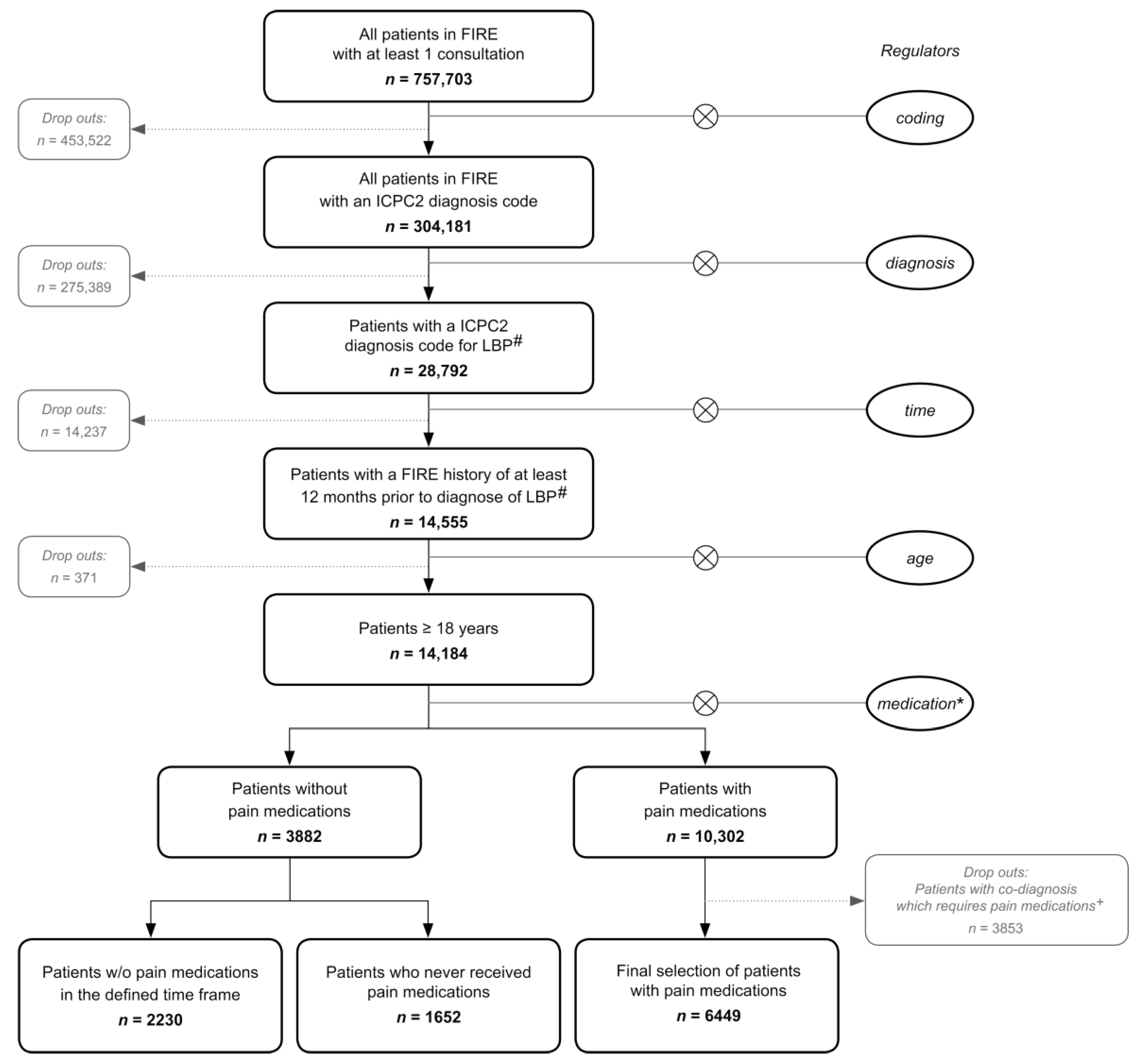
2.2. Inclusion Criteria
2.3. Study Variables
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Basic Characteristics
3.2. Prescribing Patterns
3.3. Time Patterns of Prescriptions
3.4. Regression Analysis: GP and Patient Characteristics Association
3.5. Co-Medications
4. Discussion
4.1. Pattern of Prescriptions
4.2. Time Pattern of the Prescriptions during Baseline and Follow-Up Period
4.3. Association with Pain Medication Prescriptions
4.4. Co-Medications and LBP
4.5. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [CrossRef]
- Donnoli, F.; Azari, M. Transition from acute to chronic low back pain; A biopsychosocial perspective. Chiropr. J. Aust. 2013, 43, 93–98. [Google Scholar]
- Di Iorio, D.; Henley, E.; Doughty, A. A survey of primary care physician practice patterns and adherence to acute low back problem guidelines. Arch. Fam. Med. 2000, 9, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Back-Report Switzerland 2020. Rheumaliga Schweiz Juli 2020. Available online: https://www.rheumaliga.ch/assets/doc/CH_Dokumente/blog/2020/rueckenreport-2020/Rueckenreport-2020.pdf (accessed on 25 March 2021).
- Health Statistics 2019. Swiss Federal Statistical Office. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/health.html (accessed on 25 March 2021).
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 2019, 39, 619–626. [Google Scholar] [CrossRef]
- Finley, C.R.; Chan, D.S.; Garrison, S.; Korownyk, C.; Kolber, M.R.; Campbell, S.; Eurich, D.T.; Lindblad, A.J.; Vandermeer, B.; Allan, G.M. What are the most common conditions in primary care? Systematic review. Can. Fam. Phys. 2018, 64, 832–840. [Google Scholar]
- Pengel, L.H.; Herbert, R.D.; Maher, C.G.; Refshauge, K.M. Acute low back pain: Systematic review of its prognosis. BMJ 2003, 327, 323. [Google Scholar] [CrossRef]
- Schers, H.; Braspenning, J.; Drijver, R.; Wensing, M.; Grol, R. Low back pain in general practice: Reported management and reasons for not adhering to the guidelines in The Netherlands. Br. J. Gen. Pract. 2000, 50, 640–644. [Google Scholar]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.C.; Chenot, J.F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef] [PubMed]
- Ivanova, J.I.; Birnbaum, H.G.; Schiller, M.; Kantor, E.; Johnstone, B.M.; Swindle, R.W. Real-world practice patterns, health-care utilization, and costs in patients with low back pain: The long road to guideline-concordant care. Spine J. 2011, 11, 622–632. [Google Scholar] [CrossRef] [PubMed]
- Bishop, P.B.; Wing, P.C. Knowledge transfer in family physicians managing patients with acute low back pain: A prospective randomized control trial. Spine J. 2006, 6, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Piccoliori, G.; Engl, A.; Gatterer, D.; Sessa, E.; in der Schmitten, J.; Abholz, H.-H. Management of low back pain in general practice—is it of acceptable quality: An observational study among 25 general practices in South Tyrol (Italy). BMC Fam. Pract. 2013, 14, 148. [Google Scholar] [CrossRef]
- Williams, C.M.; Maher, C.G.; Hancock, M.J.; McAuley, J.H.; McLachlan, A.J.; Britt, H.; Fahridin, S.; Harrison, C.; Latimer, J. Low back pain and best practice care: A survey of general practice physicians. Arch. Intern. Med. 2010, 170, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Morland, R. Evolution of the national opioid crisis. Nursing 2019, 49, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Belzak, L.; Halverson, J. The opioid crisis in Canada: A national perspective. Health Promot. Chronic Dis. Prev. Can. 2018, 38, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Mens, J.M. The use of medication in low back pain. Best Pract. Res. Clin. Rheumatol. 2005, 19, 609–621. [Google Scholar] [CrossRef] [PubMed]
- Kobus, A.M.; Smith, D.H.; Morasco, B.J.; Johnson, E.S.; Yang, X.; Petrik, A.F.; Deyo, R.A. Correlates of higher-dose opioid medication use for low back pain in primary care. J. Pain 2012, 13, 1131–1138. [Google Scholar] [CrossRef]
- Deyo, R.A.; Von Korff, M.; Duhrkoop, D. Opioids for low back pain. BMJ 2015, 350, g6380. [Google Scholar] [CrossRef]
- Higgins, C.; Smith, B.H.; Matthews, K. Incidence of iatrogenic opioid dependence or abuse in patients with pain who were exposed to opioid analgesic therapy: A systematic review and meta-analysis. Br. J. Anaesth 2018, 120, 1335–1344. [Google Scholar] [CrossRef]
- Volinn, E.; Fargo, J.D.; Fine, P.G. Opioid therapy for nonspecific low back pain and the outcome of chronic work loss. Pain 2009, 142, 194–201. [Google Scholar] [CrossRef]
- Ashworth, J.; Green, D.J.; Dunn, K.M.; Jordan, K.P. Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up? Pain 2013, 154, 1038–1044. [Google Scholar] [CrossRef]
- Chau, D.L.; Walker, V.; Pai, L.; Cho, L.M. Opiates and elderly: Use and side effects. Clin. Interv. Aging 2008, 3, 273–278. [Google Scholar] [CrossRef]
- Wilcox, C.M.; Cryer, B.; Triadafilopoulos, G. Patterns of use and public perception of over-the-counter pain relievers: Focus on nonsteroidal antiinflammatory drugs. J. Rheumatol. 2005, 32, 2218–2224. [Google Scholar]
- Enthoven, W.T.M.; Scheele, J.; Bierma-Zeinstra, S.M.A.; Bueving, H.J.; Bohnen, A.M.; Peul, W.C.; van Tulder, M.W.; Berger, M.Y.; Koes, B.W.; Luijsterburg, P.A.J. Analgesic Use in Older Adults with Back Pain: The BACE Study. Pain Med. 2014, 15, 1704–1714. [Google Scholar] [CrossRef]
- Chou, R.; Huffman, L.H. Medications for Acute and Chronic Low Back Pain: A Review of the Evidence for an American Pain Society/American College of Physicians Clinical Practice Guideline. Ann. Intern. Med. 2007, 147, 505–514. [Google Scholar] [CrossRef]
- Chou, R.; Qaseem, A.; Owens, D.K.; Shekelle, P. Clinical Guidelines Committee of the American College of Physicians. Diagnostic Imaging for Low Back Pain: Advice for High-Value Health Care from the American College of Physicians. Ann. Intern. Med. 2011, 154, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Smith, D.H.M.; Johnson, E.S.; Donovan, M.; Tillotson, C.J.; Yang, X.; Petrik, A.F.; Dobscha, S.K. Opioids for back pain patients: Primary care prescribing patterns and use of services. J. Am. Board Fam. Med. 2011, 24, 717–727. [Google Scholar] [CrossRef]
- Low back pain and sciatica in over 16s: Assessment and management (NICE guideline NG59) 2016 25.05.2020. Available online: https://www.nice.org.uk/guidance/ng59 (accessed on 25 March 2021).
- Stochkendahl, M.J.; Kjaer, P.; Hartvigsen, J.; Kongsted, A.; Aaboe, J.; Andersen, M.; Andersen, M.Ø.; Fournier, G.; Højgaard, B.; Jensen, M.B.; et al. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur. Spine J. 2018, 27, 60–75. [Google Scholar] [CrossRef]
- Mann, E.G.; Johnson, A.; Van Den Kerkhof, E.G. Frequency and characteristics of healthcare visits associated with chronic pain: Results from a population-based Canadian study. Can. J. Anaesth 2016, 63, 411–441. [Google Scholar] [CrossRef] [PubMed]
- Trottmann, M.; Frueh, M.; Telser, H.; Reich, O. Physician drug dispensing in Switzerland: Association on health care expenditures and utilization. BMC Health Serv. Res. 2016, 16, 238. [Google Scholar] [CrossRef] [PubMed]
- van Tulder, M.W.; Touray, T.; Furlan, A.D.; Solway, S.; Bouter, L.M. Muscle Relaxants for Nonspecific Low Back Pain: A Systematic Review Within the Framework of the Cochrane Collaboration. Spine (Phila Pa 1976) 2003, 28, 1978–1992. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, D.M.; Hoving, J.L.; Assendelft, W.W.; Roland, M.; van Tulder, M.W. Antidepressants for non-specific low back pain. Cochrane Database Syst. Rev. 2008, 2008, Cd001703. [Google Scholar] [CrossRef]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The association of sleep and pain: An update and a path forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef] [PubMed]
- Alsaadi, S.M.; McAuley, J.H.; Hush, J.M.; Maher, C.G. Prevalence of sleep disturbance in patients with low back pain. Eur. Spine J. 2011, 20, 737–743. [Google Scholar] [CrossRef]
- Lanza, F.L.; Chan, F.K.; Quigley, E.M. Guidelines for prevention of NSAID-related ulcer complications. Am. J. Gastroenterol. 2009, 104, 728–738. [Google Scholar] [PubMed]
- Schmidt, C.O.; Raspe, H.; Pfingsten, M.; Hasenbring, M.; Basler, H.D.; Eich, W.; Kohlmann, T. Back pain in the German adult population: Prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine 2007, 32, 2005–2011. [Google Scholar] [CrossRef] [PubMed]
- Raspe, H. Rückenschmerzen. Gesundheitsberichterstattung des Bundes [Internet] 2012 May 2020, 53. Available online: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsT/rueckenschmerzen.pdf?__blob=publicationFile (accessed on 25 March 2021).

| Variables | All Patients | Back Syndrome with Radiating Pain | Back Syndrome without Radiating Pain | Low Back Symptom/Complaint | Combination of Symptoms 1 | p |
|---|---|---|---|---|---|---|
| Number of patients, n | 10,331 | 1758 | 2465 | 5663 | 445 | |
| Number of consultations per patient, mean (SD2; range (min–max)) | 2.12 (3.25; (1–63)) | 2.58 (3.74; (1–43)) | 1.89 (2.74; (1–41)) | 2.01 (3.25; (1–63)) | 2.83 (3.53; (1–28)) | <0.001 |
| Age, mean (SD, range (min–max)) | 51.66 (18.24; (18–100)) | 56.52 (17.25; (18–97)) | 49.38 (18.32; (18–97)) | 51.01 (18.31; (18–100)) | 53.41 (17.14; (18–93)) | 0.005 |
| Sex | <0.001 | |||||
| male, n (%) | 5042 (48.8) | 835 (47.5) | 1271 (51.6) | 2709 (47.8) | 227 (51.0) | |
| female, n (%) | 5289 (51.2) | 923 (52.5) | 1194 (48.4) | 2954 (52.2) | 218 (49.0) |
| Variables | Total | Back Syndrome with Radiating Pain | Back Syndrome without Radiating Pain | Low Back Symptom/Complaint | Combination of Symptoms | p |
|---|---|---|---|---|---|---|
| n1 = 10,331 | n = 1758 | n = 2465 | n = 5663 | n = 445 | ||
| A—Basic prescribing patterns 2 | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Patients without any pain medication | 3882 (37.6) | 588 (33.4) | 814 (33.0) | 2360 (41.7) | 120 (27.0) | <0.001 |
| Patients with at least one pain medication | 6449 (62.4) | 1170 (66.6) | 1651 (67.0) | 3303 (58.3) | 325 (73.0) | <0.001 |
| Patients with one pain medication | 3826 (37.0) | 614 (34.9) | 1071 (75.7) | 1992 (35.2) | 149 (33.5) | <0.001 |
| Patients with two or more pain medications | 2623 (25.4) | 556 (31.6) | 580 (23.5) | 1311 (23.2) | 176 (39.6) | <0.001 |
| Patients in which the first prescribed pain medication after or at diagnosis was | ||||||
| NSAID | 2813 (27.2) | 465 (26.5) | 813 (33.0) | 1408 (24.9) | 127 (28.5) | <0.001 |
| Opioid | 505 (4.9) | 132 (7.5) | 104 (4.2) | 221 (3.9) | 48 (10.8) | <0.001 |
| Paracetamol | 853 (8.3) | 118 (6.7) | 153 (6.2) | 528 (9.3) | 54 (12.1) | <0.001 |
| B—Specific prescribing patterns 3 | ||||||
| NSAID | ||||||
| Patients receiving NSAIDs | 5545 (86.0) | 1014 (86.7) | 1478 (89.5) | 2779 (84.1) | 274 (84.3) | <0.001 |
| Patients receiving only NSAIDs | 3088 (47.9) | 514 (43.9) | 966 (58.5) | 1509 (45.7) | 99 (30.5) | <0.001 |
| Opioids | ||||||
| Patients receiving opioids | 1417 (22.0) | 367 (31.4) | 278 (16.8) | 652 (19.7) | 120 (36.9) | <0.001 |
| Patients receiving only opioids | 178 (2.8) | 44 (3.8) | 38 (2.3) | 81 (2.5) | 15 (4.6) | 0.033 |
| Paracetamol | ||||||
| Patients receiving paracetamol | 2544 (39.4) | 441 (37.7) | 512 (31.0) | 1439 (43.6) | 152 (46.8) | <0.001 |
| Patients receiving only paracetamol | 602 (9.3) | 89 (7.6) | 115 (7.0) | 372 (11.3) | 26 (8.0) | <0.001 |
| Combination therapies | ||||||
| Patients receiving NSAIDs and paracetamol | 1342 (20.8) | 200 (17.1) | 292 (17.7) | 770 (23.3) | 80 (24.6) | <0.001 |
| Patients receiving NSAIDs and opioids | 639 (9.9) | 171 (14.6) | 135 (8.2) | 274 (8.3) | 59 (18.2) | <0.001 |
| Patients receiving NSAIDs, opioids and paracetamol | 476 (7.4) | 129 (11.0) | 85 (5.1) | 226 (6.8) | 36 (11.1) | <0.001 |
| Patients receiving opioids and paracetamol | 124 (1.9) | 23 (2.0) | 20 (1.2) | 71 (2.1) | 10 (3.1) | 0.068 |
| C—Timing 4 | ||||||
| Time from diagnosis to first NSAID prescription | 8.71 (30.11) | 8.38 (28.82) | 8.53 (30.59) | 8.76 (29.95) | 10.41 (33.59) | 0.966 |
| Time from diagnosis to first Opioid prescription | 7.53 (25.14) | 6.61 (21.95) | 7.51 (26.45) | 6.24 (23.11) | 16.04 (36.31) | 0.903 |
| Time from diagnosis to first paracetamol prescription | 13.13 (37.13) | 11.78 (33.68) | 14.80 (36.27) | 13.42 (38.84) | 8.56 (29.23) | 0.807 |
| Outcome | Prescription of Any Pain Medication | NSAID | Opioid | Paracetamol | |||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor (Reference, Where Applicable) | Number of Patients/GP | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| GP characteristics | |||||||||
| Age 1 (continuous) | n = 9825, GP = 161 | 0.99 (0.98, 1.01) | 0.195 | 0.98 (0.96, 0.99) | 0.007 | ||||
| 0.97 (0.95, 0.99) | <0.001 | ||||||||
| Age (age ≤ 55) | 1.07 (0.90, 1.26) | 0.450 | 1.00 (0.83, 1.20) | 0.988 | |||||
| 0.84 (0.66, 1.06) | 0.132 | ||||||||
| Male gender (female) | n = 10252, GP = 178 | 1.67 (1.11, 2.5) | 0.014 | 1.86 (1.25, 2.77) | 0.002 | 1.38 (0.92, 2.07) | 0.118 | 1.27 (0.88, 1.85) | 0.206 |
| 1.32 (0.92, 1.90) | 0.130 | ||||||||
| Type of practice (single practice) Double practice | n = 10331, GP = 180 | 1.13 (0.40, 3.19) | 0.820 | 1.27 (0.46, 3.51) | 0.647 | 1.35 (0.54, 3.34) | 0.521 | 1.10 (0.45, 2.65) | 0.838 |
| Group practice | 1.25 (0.67, 2.35) | 0.487 | 1.19 (0.64, 2.20) | 0.579 | 1.00 (0.57, 1.76) | 1.000 | 1.12 (0.66, 1.92) | 0.668 | |
| Years in practice | n = 9731, GP = 148 | 0.99 (0.98, 1.01) | 0.431 | 0.99 (0.98, 1.01) | 0.882 | 0.98 (0.97, 1.00) | 0.050 | 0.99 (0.97, 1.00) | 0.077 |
| 0.98 (0.96, 1.00) | 0.012 | ||||||||
| Self-Employed (employee) | n = 9978, GP = 161 | 3.03 (2.04, 4.51) | <0.001 | 3.13 (2.13, 4.60) | <0.001 | 2.59 (1.67, 4.03) | <0.001 | 1.71 (1.16, 2.52) | 0.007 |
| 2.36 (1.64, 3.40) | <0.001 | 2.38 (1.63, 3.47) | <0.001 | 2.34 (1.50, 3.63) | <0.001 | 1.56 (1.07, 2.28) | 0.020 | ||
| Employment level (100%) <50% | n = 8938, GP = 143 | 0.41 (0.20, 0.84) | 0.016 | 0.52 (0.26, 1.06) | 0.073 | 0.42 (0.19, 0.91) | 0.028 | 0.57 (0.29, 1.11) | 0.098 |
| 50–79% | 0.55 (0.34, 0.87) | 0.010 | 0.56 (0.36, 0.88) | 0.013 | 0.59 (0.37, 0.94) | 0.025 | 0.72 (0.48, 1.08) | 0.113 | |
| 80–99% | 0.82 (0.51, 1.34) | 0.437 | 0.90 (0.56, 1.44) | 0.666 | 0.70 (0.44, 1.11) | 0.132 | 0.95 (0.63, 1.45) | 0.822 | |
| Self-dispensing (yes) No | n = 10311, GP = 175 | 1.98 (1.29, 3.05) | 0.002 | 2.00 (1.32, 3.04) | 0.001 | 1.21 (0.83, 1.78) | 0.315 | 1.44 (0.97, 2.14) | 0.070 |
| 1.76 (1.22, 2.52) | 0.002 | 1.79 (1.26, 2.55) | 0.001 | ||||||
| Patient characteristics | |||||||||
| Age at diagnosis > 50 (≤50) years old | n = 10331, GP = 180 | 0.83 (0.76, 0.91) | <0.001 | 1.11 (1.01, 1.21) | 0.024 | 0.52 (0.46, 0.59) | <0.001 | 0.72 (0.65, 0.79) | <0.001 |
| 1.24 (1.13, 1.36) | <0.001 | 0.66 (0.58, 0.76) | <0.001 | 0.84 (0.75, 0.93) | 0.001 | ||||
| Male gender (female) | n = 10331, GP = 180 | 1.07 (0.97, 1.16) | 0.167 | 1.17 (1.08, 1.28) | <0.001 | 0.99 (0.88, 1.12) | 0.912 | 0.79 (0.72, 0.87) | <0.001 |
| 1.10 (1.00, 1.21) | 0.044 | 1.20 (1.09, 1.31) | <0.001 | 0.82 (0.74, 0.90) | <0.001 | ||||
| Number of consultations after diagnosis | n = 10331, GP = 180 | 2.21 (2.05 2.39) | <0.001 | 1.24 (1.2 1.27) | <0.001 | 1.24 (1.22, 1.27) | <0.001 | 1.24 (1.21, 1.27) | <0.001 |
| 2.20 (2.04, 2.37) | <0.001 | 1.27 (1.23, 1.31) | <0.001 | 1.27 (1.24, 1.30) | <0.001 | 1.25 (1.22, 1.28) | <0.001 | ||
| Diagnosis Code 2 (Back syndrome with radiating pain) Low back symptom/complaint | n = 9886, GP = 179 | 0.88 (0.76, 1.01) | 0.065 | 0.92 (0.81, 1.06) | 0.257 | 0.92 (0.81, 1.06) | 0.257 | 0.81 (0.70, 0.94) | 0.005 |
| Back syndrome without radiating pain | 1 (0.86, 1.17) | 0.964 | 1.03 (0.89, 1.19) | 0.726 | 1.03 (0.89, 1.19) | 0.726 | 0.86 (0.74, 1.02) | 0.076 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Gangi, S.; Pichierri, G.; Zechmann, S.; Rosemann, T.; Plate, A. Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis. J. Clin. Med. 2021, 10, 1366. https://doi.org/10.3390/jcm10071366
Di Gangi S, Pichierri G, Zechmann S, Rosemann T, Plate A. Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis. Journal of Clinical Medicine. 2021; 10(7):1366. https://doi.org/10.3390/jcm10071366
Chicago/Turabian StyleDi Gangi, Stefania, Giuseppe Pichierri, Stefan Zechmann, Thomas Rosemann, and Andreas Plate. 2021. "Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis" Journal of Clinical Medicine 10, no. 7: 1366. https://doi.org/10.3390/jcm10071366
APA StyleDi Gangi, S., Pichierri, G., Zechmann, S., Rosemann, T., & Plate, A. (2021). Prescribing Patterns of Pain Medications in Unspecific Low Back Pain in Primary Care: A Retrospective Analysis. Journal of Clinical Medicine, 10(7), 1366. https://doi.org/10.3390/jcm10071366








