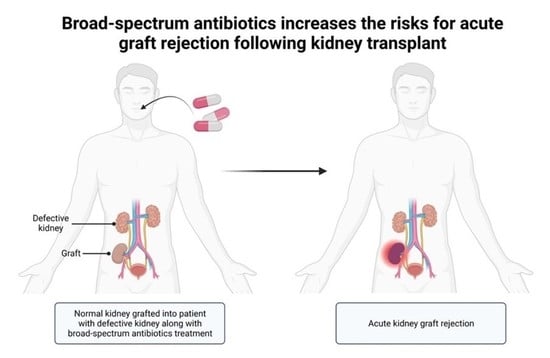
Piperacillin/Tazobactam and Meropenem Use Increases the Risks for Acute Graft Rejection Following First Kidney Transplantation
Abstract
:1. Introduction
2. Patients and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Patients
3.2. Acute Graft Rejection and Graft Survival
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghanem, S.; Kim, C.J.; Dutta, D.; Salifu, M.; Lim, S.H. Antimicrobial therapy during cancer treatment: Beyond antibacterial effects. J. Intern. Med. 2021, 290, 40–56. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Mazmanian, S.K. Has the microbiota played a critical role in the evolution of the adaptive immune system? Science 2010, 330, 1768–1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, J.; Kumar, A.; Parikh, K.; Anwar, A.; Knoll, B.M.; Puccio, C.; Chun, H.; Fanucchi, M.; Lim, S.H. Use of broad-spectrum antibiotics impacts outcome in patients treated with immune checkpoint inhibitors. Oncoimmunology 2018, 7, e1507670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Routy, B.; Le Chatelier, E.; Derosa, L.; Duong, C.P.; Alou, M.T.; Daillère, R.; Fluckiger, A.; Messaoudene, M.; Rauber, C.; Roberti, M.P.; et al. Gut microbiome influences efficacy of PD-1–based immunotherapy against epithelial tumors. Science 2018, 359, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Elgarten, C.W.; Li, Y.; Getz, K.D.; Hemmer, M.; Huang, Y.S.V.; Hall, M.; Wang, T.; Kitko, C.L.; Jagasia, M.H.; Nishihori, T.; et al. Broad-Spectrum Antibiotics and Risk of Graft-versus-Host Disease in Pediatric Patients Undergoing Transplantation for Acute Leukemia: Association of Carbapenem Use with the Risk of Acute Graft-versus-Host Disease. Transplant. Cell. Ther. 2021, 27, 177.e1–177.e8. [Google Scholar] [CrossRef]
- Shono, Y.; Docampo, M.D.; Peled, J.U.; Perobelli, S.M.; Velardi, E.; Tsai, J.J.; Slingerland, A.E.; Smith, O.M.; Young, L.F.; Gupta, J.; et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci. Transl. Med. 2016, 8, 339ra71. [Google Scholar] [CrossRef] [Green Version]
- Farowski, F.; Bücker, V.; Vehreschild, J.J.; Biehl, L.; Cruz-Aguilar, R.; Scheid, C.; Holtick, U.; Jazmati, N.; Wisplinghoff, H.; Cornely, O.A.; et al. Impact of choice, timing, sequence and combination of broad-spectrum antibiotics on the outcome of allogeneic haematopoietic stem cell transplantation. Bone Marrow Transplant. 2018, 53, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Garrido-Mesa, N.; Zarzuelo, A.; Gálvez, J. Minocycline: Far beyond an antibiotic. Br. J. Pharmacol. 2013, 169, 337–352. [Google Scholar] [CrossRef] [Green Version]
- Čulić, O.; Eraković, V.; Parnham, M.J. Anti-inflammatory effects of macrolide antibiotics. Eur. J. Pharmacol. 2001, 429, 209–229. [Google Scholar] [CrossRef]
- Galli, G.; Triulzi, T.; Proto, C.; Signorelli, D.; Imbimbo, M.; Poggi, M.; Fucà, G.; Ganzinelli, M.; Vitali, M.; Palmieri, D.; et al. Association between antibiotic-immunotherapy exposure ratio and outcome in metastatic non-small cell lung cancer. Lung Cancer 2019, 132, 72–78. [Google Scholar] [CrossRef]
- Williams, K.M.; Cheng, G.S.; Pusic, I.; Jagasia, M.; Burns, L.; Ho, V.T.; Pidala, J.; Palmer, J.; Johnston, L.; Mayer, S.; et al. Fluticasone, Azithromycin, and Montelukast Treatment for New-Onset Bronchiolitis Obliterans Syndrome after Hematopoietic Cell Transplantation. Biol. Blood Marrow Transplant. 2016, 22, 710–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kingah, P.L.; Muma, G.; Soubani, A. Azithromycin improves lung function in patients with post-lung transplant bronchiolitis obliterans syndrome: A meta-analysis. Clin. Transplant. 2014, 28, 906–910. [Google Scholar] [CrossRef] [PubMed]
- Stone, M.; Fortin, P.R.; Pacheco-Tena, C.; Inman, R.D. Should tetracycline treatment be used more extensively for rheumatoid arthritis? Metaanalysis demonstrates clinical benefit with reduction in disease activity. J. Rheumatol. 2003, 30, 2112–2122. [Google Scholar] [PubMed]
- Ory, E.M.; Yow, E.M. The use and abuse of the broad spectrum antibiotics. JAMA 1963, 185, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Palleja, A.; Mikkelsen, K.H.; Forslund, S.K.; Kashani, A.; Allin, K.H.; Nielsen, T.; Hansen, T.H.; Liang, S.; Feng, Q.; Zhang, C.; et al. Recovery of gut microbiota of healthy adults following antibiotic exposure. Nat. Microbiol. 2018, 3, 1255–1265. [Google Scholar] [CrossRef]
- Elvers, K.T.; Wilson, V.J.; Hammond, A.; Duncan, L.; Huntley, A.L.; Hay, A.D.; Van Der Werf, E.T. Antibiotic-induced changes in the human gut microbiota for the most commonly prescribed antibiotics in primary care in the UK: A systematic review. BMJ Open 2020, 10, e035677. [Google Scholar] [CrossRef]
- Transplant Trends. Available online: https://unos.org/data/transplant-trends/ (accessed on 20 February 2022).
- Organ Procurement and Transplantation Network (OPTN); Scientific Registry of Transplant Recipients: (SRTR). OPTN/SRTR 2011 Annual Data Report; Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation: Rockville, MD, USA, 2012.
- Australia and New Zealand Dialysis and Transplant Registry: 39th Annual Report, Chapter 8, Transplantation; Australia and New Zealand Dialysis and Transplant Registry: Adelaide, Australia, 2016.
- Clayton, P.A.; McDonald, S.P.; Russ, G.R.; Chadban, S.J. Long-term outcomes after acute rejection in kidney transplant recipients: An ANZDATA analysis. J. Am. Soc. Nephrol. 2019, 30, 1697–1707. [Google Scholar] [CrossRef]
- Assar, S.; Nosratabadi, R.; Khorramdel Azad, H.; Masoumi, J.; Mohamadi, M.; Hassanshahi, G. A review of immunomodulatory effects of fluoroquinolones. Immunol. Investig. 2021, 50, 1007–1026. [Google Scholar] [CrossRef]
- Murphy, B.S.; Sundareshan, V.; Cory, T.J.; Hayes, D., Jr.; Anstead, M.I.; Feola, D.J. Azithromycin alters macrophage phenotype. J. Antimicrob. Chemother. 2008, 61, 554–560. [Google Scholar] [CrossRef] [Green Version]
- Bahrami, F.; Morris, D.L.; Pourgholami, M.H. Tetracyclines: Drugs with huge therapeutic potential. Mini Rev. Med. Chem. 2012, 12, 44–52. [Google Scholar] [CrossRef]
- Eckburg, P.B.; Bik, E.M.; Bernstein, C.N.; Purdom, E.; Dethlefsen, L.; Sargent, M.; Gill, S.R.; Nelson, K.E.; Relman, D.A. Microbiology: Diversity of the human intestinal microbial flora. Science 2005, 308, 1635–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maier, E.; Anderson, R.C.; Roy, N.C. Understanding how commensal obligate anaerobic bacteria regulate immune functions in the large intestine. Nutrients 2014, 7, 45–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narushima, S.; Sugiura, Y.; Oshima, K.; Atarashi, K.; Hattori, M.; Suematsu, M.; Honda, K. Characterization of the 17 strains of regulatory T cell-inducing human-derived Clostridia. Gut Microbes 2014, 5, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Puong, K.Y.; Ouwehand, A.C.; Salminen, S. Displacement of bacterial pathogens from mucus and Caco-2 cell surface by lactobacilli. J. Med. Microbiol. 2003, 52, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Crost, E.H.; Ajandouz, E.H.; Villard, C.; Geraert, P.A.; Puigserver, A.; Fons, M. Ruminococcin C, a new anti-Clostridium perfringens bacteriocin produced in the gut by the commensal bacterium Ruminococcus gnavus E1. Biochimie 2011, 93, 1487–1494. [Google Scholar] [CrossRef]
- Hooper, L.V.; Xu, J.; Falk, P.G.; Midtvedt, T.; Gordon, J.I. A molecular sensor that allows a gut commensal to control its nutrient foundation in a competitive ecosystem. Proc. Natl. Acad. Sci. USA 1999, 96, 9833–9838. [Google Scholar] [CrossRef] [Green Version]
- Jenq, R.R.; Taur, Y.; Devlin, S.M.; Ponce, D.M.; Goldberg, J.D.; Ahr, K.F.; Littmann, E.R.; Ling, L.; Gobourne, A.C.; Miller, L.C.; et al. Intestinal Blautia is associated with reduced death from graft-versus-host disease. Biol. Blood Marrow Transplant. 2015, 21, 1373–1383. [Google Scholar] [CrossRef] [Green Version]
- Smith, M.; Dai, A.; Ghilardi, G.; Amelsberg, K.V.; Devlin, S.M.; Pajarillo, R.; Slingerland, J.B.; Beghi, S.; Herrera, P.S.; Giardina, P.; et al. Gut microbiome correlates of response and toxicity following anti-CD19 CAR T cell therapy. Nat. Med. 2022, 28, 713–723. [Google Scholar] [CrossRef]
- Creta, M.; Calogero, A.; Sagnelli, C.; Peluso, G.; Incollingo, P.; Candida, M.; Minieri, G.; Longo, N.; Fusco, F.; Tammaro, V.; et al. Donor and Recipient Outcomes following Robotic-Assisted Laparoscopic Living Donor Nephrectomy: A Systematic Review. BioMed Res. Int. 2019, 2019, 1729138. [Google Scholar] [CrossRef]
- Sagnelli, C.; Sica, A.; Gallo, M.; Peluso, G.; Varlese, F.; D’Alessandro, V.; Ciccozzi, M.; Crocetto, F.; Garofalo, C.; Fiorelli, A.; et al. Renal involvement in COVID-19: Focus on kidney transplant sector. Infection 2021, 49, 1265–1275. [Google Scholar] [CrossRef]




| No Antibiotic (n = 286) | Antibiotics (n = 71) | p Value | |
|---|---|---|---|
| Age (years) | |||
| Median | 53 | 50 | N.S. |
| Range | 7–76 | 13–74 | |
| Gender (F:M) | 117:169 | 26:45:00 | N.S. |
| Median Follow-up (days) | 1269.5 | 1270 | N.S. |
| Number of HLA mismatch | |||
| 6/6 antigens | 51 (17.5%) | 15 (21.1%) | N.S. |
| 5/6 antigens | 100 (35.1%) | 23 (32.4%) | N.S. |
| 4/6 antigens | 57 (20%) | 13 (18.3%) | N.S. |
| 3/6 antigens | 40 14%) | 11 (15.5%) | N.S. |
| 2/6 antigens | 16 (5.6%) | 5 (7%) | N.S. |
| 1/6 antigens | 2 (0.7%) | 0 (0%) | N.S. |
| 0/6 antigens | 20 (7%) | 4 (5.6%) | N.S. |
| Kidney donor source | |||
| Deceased donor | 226 (79%) | 64 (90%) | 0.04 |
| Living donor | 60 (21%) | 7 (10%) |
| Pre-Transplant (n) | Immediately Post-Transplant (n) |
|---|---|
| Urinary tract infection (7) Soft tissue infection (5) Bacteremia (1) Pneumonia (1) Latent tuberculosis (1) Bacteruria (1) Asthma exacerbation (1) Sinusitis (1) Upper respiratory infection (1) | Bacteruria (18) Donor bacteruria (8) Donor bacteremia (8) Soft tissue infection (7) Bacteremia/septicemia (4) Contaminated organ (4) Pneumonia (3) History of infective endocarditis (1) Peritonitis (1) Donor positive bronchial washing (1) |
| PM Exposure (n = 32) | No PM Exposure (n = 325) | p Value | |
|---|---|---|---|
| Age (years) | |||
| Median | 54 | 51 | N.S. |
| Range | 13–70 | 7–76 | |
| Gender (F:M) | 14:18 | 128:197 | N.S. |
| Number of HLA mismatch | |||
| 6/6 antigens | 8 (25%) | 57 (17.5%) | N.S. |
| 5/6 antigens | 11 (34.4%) | 112 (34.5%) | N.S. |
| 4/6 antigens | 6 (18.8%) | 64 (19.7%) | N.S. |
| 3/6 antigens | 3 (9.4%) | 48 (14.8%) | N.S. |
| 2/6 antigens | 2 (6.3%) | 19 (5.8%) | N.S. |
| 1/6 antigens | 0 (0%) | 2 (0.6%) | N.S. |
| 0/6 antigens | 2 (6.3%) | 23 (7.1%) | N.S. |
| Kidney donor source | |||
| Deceased donor | 29 (90.6%) | 261 (80.3%) | N.S. |
| Living donor | 3 (9.4%) | 64 (19.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nasr, D.; Moein, M.; Niforatos, S.; Nasr, S.; Ombada, M.; Khokhar, F.; Shahnawaz, M.; Poudyal, B.; Bou Zerdan, M.; Dutta, D.; et al. Piperacillin/Tazobactam and Meropenem Use Increases the Risks for Acute Graft Rejection Following First Kidney Transplantation. J. Clin. Med. 2022, 11, 2726. https://doi.org/10.3390/jcm11102726
Nasr D, Moein M, Niforatos S, Nasr S, Ombada M, Khokhar F, Shahnawaz M, Poudyal B, Bou Zerdan M, Dutta D, et al. Piperacillin/Tazobactam and Meropenem Use Increases the Risks for Acute Graft Rejection Following First Kidney Transplantation. Journal of Clinical Medicine. 2022; 11(10):2726. https://doi.org/10.3390/jcm11102726
Chicago/Turabian StyleNasr, Dayana, Mahmoudreza Moein, Stephanie Niforatos, Sandy Nasr, Mulham Ombada, Farzam Khokhar, Myera Shahnawaz, Bhavya Poudyal, Maroun Bou Zerdan, Dibyendu Dutta, and et al. 2022. "Piperacillin/Tazobactam and Meropenem Use Increases the Risks for Acute Graft Rejection Following First Kidney Transplantation" Journal of Clinical Medicine 11, no. 10: 2726. https://doi.org/10.3390/jcm11102726
APA StyleNasr, D., Moein, M., Niforatos, S., Nasr, S., Ombada, M., Khokhar, F., Shahnawaz, M., Poudyal, B., Bou Zerdan, M., Dutta, D., Saidi, R. F., & Lim, S. H. (2022). Piperacillin/Tazobactam and Meropenem Use Increases the Risks for Acute Graft Rejection Following First Kidney Transplantation. Journal of Clinical Medicine, 11(10), 2726. https://doi.org/10.3390/jcm11102726