Ibero-American Society of Interventionism (SIDI) and the Spanish Society of Vascular and Interventional Radiology (SERVEI) Standard of Practice (SOP) for the Management of Inferior Vena Cava Filters in the Treatment of Acute Venous Thromboembolism
Abstract
:1. Introduction
2. Material and Methods
3. Results
3.1. Interventional Radiologist Participation in the Development of Multidisciplinary Clinical Guidelines in the Management of Inferior Vena Cava Filters
3.2. Compliance with the Current Clinical Guidelines
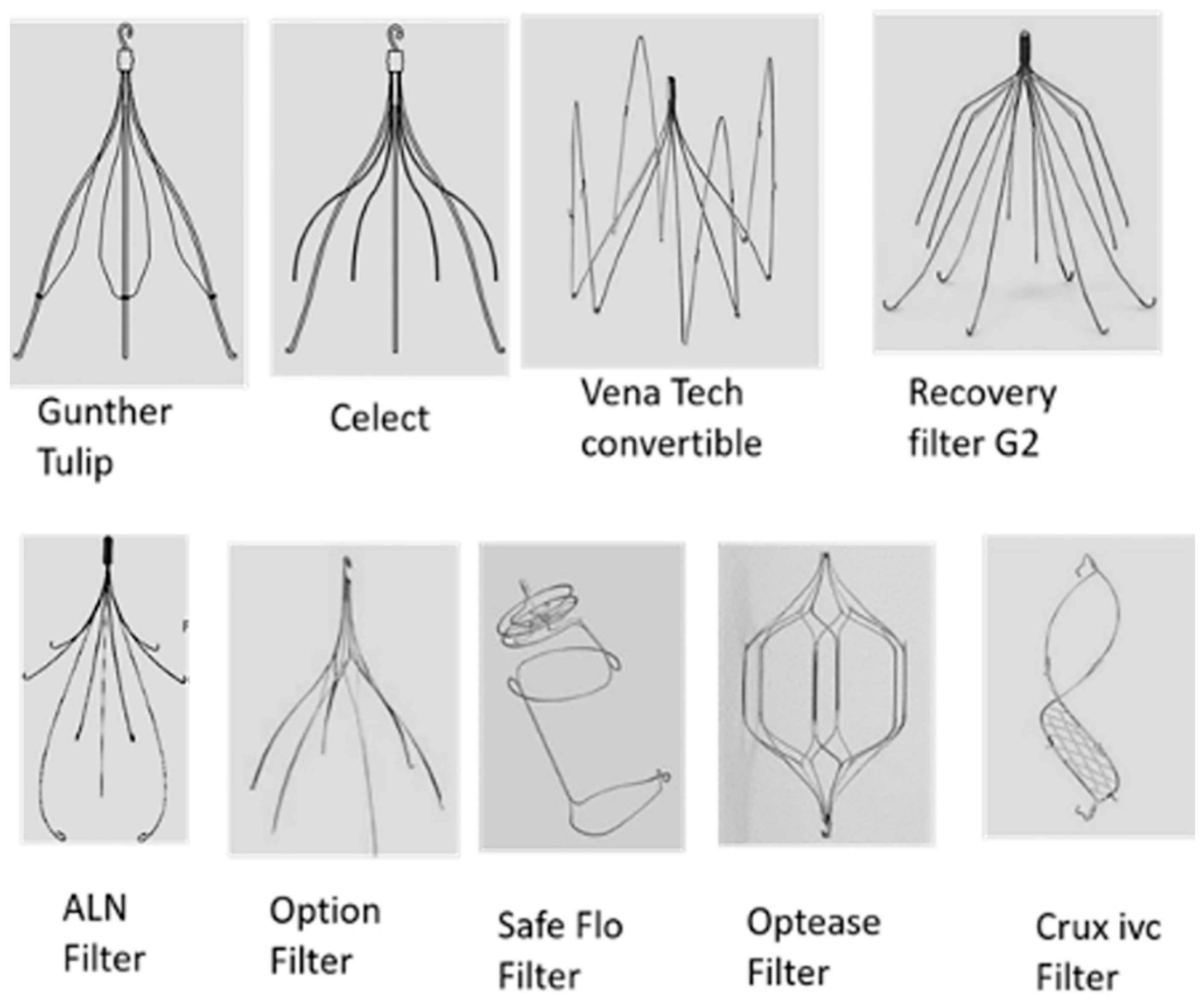
3.3. Venous Flow Interruption in IVC and Types of Filters
3.4. Safety and Efficacy of IVC Filters for Acute VTE
3.5. Indications and Contraindications Placement of IVCF
3.5.1. Absolute Indication for Placement of Inferior Vena Cava Filters
3.5.2. Relative Indication for the Placement of Inferior Vena Cava Filters
Filter Placement in Hemodynamically Unstable Patients with VTE
Filter Placement in Recurrent PE or Chronic PE
Placement of IVCF before CDT in Proximal DVT
Prophylactic Indication for the Placement of Inferior Vena Cava Filters
4. Contraindications
5. Removal of Retrievable Inferior Vena Cava Filters
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACT | Anticoagulation therapy |
| ACCP | American College of Chest Physicians |
| ACR | American College of Radiology |
| AHA | American Heart Association |
| PE | Pulmonary embolism |
| ESC | European Society of Cardiology |
| VTE | Venous thromboembolism |
| IVCF | Inferior vena cava filters |
| MAUDE | Manufacturer and User Facility Device Experience |
| NIH | National Institute of Heath |
| DVT | Deep venous thrombosis |
| SIR | Society of Interventional Radiology |
| SIDI | Iberoamerican Interventional Society |
| SERVEI | Spanish Society of Vascular and Interventional Radiology |
| SEPAR | Spanish Society for Pneumology and Thoracic Surgery |
| US FDA | US Food and Drug Administration |
| IVC | Inferior vena cava |
| CDT | Catheter-directed treatment |
| IRs | Interventional radiologists |
References
- Aycock, K.I.; Campbell, R.L.; Lynch, F.C.; Manning, K.B.; Craven, B.A. Computational predictions of the embolus-trapping performance of an IVC filter in patient-specific and idealized IVC geometries. Biomech. Model. Mechanobiol. 2017, 16, 1957–1969. [Google Scholar] [CrossRef] [PubMed]
- Decousus, H.; Leizorovicz, A.; Parent, F.; Page, Y.; Tardy, B.; Girard, P.; Laporte, S.; Faivre, R.; Charbonnier, B.; Barral, F.-G.; et al. A Clinical Trial of Vena Caval Filters in the Prevention of Pulmonary Embolism in Patients with Proximal Deep-Vein Thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N. Engl. J. Med. 1998, 338, 409–416. [Google Scholar] [CrossRef]
- Kaufman, J.A.; Rundback, J.H.; Kee, S.T.; Geerts, W.; Gillespie, D.; Kahn, S.R.; Kearon, C.; Rectenwald, J.; Rogers, F.B.; Stavropoulos, S.W.; et al. Development of a Research Agenda for Inferior Vena Cava Filters: Proceedings from a Multidisciplinary Research Consensus Panel. J. Vasc. Interv. Radiol. JVIR 2009, 20, 697–707. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.J.; Harjola, V.P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur. Heart J. 2020, 41, 543–603. [Google Scholar] [CrossRef] [PubMed]
- Cushman, M.; Barnes, G.D.; Creager, M.A.; Diaz, J.A.; Henke, P.K.; Machlus, K.R.; Nieman, M.T.; Wolberg, A.S. Venous Thromboembolism Research Priorities: A Scientific Statement From the American Heart Association and the International Society on Thrombosis and Haemostasis. Circulation 2020, 142, e85–e94. [Google Scholar] [CrossRef] [PubMed]
- Endovascular TODAY. IVC Filter Placement: Is Intersociety Consensus Possible? Available online: https://evtoday.com/articles/2019-july/ivc-filter-placement-is-intersociety-consensus-possible (accessed on 9 December 2021).
- Ahmed, O.; Sheikh, S.; Tran, P.; Funaki, B.; Shadid, A.M.; Navuluri, R.; Van Ha, T. Inferior Vena Cava Filter Evaluation and Management for the Diagnostic Radiologist: A Comprehensive Review Including Inferior Vena Cava Filter-Related Complications and PRESERVE Trial Filters. Can. Assoc. Radiol. J. 2019, 70, 367–382. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, O.; Wadhwa, V.; Patel, K.; Patel, K.; Lionberg, A.; Klejch, W.; Lizardo, A.; Ginsburg, M. Rising Retrieval Rates of Inferior Vena Cava Filters in the United States: Insights From the 2012 to 2016 Summary Medicare Claims Data. J. Am. Coll. Radiol. JACR 2018, 15, 1553–1557. [Google Scholar] [CrossRef]
- Jaff, M.R.; Mc Murtry, M.A.; Archer, S.L.; Cusmhman, M.; Goldenberg, N.; Golhaber, S.Z.; Jenkins, J.S.; Kline, J.A.; Michaels, A.D.; Zieler, B.; et al. Management of Massive and Submassive Pulmonary Embolism, Iliofemoral Deep Vein Thrombosis, and Chronic Thromboembolic Pulmonary Hypertension. Circulation 2011, 123, 1788–1830. [Google Scholar] [CrossRef] [Green Version]
- Uresandi, F.; Monreal, M.; García-Bragado, F.; Domenech, P.; Lecumberri, R.; Escribano, P.; Zamorano, J.L.; Jiménez, S.; Ruiz-Artacho, P.; Lozano, F.; et al. National Consensus on the Diagnosis, Risk Stratification and Treatment of Patients with Pulmonary Embolism. Spanish Society of Pneumology and Thoracic Surgery (SEPAR). Society Española Internal Medicine (SEMI). Spanish Society of Thrombosis and Haemostasi. Arch. Bronconeumol. 2013, 49, 534–547. [Google Scholar] [CrossRef]
- Howard, L.S.G.E.; Barden, S.; Condliffe, R.; Connolly, V.; Davies, C.W.H.; Donaldson, J.; Everett, B.; Free, C.; Horner, D.; Hunter, L.; et al. British Thoracic Society Guideline for the initial outpatient management of pulmonary embolism (PE). Thorax 2018, 73, ii1–ii29. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.A.; Barnes, G.D.; Chaer, R.A.; Cuschieri, J.; Eberhardt, R.T.; Johnson, M.S.; Kuo, W.T.; Murin, S.; Patel, S.; Rajasekhar, A.; et al. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest P. J. Vasc. Interv. Radiol. JVIR 2020, 31, 1529–1544. [Google Scholar] [CrossRef]
- Minocha, J.; Smith, A.M.; Kapoor, B.S.; Fidelman, N.; Cain, T.R.; Caplin, D.M.; Eldrup-Jorgensen, J.; Farsad, K.; Gupta, A.; Lee, M.H.; et al. ACR Appropriateness Criteria® Radiologic Management of Venous Thromboembolism-Inferior Vena Cava Filters. J. Am. Coll. Radiol. JACR 2019, 16, S214–S226. [Google Scholar] [CrossRef] [Green Version]
- Mismetti, P.; Laporte, S.; Pellerin, O.; Ennezat, P.V.; Couturaud, F.; Elias, A.; Falvo, N.; Meneveau, N.; Quere, I.; Roy, P.M.; et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: A randomized clinical trial. JAMA 2015, 313, 1627–1635. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Munger, H.; Brower, S.; O’Donell, M.; Crowther, M.; Cook, D.; Guyatt, G. Methodology for guideline development for the Seventh American College of Chest Physicians Conference on Antithrombotic and Thrombolytic Therapy: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004, 126, 174S–178S. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.A.; Kinney, T.B.; Streiff, M.B.; Sing, R.F.; Proctor, M.C.; Becker, D.; Cipolle, M.; Comerota, A.J.; Millward, S.F.; Rogers, F.B.; et al. Guidelines for the use of retrievable and convertible vena cava filters: Report from the Society of Interventional Radiology multidisciplinary consensus conference. J. Vasc. Interv. Radiol. JVIR 2006, 17, 449–459. [Google Scholar] [CrossRef]
- Greenfield, L.J.; Proctor, M.C. Vena caval filters for the prevention of pulmonary embolism. N. Engl. J. Med. 1998, 339, 47–48. [Google Scholar]
- Spencer, F.A.; Bates, S.M.; Goldberg, R.J.; Lessard, D.; Emery, C.; Glushchenko, A.; Gore, J.M.; White, R.H. A population-based study of inferior vena cava filters in patients with acute venous thromboembolism. Arch. Intern. Med. 2010, 170, 1456–1462. [Google Scholar] [CrossRef] [Green Version]
- Baadh, A.S.; Zikria, J.F.; Rivoli, S.; Graham, R.E.; Javit, D.; Ansell, J.E. Indications for inferior vena cava filter placement: Do physicians comply with guidelines? J. Vasc. Interv. Radiol. JVIR 2012, 23, 989–995. [Google Scholar] [CrossRef]
- DeYoung, E.; Minocha, J. Inferior Vena Cava Filters: Guidelines, Best Practice, and Expanding Indications. Semin. Intervent. Radiol. 2016, 33, 65–70. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.A. Inferior Vena Cava Filters: Current and Future Concepts. Interv. Cardiol. Clin. 2018, 7, 129–135. [Google Scholar] [CrossRef]
- Eggers, M.D.; McArthur, M.J.; Figueira, T.A.; Abdelsalam, M.E.; Dixon, K.P.; Pageon, L.R.; Wallace, M.J.; Huang, S.Y. Pilot in vivo study of an absorbable polydioxanone vena cava filter. J. Vasc. Surg. Venous Lymphat. Disord. 2015, 3, 409–420. [Google Scholar] [CrossRef]
- Dake, M.D.; Ansel, G.M.; Johnson, M.S.; Mendes, R.; Smouse, H.B. The Clinical Rationale for the Sentry Bioconvertible Inferior Vena Cava Filter for the Prevention of Pulmonary Embolism. Int. J. Vasc. Med. 2019, 2019, 5795148. [Google Scholar] [CrossRef] [Green Version]
- Stein, P.D.; Kayali, F.; Olson, R.E. Twenty-one-year trends in the use of inferior vena cava filters. Arch. Intern. Med. 2004, 164, 1541–1545. [Google Scholar] [CrossRef] [Green Version]
- Streiff, M.B. Vena caval filters: A comprehensive review. Blood 2000, 95, 3669–3677. [Google Scholar] [CrossRef]
- Billett, H.H.; Jacobs, L.G.; Madsen, E.M.; Giannattasio, E.R.; Mahesh, S.; Cohen, H.W. Efficacy of inferior vena cava filters in anticoagulated patients. J. Thromb. Haemost. JTH 2007, 5, 1848–1853. [Google Scholar] [CrossRef]
- Group, P.S. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: The PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation 2005, 112, 416–422. [Google Scholar] [CrossRef] [Green Version]
- Duffett, L.; Carrier, M. Inferior vena cava filters. J. Thromb. Haemost JTH 2017, 15, 3–12. [Google Scholar] [CrossRef]
- Arous, E.J.; Messina, L.M. Temporary inferior vena cava filters: How do we move forward? Chest 2016, 149, 1143–1145. [Google Scholar] [CrossRef] [Green Version]
- Streiff, M.B.; Agnelli, G.; Connors, J.M.; Crowther, M.; Eichinger, S.; Lopes, R.; McBane, R.D.; Moll, S.; Ansell, J. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J. Thromb. Thrombolysis 2016, 41, 32–67. [Google Scholar] [CrossRef] [Green Version]
- Angel, L.F.; Tapson, V.; Galgon, R.E.; Restrep, M.I.; Kaufman, J.A. Systematic review of the use of retrievable inferior vena cava filters. J. Vasc. Interv. Radiol. JVIR 2011, 22, 1522–1530. [Google Scholar] [CrossRef]
- Nicolaides, A.; Hull, R.D.; Fareed, J. Inferior vena cava filters. Clin. Appl. Thromb. Off. J. Int. Acad. Clin. Appl. Thromb. 2013, 19, 204–205. [Google Scholar] [CrossRef]
- Achaibar, K.; Waldmann, C.; Taccone, F.S. The Angel catheter for the prevention of pulmonary embolism: Combining an IVC filter and a triple-lumen central venous catheter. Expert Rev. Med. Devices 2019, 16, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Serednicki, W.; Dobrowolska, E.; Kałuża, K.; Kopacz, M.; Wordliczek, J. Angel(®) Catheter use for pulmonary embolism prophylaxis in a polytrauma patient. Injury 2015, 46, 1167–1170. [Google Scholar] [CrossRef]
- Taccone, F.S.; Bunker, N.; Waldmann, C.; De Backer, D.; Brohi, K.; Jones, R.G.; Vincent, J.L. A new device for the prevention of pulmonary embolism in critically ill patients: Results of the European Angel Catheter Registry. J. Trauma Acute Care Surg. 2015, 79, 456–462. [Google Scholar] [CrossRef]
- Matusov, Y.; Weinberg, A.S.; Liang, R.; Meza, J.; Friedman, O.; Tapson, V.F. Use of the Bedside-Placed Angel Catheter IVC Filter for Venous Thromboembolic Disease in Critically Ill Medical Patients. J. Intensive Care Med. 2020, 35, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.R.; Tun, J.K.; Alchanan, R.; Jaffer, O.; Patel, S.; Chun, J.Y.; Bunker, N.; Fotheringham, T. Broken Wings: First Reported Cases of Fractured Angel® Catheters, a Temporary Combined Femoral Venous Catheter and Retrievable IVC Filter Device. Cardiovasc. Intervent. Radiol. 2018, 41, 1128–1133. [Google Scholar] [CrossRef] [PubMed]
- Ha, C.P.; Rectenwald, J.E. Inferior Vena Cava Filters: Current Indications, Techniques, and Recommendations. Surg. Clin. N. Am. 2018, 98, 293–319. [Google Scholar] [CrossRef]
- Chuu, W.M.; Wang, N.Y.; Perry, D. Vena caval filters for the prevention of pulmonary embolism. N. Engl. J. Med. 1998, 339, 47–48. [Google Scholar] [CrossRef] [Green Version]
- Murphy, T.P.; Trerotola, S.O.; Vogelzang, R.L. Vena caval filters for the prevention of pulmonary embolism. N. Engl. J. Med. 1998, 339, 46–48. [Google Scholar]
- Young, T.; Sriram, K.B. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst. Rev. 2020, 10, CD006212. [Google Scholar] [CrossRef] [PubMed]
- Health C for D and R Safety Communications—Removing Retrievable Inferior Vena Cava Filters: FDA Safety Communication. Available online: https://2wt0853vtha23hf7qg2rwk3g-wpengine.netdna-ssl.com/wp-content/uploads/2017/12/Removing-Retrievable-Inferior-Vena-Cava-Filters.pdf (accessed on 9 December 2021).
- Jia, Z.; Wu, A.; Tam, M.; Spain, J.; McKinney, J.M.; Wang, W. Caval Penetration by Inferior Vena Cava Filters: A Systematic Literature Review of Clinical Significance and Management. Circulation 2015, 132, 944–952. [Google Scholar] [CrossRef]
- Muriel, A.; Jiménez, D.; Aujesky, D.; Bertoletti, L.; Decousus, H.; Laporte, S.; Mismetti, P.; Muñoz, F.J.; Yusen, R.; Monreal, M.; et al. Survival effects of inferior vena cava filter in patients with acute symptomatic venous thromboembolism and a significant bleeding risk. J. Am. Coll. Cardiol. 2014, 63, 1675–1683. [Google Scholar] [CrossRef] [Green Version]
- Mellado, M.; Pijoan, J.I.; Jiménez, D.; Muriel, A.; AUsjesky, D.; Bertoletti, L.; Decousus, H.; Barrios, D.; Clara, A.; Yusen, R.D.; et al. Outcomes Associated With Inferior Vena Cava Filters Among Patients With Thromboembolic Recurrence During Anticoagulant Therapy. JACC Cardiovasc. Interv. 2016, 9, 2440–2448. [Google Scholar] [CrossRef] [PubMed]
- Rajasekhar, A.; Streiff, M.B. Vena cava filters for management of venous thromboembolism: A clinical review. Blood Rev. 2013, 27, 225–241. [Google Scholar] [CrossRef]
- De Gregorio, M.A.; Guirola, J.A.; Serrano, C.; Figueredo, A.; Kuo, W.T.; Quezada, C.A.; Jimenez, D. Success in Optional Vena Cava Filter Retrieval. An Analysis of 246 Patients. Arch. Bronconeumol. 2018, 54, 371–377. [Google Scholar] [CrossRef]
- Ortel, T.L.; Neumann, I.; Ageno, W.; Beyth, R.; Clark, N.P.; Cuker, A.; Hutten, B.A.; Jaff, M.R.; Manja, V.; Schulman, S.; et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: Treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. 2020, 4, 4693–4738. [Google Scholar] [CrossRef]
- Sharifi, M.; Bay, C.; Skrocki, L.; Lawson, D.; Mazdeh, S. Role of IVC filters in endovenous therapy for deep venous thrombosis: The FILTER-PEVI (filter implantation to lower thromboembolic risk in percutaneous endovenous intervention) trial. Cardiovasc. Interv. Radiol. 2012, 35, 1408–1413. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Kim, H.; Hwang, J.; Kim, S.D.; Park, S.C.; Kim, J.I.; Won, Y.S.; Youn, S.S.; Moon, I.S. Efficacy of Retrievable Inferior Vena Cava Filter Placement in the Prevention of Pulmonary Embolism during Catheter-Directed Thrombectomy for Proximal Lower-Extremity Deep Vein Thrombosis. Ann. Vasc. Surg. 2016, 33, 181–186. [Google Scholar] [CrossRef]
- Jiang, J.; Tu, J.; Jia, Z.; Cao, H.; Meng, Q.; Fuller, T.A.; Tian, F. Incidence and Outcomes of Inferior Vena Cava Filter Thrombus during Catheter-directed Thrombolysis for Proximal Deep Venous Thrombosis. Ann. Vasc. Surg. 2017, 38, 305–309. [Google Scholar] [CrossRef]
- Stawicki, S.P.; Sims, C.; Sharma, R.; Wege, N.S.; Truitt, M.; Cipolla, J.; Schrag, S.P.; Lorenzo, M.; El Chaar, M.; Torigian, D.A.; et al. Vena cava filters: A synopsis of complications and related topics. J. Vasc. Access 2008, 9, 102–110. [Google Scholar] [CrossRef]
- Lorch, H.; Welger, D.; Wagner, V.; Hillner, B.; Strecker, E.P.; Herrmann, H.; Voshage, G.; Zur, C.; Schwarzbach, C.; Schröder, J.; et al. Current practice of temporary vena cava filter insertion: A multicenter registry. J. Vasc. Interv. Radiol. JVIR 2000, 11, 83–88. [Google Scholar] [CrossRef]
- Ayad, M.T.; Gillespie, D.L. Long-term complications of inferior vena cava filters. J. Vasc. Surg. Venous Lymphat. Disord. 2019, 7, 139–144. [Google Scholar] [CrossRef]
- Wang, S.L.; Siddiqui, A.; Rosenthal, E. Long-term complications of inferior vena cava filters. J. Vasc. Surg. Venous Lymphat. Disord. 2017, 5, 33–41. [Google Scholar] [CrossRef]
- De Gregorio, M.A.; Guirola, J.A.; Urbano, J.; Díaz-Lorenzo, I.; Muñoz, J.J.; Villacastin, E.; Lopez-Medina, A.; Figueredo, A.L.; Guerrero, J.; Sierre, S.; et al. Spanish multicenter real—Life registry of retrievable vena cava filters (REFiVeC). CVIR Endovasc. 2020, 3, 26. [Google Scholar] [CrossRef]
- Uberoi, R.; Tapping, C.R.; Chalmers, N.; Allgar, V. British Society of Interventional Radiology (BSIR) Inferior Vena Cava (IVC) Filter Registry. Cardiovasc. Interv. Radiol. 2013, 36, 1548–1561. [Google Scholar] [CrossRef] [Green Version]
- Lee, M.J.; Valenti, D.; de Gregorio, M.A.; Minocha, J.; Rimon, U.; Pellerin, O. The CIRSE Retrievable IVC Filter Registry: Retrieval Success Rates in Practice. Cardiovasc. Interv. Radiol. 2015, 38, 1502–1507. [Google Scholar] [CrossRef] [PubMed]
- Morales, J.P.; Li, X.; Irony, T.Z.; Ibrahim, N.G.; Moynahan, M.; Cavanaugh, K.J., Jr. Decision analysis of retrievable inferior vena cava filters in patients without pulmonary embolism. J Vasc Surg. Venous Lymphat. Disord. 2013, 1, 376–384. [Google Scholar] [CrossRef]
- Baschera, D.; Sebunya, J.; Zellweger, R. Who is responsible for the removal of inferior vena cava filters? Unfallchirurg 2012, 115, 541–543. [Google Scholar] [CrossRef] [PubMed]
- Irwin, E.; Byrnes, M.; Schultz, S.; Chipman, J.; Beal, A.; Ahrendt, M.; Beilman, G.; Croston, J.K. A systematic method for follow-up improves removal rates for retrievable inferior vena cava filters in a trauma patient population. J. Trauma 2010, 69, 866–869. [Google Scholar] [CrossRef]
- Rottenstreich, A.; Arad, A.; Lev Cohain, N.; Bloom, A.I.; Varon, D.; Klimov, A.; Roth, B.; Kalish, Y. Implementation of an institutional protocol to improve inferior vena cava utilization and outcomes. J. Thromb. Thrombolysis 2017, 44, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Jaberi, A.; Tao, M.J.; Eisenberg, N.; Tan, K.; Roche-Nagle, G. IVC filter removal after extended implantation periods. Surg. J. R. Coll. Surg. Edinb. Irel. 2020, 18, 265–268. [Google Scholar] [CrossRef] [PubMed]
- Dinglasan, L.A.V.; Oh, J.C.; Schmitt, J.E.; Trerotola, S.O.; Shlansky-Golberg, R.D.; Stavropoulos, A.W. Complicated inferior vena cava filter retrievals: Associated factors identified at preretrieval, C.T. Radiology 2013, 266, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Spivack, S.; Kalker, E.; Samuels, D.; Orron, D.E. Filter placement in duplicated inferior vena cava. Isr. Med. Assoc. J. IMAJ 2001, 3, 459–460. [Google Scholar]
- Baheti, A.; Sheeran, D.; Patrie, J.; Sabri, S.S.; Angle, J.F.; Wilkins, L. Suprarenal Inferior Vena Cava Filter Placement and Retrieval: Safety Analysis. J. Vasc. Interv. Radiol. JVIR 2020, 31, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Lopera, J.E.; Barnes, L. A single center 10-year clinical experience with superior vena cava retrievable filters. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2020, 95, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Andreoli, J.M.; Lewandowski, R.J.; Vogelzang, R.L.; Ryu, R.K. Comparison of complication rates associated with permanent and retrievable inferior vena cava filters: A review of the MAUDE database. J. Vasc. Interv. Radiol. JVIR 2014, 25, 1181–1185. [Google Scholar] [CrossRef]
- Stein, P.D.; Matta, F.; Hughes, M.J. Continuing Use of Inferior Vena Cava Filters Despite Data and Recommendations Against Their Use in Patients With Deep Venous Thrombosis. Am. J. Cardiol. 2019, 124, 1643–1645. [Google Scholar] [CrossRef]
- Moriarty, H.K.; Marshall, E.; Clements, W. A 7-year retrospective review of the technical success of the “low-profile” hangman technique for complicated inferior vena cava (IVC) filter retrievals. Diagn. Interv. Radiol. 2020, 26, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Kassamali, R.H.; Burlak, K.; Lee, J.T.L.; Aberdein, G.; Harisis, G.; Goh, G.S.; Kavnoudias, H.; Clements, W. The Safety of Continuing Therapeutic Anticoagulation During Inferior Vena Cava Filter Retrieval: A 6-Year Retrospective Review from a Tertiary Centre. Cardiovasc. Interv. Radiol. 2019, 42, 1110–1116. [Google Scholar] [CrossRef]
- Kuo, W.T.; Tong, R.T.; Hwang, G.L.; Louie, J.D.; Lebowitz, E.A.; Sze, D.Y.; Hofmann, L.V. High-risk retrieval of adherent and chronically implanted IVC filters: Techniques for removal and management of thrombotic complications. J. Vasc. Interv. Radiol. JVIR 2009, 20, 1548–1556. [Google Scholar] [CrossRef]
- Kuo, W.T.; Doshi, A.A.; Ponting, J.M.; Rosenberg, J.K.; Liang, T.; Hofmann, L.V. Laser-Assisted Removal of Embedded Vena Cava Filters: A First-In-Human Escalation Trial in 500 Patients Refractory to High-Force Retrieval. J. Am. Heart Assoc. 2020, 9, e017916. [Google Scholar] [CrossRef] [PubMed]
- Crosby, D.A.; Ryan, K.; McEniff, N.; Dicker, P.; Regan, C.; Lynch, C.; Byrne, B. Retrievable Inferior vena cava filters in pregnancy: Risk versus benefit? Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 222, 25–30. [Google Scholar] [CrossRef] [PubMed]
| Indications | Class | Level |
|---|---|---|
| Absolute | ||
| IIa IIa | C C |
| Relative | ||
| IIb IIb IIb IIb IIb IIb | C C C C C C |
| Prophylaxis | ||
| IIb IIb | C C |
| Routine | ||
| III | A |
| Indication | ACCP | AHA | ESC | CIRSE | SIR | SEPAR |
|---|---|---|---|---|---|---|
| Absolute | ||||||
| VTE with contraindication ACT | Yes | Yes | Yes | Yes | Yes | Yes |
| Major complication with ACT | Yes | Yes | Yes | Yes | Yes | Yes |
| PE recurrent despite correct ACT | No | Yes | Yes | Yes | Consider | Consider |
| Relative | ||||||
| Massive PE and thrombectomy with/without fibrinolysis | No | Consider | No | Consider | Consider | - |
| Proximal floating thrombus | No | No | No | Consider | Consider | - |
| Thrombolysis/thrombectomy in proximal DVT | No | No | No | Consider | Consider | - |
| High-risk PE with poor pulmonary reserve | No | Consider | No | Yes | Yes | - |
| Chronic PE and PAH | No | No | No | Consider | No | - |
| Thromboendarterectomy | No | No | No | Consider | No | - |
| Prophylaxis | ||||||
| Trauma with high risk without possibility of ACT | No | No | No | Yes | No | - |
| Paraplegia without the possibility of ACT | - | - | No | Yes | No | - |
| Surgery with high-risk VTE | No | - | No | Consider | No | - |
| Technical Recommendation | |
|---|---|
| Image Guidance | Fluoroscopic guidance is recommended for placement and retrieval of IVCF compared to other imaging techniques. However, preprocedural imaging for filter retrieval is not necessary; some authors recommend abdominal CT before retrieval of the filter to rule out complications [57,64,65]. |
| Venous approach | Jugular, femoral, or brachial access can be used depending on operator skills, filter type, and favorable anatomy [13]. |
| Duplicated inferior vena cava | There are two possibilities: placement of a filter in each vena cava or a single filter in a suprarenal localization [66]. |
| Suprarenal placement of inferior vena cava filters | The main indication of the suprarenal filter is IVC thrombosis. Its retrieval should be the same as an infrarenal filter with a jugular approach [67]. |
| Superior vena cava filter | Superior vena cava filters are not recommended because there are limited indications with a high-risk of filter migration. However, some authors admit the safety and efficacy of the procedure [68]. |
| The positioning of the IVCF | It is important to ensure the position of the filter, avoiding angulations, tilting, or the introduction of the retriever hook into the renal veins. It is advisable to reposition it in the same procedure to guarantee proper placement of the filter and prevent future complications during retrieval [13]. |
| Estimated retrieval time | There is no clear retrieval time. It is recommended when the IVCF is no longer necessary and should be removed as soon as possible. The FDA recommends between 29 and 54 days [55,69,70]. |
| Anticoagulation therapy and inferior vena cava filters | If the patient has no contraindication for the ACT, it should be continued after filter placement, retrieval, or during the indwelling time of the IVCF. It is not necessary to discontinue the ACT for the retrieval procedure; however, it is advisable to determine a preoperative assessment of hemostasis before filter retrieval [57,71,72,73]. |
| Hospitalization | Hospital admission is not necessary [13]. |
| Recovery attempts | Sometimes, the IVCF, due to its positioning, inclination, or organ penetration, cannot be recovered on a first attempt. Additional maneuvers with special techniques are recommended. In the case of a lack of experience, it is recommended to send patients for advanced techniques for retrieval procedures in specialized centers. An IVCF can always be retrieved; however, it is important to evaluate the risk versus benefit of this procedure [13,74]. |
| IVC filters in pregnancy | There are limited data regarding retrievable IVCF in patients with high-risk VTE in pregnancy. Complications seem to be higher in pregnant patients with thrombosis and IVC penetration [75]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Gregorio, M.A.; Guirola, J.A.; Sierre, S.; Urbano, J.; Ciampi-Dopazo, J.J.; Abadal, J.M.; Pulido, J.; Eyheremendy, E.; Lonjedo, E.; Guerrero, G.; et al. Ibero-American Society of Interventionism (SIDI) and the Spanish Society of Vascular and Interventional Radiology (SERVEI) Standard of Practice (SOP) for the Management of Inferior Vena Cava Filters in the Treatment of Acute Venous Thromboembolism. J. Clin. Med. 2022, 11, 77. https://doi.org/10.3390/jcm11010077
De Gregorio MA, Guirola JA, Sierre S, Urbano J, Ciampi-Dopazo JJ, Abadal JM, Pulido J, Eyheremendy E, Lonjedo E, Guerrero G, et al. Ibero-American Society of Interventionism (SIDI) and the Spanish Society of Vascular and Interventional Radiology (SERVEI) Standard of Practice (SOP) for the Management of Inferior Vena Cava Filters in the Treatment of Acute Venous Thromboembolism. Journal of Clinical Medicine. 2022; 11(1):77. https://doi.org/10.3390/jcm11010077
Chicago/Turabian StyleDe Gregorio, Miguel A., Jose A. Guirola, Sergio Sierre, Jose Urbano, Juan Jose Ciampi-Dopazo, Jose M. Abadal, Juan Pulido, Eduardo Eyheremendy, Elena Lonjedo, Guadalupe Guerrero, and et al. 2022. "Ibero-American Society of Interventionism (SIDI) and the Spanish Society of Vascular and Interventional Radiology (SERVEI) Standard of Practice (SOP) for the Management of Inferior Vena Cava Filters in the Treatment of Acute Venous Thromboembolism" Journal of Clinical Medicine 11, no. 1: 77. https://doi.org/10.3390/jcm11010077






